Abstract
-
Background
Mental health problems are emerging issues in occupational safety and health, whereas the findings on the relationship between physical hazards and mental health are not consistent. The aim of our study was to investigate the association between physical hazard exposure and mental health outcomes including depression and anxiety.
-
Methods
We included 48,476 participants from the fifth Korean Working Conditions Survey (KWCS) in this study. The χ2 test and logistic regression analyses were conducted to assess the association between physical hazard exposures and mental health. All statistical analyses were performed sex-specifically.
-
Results
In logistic regression analysis, the odds ratios (ORs) of depression were significantly increased in male workers who were exposed to vibration (severe OR: 1.54, 95% confidence interval [CI]: 1.21–1.95) and noise (severe OR: 1.93, 95% CI: 1.49–2.48) whereas the ORs of depression were not significant in female workers from vibration (severe OR: 0.86, 95% CI: 0.50–1.38) or noise exposure (severe OR: 1.39, 95% CI: 0.84–2.17). The ORs of anxiety were significantly increased in male workers with vibration (severe OR: 1.76, 95% CI: 1.43–2.15) and noise exposure (severe OR: 2.12, 95% CI: 1.69–2.63) whereas the OR between vibration and anxiety (severe OR: 1.45, 95% CI: 0.91–2.21) was not significant in female workers. High or low temperature exposure had significant associations with depression and anxiety in both male and female subjects.
-
Conclusions
Results of our study suggest that physical hazard exposures may be associated with increased risk of mental health problems including depression and anxiety. These associations are more prominent in male workers in comparison with female workers.
-
Keywords: Noise; Vibration; Temperature; Mental health; Depression; Anxiety
BACKGROUND
Mental health problems are emerging occupational safety and health issues worldwide including in South Korea.
1,2 Mental and substance use disorders cause significant disease burden and their estimated prevalence is greater than one billion.
3 One hundred-sixty-two-point-five million disability-adjusted life years (DALYs) were lost due to mental health conditions in 2016 which corresponds to 6.8% of all DALYs lost.
3 Mental disorders lead to workers' sickness absence, presenteeism and productivity loss.
4 Productivity loss due to unemployment, disability, and lower work performance is one of the major sources of the disease burden of mental illness.
5 Among various mental health conditions, depressive and anxiety disorders show the largest mental illness burden and the highest prevalence.
3,4
Until the present day, numerous studies were conducted on psychosocial risk factors of mental health problems in workers. Harvey et al.
6 suggested an unifying model of workplace risk factors which consist of three main domains: imbalanced job design, occupational uncertainty, and lack of value and respect in the workplace. Systematic review and meta-analysis on stress-related mental disorders
7 and sickness absence due to mental disorder
8 reported effort-reward imbalance, low organizational justice, high job demands, high psychological demands, low job control, and low reward as important work-related psychosocial risk factors. Sohn et al.
9 suggested that high workload, high emotional labor, and low social support are significantly related to higher odds for depressive symptoms.
However, only a limited number studies researched the association between mental health and physical risk factors in the workplace.
10 Joh et al.
11 conducted a cross-sectional study using 1st Korean Working Conditions Survey (KWCS) data to identify the association between physical or chemical hazard exposures and mental health problems. Whole-body oscillation, noise and high temperature exposures show significantly high odds ratios (ORs) of mental health problems including sleep disorders, anxiety or depression. Russo et al.
10 reported a positive correlation between low temperature and mental health outcomes from the 5th European Working Conditions Survey (EWCS) data. Nari et al.
12 demonstrated the positive association between vibration and noise plus vibration exposure and insomnia in both male and female subjects by analyzing 5th KWCS data. Furthermore, using data from the Thai Cohort Study, high ORs of psychological distress and low life satisfaction were observed in subjects with higher physical hazard scores.
13 On the other hand, results from the SUrveillance Médicale des Expositions aux Risques professionnels (SUMER) study demonstrated an insignificant association between physical hazard exposures and depression in the French working population.
14
Mental health issues in occupational health have become important problems in recent years, and so far, there are no consistent findings on the relationship between physical hazards and mental health outcomes. Thus, our study investigated the association between physical hazardous agent exposures such as vibration, noise, high and low temperatures and mental health problems including depression and anxiety in the Korean working population.
METHODS
Participants
This study utilized the data of the 5th KWCS which was conducted in 2017 by the Korea Occupational Safety and Health Agency. The KWCS adopted the European Union's EWCS and the UK Labor Force Survey. The KWCS investigated components of the workplace environment such as working pattern, employment pattern, job classification, employment stability and hazardous agent exposure. The population of the KWCS is based on the 2010 Population and Housing Census and consists of the active working population of Koreans aged 15 years or older.
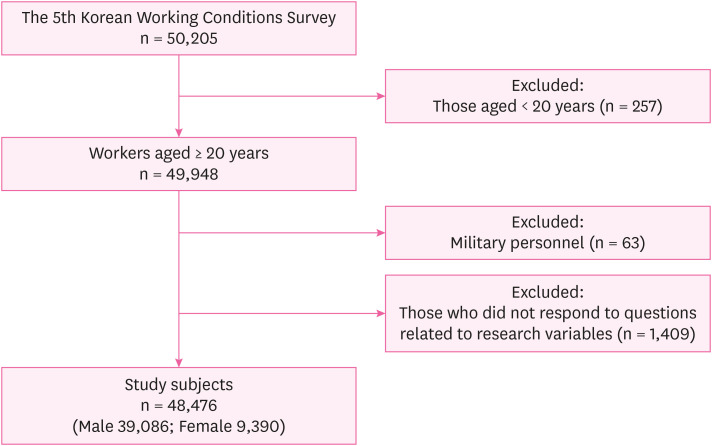
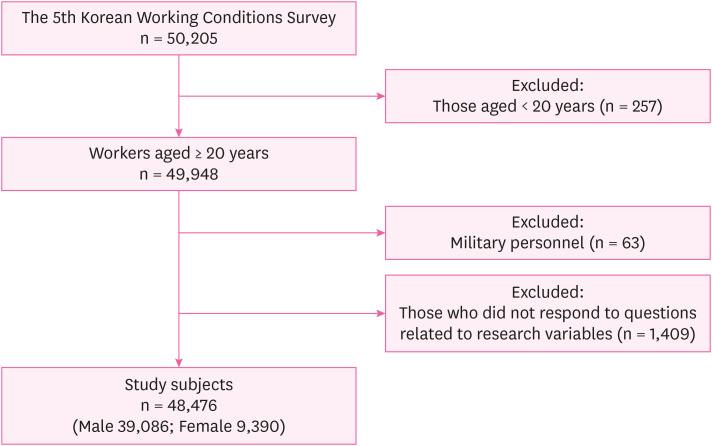
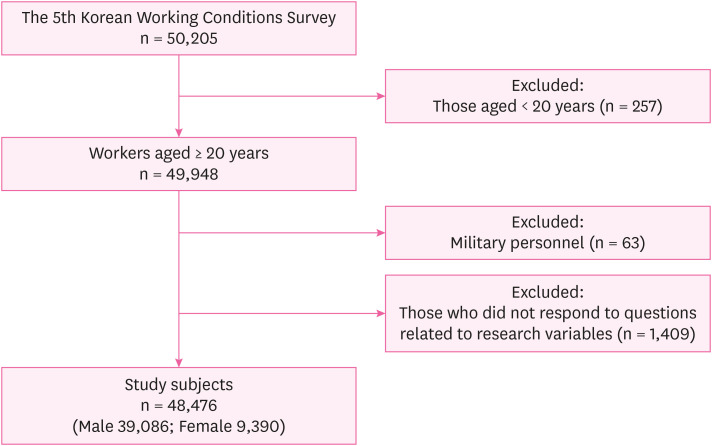
Overall, 50,205 workers participated in the 5th KWCS. To represent the general working population, employees younger than 20 years old (n = 257) and military personnel (n = 63) were excluded from the study population. After exclusion of those who did not respond to questions related to research variables (n = 1,402), the final study population included 48,476 participants. Among the study subjects, 39,086 were male (80.6%) and 9,390 were female (19.4%) (
Fig. 1).
Fig. 1Flowchart of the selection of study subjects.
Main variables
Physical hazardous agents (vibration, noise, high and low temperatures) exposure was assessed by the following questions: “Please tell me, using the following scale, are you exposed at work to…?” The participants could subjectively respond to each question on 7 steps (never, almost never, around 1/4 of the time, around half of the time, around 3/4 of the time, almost all the time and all the time). The subjects were classified into three exposure categories according to their answer: never (never, almost never), moderate (around 1/4 of the time, around half of the time) and severe (around 3/4 of the time, almost all the time, all the time).
Anxiety and depression were identified with the following question: “Over the last 12 months, did you have any of the following health problems?” The respondents answered “Yes” or “No” to the “depressive mood” and “anxious mood” sections.
Covariates
Individual factors (age, monthly income) and occupational factors (job classification, employment status, working time, personal protective equipment [PPE] usage, working duration) were considered as potential confounding variables. Age was split into five groups: 20s, 30s, 40s, 50s, and aged 60 years or older. Monthly income was divided into two levels: less than 2 million Korean won (KRW), and two million KRW or more. Jobs were classified into four groups according to the Korean Standard Occupational Classification (6th revision): office workers (managers, professionals and related workers, clerks), service and sales workers (service workers, sales workers), skilled agricultural, forestry and fishery workers, and manual workers (craft and related trades workers, equipment, machine operating and assembling workers, elementary workers). Employment status was divided into three categories: full-time, part-time, and self-employed. Working time was split into three groups: 40 hours per week or below, 40–52 hours per week, and more than 52 hours per week. The PPE usage habits were evaluated by two questions: “Does your job ever require that you wear personal protective equipment?” and “Do you always use it when it is required?” Subjects who responded “No” to the former question were classified as the “No need” group. Those who responded “Yes” to the former question were asked the latter question. Subjects who answered “Yes” to the latter question were sorted into the “Need/wear” group whereas subjects who answered “No” to the latter question were sorted into the “Need/no wear” group. KWCS includes a question which assess working duration in current company or organization: "How many years have you been in your company or organization?" Working duration was classified into two groups: less than 10 years and 10 years or longer.
Statistical analysis
Study participants were separated into male and female groups to conduct statistical analyses because of differences in physical job demands and mental health responses.
15 The χ
2 test was applied to compare the general characteristics of the study subjects according to the self-reported depression and anxiety. Logistic regression analysis was performed to assess the association between each physical hazardous agent exposure, and depression and anxiety. The OR and 95% confidence interval (CI) were calculated. Regression models were adjusted for age, monthly income, job classification, employment status, working time, PPE usage and working duration. Subgroup analysis was conducted to evaluate the effects of simultaneous vibration and noise exposure on depression and anxiety. None exposure group was compared using logistic regression analysis with the single exposure to vibration or noise group and the multiple exposure to vibration and noise exposure group. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
This study was conducted after obtaining an approval from the Institutional Review Board (IRB) of Korea University Medical Center (IRB No. 2021AS0133).
RESULTS
General characteristics of the study population are described in
Table 1. The proportion of workers in their 20s and over 60s was higher in female workers. The percentage of monthly income exceeding 2 million KRW was higher in male workers. Both male and female subjects had the highest portion of service and sales workers whereas the percentage of office workers and manual workers were greater in male workers. The proportion of full-time workers was higher in male subjects and male workers reported longer working time. The PPE requirement was higher in male workers in comparison with female workers. The proportion of workers with working duration less than 10 years was higher in female workers. Male workers were more likely to be exposed to vibration and noise and exposure to high or low temperatures was more frequent in female workers.
Table 1 General characteristics of subjects
|
Characteristics |
Male (n = 39,086) |
Female (n = 9,390) |
|
No. (%) |
No. (%) |
|
Age (years) |
|
|
|
20–29 |
3,009 (7.7) |
1,113 (11.9) |
|
30–39 |
7,136 (18.3) |
1,180 (12.6) |
|
40–49 |
10,011 (25.6) |
1,460 (15.6) |
|
50–59 |
10,614 (27.2) |
2,230 (23.8) |
|
≥ 60 |
8,316 (21.3) |
3,407 (36.3) |
|
Income (million Korean won) |
|
|
|
< 2 |
13,326 (34.1) |
5,471 (58.3) |
|
≥ 2 |
25,760 (65.9) |
3,919 (41.7) |
|
Job |
|
|
|
Office workers |
11,516 (29.5) |
1,858 (19.8) |
|
Service and sales workers |
14,302 (36.6) |
4,251 (45.3) |
|
Skilled agricultural, forestry and fishery workers |
2,968 (7.6) |
1,284 (13.7) |
|
Manual workers |
10,300 (26.4) |
1,997 (21.3) |
|
Status |
|
|
|
Full-time |
19,238 (49.2) |
3,627 (38.6) |
|
Part-time |
4,944 (12.7) |
1,808 (19.3) |
|
Self-employed |
14,904 (38.1) |
3,955 (42.1) |
|
Working time (hours) |
|
|
|
≤ 40 |
18,344 (46.9) |
5,105 (54.4) |
|
40–52 |
10,609 (27.1) |
2,169 (23.1) |
|
> 52 |
10,133 (25.9) |
2,116 (22.5) |
|
PPE |
|
|
|
No need |
27,366 (70.0) |
7,048 (75.1) |
|
Need/wear |
10,312 (26.4) |
1,939 (20.7) |
|
Need/no wear |
1,408 (3.6) |
403 (4.3) |
|
Duration (years) |
|
|
|
< 10 |
22,806 (58.4) |
5,969 (63.6) |
|
≥ 10 |
16,280 (41.7) |
3,421 (36.4) |
|
Vibration |
|
|
|
None |
29,457 (75.4) |
7,908 (84.2) |
|
Moderate |
6,354 (16.3) |
1,024 (10.9) |
|
Severe |
3,275 (8.4) |
458 (4.9) |
|
Noise |
|
|
|
None |
31,194 (79.8) |
8,013 (85.3) |
|
Moderate |
5,807 (14.9) |
1,005 (10.7) |
|
Severe |
2,085 (5.3) |
372 (4.0) |
|
High temperature |
|
|
|
None |
29,045 (74.3) |
6,883 (73.3) |
|
Moderate |
6,773 (17.3) |
1,574 (16.8) |
|
Severe |
3,268 (8.4) |
933 (9.9) |
|
Low temperature |
|
|
|
None |
31,131 (79.7) |
7,435 (79.2) |
|
Moderate |
5,678 (14.5) |
1,294 (13.8) |
|
Severe |
2,277 (5.8) |
661 (7.0) |
The prevalence of depression and anxiety according to individual and occupational characteristics of subjects is presented in
Tables 2 and
3. Prevalence of both depression and anxiety was higher in female workers (4.4% and 4.0%, respectively) than male workers (2.4% and 3.0%, respectively). The distributions of age, job classification, employment status, working time, PPE-wearing behavior, working duration and physical hazardous agent (vibration, noise, high temperature, low temperature) exposures in male workers show statistically significant differences (
p < 0.05) between the normal mood group and the depressive or anxious mood groups. The distribution of monthly income was significantly different between normal and depressive mood groups in male workers. In female workers, the distributions of age, employment status, working time, PPE-wearing behavior, working duration and exposure to high or low temperature show statistically significant differences between the normal mood group and depressive or anxious mood groups. The distributions of monthly income and job classification were significantly different between the normal and depressive mood groups in female workers. The distribution of noise exposure was significantly different between the normal and anxious mood groups in female workers.
Table 2 Prevalence of depression according to characteristics of subjects stratified by sex
|
Depression |
Male (n = 39,086) |
Female (n = 9,390) |
|
No |
Yes |
p
|
No |
Yes |
p
|
|
No. (%) |
No. (%) |
No. (%) |
No. (%) |
|
Total |
38,166 (97.7) |
920 (2.4) |
|
8,977 (95.6) |
413 (4.4) |
|
|
Age (years) |
|
|
< 0.001***
|
|
|
< 0.001***
|
|
20–29 |
2,958 (98.3) |
51 (1.7) |
1,091 (98.0) |
22 (2.0) |
|
30–39 |
7,019 (98.4) |
117 (1.6) |
1,147 (97.2) |
33 (2.8) |
|
40–49 |
9,781 (97.7) |
230 (2.3) |
1,419 (97.2) |
41 (2.8) |
|
50–59 |
10,365 (97.7) |
249 (2.4) |
2,122 (95.2) |
108 (4.8) |
|
≥ 60 |
8,043 (96.7) |
273 (3.3) |
3,198 (93.9) |
209 (6.1) |
|
Income (million Korean won) |
|
|
< 0.001***
|
|
|
< 0.001***
|
|
< 2 |
12,924 (97.0) |
402 (3.0) |
5,178 (94.6) |
293 (5.4) |
|
≥ 2 |
25,242 (98.0) |
518 (2.0) |
3,799 (96.9) |
120 (3.1) |
|
Job |
|
|
< 0.001***
|
|
|
< 0.001***
|
|
Office workers |
11,299 (98.1) |
217 (1.9) |
1,815 (97.7) |
43 (2.3) |
|
Service and sales workers |
13,956 (97.6) |
346 (2.4) |
4,074 (95.8) |
177 (4.2) |
|
Skilled agricultural, forestry and fishery workers |
2,869 (96.7) |
99 (3.3) |
1,202 (93.6) |
82 (6.4) |
|
Manual workers |
10,042 (97.5) |
258 (2.5) |
1,886 (94.4) |
111 (5.6) |
|
Status |
|
|
< 0.001***
|
|
|
< 0.001***
|
|
Full-time |
18,863 (98.1) |
375 (2.0) |
3,512 (96.8) |
115 (3.2) |
|
Part-time |
4,808 (97.3) |
136 (2.8) |
1,737 (96.1) |
71 (3.9) |
|
Self-employed |
14,495 (97.3) |
409 (2.7) |
3,728 (94.3) |
227 (5.7) |
|
Working time (hours) |
|
|
< 0.001***
|
|
|
0.019*
|
|
≤ 40 |
17,952 (97.9) |
392 (2.1) |
4,867 (95.3) |
238 (4.7) |
|
40–52 |
10,376 (97.8) |
233 (2.2) |
2,097 (96.7) |
72 (3.3) |
|
> 52 |
9,838 (97.1) |
295 (2.9) |
2,013 (95.1) |
103 (4.9) |
|
PPE |
|
|
< 0.001***
|
|
|
< 0.001***
|
|
No need |
26,724 (97.7) |
642 (2.4) |
6,761 (95.9) |
287 (4.1) |
|
Need/wear |
10,099 (97.9) |
213 (2.1) |
1,854 (95.6) |
85 (4.4) |
|
Need/no wear |
1,343 (95.4) |
65 (4.6) |
362 (89.8) |
41 (10.2) |
|
Duration (years) |
|
|
0.002**
|
|
|
< 0.001***
|
|
< 10 |
22,316 (97.9) |
490 (2.2) |
5,753 (96.4) |
216 (3.6) |
|
≥ 10 |
15,850 (97.4) |
430 (2.6) |
3,224 (94.2) |
197 (5.8) |
|
Vibration |
|
|
0.002**
|
|
|
0.095 |
|
None |
28,809 (97.8) |
648 (2.2) |
7,570 (95.7) |
338 (4.3) |
|
Moderate |
6,178 (97.2) |
176 (2.8) |
966 (94.3) |
58 (5.7) |
|
Severe |
3,179 (97.1) |
96 (2.9) |
441 (96.3) |
17 (3.7) |
|
Noise |
|
|
< 0.001***
|
|
|
0.063 |
|
None |
30,509 (97.8) |
685 (2.2) |
7,677 (95.8) |
336 (4.2) |
|
Moderate |
5,647 (97.2) |
160 (2.8) |
948 (94.3) |
57 (5.7) |
|
Severe |
2,010 (96.4) |
75 (3.6) |
352 (94.6) |
20 (5.4) |
|
High temperature |
|
|
< 0.001***
|
|
|
< 0.001***
|
|
None |
28,468 (98.0) |
577 (2.0) |
6,651 (96.6) |
232 (3.4) |
|
Moderate |
6,561 (96.9) |
212 (3.1) |
1,453 (92.3) |
121 (7.7) |
|
Severe |
3,137 (96.0) |
131 (4.0) |
873 (93.6) |
60 (6.4) |
|
Low temperature |
|
|
< 0.001***
|
|
|
< 0.001***
|
|
None |
30,449 (97.8) |
682 (2.2) |
7,145 (96.1) |
290 (3.9) |
|
Moderate |
5,510 (97.0) |
168 (3.0) |
1,213 (93.7) |
81 (6.3) |
|
Severe |
2,207 (96.9) |
70 (3.1) |
619 (93.7) |
42 (6.4) |
Table 3 Prevalence of anxiety according to characteristics of subjects stratified by sex
|
Anxiety |
Male (n = 39,086) |
Female (n = 9,390) |
|
No |
Yes |
p
|
No |
Yes |
p
|
|
No. (%) |
No. (%) |
No. (%) |
No. (%) |
|
Total |
37,924 (97.0) |
1,162 (3.0) |
|
9,013 (96.0) |
377 (4.0) |
|
|
Age (years) |
|
|
< 0.001***
|
|
|
< 0.001***
|
|
20–29 |
2,941 (97.7) |
68 (2.3) |
1,084 (97.4) |
29 (2.6) |
|
30–39 |
6,972 (97.7) |
164 (2.3) |
1,140 (96.6) |
40 (3.4) |
|
40–49 |
9,701 (96.9) |
310 (3.1) |
1,421 (97.3) |
39 (2.7) |
|
50–59 |
10,258 (96.7) |
356 (3.4) |
2,119 (95.0) |
111 (5.0) |
|
≥ 60 |
8,052 (96.8) |
264 (3.2) |
3,249 (95.4) |
158 (4.6) |
|
Income (million Korean won) |
|
|
0.213 |
|
|
0.051 |
|
< 2 |
12,910 (96.9) |
416 (3.1) |
5,233 (95.7) |
238 (4.4) |
|
≥ 2 |
25,014 (97.1) |
746 (2.9) |
3,780 (96.5) |
139 (3.6) |
|
Job |
|
|
0.008**
|
|
|
0.170 |
|
Office workers |
11,221 (97.4) |
295 (2.6) |
1,797 (96.7) |
61 (3.3) |
|
Service and sales workers |
13,831 (96.7) |
471 (3.3) |
4,075 (95.9) |
176 (4.1) |
|
Skilled agricultural, forestry and fishery workers |
2,881 (97.1) |
87 (2.9) |
1,222 (95.2) |
62 (4.8) |
|
Manual workers |
9,991 (97.0) |
309 (3.0) |
1,919 (96.1) |
78 (3.9) |
|
Status |
|
|
< 0.001***
|
|
|
< 0.001***
|
|
Full-time |
18,739 (97.4) |
499 (2.6) |
3,514 (96.9) |
113 (3.1) |
|
Part-time |
4,801 (97.1) |
143 (2.9) |
1,743 (96.4) |
65 (3.6) |
|
Self-employed |
14,384 (96.5) |
520 (3.5) |
3,756 (95.0) |
199 (5.0) |
|
Working time (hours) |
|
|
< 0.001***
|
|
|
0.019*
|
|
≤ 40 |
17,882 (97.5) |
462 (2.5) |
4,902 (96.0) |
203 (4.0) |
|
40–52 |
10,290 (97.0) |
319 (3.0) |
2,099 (96.8) |
70 (3.2) |
|
> 52 |
9,752 (96.2) |
381 (3.8) |
2,012 (95.1) |
104 (4.9) |
|
PPE |
|
|
< 0.001***
|
|
|
< 0.001***
|
|
No need |
26,557 (97.0) |
809 (3.0) |
6,774 (96.1) |
274 (3.9) |
|
Need/wear |
10,032 (97.3) |
280 (2.7) |
1,867 (96.3) |
72 (3.7) |
|
Need/no wear |
1,335 (94.8) |
73 (5.2) |
372 (92.3) |
31 (7.7) |
|
Duration (years) |
|
|
0.005**
|
|
|
0.002**
|
|
< 10 |
22,174 (97.2) |
632 (2.8) |
5,758 (96.5) |
211 (3.5) |
|
≥ 10 |
15,750 (96.7) |
530 (3.3) |
3,255 (95.2) |
166 (4.9) |
|
Vibration |
|
|
< 0.001***
|
|
|
0.082 |
|
None |
28,651 (97.3) |
806 (2.7) |
7,606 (96.2) |
302 (3.8) |
|
Moderate |
6,135 (96.6) |
219 (3.5) |
972 (94.9) |
52 (5.1) |
|
Severe |
3,138 (95.8) |
137 (4.2) |
435 (95.0) |
23 (5.0) |
|
Noise |
|
|
< 0.001***
|
|
|
< 0.001***
|
|
None |
30,352 (97.3) |
842 (2.7) |
7,717 (96.3) |
296 (3.7) |
|
Moderate |
5,590 (96.3) |
217 (3.7) |
946 (94.1) |
59 (5.9) |
|
Severe |
1,982 (95.1) |
103 (4.9) |
350 (94.1) |
22 (5.9) |
|
High temperature |
|
|
< 0.001***
|
|
|
< 0.001***
|
|
None |
28,316 (97.5) |
729 (2.5) |
6,653 (96.7) |
230 (3.3) |
|
Moderate |
6,494 (95.9) |
279 (4.1) |
1,484 (94.3) |
90 (5.7) |
|
Severe |
3,114 (95.3) |
154 (4.7) |
876 (93.9) |
57 (6.1) |
|
Low temperature |
|
|
< 0.001***
|
|
|
< 0.001***
|
|
None |
30,330 (97.4) |
801 (2.6) |
7,171 (96.5) |
264 (3.6) |
|
Moderate |
5,428 (95.6) |
250 (4.4) |
1,226 (94.7) |
68 (5.3) |
|
Severe |
2,166 (95.1) |
111 (4.9) |
616 (93.2) |
45 (6.8) |
Tables 4 and
5 present the crude odds ratios (CORs) and adjusted odds ratios (AORs) from logistic regression analyses according to the sex of study participants which compare mood symptoms of moderate and severe exposure groups with those of the no exposure group. In male subjects, the AORs of depression for moderate and severe vibration exposure were 1.28 (95% CI: 1.06–1.53) and 1.54 (95% CI: 1.21–1.95), respectively. The individual AORs of depression for moderate and severe noise exposure were 1.32 (95% CI: 1.10–1.58) and 1.93 (95% CI: 1.49–2.48). The respective AORs of depression for moderate and severe high temperature exposure were 1.56 (95% CI: 1.31–1.85) and 2.06 (95% CI: 1.67–2.54). The individual AORs of depression for moderate and severe low temperature exposure were 1.27 (95% CI: 1.06–1.51) and 1.38 (95% CI: 1.06–1.76). In female subjects, the AORs of depression for vibration and noise exposure were not statistically significant at any level of exposure. The AORs of depression for moderate and severe high temperature exposure were 1.89 (95% CI: 1.47–2.41) and 1.59 (95% CI: 1.15–2.16), respectively, which showed a higher risk in the moderate exposure group. In the case of low temperature exposure, only the severe exposure group had a statistically significant AOR (1.48, 95% CI: 1.04–2.06).
Table 4 CORs and AORs for depression according to physical hazardous agents stratified by sex
|
Depression |
Male |
Female |
|
COR (95% CI) |
AORa (95% CI) |
COR (95% CI) |
AORa (95% CI) |
|
Vibration |
|
|
|
|
|
None |
|
|
|
|
|
Moderate |
1.27 (1.07–1.50) |
1.28 (1.06–1.53) |
1.35 (1.00–1.78) |
1.16 (0.86–1.55) |
|
Severe |
1.34 (1.07–1.66) |
1.54 (1.21–1.95) |
0.86 (0.51–1.38) |
0.86 (0.50–1.38) |
|
Noise |
|
|
|
|
|
None |
|
|
|
|
|
Moderate |
1.26 (1.06–1.50) |
1.32 (1.10–1.58) |
1.38 (1.02–1.82) |
1.28 (0.95–1.71) |
|
Severe |
1.66 (1.29–2.10) |
1.93 (1.49–2.48) |
1.30 (0.79–2.01) |
1.39 (0.84–2.17) |
|
High temperature |
|
|
|
|
|
None |
|
|
|
|
|
Moderate |
1.59 (1.36–1.87) |
1.56 (1.31–1.85) |
2.39 (1.90–2.99) |
1.89 (1.47–2.41) |
|
Severe |
2.06 (1.69–2.49) |
2.06 (1.67–2.54) |
1.97 (1.46–2.62) |
1.59 (1.15–2.16) |
|
Low temperature |
|
|
|
|
|
None |
|
|
|
|
|
Moderate |
1.36 (1.14–1.61) |
1.27 (1.06–1.51) |
1.65 (1.27–2.11) |
1.29 (0.98–1.67) |
|
Severe |
1.42 (1.09–1.80) |
1.38 (1.06–1.76) |
1.67 (1.18–2.31) |
1.48 (1.04–2.06) |
Table 5 CORs and AORs for anxiety according to physical hazardous agents stratified by sex
|
Anxiety |
Male |
Female |
|
COR (95% CI) |
AORa (95% CI) |
COR (95% CI) |
AORa (95% CI) |
|
Vibration |
|
|
|
|
|
None |
|
|
|
|
|
Moderate |
1.27 (1.09–1.47) |
1.33 (1.12–1.57) |
1.35 (0.99–1.81) |
1.30 (0.95–1.77) |
|
Severe |
1.55 (1.29–1.86) |
1.76 (1.43–2.15) |
1.33 (0.84–2.01) |
1.45 (0.91–2.21) |
|
Noise |
|
|
|
|
|
None |
|
|
|
|
|
Moderate |
1.40 (1.20–1.63) |
1.47 (1.25–1.72) |
1.63 (1.21–2.15) |
1.61 (1.19–2.13) |
|
Severe |
1.87 (1.51–2.30) |
2.12 (1.69–2.63) |
1.64 (1.02–2.50) |
1.79 (1.11–2.76) |
|
High temperature |
|
|
|
|
|
None |
|
|
|
|
|
Moderate |
1.67 (1.45–1.92) |
1.76 (1.51–2.04) |
1.75 (1.36–2.24) |
1.66 (1.27–2.17) |
|
Severe |
1.92 (1.60–2.29) |
2.15 (1.77–2.60) |
1.88 (1.39–2.52) |
1.84 (1.33–2.53) |
|
Low temperature |
|
|
|
|
|
None |
|
|
|
|
|
Moderate |
1.74 (1.51–2.01) |
1.74 (1.50–2.02) |
1.51 (1.14–1.97) |
1.39 (1.04–1.84) |
|
Severe |
1.94 (1.58–2.37) |
2.03 (1.64–2.49) |
1.98 (1.42–2.72) |
1.97 (1.40–2.73) |
In male subjects, the AORs of anxiety for moderate and severe vibration exposure were 1.33 (95% CI: 1.12–1.57) and 1.76 (95% CI: 1.43–2.15), respectively. The discrete AORs of anxiety for moderate and severe noise exposure were 1.47 (95% CI: 1.25–1.72) and 2.12 (95% CI: 1.69–2.63). The AORs of anxiety for moderate and severe high temperature exposure were 1.76 (95% CI: 1.51–2.04) and 2.15 (95% CI: 1.77–2.60), respectively. The individual AORs of anxiety for moderate and severe low temperature exposure were 1.74 (95% CI: 1.50–2.02) and 2.03 (95% CI: 1.64–2.49).
In female subjects, the AORs of anxiety for vibration exposure were not statistically significant at any level of exposure. The specific AORs of anxiety for moderate and severe noise exposure were 1.61 (95% CI: 1.19–2.13) and 1.79 (95% CI: 1.11–2.76). The AORs of anxiety for moderate and severe high temperature exposure were 1.66 (95% CI: 1.27–2.17) and 1.84 (95% CI: 1.33–2.53), respectively. The individual AORs of anxiety for moderate and severe low temperature exposure were 1.39 (95% CI: 1.04–1.84) and 1.97 (95% CI: 1.40–2.73).
In subgroup analyses, the effects of simultaneous exposure of vibration and noise on depression and anxiety were evaluated (
Supplementary Tables 1 and
2). For female workers, AORs of depression and anxiety for single exposure were higher than AORs for simultaneous exposure. For male workers, AOR of anxiety for simultaneous exposure was higher than AOR for single exposure, whereas AORs of depression for simultaneous and single exposure were similar.
DISCUSSION
This study investigated the association between physical hazardous agent exposures and mental health, using the data from the 5th KWCS. Among study populations, female subjects had a higher prevalence of depressive and anxious symptoms. The prevalence of depression and anxiety was higher in the longer working duration group than in the shorter working duration, whereas adjustment of working duration did not change the association between physical hazardous agents and mental health problems. The AORs of depression were significantly increased in male subjects who work with vibration and noise, whereas the AORs between vibration and noise exposures and depression were not significant in female subjects. In male subjects, the AORs of anxiety were significantly increased with exposure to vibration and noise, and the AOR between vibration exposure and anxiety was not significant in female subjects. High or low temperature exposure showed a significant association with depression and anxiety in both male and female subjects. The result of subgroup analyses to assess the effect of simultaneous exposure of vibration and noise on mental health were inconsistent. Thus, there is no clear evidence of synergistic effect of co-exposure to noise and vibration.
A previous study conducted by Joh et al., which examined the relationship between physical and chemical harmful factors and mental health using 1st KWCS data,
11 differs in research design from this study, but the results are worth comparing. In their study, AORs of total mental health problems (depression, anxiety, and insomnia) for whole-body oscillation, noise, and high temperature were 1.43 (95% CI: 1.15–1.78), 1.22 (95% CI: 1.01–1.53), and 1.29 (95% CI: 1.06–1.57), respectively. On the other hand, hand oscillation and low temperature exposure did not show a significant association with mental health problems. In comparison with the previous study, the association between physical hazards and mental health was more evident in this study. One of the explanations for these changes over time is that workers' awareness of mental health problems has increased compared to the past. In addition, the research design of this study that evaluated depression and anxiety separately, may have made a difference in the results of the 2 studies.
Biological and psychosocial factors simultaneously play a role in the development of depression and anxiety.
16,17 Hypothalamic-pituitary-adrenal (HPA) axis activation and cortisol level elevation were considered as the main hormonal changes in depression or anxiety.
18,19 Furthermore, the associations between oxidative stress and depression and anxiety were reported.
20,21 Stressful events are likely to precipitate mental disorders through alteration of neurotransmitter and signal transduction pathways caused by stress-related biological changes.
16,17 One study from the United States suggested that marital status (divorced or unmarried), employment status (unemployed, unable to work), smoking, heavy drinking, obesity, physical inactivity, and chronic disease (cardiovascular disease, diabetes, and asthma) were contributing factors that were significantly associated with either current depressive symptoms or a lifetime diagnosis of depression and anxiety.
22 Studies on work-related mental illness proposed that various psychosocial factors such as effort-reward imbalance,
7,8 high job demands,
7,8,9 and emotional labor with high psychological demands
8,9 are important risk factors of mental disorder in the workplace.
Stratification analysis according to sex was performed in consideration of gender differences in mental health
23,24 and occupation.
15,25 Although the prevalence of depression and anxiety was higher in females, the estimated AORs of depression and anxiety in male participants were greater than female participants that were exposed to physical hazardous agents except for depression of low temperature-exposed workers. In male subjects, the severe physical hazard exposure group showed higher AORs of depression than the moderate exposure group, but in female subjects, the dose-response relationship between exposure and depression was not observed. The AORs of anxiety for the severe physical hazard exposure group were higher than the AORs for the moderate exposure group in both male and female subjects. However, the vibration exposure of female workers was not significant. Sex differences in mental health effects of physical hazards were observed in this study. One possible explanation is that the male workers are more likely to be in high-risk occupations which may lead to exposure to greater physical risks than female workers, even though both male and female workers reported physical hazard exposure.
25 The other possibility is that the female workers are more likely to experience workplace violence
26,27 or emotional labor
28 and complain of mental symptoms that are independent from the physical risk factors.
The link between physical hazard exposure and mental health problems has not been well defined. Although studies on the effects of occupational noise exposure on mental health are limited, the studies on environmental noise exposure reported the association between noise and depression or anxiety.
29 Yoon et al.
30 investigated the association between workplace noise annoyance and depression and suicidal ideation from the 4th Korean National Health and Nutrition Examination Survey. A systematic review on the effect of environmental noise exposure suggests that aircraft, road traffic and railway noise have a negative effect on mental health, well-being, quality of life (QOL) and cognitive function.
31 Previous studies reported the relationship between occupational noise and elevated salivary cortisol level.
32,33 These results suggest that noise exposure may affect HPA axis activation which is associated with the development of depression and anxiety.
18,19
Results of prior studies on mental health effects of vibration exposure are consistent with the current work. A case-control study reported that mechanical trolley drivers who were exposed to whole body vibration showed higher scores for fatigue, depression, and anxiety in neurobehavioral tests.
34 A study on metalworkers who reported vibration-induced white fingers, numbness, tingling, or carpal tunnel syndrome-related symptoms showed an inverse relationship between hand-arm vibration exposure and QOL.
35
Studies that examined how temperature changes affect mental health have not been well established. Although the effect of high temperature exposure on mental health was not statistically significant, the investigation from the 5th EWCS reported an association between poor mental health and temperature change.
10 Studies utilizing weather information, meanwhile, reported that high temperatures worsen mental health difficulties.
36,37 Exposure to low temperatures affected both positive and negative mental well-being.
38 In the case of low temperature exposure in the workplace, a negative mental well-being pathway is plausible as proper temperature control would not be provided.
The health effects such as noise-induced hearing loss (NIHL), hand-arm vibration syndrome (HAVS), hypothermia and hyperthermia from the exposure to physical risk factors may affect mental health. Noise-induced hearing loss and its accompanied tinnitus are associated with depression, anxiety, and adverse effects on QOL.
29 Hand-arm vibration syndrome is associated with poor QOL
39 and other psychological impacts such as frustration, loss of independence and withdrawal from social activities.
40
From a different perspective, workers who reported physical hazardous agent exposure are more likely to be under worse working conditions causing work-related stress and mental health problems when compared to those workers who do not have physical risk factors and poor workplace environments.
11,41 Another study suggested that the self-reported workplace risk perception can be an indicator of work anxiety.
42
Proper management of a workplace mental illness should be accomplished because mental disorders have a substantial portion of global disease burden
3 and cause absenteeism, presenteeism and productivity loss.
4 The need for mental health screening tests has been raised.
43 Furthermore, the concept of an integrated approach to workplace mental health was adopted to prevent and manage mental illness of workers.
44 As the findings in this study suggest, mental health care is essential not only to those workers with psychosocial risk factors but also for those workers with physical hazard exposure.
This study has several limitations of the cross-sectional study using national survey data. First, even though the association between physical hazard exposure and mental health was statistically significant, we could not determine causality or mechanism of mental health problems due to physical hazard exposure. Second, the main variables in this study were assessed by self-reported questionnaire and were only based on subjective data points. We did not use information about psychiatric disorder diagnoses or standardized mental health symptom assessment tools such as Patient Health Questionnaire-9 (PHQ-9)
45 or Generalized Anxiety Disorder questionnaire-7 (GAD-7).
46 Furthermore, workplace hazard evaluation was based on self-reported subjective risk perception rather than an exact measurement of noise, vibration, or temperature. Third, as the KWCS is not longitudinal data, the healthy worker effect must be considered to interpret the result of this study. Individuals unable to work because of severe mental disorders would be excluded and it may cause the healthy worker survivor effect in the current study.
47
Despite its limitations, this study has some strengths. First, this study is based on a large-size study population from the 5th KWCS dataset, which is a representative nationwide large-size study of the Korean working population. Second, sex-specific analysis was conducted to investigate the association among noise, vibration, high and low temperature exposure and depression or anxiety because occupational characteristics and mental health profiles are different from male and female workers.
15 Lastly, only a few studies have tried to assess the relationship between physical hazard exposure and mental health problems and the results of those studies were inconsistent. Our study investigated these controversial relationships between physical hazards and mental health outcomes and improved understanding of this topic.
CONCLUSIONS
In conclusion, noise, vibration, and high and low temperature exposures were associated with high ORs of depression and anxiety in male workers. On the other hand, female subjects showed a less robust relationship between physical risk factor exposure and mental health problems. Further investigations including longitudinal studies are required to reveal the mechanism of physical hazard induced mental health problems and to explain the sex difference of mental health response to the physical hazard exposure.
ACKNOWLEDGEMENTS
The authors would like to thank the Safety and Health Policy Research Department (Occupational Safety and Health Research Institute; OSHRI) for offering raw-data of Korean Working Conditions Survey (KWCS). The paper's contents are solely the responsibility of the author and do not necessarily represent the official view of the OSHRI.
Abbreviations
disability-adjusted life years
European Working Conditions Survey
Generalized Anxiety Disorder questionnaire-7
hand-arm vibration syndrome
hypothalamic-pituitary-adrenal
Korean Working Conditions Survey
noise-induced hearing loss
Patient Health Questionnaire-9
personal protective equipment
NOTES
-
Competing interests: The authors declare that they have no competing interests.
-
Author Contributions:
Conceptualization: Kwon D, Park JT, Kwak K.
Data curation: Kwon D, Chi Y, Na S.
Formal analysis: Kwon D, Kwak K.
Supervision: Park JT.
Writing - original draft: Kwon D, Park JT.
Writing - review & editing: Park JT, Kwak K, Baek K, Chi Y, Na S.
SUPPLEMENTARY MATERIALS
Supplementary Table 1
Effect of simultaneous exposure of vibration and noise on depression
aoem-33-e33-s001.xls
Supplementary Table 2
Effect of simultaneous exposure of vibration and noise on anxiety
aoem-33-e33-s002.xls
REFERENCES
REFERENCES
- 1. Wong K, Chan AHS. Emerging issues in occupational safety and health. Int J Environ Res Public Health 2018;15(12):2897.ArticlePubMedPMC
- 2. Park J, Kim Y. The history of occupational health in South Korea. Arch Environ Occup Health 2019;74(1-2):50–57. 30585530.ArticlePubMed
- 3. Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep 2019;21(2):10. 30729322.ArticlePubMedPDF
- 4. Nicholson PJ. Common mental disorders and work. Br Med Bull 2018;126(1):113–121. 29684103.ArticlePubMed
- 5. Goetzel RZ, Roemer EC, Holingue C, Fallin MD, McCleary K, Eaton W, et al. Mental health in the workplace: a call to action proceedings from the mental health in the workplace-public health summit. J Occup Environ Med 2018;60(4):322–330. 29280775.PubMedPMC
- 6. Harvey SB, Modini M, Joyce S, Milligan-Saville JS, Tan L, Mykletun A, et al. Can work make you mentally ill? A systematic meta-review of work-related risk factors for common mental health problems. Occup Environ Med 2017;74(4):301–310. 28108676.ArticlePubMed
- 7. van der Molen HF, Nieuwenhuijsen K, Frings-Dresen MHW, de Groene G. Work-related psychosocial risk factors for stress-related mental disorders: an updated systematic review and meta-analysis. BMJ Open 2020;10(7):e034849.ArticlePubMedPMC
- 8. Duchaine CS, Aubé K, Gilbert-Ouimet M, Vézina M, Ndjaboué R, Massamba V, et al. Psychosocial stressors at work and the risk of sickness absence due to a diagnosed mental disorder: a systematic review and meta-analysis. JAMA Psychiatry 2020;77(8):842–851. 32236498.ArticlePubMedPMC
- 9. Sohn M, Choi M, Jung M. Working conditions, psychosocial environmental factors, and depressive symptoms among wage workers in South Korea. Int J Occup Environ Health 2016;22(3):209–217. 27373792.ArticlePubMedPMC
- 10. Russo M, Lucifora C, Pucciarelli F, Piccoli B. Work hazards and workers' mental health: an investigation based on the fifth European Working Conditions Survey. Med Lav 2019;110(2):115–129. 30990473.ArticlePubMedPMC
- 11. Joh KO, Park TJ, Oh JI, Paek DM, Park JS, Cho SI. Relationship between workplace physical and chemical hazard exposures and mental health problems in Korea. Korean J Occup Environ Med 2011;23(3):287–297.ArticlePDF
- 12. Nari F, Kim YK, Kang SH, Park EC, Jang SI. Association between occupational noise and vibration exposure and insomnia among workers in Korea. Life (Basel) 2020;10(4):46.ArticlePubMedPMC
- 13. Yiengprugsawan V, Strazdins L, Lim LL, Kelly M, Seubsman SA, Sleigh AC, et al. Physically and psychologically hazardous jobs and mental health in Thailand. Health Promot Int 2015;30(3):531–541. 24218225.ArticlePubMedPMC
- 14. Niedhammer I, Coindre K, Memmi S, Bertrais S, Chastang JF. Working conditions and depression in the French national working population: results from the SUMER study. J Psychiatr Res 2020;123:178–186. 32078835.ArticlePubMed
- 15. Halonen JI, Koskinen A, Varje P, Kouvonen A, Hakanen JJ, Väänänen A. Mental health by gender-specific occupational groups: profiles, risks and dominance of predictors. J Affect Disord 2018;238:311–316. 29902735.ArticlePubMed
- 16. Hammen C. Risk factors for depression: an autobiographical review. Annu Rev Clin Psychol 2018;14(1):1–28. 29328780.ArticlePubMed
- 17. Giacobbe P, Flint A. Diagnosis and management of anxiety disorders. Continuum (Minneap Minn) 2018;24(3, BEHAVIORAL NEUROLOGY AND PSYCHIATRY):893–919. 29851884.ArticlePubMed
- 18. Varghese FP, Brown ES. The hypothalamic-pituitary-adrenal axis in major depressive disorder: a brief primer for primary care physicians. Prim Care Companion J Clin Psychiatry 2001;3(4):151–155. 15014598.PubMedPMC
- 19. Faravelli C, Lo Sauro C, Godini L, Lelli L, Benni L, Pietrini F, et al. Childhood stressful events, HPA axis and anxiety disorders. World J Psychiatry 2012;2(1):13–25. 24175164.ArticlePubMedPMC
- 20. Black CN, Bot M, Scheffer PG, Cuijpers P, Penninx BW. Is depression associated with increased oxidative stress? A systematic review and meta-analysis. Psychoneuroendocrinology 2015;51:164–175. 25462890.ArticlePubMed
- 21. Bouayed J, Rammal H, Soulimani R. Oxidative stress and anxiety: relationship and cellular pathways. Oxid Med Cell Longev 2009;2(2):63–67. 20357926.ArticlePubMedPMCPDF
- 22. Strine TW, Mokdad AH, Balluz LS, Gonzalez O, Crider R, Berry JT, et al. Depression and anxiety in the United States: findings from the 2006 behavioral risk factor surveillance system. Psychiatr Serv 2008;59(12):1383–1390. 19033164.ArticlePubMed
- 23. Altemus M, Sarvaiya N, Neill Epperson C. Sex differences in anxiety and depression clinical perspectives. Front Neuroendocrinol 2014;35(3):320–330. 24887405.ArticlePubMedPMC
- 24. McHenry J, Carrier N, Hull E, Kabbaj M. Sex differences in anxiety and depression: role of testosterone. Front Neuroendocrinol 2014;35(1):42–57. 24076484.ArticlePubMedPMC
- 25. Stergiou-Kita M, Mansfield E, Bezo R, Colantonio A, Garritano E, Lafrance M, et al. Danger zone: men, masculinity and occupational health and safety in high risk occupations. Saf Sci 2015;80:213–220. 27239098.ArticlePubMedPMC
- 26. Lanthier S, Bielecky A, Smith PM. Examining risk of workplace violence in Canada: a sex/gender-based analysis. Ann Work Expo Health 2018;62(8):1012–1020. 30016390.ArticlePubMed
- 27. Zhao S, Xie F, Wang J, Shi Y, Zhang S, Han X, et al. Prevalence of workplace violence against Chinese nurses and its association with mental health: a cross-sectional survey. Arch Psychiatr Nurs 2018;32(2):242–247. 29579519.ArticlePubMed
- 28. Guy ME, Newman MA. Women's jobs, men's jobs: sex segregation and emotional labor. Public Adm Rev 2004;64(3):289–298.Article
- 29. Themann CL, Masterson EA. Occupational noise exposure: a review of its effects, epidemiology, and impact with recommendations for reducing its burden. J Acoust Soc Am 2019;146(5):3879–3905. 31795665.ArticlePubMedPDF
- 30. Yoon JH, Won JU, Lee W, Jung PK, Roh J. Occupational noise annoyance linked to depressive symptoms and suicidal ideation: a result from nationwide survey of Korea. PLoS One 2014;9(8):e105321. 25144292.ArticlePubMedPMC
- 31. Clark C, Crumpler C, Notley AH. Evidence for environmental noise effects on health for the United Kingdom policy context: a systematic review of the effects of environmental noise on mental health, wellbeing, quality of life, cancer, dementia, birth, reproductive outcomes, and cognition. Int J Environ Res Public Health 2020;17(2):393.ArticlePubMedPMC
- 32. Yaghoubi K, Alimohammadi I, Abolghasemi J, Shandiz MS, Aboutaleb N, Ebrahimi H. The relationship between noise annoyance and salivary cortisol. Appl Acoust 2020;160:107131.Article
- 33. Selander J, Bluhm G, Theorell T, Pershagen G, Babisch W, Seiffert I, et al. Saliva cortisol and exposure to aircraft noise in six European countries. Environ Health Perspect 2009;117(11):1713–1717. 20049122.ArticlePubMedPMC
- 34. Abbate C, Micali E, Giorgianni C, Munaò F, Brecciaroli R, Salmaso L, et al. Affective correlates of occupational exposure to whole-body vibration. A case-control study. Psychother Psychosom 2004;73(6):375–379. 15479993.ArticlePubMedPDF
- 35. Sauni R, Virtema P, Pääkkönen R, Toppila E, Pyykkö I, Uitti J. Quality of life (EQ-5D) and hand-arm vibration syndrome. Int Arch Occup Environ Health 2010;83(2):209–216. 19593581.ArticlePubMedPDF
- 36. Mullins JT, White C. Temperature and mental health: evidence from the spectrum of mental health outcomes. J Health Econ 2019;68:102240. 31590065.ArticlePubMed
- 37. Li M, Ferreira S, Smith TA. Temperature and self-reported mental health in the United States. PLoS One 2020;15(3):e0230316. 32210473.ArticlePubMedPMC
- 38. Liddell C, Guiney C. Living in a cold and damp home: frameworks for understanding impacts on mental well-being. Public Health 2015;129(3):191–199. 25726123.ArticlePubMed
- 39. House R, Wills M, Liss G, Switzer-McIntyre S, Lander L, Jiang D. The effect of hand-arm vibration syndrome on quality of life. Occup Med (Lond) 2014;64(2):133–135. 24486514.ArticlePubMed
- 40. Ayers B, Forshaw M. An interpretative phenomenological analysis of the psychological ramifications of hand-arm vibration syndrome. J Health Psychol 2010;15(4):533–542. 20460410.ArticlePubMedPDF
- 41. Colligan TW, Higgins EM. Workplace stress: etiology and consequences. J Workplace Behav Health 2005;21(2):89–97.
- 42. Muschalla B, Fay D, Linden M. Self-reported workplace perception as indicators of work anxieties. Occup Med (Lond) 2016;66(2):168–170. 26511747.PubMed
- 43. Bender A, Kennedy S. Mental health and mental illness in the workplace: diagnostic and treatment issues. Healthc Pap 2004;5(2):54–67. 15829776.ArticlePubMed
- 44. LaMontagne AD, Martin A, Page KM, Reavley NJ, Noblet AJ, Milner AJ, et al. Workplace mental health: developing an integrated intervention approach. BMC Psychiatry 2014;14(1):131. 24884425.ArticlePubMedPMCPDF
- 45. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16(9):606–613. 11556941.ArticlePubMedPMC
- 46. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166(10):1092–1097. 16717171.ArticlePubMed
- 47. Arrighi HM, Hertz-Picciotto I. The evolving concept of the healthy worker survivor effect. Epidemiology 1994;5(2):189–196. 8172994.ArticlePubMed
 , Kyeongmin Kwak1
, Kyeongmin Kwak1 , Kiook Baek1
, Kiook Baek1 , Youngchan Chi1
, Youngchan Chi1 , Sewhan Na1
, Sewhan Na1 , Jong-Tae Park1
, Jong-Tae Park1

 KSOEM
KSOEM

 Cite
Cite

