Abstract
-
Background
The prevalence of multiple job-holding (MJH) is expected to show an upward trend among Korean workers, yet its potential impact on workers’ health remains poorly discussed. This study aimed to explore the association between MJH and experience of physical and psychological symptoms in various aspects among active Korean workers and to identify its differences depending on workers’ gender.
-
Methods
We conducted a population-based cross-sectional study among South Korean workers aged 15–59 using data from the 6th Korean Working Conditions Survey. The final study sample comprised 34,175 participants. MJH status and symptoms, such as musculoskeletal pain, headache or eyestrain, fatigue, insomnia, and anxiety, were measured by self-reported data. Logistic regression analyses were performed on the total sample and gender-stratified groups, with adjustments for the sociodemographic and occupational characteristics of the participants.
-
Results
One hundred thirty-five men and 103 women were defined as multiple job-holders (MJHers) among the study sample. When adjusted for sociodemographic and occupational characteristics, MJHers suffered more events of headache or eyestrain (odds ratio [OR]: 1.85, 95% confidence interval [CI]: 1.23–2.78) and anxiety (OR: 1.99, 95% CI: 1.05–3.79). Gender-stratified analyses with adjustment showed that among women workers, MJH was associated with musculoskeletal pain (OR: 1.85, 95% CI: 1.02–3.34), headache or eyestrain (OR: 2.53, 95% CI: 1.37–4.67), fatigue (OR: 2.38, 95% CI: 1.29–4.40), insomnia (OR: 1.92, 95% CI: 1.04–3.57), and anxiety (OR: 2.83, 95% CI: 1.11–7.20).
-
Conclusions
We found a significant association between MJH and various symptoms. Women MJHers were revealed to be a more vulnerable population than their men counterparts. Further research should account for the social context of MJH, and appropriate monitoring and intervention for maintaining the well-being of MJHers are needed.
-
Keywords: Adult; Cross-sectional studies; Employment; Health status; Republic of Korea
BACKGROUND
The phenomenon of people working more than a single job at a time has recently gained increasing public attention, and in turn, scholarly regard, challenging the historical perspective of employment as a person working a single job.
1 Researchers state such phenomenon as ‘multiple job-holding’ (MJH) and, albeit with range to some degree, define the term as “the act or the status of working more than one job simultaneously, wherein tasks are performed in exchange for compensation.”
1 Technological advances, globalization, and economic crises have driven a considerable number of workers worldwide to seek ‘unconventional’ opportunities for work.
2 Various incentives are thought to draw workers to MJH, such as extra income, entrepreneurial advancements, or psychological fulfillment.
1,3 In 2022, approximately 5% and 4% of workers in the United States and European nations, respectively, reported working more than one job in the same week.
4,5 Although trends in the prevalence of MJH are reported to vary by country,
6 MJH is expected to become more frequent, as short-term labor contracts, freelancing, and various part-time platform work grow in prevalence.
7
Although the health effects of MJH have been explored across various dimensions, the results have been conflicting. Some studies concluded that MJH may be beneficial to workers’ health, with one study reporting that multiple job-holders (MJHers) enjoyed higher overall job satisfaction, and suffered less stress than their single job-holding (SJH) counterparts.
8 On the other hand, a comparably larger number of studies warned that MJH may cause deterioration of workers’ health. Researchers have found that MJHers are at greater risk of having work or non-work injuries than single job-holders (SJHers).
9,10,11 MJHers also spend less time sleeping and resting, possibly leading to fatigue and a poor sense of subjective well-being.
12 At the same time, MJH has also been shown to be related to depressive moods,
13 and elevated psychological stress, coupled with work-family conflict.
14 While some studies reported no significant association between MJH and worker health,
15,16 they did not dismiss the possibility of MJH serving as a detrimental factor for health and safety, suggesting the need for further research.
Contrary to the worldwide attention MJH has gained as a potential novel risk to workers’ health, Korean society seems to have overlooked this aspect. This is unsurprising given that workers holding 2 or more jobs are relatively scarce in Korea, reported as a mere 1% of the total working population.
17 This can largely be attributed to the conventional values that consider having a lifelong career as a social norm, and engaging in sidelines as an undesirable option.
18 Nevertheless, Koreans are now becoming more open towards MJH; the media are increasingly focusing on the life of MJHers and their drive towards engaging in work other than their main jobs.
19 In a qualitative study on Korean MJHers, participants narrated that they were attracted to flexible work schedule and chances to experience new opportunities by juggling multiple jobs, suggesting that MJH by itself could be the appealing alternative form of labor, rather than a transitory phase during their job trajectories.
19 The prevalence of MJH in the Korean labor force has steadily increased over the past few years, and experts anticipate that it will continue to grow in the future.
20 It is thus imperative to fully understand how MJH poses a threat to workers, to provide successful interventions for improving Korean workers’ health.
Gender is an important aspect in studying the occupational risk of MJH; it is well-established that there are differences in occupational hazard exposures faced by men and women.
21 While more men were found to be unprotected from physical hazards, more women suffered poor psychosocial working environments, possibly reflecting gender-based work divisions in certain industries, and gender inequalities in employment conditions.
22 Under these circumstances, it is plausible that MJH may impact men and women workers’ health in different ways; articulating this difference could enlighten the health effect pathway of MJH.
In this context, this study explored the association between MJH and various physical and psychological symptoms workers experience, using large survey data representing the Korean workforce, especially those aged 15–59 years, considered active laborers. Furthermore, gender-stratified analysis was conducted to identify differences in the effects of MJH depending on workers’ gender.
METHODS
Data source and study population
We conducted a population-based cross-sectional study among workers aged below 60 years in South Korea, to investigate the association between MJH status and various symptoms worker experience. We used data from the 6
th Korean Working Conditions Survey (KWCS), which conducts cross-sectional surveys on various working conditions related to occupational safety and health among workers in South Korea. Survey items are based on a recent version of the European Working Conditions Survey.
23,24 A total of 50,538 workers aged above 15 years in South Korea participated in the survey held from October 5, 2020, to December 12, 2020, and from January 27, 2021, to April 11, 2021.
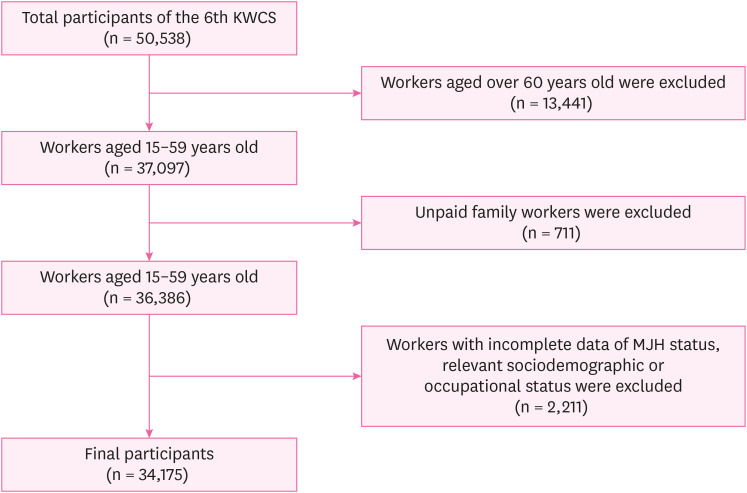
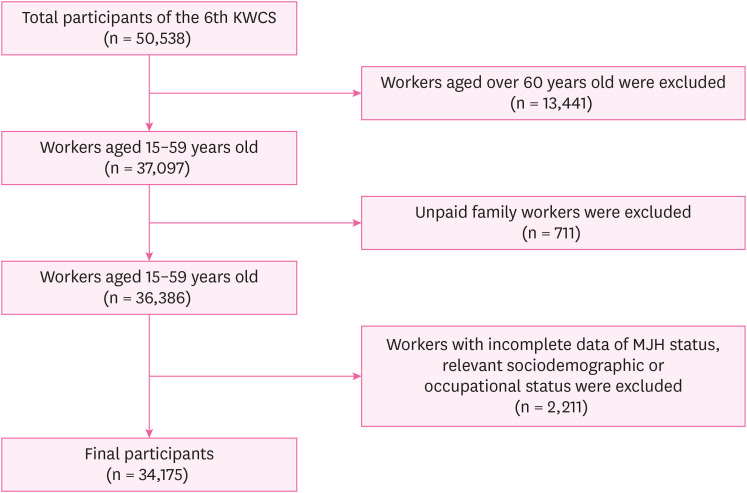
The study selection process is shown in
Fig. 1. First, workers aged 60 years or above (n = 13,441), the statutory retirement age defined by the Korean law, were excluded. Elderly workers differ to those younger in several aspects regarding employment. For instance, they might make income from pensions and other sources than their job wages,
25 and enjoy support from projects promoting senior employment held by government.
26 On the other hand, they might suffer disadvantages when seeking a job, such as employers’ unwillingness to hire the elderly.
27 Such context extends to the phenomenon of MJH. Although only a few qualitative researches and no direct comparative study dealt MJH of the elderly, it has been suggested that older MJHers may differ to the younger workers.
27 Therefore we decided to limit the participants to those aged under 60 years to avoid possible heterogeneity among the workers and observe characteristic effect of MJH.
Fig. 1
Sample selection with inclusion and exclusion criteria.
KWCS: Korean Working Conditions Survey; MJH: multiple job-holding.
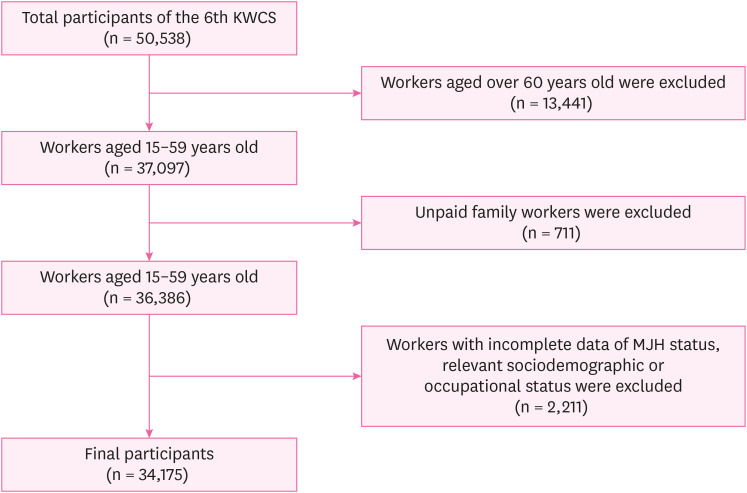
In addition, unpaid family workers (n = 711) were excluded to ensure that the analysis of MJH effect to be consistent with the definition of MJH, as the component of ‘compensation’ was stressed by prior research on MJH.
1 Participants who did not answer questions on their MJH status, relevant sociodemographic and occupational status (n = 2,211) were also excluded. As a result, the final sample comprised 34,175 participants.
MJH status was defined as the primary exposure variable. Participants were asked, “How many jobs do you have?” Those responding “1” were categorized as SJHers; those responding “2” or “3 or more” were categorized as MJHers.
Five symptoms were defined as outcome variables. Participants were asked if they had experienced certain symptoms over the past 12 months. Musculoskeletal pain events were identified by the response “yes” to at least one of the 3 items regarding physical pain: lower back, upper limbs, and lower limbs. Similarly, headache or eyestrain, fatigue, and anxiety events were identified by the response “yes” to the corresponding items. Insomnia was measured using the Minimal Insomnia Symptom Scale, consisting of a 3-item questionnaire. Responses for each item are measured by a 5-point Likert scale, where the higher points on the scale indicate a higher score; point of 1 = “daily,” score 0, to points of 5 = “never,” score 4. The sum of the scores ranged from 0 to 12, and participants with a total score higher than 6 were identified as being affected by insomnia, in accordance with previous studies.
28
Other variables were measured as covariates. Sociodemographic characteristics included age (15–29, 30–39, 40–49, or 50–59), gender (man or woman), education level (high-school graduate or lower, or college graduate), and monthly income (per 10,000 KRW: < 200, 200–299, 300–399, or ≥ 400) from the main job. Occupational characteristics included status of employment (employed by other employer, or self-employed) of the main job, occupational category (white-collar, service, or blue-collar) of the main job, weekly workhours (≤ 40, > 40 and ≤ 52, or > 52 hours) in all jobs, shift work (yes or no) of the main job, and night work (yes or no) of the main job. Occupational categories were identified according to the 7th Korean Standard Classification of Occupations. Weekly working hours were categorized according to the Labor Standard Act of Korea.
Statistical analysis
Descriptive analyses were performed to describe the characteristics and prevalence of various symptoms of MJHers and SJHers. Chi-square tests were conducted to evaluate differences in characteristics and symptoms among the groups. Multiple logistic regression analyses were performed, with SJHers as the reference group, to estimate the odds ratio (OR) with 95% confidence intervals (CIs) and to verify the associations between MJH and symptoms. Stratified analyses were repeated in the groups of men and women workers to determine the differences in the effects of MJH depending on gender. All regression analyses were conducted using crude and adjusted models, with the latter adjusted for sociodemographic and occupational characteristics. All analyses were performed using the survey weight values assigned to each participant provided by the 6th KWCS to obtain unbiased estimates. The analyses were performed using SAS software (version 9.4; SAS Institute, Cary, NC, USA) at a significance level of 0.05.
Ethics statement
Institutional Review Board (IRB) of Seoul National University Hospital determined to exempt the review of this study and approved the waiver of written informed consent due to the secondary use of anonymous information (IRB No. E-2208-111-1351).
RESULTS
Table 1 shows the sociodemographic and occupational characteristics of the study population according to MJH status. The final sample consisted of 238 MJHers and 36,749 SJHers. Among the participants, 135 were men MJHers and 103 were women. Compared to SJHers, MJHers were more likely to be older (40–59 years, 68.51%) and earn lower incomes (< 2 million KRW, 38.20%). However, gender and education levels of MJHers did not differ significantly from that of the SJHers. From the perspective of occupational characteristics, MJHers were more likely to be self-employed (35.47%) and work for more than 40 hours (63.52%). Meanwhile, MJHers were less likely to engage in shifts at their main job (4.54%). The differences in occupational categories and nighttime work engagement between MJHers and SJHers were not statistically significant.
Table 1 Participants’ characteristics according to multiple job-holding status
|
Characteristics |
Total |
SJHers (weighted) |
MJHers (weighted) |
p-value |
|
Total |
36,986 (100.0) |
36,749 (99.4) |
238 (0.6) |
|
|
Gender |
|
|
|
0.757 |
|
Man |
21,516 (58.2) |
21,381 (58.2) |
135 (56.8) |
|
Woman |
15,470 (41.8) |
15,368 (41.8) |
103 (43.2) |
|
Age (year) |
|
|
|
0.050*
|
|
15–29 |
6,507 (17.6) |
6,466 (17.6) |
41 (17.3) |
|
30–39 |
9,083 (24.6) |
9,049 (24.6) |
34 (14.2) |
|
40–49 |
10,710 (29.0) |
10,623 (28.9) |
88 (37.0) |
|
50–59 |
10,686 (28.9) |
10,611 (28.9) |
75 (31.5) |
|
Education |
|
|
|
0.219 |
|
High-school graduate or lower |
23,433 (63.4) |
23,270 (63.3) |
163 (68.7) |
|
College graduate |
13,553 (36.6) |
13,479 (36.7) |
74 (31.3) |
|
Monthly income (10,000 KRW) |
|
|
|
< 0.001***
|
|
< 200 |
8,081 (21.8) |
7,990 (21.7) |
91 (38.2) |
|
200–299 |
12,004 (32.5) |
11,931 (32.5) |
74 (31.1) |
|
300–399 |
8,979 (24.3) |
8,942 (24.3) |
37 (15.6) |
|
≥ 400 |
7,922 (21.4) |
7,886 (21.5) |
36 (15.1) |
|
Status of employment |
|
|
|
< 0.001***
|
|
Employed by other employer |
30,780 (83.2) |
30,626 (83.3) |
153 (64.5) |
|
Self-employed |
6,206 (16.8) |
6,122 (16.7) |
84 (35.5) |
|
Category |
|
|
|
0.811 |
|
White-collar |
17,380 (47.0) |
17,262 (47.0) |
117 (49.4) |
|
Service |
8,070 (21.8) |
8,023 (21.8) |
47 (19.8) |
|
Blue-collar |
11,536 (31.2) |
11,463 (31.2) |
73 (30.8) |
|
Weekly workhours (hours) |
|
|
|
< 0.001***
|
|
≤ 40 |
24,035 (65.0) |
23,948 (65.2) |
87 (36.5) |
|
> 40, ≤ 52 |
8,674 (23.5) |
8,595 (23.4) |
79 (33.1) |
|
> 52 |
4,278 (11.6) |
4,205 (11.4) |
72 (30.5) |
|
Shift work |
|
|
|
0.042*
|
|
No |
33,714 (91.2) |
33,488 (91.1) |
227 (95.5) |
|
Yes |
3,272 (8.8) |
3,261 (8.9) |
11 (4.5) |
Table 2 shows the prevalence of various symptoms and differences among the participants according to their MJH status. Several symptoms were more frequently experienced by MJHers than SJHers, as they reported more headaches or eyestrain (32.17% vs. 19.94%,
p-value = 0.001), fatigue (33.86% vs. 24.28%,
p-value = 0.02), insomnia (12.80% vs. 7.54%,
p-value = 0.008), and anxiety (12.75% vs. 5.56%,
p-value = 0.003). Musculoskeletal pain (44.90% vs. 36.81%) was also more common among MJHers; however, the difference was not statistically significant. When stratified by gender, no symptoms were significantly more frequent among men. In contrast, more symptoms were observed among women MJHers, all of which were statistically significant (
Table 3).
Table 2 Prevalence of the physical and psychological health symptoms according to multiple job-holding status
|
Health outcomes |
SJHers |
MJHers |
p-value |
|
Physical symptoms |
|
|
|
|
Musculoskeletal pain |
13,512 (36.81) |
107 (44.90) |
0.072 |
|
Headache or eyestrain |
7,318 (19.94) |
76 (32.17) |
0.001**
|
|
Fatigue |
8,911 (24.28) |
80 (33.86) |
0.020*
|
|
Psychological symptoms |
|
|
|
|
Insomnia |
2,771 (7.54) |
30 (12.80) |
0.008**
|
|
Anxiety |
2,040 (5.56) |
30 (12.75) |
0.003**
|
Table 3 Prevalence of the physical and psychological symptoms in the participants according to multiple job-holding status, stratified by gender
|
Health outcomes |
SJHers |
MJHers |
p-value |
|
Man |
|
|
|
|
Physical health |
|
|
|
|
|
Musculoskeletal pain |
7,634 (35.74) |
51 (38.16) |
0.671 |
|
|
Headache or eyestrain |
4,159 (19.48) |
35 (25.61) |
0.185 |
|
|
Fatigue |
5,206 (24.37) |
35 (26.07) |
0.730 |
|
Psychological health |
|
|
|
|
|
Insomnia |
1,504 (7.04) |
15 (10.94) |
0.140 |
|
|
Anxiety |
1,207 (5.65) |
14 (10.33) |
0.109 |
|
Woman |
|
|
|
|
Physical health |
|
|
|
|
|
Musculoskeletal pain |
5,878 (38.31) |
55 (53.73) |
0.027*
|
|
|
Headache or eyestrain |
3,158 (20.58) |
42 (40.77) |
< 0.001***
|
|
|
Fatigue |
3,705 (24.15) |
45 (44.08) |
0.020*
|
|
Psychological health |
|
|
|
|
|
Insomnia |
1,267 (8.25) |
16 (15.23) |
0.023*
|
|
|
Anxiety |
833 (5.43) |
16 (15.94) |
0.007**
|
The associations between MJH status and various symptoms are shown in
Table 4. In the crude model, MJHers were more likely to suffer headache or eyestrain (OR: 1.91, 95% CI: 1.27–2.85), fatigue (OR: 1.60, 95% CI: 1.07–2.38), insomnia (OR: 1.80, 95% CI: 1.16–2.80) and anxiety (OR: 2.49, 95% CI: 1.34–4.64). Musculoskeletal pain (OR: 1.40, 95% CI: 0.97–2.02) was not significantly associated with MJH. When adjusted for sociodemographic and occupational characteristics, headache or eyestrain (OR: 1.85, 95% CI: 1.23–2.78) and anxiety (OR: 1.99, 95% CI: 1.05–3.79) remained significantly associated with MJH. The VIF of all covariates entered in every regression model ranged from 1 to 2 (Supplementary Table 1), hence multicollinearity between the covariates were assumed acceptable.
Table 4 ORs (95% CIs) for the symptoms of multiple job-holders (single job-holding is reference category)
|
Health outcomes |
Crude model |
Adjusted modela
|
|
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
|
Physical health |
|
|
|
|
|
Musculoskeletal pain |
1.40 (0.97–2.02) |
0.073 |
1.20 (0.80–1.80) |
0.3722 |
|
Headache or eyestrain |
1.91 (1.27–2.85) |
0.002**
|
1.85 (1.23–2.78) |
0.0034**
|
|
Fatigue |
1.60 (1.07–2.38) |
0.021*
|
1.38 (0.90–2.12) |
0.1429 |
|
Psychological health |
|
|
|
|
|
Insomnia |
1.80 (1.16–2.80) |
0.009**
|
1.56 (0.98–2.47) |
0.0587 |
|
Anxiety |
2.49 (1.34–4.64) |
0.004**
|
1.99 (1.05–3.79) |
0.0363*
|
Table 5 presents the results of the gender-stratified analyses. The effects of MJH on workers’ experience on various symptoms differed significantly between the genders. Among men, no symptoms were associated with MJH in the crude or adjusted models. On the other hand, women MJHers showed to be more sensitive to the effect of MJH, as they showed higher risk of musculoskeletal pain (OR: 1.85, 95% CI: 1.02–3.34), headache or eyestrain (OR: 2.53, 95% CI: 1.37–4.67), fatigue (OR: 2.38, 95% CI: 1.29–4.40), insomnia (OR: 1.92, 95% CI: 1.04–3.57), and anxiety (OR: 2.83, 95% CI: 1.11–7.20).
Table 5 ORs (95% CIs) for the symptoms of multiple job-holders (single job-holding is reference category), stratified by gender
|
Health outcomes |
Crude model |
Adjusted modela
|
|
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
|
Male |
|
|
|
|
|
Physical health |
|
|
|
|
|
|
Musculoskeletal pain |
1.11 (0.69–1.80) |
0.667 |
0.81 (0.48–1.39) |
0.4460 |
|
|
Headache or eyestrain |
1.42 (0.84–2.41) |
0.186 |
1.39 (0.80–2.40) |
0.2455 |
|
|
Fatigue |
1.10 (0.66–1.83) |
0.724 |
0.82 (0.48–1.42) |
0.4858 |
|
Psychological health |
|
|
|
|
|
|
Insomnia |
1.62 (0.85–3.11) |
0.144 |
1.27 (0.64–2.52) |
0.4955 |
|
|
Anxiety |
1.92 (0.85–4.34) |
0.115 |
1.44 (0.63–3.32) |
0.3911 |
|
Female |
|
|
|
|
|
Physical health |
|
|
|
|
|
|
Musculoskeletal pain |
1.87 (1.07–3.28) |
0.029*
|
1.85 (1.02–3.34) |
0.0415*
|
|
|
Headache or eyestrain |
2.66 (1.46–4.84) |
0.001**
|
2.53 (1.37–4.67) |
0.0029**
|
|
|
Fatigue |
2.48 (1.38–4.47) |
0.003**
|
2.38 (1.29–4.40) |
0.0055**
|
|
Psychological health |
|
|
|
|
|
|
Insomnia |
2.00 (1.09–3.68) |
0.026*
|
1.92 (1.04–3.57) |
0.0385*
|
|
|
Anxiety |
3.31 (1.31–8.33) |
0.011*
|
2.83 (1.11–7.20) |
0.0289*
|
DISCUSSION
Using a nationally representative sample of Korean workers, this study investigated whether MJHers exhibit greater susceptibility to work-related health issues than SJHers. The findings revealed significantly elevated odds of experiencing conditions such as headaches or eyestrain, and anxiety among MJHers. When the data were stratified by gender, a more pronounced prevalence of symptoms was observed among women workers holding multiple jobs. In particular, their odds of experiencing musculoskeletal pain, headaches or eyestrain, fatigue, insomnia, and anxiety was 2 to 3 times higher than those of their women counterparts with a single job. Conversely, no discernible association was found between men workers with multiple jobs and those with only one job in terms of physical and psychological ailments. This study underscores the potential exacerbation of work-related physical and psychological symptoms, particularly among women MJHers engaged in more than 2 jobs.
Working in more than one job can pose a significant threat to workers’ health. Previous studies have established the heightened susceptibility of MJHers compared to SJHers in terms of occupational injuries, personal well-being, and overall quality of working life. Research conducted using data from a US national survey has consistently demonstrated that injury rates among MJHers were markedly higher than those among SJHers.
9,11,29 Notably, this increased risk remained robust even after controlling for various working conditions, such as hourly pay and weekly work hours.
9 Further research has identified an elevated rate and severity of injuries among adolescent MJHers in Wisconsin, and a higher prevalence of work-related fatalities among MJHers in Kentucky.
11,29 A separate study examining the relationship between work-related injuries and various occupational and non-occupational factors found that construction workers face a higher risk of occupational injuries than non-construction workers, with the concurrent holding of multiple jobs emerging as a significant risk factor for elevated injury rates.
10 Moreover, work-family conflict is an occupational stressor that can significantly impact employees’ health and well-being. Boyd et al.
14 investigated the influence of multiple jobs on work-family conflict among US firefighters, specifically analyzing whether work-family conflict stemming from MJHers’ first and second jobs had an additive or interactive effect on well-being. They found that work-family conflict originating from each job acts as an independent stressor, and interacts with other sources of conflict to influence well-being. This suggests that when additional stress is experienced within the second job, the effects of work-family conflict from the first job are magnified.
14
We observed significantly higher odds of experiencing adverse symptoms among MJHers, particularly women. These findings broadly align with a recent cross-sectional analysis exploring whether MJHers allocate their time differently than SJHers, and how holding a second job impacts an individual's subjective well-being.
30 The study revealed that MJHers invested more time in work and commuting activities, which led to reduced sleep and relaxation. Regarding personal well-being, MJHers tended to engage in less relaxation and reported a lower sense of well-being than SJHers. Notably, research indicates that the influence of holding multiple jobs on time allocation and subjective well-being varies by gender. Women MJHers allocated more time to housework and childcare responsibilities compared to men, both SJHers and MJHers. This suggests that the traditional pattern of time use persists, with women dedicating more time to housework and childcare, even among those who hold multiple jobs. Additionally, women MJHers were more likely to report poorer well-being compared to women SJHers, while men workers reported no significant differences in well-being regardless of the number of jobs they held. These gender-specific variations shed light on the intricate relationship between MJHs, time allocation, and subjective well-being.
Understanding why individuals engaged in MJH exhibit more pronounced health vulnerabilities requires a comprehensive grasp of the intrinsic characteristics in various occupations, as well as the gender disparities prevalent in both workplace and societal contexts. While there remains a lack of consensus on categorizing MJHs as precarious employment,
31 it is evident that MJHers frequently contend with adverse working conditions that exert a detrimental impact on their well-being and safety.
32 These conditions include prolonged working hours and temporary employment contracts, with the former being recognized as one of the most substantial occupational health hazards.
Workers engaged in multiple jobs may encounter heightened challenges in effectively managing their working hours, and may find themselves working excessively. This can be attributed to their primary jobs already consuming the maximum allowable working hours, or the complexity of their schedules stemming from the need to work at different locations and times to fulfill multiple roles. Unlike their counterparts with singular employment, MJHers face fragmented schedules, limiting their ability to allocate sufficient time for uninterrupted rest or breaks. In the instance of MJHers who undertake a morning commute to their primary job, only to return from their secondary job late in the evening, they find themselves compelled to compensate for potentially shortened nighttime sleep with daytime naps, or face the consequences of drowsiness. This ultimately results in the degradation of sleep quality, characterized by an irregular sleep pattern.
33 Furthermore, the demanding schedules of MJHers afford them even less time to engage in other essential activities aimed at rejuvenating and improving their overall well-being, including social interactions and medical appointments. This places them in a less advantageous position for safeguarding their health. Hence, extended working hours emerge as a potential risk factor contributing to the increased risks of physical and psychological symptoms suffered by individuals engaged in MJH.
The prevalence of temporary contracts presents another compelling explanation for MJHers’ health vulnerabilities. As MJHers manage their primary employment alongside contractual commitments, employers may be limited in their ability to mandate permanent positions and provide flexibility, primarily because of the MJHers’ secondary job responsibilities. Consequently, temporary, contractual, and interim positions may seem ideal. However, the labor market’s societal and institutional perspectives are predominantly structured around single-occupational roles, often failing to comprehensively protect the labor rights and safety of MJH participants. A pertinent example can be found in South Korea, where although the number of workers involved in MJH through short-term employment or platform-based work is increasing, a significant proportion of them operate under temporary or informal contracts due to the ambiguous legal status of their employment.
34 These contracts typically do not afford MJHers the full extent of protection outlined in South Korean labor laws, and they may lack access to employment-related welfare provided by employers, as noted in previous studies.
35 This state of employment precariousness can serve as a risk factor contributing to the compromised health status of MJHers.
In addition to longer working hours and temporary employment contracts, engagement in multiple jobs can introduce additional challenges, including exposure to diverse occupational hazards, the necessity to adapt to a full-time workload within the constraints of part-time schedules, and the potential for inexperience in one or more jobs that an individual holds.
9 These factors also contribute to the poor health of MJHers.
To the best of our knowledge, this study is the first to assess the increased prevalence of various physical and psychological symptoms among MJHers compared to conventional SJHers based on the same study population. Another strength of this study is the use of the KWCS data, which contain a large and nationally representative sample with reliability. This made it possible to analyze the general worker population, unlike most previous studies that were conducted on groups of specific occupations with a relatively higher proportion of MJHers. However, this study has several limitations. The weighted proportion of MJHers among the participants of this study was 0.64%, which is smaller than that reported in previous studies on South Korean workers, or laborers in foreign countries.
6,17,36 We speculate that the wording and order of the survey questions might be at play.
37 The questions regarding MJH do not specify a specific time frame, and are placed at the beginning of the entire survey, possibly leading the participants to consider their secondary jobs unimportant or insignificant compared to their primary jobs, thereby excluding them from their responses. However, we believe that the MJHers observed in this study may be considered workers who engage in MJH at a much more rigorous and precise level. The data collected in the KWCS, which primarily focused on the main job, was another limitation. There is a lack of detailed information on secondary jobs regarding occupational type, employment status, work schedule, and tenure, making it difficult to analyze the specific impact of MJH on workers’ experience of symptoms. Some of the covariates used in this study were based on the participants’ main jobs, allowing for an inaccurate reflection of the differences in working conditions between MJHers and SJHers. Additionally, owing to its cross-sectional design, this study could not clarify the causality of the effects of MJH. Finally, since the number of individuals defined as MJHers among the entire study population was relatively small, the possibility of the statistical power being insufficient to yield significant results for some symptoms cannot be ruled out.
CONCLUSIONS
The prevalence of MJH has gradually increased with technological advances and rapid societal changes. MJHers were more likely to experience various physical and psychological symptoms such as headaches or eyestrain, fatigue, insomnia, and anxiety than SJHers. This association was particularly evident among women workers. Further research is required to establish evidence of causality, the social context of MJH, and its effect on health. We suggest the need for appropriate monitoring and intervention to maintain the well-being of MJHers, and policy discussions regarding the issue.
Acknowledgements
The authors thank the Occupational Safety and Health Research Institute of Korea.
Abbreviations
Institutional Review Board
Korean Working Conditions Survey
NOTES
-
Funding: This work was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and Technology (grant number, 2022R1A2C2010463). This work was supported by the Education and Research Encouragement Fund of Seoul National University Hospital.
-
Competing interests: The authors declare that they have no competing interests.
-
Authors contributions:
Conceptualization: Son SY, Min KB.
Data curation: Son SY, Ryoo SW.
Formal analysis: Son SY.
Funding acquisition: Min KB.
Methodology: Son SY, Min KB.
Software: Son SY.
Validation: Min JY, Min KB.
Visualization: Son SY, Choi BY.
Writing - original draft: Son SY, Min JY.
Writing - review & editing: Min KB, Ryoo SW, Choi BY.
SUPPLEMENTARY MATERIALS
Supplementary Table 1
Variance inflation factor values of the covariates adjusted in each regression model
aoem-36-e21-s001.xls
REFERENCES
REFERENCES
- 1. Campion ED, Caza BB, Moss SE. Multiple jobholding: an integrative systematic review and future research agenda. J Manage 2020;46(1):165–191.ArticlePDF
- 2. Jeong S. Trends and characteristics of dual job holders. Mon Labor Rev 2017;143:51–67.
- 3. Hipple SF. Multiple Jobholding during the 2000s. Mon Labor Rev 2010;133(7):21–32.
- 4. US Bureau of Labor Statistics. Labor force statistics from the current population study: household data, table 36. Multiple jobholders by selected characteristics. Updated 2023]. Accessed November 13, 2023].
https://www.bls.gov/cps/cpsaat36.htm
.
- 5. Eurostat. Labour force survey: employed persons having a second job by sex, age and educational attainment level (1000), 2013 to 2022. Updated 2023]. Accessed November 13, 2023].
https://ec.europa.eu/eurostat/databrowser/view/LFSA_E2GED/default/table?lang=en
.
- 6. Pouliakas K, Conen WS. Multiple job-holding: career pathway or dire straits? IZA World Labor 2023;356.
- 7. Conen W, Stein J. A panel study of the consequences of multiple jobholding: enrichment and depletion effects. Transfer 2021;27(2):219–236.ArticlePDF
- 8. Jamal M, Baba VV, Riviere R. Job stress and well‐being of moonlighters: the perspective of deprivation or aspiration revisited. Stress Med 1998;14(3):195–202.Article
- 9. Marucci-Wellman HR, Willetts JL, Lin TC, Brennan MJ, Verma SK. Work in multiple jobs and the risk of injury in the US working population. Am J Public Health 2014;104(1):134–142. 24228681.ArticlePubMedPMC
- 10. Dong XS, Wang X, Largay JA. Occupational and non-occupational factors associated with work-related injuries among construction workers in the USA. Int J Occup Environ Health 2015;21(2):142–150. 25816923.ArticlePubMedPMC
- 11. Bush AM, McKee SE, Bunn TL. Multiple jobholder mortality patterns in Kentucky: an examination of occupational fatalities. Am J Ind Med 2013;56(8):881–888. 23729179.ArticlePubMed
- 12. Marucci-Wellman HR, Lombardi DA, Willetts JL. Working multiple jobs over a day or a week: short-term effects on sleep duration. Chronobiol Int 2016;33(6):630–649. 27092404.ArticlePubMedPMCPDF
- 13. Bruns A, Pilkauskas N. Multiple job holding and mental health among low-income mothers. Womens Health Issues 2019;29(3):205–212. 30827826.ArticlePubMedPMC
- 14. Boyd EM, Sliter MT, Chatfield S. Double trouble: work–family conflict and well-being for second job holders. Community Work Fam 2016;19(4):462–480.Article
- 15. Bouwhuis S, Garde AH, Geuskens GA, Boot CR, Bongers PM, van der Beek AJ. The longitudinal association between multiple job holding and long-term sickness absence among Danish employees: an explorative study using register-based data. Int Arch Occup Environ Health 2017;90(8):799–807. 28669035.ArticlePubMedPMCPDF
- 16. Alali H, Braeckman L, Van Hecke T, De Clercq B, Janssens H, Wahab MA. Relationship between non-standard work arrangements and work-related accident absence in Belgium. J Occup Health 2017;59(2):177–186. 28111414.ArticlePubMedPMCPDF
- 17. Im Y. Characteristics of moonlighters and their relationships between primary jobs according to their age. Mon Labor Rev 2021;200:91–95.
- 18. Jang DJ, Kong HS. A study on factors influencing the subjective health status of dual job worker. J Convergence Cult Technol 2023;9(1):513–523.
- 19. Hwang S. Exploring the structural and personal factors of the ‘N-job phenomenon’. Korean J Ind Relat 2022;32(3):89–122.Article
- 20. Kim D. Analyses on scale and characteristics of side hustles. Labor Trend Brief 2022;1:2–13.
- 21. Biswas A, Harbin S, Irvin E, Johnston H, Begum M, Tiong M, et al. Sex and gender differences in occupational hazard exposures: a scoping review of the recent literature. Curr Environ Health Rep 2021;8(4):267–280. 34839446.ArticlePubMedPMCPDF
- 22. Campos-Serna J, Ronda-Pérez E, Artazcoz L, Moen BE, Benavides FG. Gender inequalities in occupational health related to the unequal distribution of working and employment conditions: a systematic review. Int J Equity Health 2013;12(1):57. 23915121.ArticlePubMedPMC
- 23. Parent-Thirion A, Biletta I, Cabrita J, Vargas Llave O, Vermeylen G, Wilczyńska A, et al. Sixth European Working Conditions Survey: Overview Report. Dublin, Ireland: Eurofound; 2016.
- 24. Cho Y. Data resource profile: the Korean Working Conditions Survey (KWCS). Ann Occup Environ Med 2023;35(1):e49. 38148917.ArticlePubMedPMCPDF
- 25. Lee S, Lee W, Kim S. Elderly Labor and Poverty. Sejong, Korea: Korea Labor Institute; 2020.
- 26. Kim JS, Kim SW. Factors on continuing participation in the elderly employment program with the semi-elderly. J Korea Contents Assoc 2016;16(4):718–728.
- 27. Bouwhuis S, De Wind A, De Kruif A, Geuskens GA, Van der Beek AJ, Bongers PM, et al. Experiences with multiple job holding: a qualitative study among Dutch older workers. BMC Public Health 2018;18(1):1054. 30134871.ArticlePubMedPMCPDF
- 28. Westergren A, Broman JE, Hellström A, Fagerström C, Willman A, Hagell P. Measurement properties of the minimal insomnia symptom scale as an insomnia screening tool for adults and the elderly. Sleep Med 2015;16(3):379–384. 25666846.ArticlePubMed
- 29. Zierold KM, Appana S, Anderson HA. School-sponsored work programs: a first look at differences in work and injury outcomes of teens enrolled in school-to-work programs compared to other-working teens. Occup Environ Med 2011;68(11):818–825. 21398680.ArticlePubMed
- 30. Hill B. Time use and subjective well-being of multiple jobholders: evidence from the American time use survey. Labor Stud J 2023;48(4):305–323.ArticlePDF
- 31. Bouwhuis S, Geuskens GA, van der Beek AJ, Boot CR. Multiple-job holding is not a type of precarious employment. Scand J Work Environ Health 2019;45(1):98–99. 30358881.ArticlePubMed
- 32. Koranyi I, Jonsson J, Rönnblad T, Stockfelt L, Bodin T. Precarious employment and occupational accidents and injuries - a systematic review. Scand J Work Environ Health 2018;44(4):341–350. 29443355.ArticlePubMed
- 33. Weaver MD, Sletten TL, Foster RG, Gozal D, Klerman EB, Rajaratnam SM, et al. Adverse impact of polyphasic sleep patterns in humans: report of the National Sleep Foundation sleep timing and variability consensus panel. Sleep Health 2021;7(3):293–302. 33795195.ArticlePubMed
- 34. Kim J, Jang J, Kim G, Bak S. Scales and working conditions of platform workers. Updated 2022]. Accessed May 16, 2024].
https://www.keis.or.kr/user/extra/main/3885/publication/publicationList/jsp/LayOutPage.do?categoryIdx=131&pubIdx=8972&spage2=12
.
- 35. Lee SW. Legislative approaches to protect ‘economically dependent workers’. J Labour Law 2006;23:185–228.
- 36. Bailey KA, Spletzer JR. A new measure of multiple jobholding in the U.S. economy. Labour Econ 2021;71:102009.Article
- 37. Moore DW. Measuring new types of question-order effects: additive and subtractive. Public Opin Q 2002;66(1):80–91.
 , Jin-Young Min2
, Jin-Young Min2 , Seung-Woo Ryoo1
, Seung-Woo Ryoo1 , Baek-Yong Choi1
, Baek-Yong Choi1 , Kyoung-Bok Min1
, Kyoung-Bok Min1

 KSOEM
KSOEM

 Cite
Cite

