Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 36; 2024 > Article
- Original Article Association between single-person household wage workers in South Korea and insomnia symptoms: the 6th Korean Working Conditions Survey (KWCS)
-
Yoon Ho Lee
 , Yong-Jin Lee
, Yong-Jin Lee , Eun-Chul Jang
, Eun-Chul Jang , Young-Sun Min
, Young-Sun Min , Soon-Chan Kwon,*
, Soon-Chan Kwon,*
-
Annals of Occupational and Environmental Medicine 2024;36:e25.
DOI: https://doi.org/10.35371/aoem.2024.36.e25
Published online: September 6, 2024
Department of Occupational and Environmental Medicine, Soonchunhyang University Cheonan Hospital, Cheonan, Korea
- *Correspondence: Soon-Chan Kwon Department of Occupational and Environmental Medicine, Soonchunhyang University Cheonan Hospital, 31 Suncheonhyang 6-gil, Dongnam-gu, Cheonan 31151, Korea E-mail: 91ksc@hanmail.net
© 2024 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 6,393 Views
- 285 Download
- 1 Crossref
Abstract
-
Background The rise in single-person households is a global phenomenon with well-documented implications for both physical and mental well-being. However, there remains a scarcity of studies focusing specifically on the health impacts of single-person households on workers. This study aims to address this gap by comparing insomnia symptoms between single- and multi-person household workers, shedding light on the health implications of household composition.
-
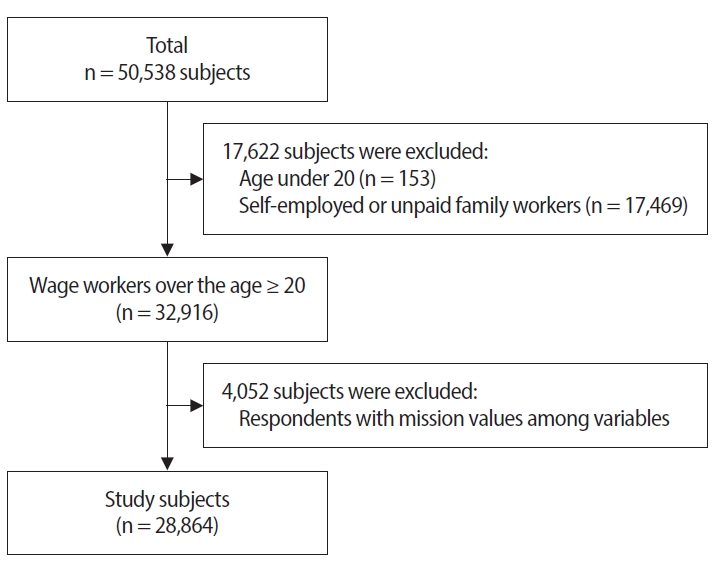
Methods This study utilized data from the Sixth Korean Working Conditions Survey. Insomnia symptoms were categorized into normal sleep and insomnia symptom groups utilizing the 3-item Minimal Insomnia Symptom Scale. Multiple logistic regression analysis was employed to examine the association between single-person household wage workers and insomnia symptoms.
-
Results In comparison to wage workers from multi-person households, those from single-person households exhibited heightened risks of reporting insomnia symptoms. In the fully adjusted model, the odds ratios for symptoms of insomnia among single-person household wage workers was 1.173 (95% confidence interval: 1.020–1.349).
-
Conclusions This study underscores that single-person household wage workers in Korea face an elevated risk of insomnia symptoms compared to their counterparts in multi-person households.
BACKGROUND
METHODS
Single-person household and multi-person household
Insomnia symptoms
Covariates
RESULTS
DISCUSSION
CONCLUSIONS
Abbreviations
CI
COVID-19
KWCS
MISS
OECD
OR
-
Funding
This work was supported by the Soonchunhyang University Research Fund.
-
Competing interests
Young-Sun Min, contributing editor of the Annals of Occupational and Environmental Medicine, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
-
Author contributions
Conceptualization: Lee YH, Kwon SC. Data curation: Lee YH, Lee YJ, Jang EC, Kwon SC, Min YS. Formal analysis: Lee YH, Jang EC, Lee YJ, Kwon SC, Min YS. Investigation: Lee YH, Jang EC, Lee YJ, Kwon SC, Min YS. Writing - original draft: Lee YH. Writing - review & editing: Kwon SC.
-
Acknowledgments
We appreciate the Occupational Safety and Health Research Institute (OSHRI) for offering the data from the 6th Korean working conditions survey. The paper's contents are solely the responsibility of the author and do not necessarily represent the official views of the OSHRI.
NOTES
| Total (n = 33,113) |
No. of household members |
p-value | ||
|---|---|---|---|---|
| ≥2 (n = 29,992) | 1 (n = 29,992) | |||
| Sex | ||||
| Men | 18,818 (56.8) | 17,045 (56.8) | 1,773 (56.8) | 0.980 |
| Women | 14,295 (43.2) | 12,947 (43.2) | 1,348 (43.2) | |
| Age (years) | ||||
| 20–29 | 5,464 (16.5) | 4,722 (15.7) | 742 (23.8) | <0.001 |
| 30–39 | 7,519 (22.7) | 6,836 (22.8) | 683 (21.9) | |
| 40–49 | 8,192 (24.7) | 7,793 (26.0) | 399 (12.8) | |
| 50–59 | 7,265 (21.9) | 6,764 (22.6) | 501 (16.1) | |
| ≥60 | 4,673 (14.1) | 3,877 (12.9) | 796 (25.5) | |
| Education level | ||||
| High school or below | 13,536 (40.9) | 11,883 (39.6) | 1,653 (53.0) | <0.001 |
| University or above | 19,577 (59.1) | 18,109 (60.4) | 1,468 (47.0) | |
| Household monthly income (KRW) | ||||
| <2,000,000 | 9,193 (27.8) | 8,062 (26.9) | 1,131 (36.2) | <0.001 |
| 2,000,000–3,000,000 | 10,775 (32.5) | 9,619 (32.1) | 1,156 (37.0) | |
| 3,000,000–4,000,000 | 7,246 (21.9) | 6,667 (22.2) | 579 (18.5) | |
| ≥4,000,000 | 5,900 (17.8) | 5,644 (18.8) | 256 (8.2) | |
| Weekly working time (hours) | ||||
| ≤40 | 23,719 (71.6) | 21,504 (71.7) | 2,215 (70.9) | 0.015 |
| 41–52 | 7,208 (21.8) | 6,545 (21.8) | 663 (21.2) | |
| ≥53 | 2,186 (6.6) | 1,942 (6.5) | 244 (7.8) | |
| Job classification | ||||
| White | 8,337 (25.2) | 7,683 (25.6) | 654 (20.9) | <0.001 |
| Pink | 13,013 (39.3) | 12,011 (40.0) | 1,002 (32.1) | |
| Green | 76 (0.2) | 63 (0.2) | 13 (0.4) | |
| Blue | 11,688 (35.3) | 10,235 (34.1) | 1,453 (46.5) | |
| No. of employees | ||||
| <50 | 21,093 (63.7) | 18,847 (62.8) | 2,246 (72.0) | <0.001 |
| 50–299 | 6,262 (18.9) | 5,773 (19.2) | 489 (15.7) | |
| ≥300 | 5,758 (17.4) | 5,372 (17.9) | 386 (12.4) | |
| Type of employment | ||||
| Regular | 26,581 (80.3) | 24,472 (81.6) | 2,109 (67.6) | <0.001 |
| Temporary | 4,732 (14.3) | 4,027 (13.4) | 705 (22.6) | |
| Day laborers | 1,800 (5.4) | 1,493 (5.0) | 307 (9.8) | |
| Shift work | ||||
| No | 29,762 (89.9) | 26,913 (89.7) | 2,849 (91.3) | 0.006 |
| Yes | 3,351 (10.1) | 3,079 (10.3) | 272 (8.7) | |
| Job stress | ||||
| Low | 7,497 (22.6) | 6,641 (22.1) | 856 (27.4) | <0.001 |
| High | 25,617 (77.4) | 23,351 (77.9) | 2,266 (72.6) | |
| Presenteeism | ||||
| No | 29,400 (88.8) | 26,591 (88.7) | 2,809 (90.0) | 0.027 |
| Yes | 3,714 (11.2) | 3,401 (11.3) | 313 (10.0) | |
| Self-rated health statusa | ||||
| Good | 27,418 (96.9) | 24,987 (97.0) | 2,431 (95.7) | <0.001 |
| Poor | 882 (3.1) | 773 (3.0) | 109 (4.3) | |
| Insomnia symptomsb | ||||
| No | 30,468 (92.0) | 27,640 (92.2) | 2,828 (90.6) | 0.002 |
| Yes | 2,645 (8.0) | 2352 (7.8) | 293 (9.4) | |
Values are presented as number (%).
aExcellent, good, fair were classified as having good self-rated health and poor, very poor were classified as having poor self-rated health;
bSubjects with Minimal Insomnia Symptom Scale (MISS) scores of 6 or higher were categorized into a group having symptoms of insomnia.
| Age (years) | Total (n = 33,113) |
Insomnia symptomsa |
p-value | p for trend | |
|---|---|---|---|---|---|
| No (n = 30,468) | Yes (n = 2,645) | ||||
| 20–29 | 5,463 (100) | 5,174 (94.7) | 289 (5.3) | <0.001 | <0.001 |
| 30–39 | 7,519 (100) | 6,975 (92.8) | 544 (7.2) | ||
| 40–49 | 8,192 (100) | 7,563 (92.3) | 629 (7.7) | ||
| 50–59 | 7,265 (100) | 6,626 (91.2) | 639 (8.8) | ||
| ≥60 | 4,674 (100) | 4,130 (88.4) | 544 (11.6) | ||
| No. of household members | Total (n = 33,113) |
Insomnia symptomsa |
p-value | p for trend | |
|---|---|---|---|---|---|
| No (n = 30,468) | Yes (n = 2,645) | ||||
| 1 | 3,121 (100) | 2,828 (90.6) | 293 (9.4) | <0.001 | <0.001 |
| 2 | 6,739 (100) | 6,156 (91.3) | 583 (8.7) | ||
| 3 | 9,068 (100) | 8,362 (92.2) | 706 (7.8) | ||
| ≥4 | 14,186 (100) | 13,123 (92.5) | 1,063 (7.5) | ||
| Insomnia symptomsa |
OR (95% CI) |
|||
|---|---|---|---|---|
| Crude | Model 1 | Model 2 | Model 3 | |
| No | Ref. | Ref. | Ref. | Ref. |
| Yes | 1.219 (1.073–1.385)** | 1.194 (1.048–1.361)** | 1.209 (1.056–1.385)** | 1.173 (1.020–1.349)* |
Crude: unadjusted; Model 1: adjusted for adjusted for sex, age, education level, household monthly income, weekly working time, shift work; Model 2: adjusted for adjusted for sex, age, education level, household monthly income, weekly working time, shift work, job classification, number of employees, type of employment, job stress, presenteeism; Model 3: adjusted for adjusted for sex, age, education level, household monthly income, weekly working time, shift work, job classification, number of employees, type of employment, job stress, presenteeism, self-rated health.
OR: odds ratio; CI: confidence interval.
*p < 0.05,
**p < 0.01.
aSubjects with Minimal Insomnia Symptom Scale (MISS) scores of 6 or higher were categorized into a group having symptoms of insomnia.
- 1. Lee HY, Noh SC, Choi EY. Growth pattern and spatial distribution of one-person households by socio-economic demographic characteristics. J Korean Geogr Soc 2011;46(4):480–500.
- 2. Eurofound. Household Composition and Well-being. Luxembourg: Publications Office of the European Union; 2019.
- 3. Organisation for Economic Co-operation and Development (OECD). OECD Family Database. Paris, France: OECD Publishing; 2013.
- 4. Statistics Korea. 2022 Population and Housing Census. Daejeon, Korea: Statistics Korea; 2022.
- 5. Statistics Korea. Household Projections 2020. Daejeon, Korea: Statistics Korea; 2020.
- 6. Berkman LF. Social support, social networks, social cohesion and health. Soc Work Health Care 2000;31(2):3–14.ArticlePubMed
- 7. Kang E, Lee M. Single-person households in south Korea and their policy implication. Health Welf Policy Forum 2016;4(234):47–56.
- 8. Shin MA. Comparative study on health behavior and mental health between one person and multi-person households: analysis of data from the National Health and Nutrition Examination Surveys (2013, 2015, 2017). J Korean Soc Wellness 2019;14(4):11–23.Article
- 9. HIRA Healthcare Bigdata Hub. Disease statistics of national interest. https://opendata.hira.or.kr/op/opc/olapMfrnIntrsIlnsInfoTab1.do. Updated 2023. Accessed December 15, 2023
- 10. Grandner MA, Patel NP, Gehrman PR, Perlis ML, Pack AI. Problems associated with short sleep: bridging the gap between laboratory and epidemiological studies. Sleep Med Rev 2010;14(4):239–47.ArticlePubMed
- 11. Wingard DL, Berkman LF. Mortality risk associated with sleeping patterns among adults. Sleep 1983;6(2):102–7.ArticlePubMed
- 12. Fietze I, Rosenblum L, Salanitro M, Ibatov AD, Eliseeva MV, Penzel T, et al. The interplay between poor sleep and work-related health. Front Public Health 2022;10:866750.ArticlePubMedPMC
- 13. Fidler AL, Chaudhari P, Sims V, Payne-Murphy J, Fischer J, Cottler LB. Insomnia among community members in Florida: associations with demographics, health conditions, and social support. J Clin Transl Sci 2023;7(1):e128.ArticlePubMedPMC
- 14. Lee MS, Song H, Kim B. Association between physical health status, health behaviors and subjective depression among single-person household. Korean J Health Educ Promot 2018;35(2):61–71.Article
- 15. Han SI, Huh Y, Sunwoo S. Comparison of health related quality of life of one- and multi-person households using EQ-5D based on the 7th Korea National Health and Nutrition Examination Survey. Korean J Fam Pract 2022;12(1):22–7.Article
- 16. Park M, Kim SA. Characteristics and types of loneliness, social isolation, and mental health problems in single-person households: focusing on single-person households in Seoul. Health Soc Welf Rev 2022;42(4):127–41.
- 17. Kim HY, Choi J, Lim HM, Park C, Hong YC. The association between non-regular work patterns and insomnia among Korean wage workers: the fifth Korean working condition survey. Ann Occup Environ Med 2021;33:e9.ArticlePubMedPMCPDF
- 18. Kim SW, Bae KH, Seo JB, Jeon JH, Lee WK, Lee IK, et al. Association between household size, residential area, and osteoporosis: analysis of 2008 to 2011 Korea National Health and Nutrition Examination Survey. Korean J Intern Med 2016;31(4):712–21.ArticlePubMedPMCPDF
- 19. Broman JE, Smedje H, Mallon L, Hetta J. The Minimal Insomnia Symptom Scale (MISS): a brief measure of sleeping difficulties. Ups J Med Sci 2008;113(2):131–42.PubMed
- 20. Grandner MA. Sleep and Health. Oxford, UK: Academic Press; 2019.
- 21. de Souza Lopes C, Robaina JR, Rotenberg L. Epidemiology of insomnia: prevalence and risk factors. In: Sahoo S, editor. Can't Sleep? Issues of Being an Insomniac. London, UK: InTech; 2012.
- 22. Morin CM, Jarrin DC. Epidemiology of insomnia: prevalence, course, risk factors, and public health burden. Sleep Med Clin 2022;17(2):173–91.PubMed
- 23. Utsugi M, Saijo Y, Yoshioka E, Horikawa N, Sato T, Gong Y, et al. Relationships of occupational stress to insomnia and short sleep in Japanese workers. Sleep 2005;28(6):728–35.ArticlePubMed
- 24. Hwang J, Cho SS, Kim JI. Association between insomnia and absenteeism or presenteeism among Korean employees. Ann Occup Environ Med 2022;34:e41.ArticlePubMedPMCPDF
- 25. Coombe AH, Epps F, Lee J, Chen ML, Imes CC, Chasens ER. Sleep and self-rated health in an aging workforce. Workplace Health Saf 2019;67(6):302–10.ArticlePubMedPDF
- 26. Simoes Maria M, Bula C, Santos-Eggimann B, Krief H, Heinzer R, Seematter-Bagnoud L. Sleep characteristics and self-rated health in older persons. Eur Geriatr Med 2020;11(1):131–8.ArticlePubMedPDF
- 27. Stefan L, Juranko D, Prosoli R, Baric R, Sporis G. Self-reported sleep duration and self-rated health in young adults. J Clin Sleep Med 2017;13(7):899–904.ArticlePubMedPMC
- 28. Segovia J, Bartlett RF, Edwards AC. The association between self-assessed health status and individual health practices. Can J Public Health 1989;80(1):32–7.PubMed
- 29. Jylha M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med 2009;69(3):307–16.ArticlePubMed
- 30. Jylha M, Volpato S, Guralnik JM. Self-rated health showed a graded association with frequently used biomarkers in a large population sample. J Clin Epidemiol 2006;59(5):465–71.ArticlePubMed
- 31. Pien LC, Chen IS, Cheng WJ, Cheng Y. Work-to-family conflict and its associations with workers' burnout, poor self-rated health, and minor mental disorder: a survey of general employees in Taiwan. J Occup Environ Med 2020;62(8):588–94.PubMed
- 32. Park MY, Park J, Myong JP, Kim HR, Lee DW, Kang MY. Poor worker's long working hours paradox: evidence from the Korea National Health and Nutrition Examination Survey, 2013-2018. Ann Occup Environ Med 2022;34:e2.ArticlePubMedPMCPDF
- 33. Han E, Kim UJ, Lee Y, Lee S, Ham S, Lee W, et al. Association between lone work and self-rated health status: using the 5th Korean Working Conditions Survey. Ann Occup Environ Med 2023;35:e29.ArticlePubMedPMCPDF
- 34. Cho YK, Shim KW, Suk HW, Lee HS, Lee SW, Byun AR, et al. Differences between one-person and multi-person households on socioeconomic status, health behavior, and metabolic syndrome across gender and age groups. Korean J Fam Pract 2019;9(4):373–82.Article
- 35. Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev 2002;6(2):97–111.ArticlePubMed
- 36. Unruh ML, Redline S, An MW, Buysse DJ, Nieto FJ, Yeh JL, et al. Subjective and objective sleep quality and aging in the sleep heart health study. J Am Geriatr Soc 2008;56(7):1218–27.ArticlePubMed
- 37. Jeon JY, Kim KT, Lee SY, Cho YW; Sleep Epidemiology Committee of the Korean Sleep Research Society. Insomnia during coronavirus disease 2019 pandemic in Korea: a National sleep survey. Sleep Biol Rhythms 2023;21(4):431–8.ArticlePubMedPMCPDF
- 38. Lee J, Hong Y, Lee W. Prevalence of insomnia in various industries and associated demographic factors in night-shift workers using workers' specific health examination data. Int J Environ Res Public Health 2021;18(13):6902.ArticlePubMedPMC
- 39. Seo K, Ryu S, Jeong S, Kang HT, Kim SK, Koh SB, et al. Risk of insomnia symptoms according to work-family conflict by workers' characteristics. Ann Occup Environ Med 2023;35:e36.ArticlePubMedPMCPDF
- 40. Roth T. Prevalence, associated risks, and treatment patterns of insomnia. J Clin Psychiatry 2005;66 Suppl 9:10–3.PubMed
- 41. Leger D, Massuel MA, Metlaine A, Group SS. Professional correlates of insomnia. Sleep 2006;29(2):171–8.PubMed
- 42. Pinquart M, Sorensen S. Risk factors for loneliness in adulthood and old age: a meta-analysis. In: Shohov SP, editor. Advances in Psychology Research. Vol. 19. Hauppauge, NY: Nova Science Publishers; 2003, 111–43.
- 43. Stickley A, Koyanagi A, Leinsalu M, Ferlander S, Sabawoon W, McKee M. Loneliness and health in Eastern Europe: findings from Moscow, Russia. Public Health 2015;129(4):403–10.ArticlePubMed
- 44. Yildirim Y, Kocabiyik S. The relationship between social support and loneliness in Turkish patients with cancer. J Clin Nurs 2010;19(5-6):832–9.ArticlePubMed
- 45. Noh HJ. Social relationships of young single-person households. Health Soc Welf Rev 2018;38(2):71–102.Article
- 46. Hawkley LC, Buecker S, Kaiser T, Luhmann M. Loneliness from young adulthood to old age: explaining age differences in loneliness. Int J Behav Dev 2022;46(1):39–49.ArticlePubMedPDF
- 47. Jessen MA, Pallesen AV, Kriegbaum M, Kristiansen M. The association between loneliness and health: a survey-based study among middle-aged and older adults in Denmark. Aging Ment Health 2018;22(10):1338–43.ArticlePubMed
- 48. Griffin SC, Williams AB, Ravyts SG, Mladen SN, Rybarczyk BD. Loneliness and sleep: A systematic review and meta-analysis. Health Psychol Open 2020;7(1):2055102920913235.ArticlePubMedPMCPDF
- 49. Bu F, Steptoe A, Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health 2020;186:31–4.ArticlePubMed
- 50. Shor E, Roelfs DJ, Yogev T. The strength of family ties: a meta-analysis and meta-regression of self-reported social support and mortality. Soc Netw 2013;35(4):626–38.Article
REFERENCES
Figure & Data
REFERENCES
Citations

- Influencing Factors of Quality of Life Among Korean Women in One-Person and Multiperson Households: Analysis of the 8th Korean National Health and Nutrition Examination Survey
Mi-Rae An, Seul-Gi Jeong, Ju-Hee Nho
Journal of Korean Maternal and Child Health.2025; 29(4): 228. CrossRef
- Figure
- Related articles
-
- Association between sudden work recall and psychological health issues: a cross-sectional analysis of the 6th Korean Working Conditions Survey
- Health effects of weekend work on Korean workers: based on the 6th Korean Working Conditions Survey
- Association between multiple jobs and physical and psychological symptoms among the Korean working population
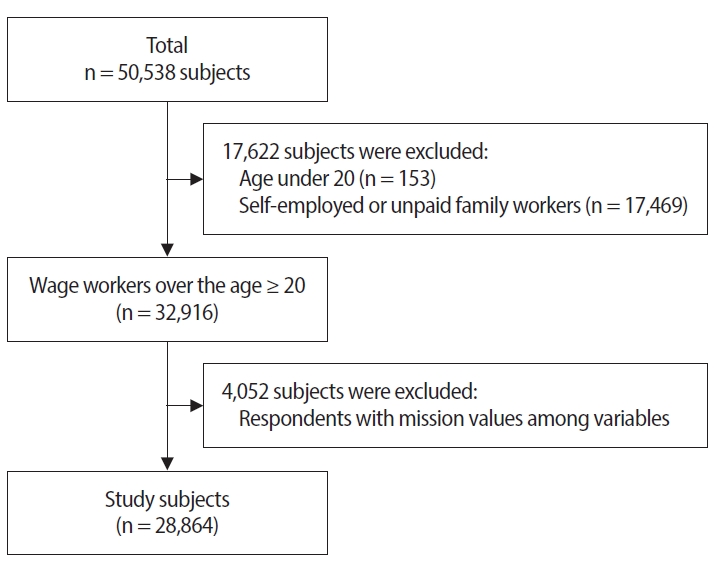
Fig. 1.
| Total (n = 33,113) | No. of household members |
p-value | ||
|---|---|---|---|---|
| ≥2 (n = 29,992) | 1 (n = 29,992) | |||
| Sex | ||||
| Men | 18,818 (56.8) | 17,045 (56.8) | 1,773 (56.8) | 0.980 |
| Women | 14,295 (43.2) | 12,947 (43.2) | 1,348 (43.2) | |
| Age (years) | ||||
| 20–29 | 5,464 (16.5) | 4,722 (15.7) | 742 (23.8) | <0.001 |
| 30–39 | 7,519 (22.7) | 6,836 (22.8) | 683 (21.9) | |
| 40–49 | 8,192 (24.7) | 7,793 (26.0) | 399 (12.8) | |
| 50–59 | 7,265 (21.9) | 6,764 (22.6) | 501 (16.1) | |
| ≥60 | 4,673 (14.1) | 3,877 (12.9) | 796 (25.5) | |
| Education level | ||||
| High school or below | 13,536 (40.9) | 11,883 (39.6) | 1,653 (53.0) | <0.001 |
| University or above | 19,577 (59.1) | 18,109 (60.4) | 1,468 (47.0) | |
| Household monthly income (KRW) | ||||
| <2,000,000 | 9,193 (27.8) | 8,062 (26.9) | 1,131 (36.2) | <0.001 |
| 2,000,000–3,000,000 | 10,775 (32.5) | 9,619 (32.1) | 1,156 (37.0) | |
| 3,000,000–4,000,000 | 7,246 (21.9) | 6,667 (22.2) | 579 (18.5) | |
| ≥4,000,000 | 5,900 (17.8) | 5,644 (18.8) | 256 (8.2) | |
| Weekly working time (hours) | ||||
| ≤40 | 23,719 (71.6) | 21,504 (71.7) | 2,215 (70.9) | 0.015 |
| 41–52 | 7,208 (21.8) | 6,545 (21.8) | 663 (21.2) | |
| ≥53 | 2,186 (6.6) | 1,942 (6.5) | 244 (7.8) | |
| Job classification | ||||
| White | 8,337 (25.2) | 7,683 (25.6) | 654 (20.9) | <0.001 |
| Pink | 13,013 (39.3) | 12,011 (40.0) | 1,002 (32.1) | |
| Green | 76 (0.2) | 63 (0.2) | 13 (0.4) | |
| Blue | 11,688 (35.3) | 10,235 (34.1) | 1,453 (46.5) | |
| No. of employees | ||||
| <50 | 21,093 (63.7) | 18,847 (62.8) | 2,246 (72.0) | <0.001 |
| 50–299 | 6,262 (18.9) | 5,773 (19.2) | 489 (15.7) | |
| ≥300 | 5,758 (17.4) | 5,372 (17.9) | 386 (12.4) | |
| Type of employment | ||||
| Regular | 26,581 (80.3) | 24,472 (81.6) | 2,109 (67.6) | <0.001 |
| Temporary | 4,732 (14.3) | 4,027 (13.4) | 705 (22.6) | |
| Day laborers | 1,800 (5.4) | 1,493 (5.0) | 307 (9.8) | |
| Shift work | ||||
| No | 29,762 (89.9) | 26,913 (89.7) | 2,849 (91.3) | 0.006 |
| Yes | 3,351 (10.1) | 3,079 (10.3) | 272 (8.7) | |
| Job stress | ||||
| Low | 7,497 (22.6) | 6,641 (22.1) | 856 (27.4) | <0.001 |
| High | 25,617 (77.4) | 23,351 (77.9) | 2,266 (72.6) | |
| Presenteeism | ||||
| No | 29,400 (88.8) | 26,591 (88.7) | 2,809 (90.0) | 0.027 |
| Yes | 3,714 (11.2) | 3,401 (11.3) | 313 (10.0) | |
| Self-rated health status |
||||
| Good | 27,418 (96.9) | 24,987 (97.0) | 2,431 (95.7) | <0.001 |
| Poor | 882 (3.1) | 773 (3.0) | 109 (4.3) | |
| Insomnia symptoms |
||||
| No | 30,468 (92.0) | 27,640 (92.2) | 2,828 (90.6) | 0.002 |
| Yes | 2,645 (8.0) | 2352 (7.8) | 293 (9.4) | |
| Age (years) | Total (n = 33,113) | Insomnia symptoms |
p-value | p for trend | |
|---|---|---|---|---|---|
| No (n = 30,468) | Yes (n = 2,645) | ||||
| 20–29 | 5,463 (100) | 5,174 (94.7) | 289 (5.3) | <0.001 | <0.001 |
| 30–39 | 7,519 (100) | 6,975 (92.8) | 544 (7.2) | ||
| 40–49 | 8,192 (100) | 7,563 (92.3) | 629 (7.7) | ||
| 50–59 | 7,265 (100) | 6,626 (91.2) | 639 (8.8) | ||
| ≥60 | 4,674 (100) | 4,130 (88.4) | 544 (11.6) | ||
| No. of household members | Total (n = 33,113) | Insomnia symptoms |
p-value | p for trend | |
|---|---|---|---|---|---|
| No (n = 30,468) | Yes (n = 2,645) | ||||
| 1 | 3,121 (100) | 2,828 (90.6) | 293 (9.4) | <0.001 | <0.001 |
| 2 | 6,739 (100) | 6,156 (91.3) | 583 (8.7) | ||
| 3 | 9,068 (100) | 8,362 (92.2) | 706 (7.8) | ||
| ≥4 | 14,186 (100) | 13,123 (92.5) | 1,063 (7.5) | ||
| Insomnia symptoms |
OR (95% CI) |
|||
|---|---|---|---|---|
| Crude | Model 1 | Model 2 | Model 3 | |
| No | Ref. | Ref. | Ref. | Ref. |
| Yes | 1.219 (1.073–1.385) |
1.194 (1.048–1.361) |
1.209 (1.056–1.385) |
1.173 (1.020–1.349) |
Values are presented as number (%). Excellent, good, fair were classified as having good self-rated health and poor, very poor were classified as having poor self-rated health; Subjects with Minimal Insomnia Symptom Scale (MISS) scores of 6 or higher were categorized into a group having symptoms of insomnia.
Values are presented as number (%). Subjects with Minimal Insomnia Symptom Scale (MISS) scores of 6 or higher were categorized into a group having symptoms of insomnia.
Values are presented as number (%). Subjects with Minimal Insomnia Symptom Scale (MISS) scores of 6 or higher were categorized into a group having symptoms of insomnia.
Crude: unadjusted; Model 1: adjusted for adjusted for sex, age, education level, household monthly income, weekly working time, shift work; Model 2: adjusted for adjusted for sex, age, education level, household monthly income, weekly working time, shift work, job classification, number of employees, type of employment, job stress, presenteeism; Model 3: adjusted for adjusted for sex, age, education level, household monthly income, weekly working time, shift work, job classification, number of employees, type of employment, job stress, presenteeism, self-rated health. OR: odds ratio; CI: confidence interval. Subjects with Minimal Insomnia Symptom Scale (MISS) scores of 6 or higher were categorized into a group having symptoms of insomnia.
 KSOEM
KSOEM

 Cite
Cite

