Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 32; 2020 > Article
- Research Article Factors related to femoral bowing among Korean female farmers: a cross-sectional study
-
Sangyoon Do1
 , Chul Gab Lee1
, Chul Gab Lee1 , Dong Hwi Kim2
, Dong Hwi Kim2 , GwangChul Lee2
, GwangChul Lee2 , Kweon Young Kim3
, Kweon Young Kim3 , So Yeon Ryu4
, So Yeon Ryu4 , Hansoo Song1
, Hansoo Song1
-
Annals of Occupational and Environmental Medicine 2020;32:e23.
DOI: https://doi.org/10.35371/aoem.2020.32.e23
Published online: July 2, 2020
1Department of Occupational and Environmental Medicine, Chosun University Hospital, Gwangju, Korea.
2Department of Orthopedic Medicine, Chosun University Hospital, Gwangju, Korea.
3Department of Rehabilitation Medicine, Chosun University Hospital, Gwangju, Korea.
4Department of Preventive Medicine, Chosun University Hospital, Gwangju, Korea.
- Correspondence: Hansoo Song. Department of Occupational and Environmental Medicine, Chosun University Hospital, 365 Pilmun-daero, Dong-gu, Gwangju 61453, Korea. oemsong@chosun.ac.kr
Copyright © 2020 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background Female farmers have a high prevalence of knee osteoarthritis (KOA) in South Korea. Femoral bowing has been reported to be related to KOA by increasing load on the mechanical axis. This study aimed to investigate factors related to femoral bowing in Korean female farmers.
-
Methods We analyzed the legs of 264 female farmers registered with the Korea farmers' knee cohort of Jeonnam Center for Farmers' Safety and Health. A structured questionnaire was used to determine sociodemographic variables, agricultural career, cumulative squatting working time (CSWT), and cumulative heavy lifting working time. Femoral bone density was measured and Kellgren-Lawrence (KL) grades were obtained from the knee radiographs. Mechanical axis angle (MAA), femoral bowing angle (FBA), anatomical lateral distal femoral angle (aLDFA), anatomical medial proximal tibial angle (aMPTA), and condylar-plateau angle (CPA) were measured. We examined the relationship between the FBA and related factors by using multiple linear regression.
-
Results The proportion of individuals with radiographic KOA (≥ KL grade 2) in this study was 37.9%. As KL grades increased, MAA, FBA, and CPA increased, whereas aLDFA and aMPTA decreased. FBA increased with age. Multiple linear regression analyses using FBA as a dependent variable showed relationship with higher age, lower height, higher BMI, lower bone mineral density, longer CSWT, and longer agricultural careers.
-
Conclusions The results of this study suggest that external factors related to agricultural work in female farmers was associated with femoral bowing, in addition to internal factors such as age, bone density, height, and obesity.
BACKGROUND
METHODS
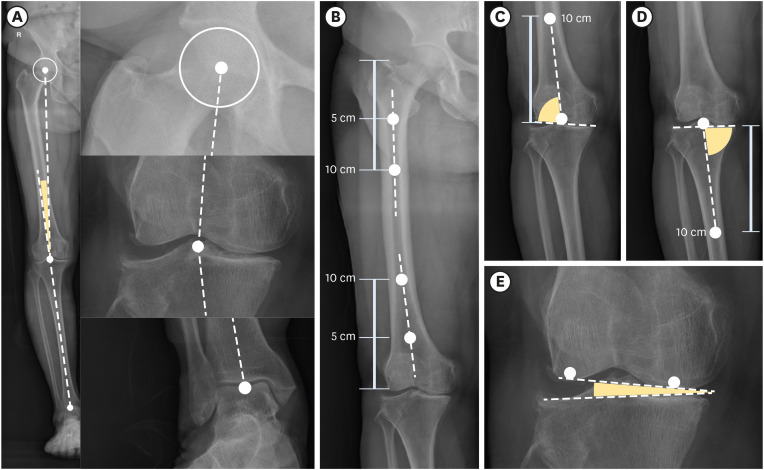
Measurement of MAA and lower limb angles. (A) MAA, (B) femoral bowing angle, (C) anatomical lateral distal femoral angle, (D) anatomical medial tibial angle, (E) condylar plateau angle.
RESULTS
General characteristics
Comparison of means of lower limb angles according to KL grade group
The correlation coefficient between factors
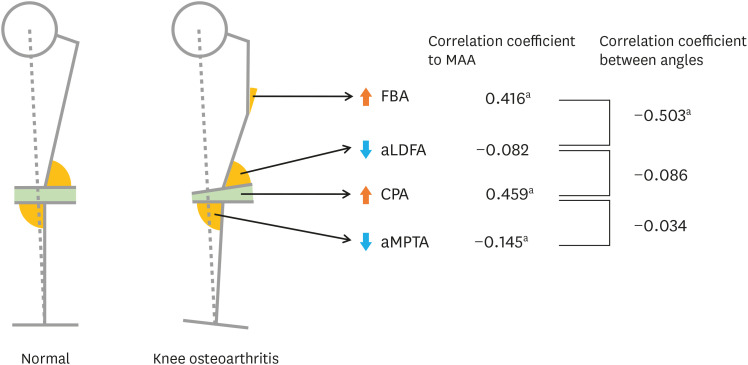
The change of lower limb angles from normal to knee osteoarthritis.
The related factors of femoral bowing angle by multiple linear regression
DISCUSSION
ACKNOWLEDGMENTS
Abbreviations
aLDFA
aMPTA
β
β*
BMD(f)
BMI
CI
CLWT
CPA
CSWT
FBA
ICC
KFKC
KL
KOA
MAA
r
4Q
-
Funding: This research was supported by the Ministry of Agriculture, Food and Rural Affairs in Republic of Korea.
-
Competing interests: The authors declare that they have no competing interests.
-
Author Contributions:
NOTES
SUPPLEMENTARY MATERIAL
Supplementary Table 1
- 1. Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis 2014;73(7):1323–1330. 24553908.ArticlePubMed
- 2. Kim H, Cho SK, Kim D, Kim D, Jung SY, Jang EJ, et al. Impact of osteoarthritis on household catastrophic health expenditures in Korea. J Korean Med Sci 2018;33(21):e161. 29780297.ArticlePubMedPMCPDF
- 3. Kim IJ, Kim HA, Seo YI, Jung YO, Song YW, Jeong JY, et al. Prevalence of knee pain and its influence on quality of life and physical function in the Korean elderly population: a community based cross-sectional study. J Korean Med Sci 2011;26(9):1140–1146. 21935267.ArticlePubMedPMCPDF
- 4. Hunter DJ, Schofield D, Callander E. The individual and socioeconomic impact of osteoarthritis. Nat Rev Rheumatol 2014;10(7):437–441. 24662640.ArticlePubMedPDF
- 5. Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage 2005;13(9):769–781. 15978850.ArticlePubMed
- 6. Koh IJ, Kim TK, Chang CB, Cho HJ, In Y. Trends in use of total knee arthroplasty in Korea from 2001 to 2010. Clin Orthop Relat Res 2013;471(5):1441–1450. 23054516.ArticlePubMedPMC
- 7. Seok H, Choi SJ, Yoon JH, Song GG, Won JU, Kim JH, et al. The association between osteoarthritis and occupational clusters in the Korean population: a nationwide study. PLoS One 2017;12(1):e0170229. 28099527.ArticlePubMedPMC
- 8. McWilliams DF, Leeb BF, Muthuri SG, Doherty M, Zhang W. Occupational risk factors for osteoarthritis of the knee: a meta-analysis. Osteoarthritis Cartilage 2011;19(7):829–839. 21382500.ArticlePubMed
- 9. Palmer KT. Occupational activities and osteoarthritis of the knee. Br Med Bull 2012;102(1):147–170. 22544778.ArticlePubMedPMC
- 10. Ding C, Cicuttini F, Scott F, Glisson M, Jones G. Sex differences in knee cartilage volume in adults: role of body and bone size, age and physical activity. Rheumatology (Oxford) 2003;42(11):1317–1323. 12810930.ArticlePubMed
- 11. Richmond RS, Carlson CS, Register TC, Shanker G, Loeser RF. Functional estrogen receptors in adult articular cartilage: estrogen replacement therapy increases chondrocyte synthesis of proteoglycans and insulin-like growth factor binding protein 2. Arthritis Rheum 2000;43(9):2081–2090. 11014360.ArticlePubMed
- 12. Jones G, Glisson M, Hynes K, Cicuttini F. Sex and site differences in cartilage development: a possible explanation for variations in knee osteoarthritis in later life. Arthritis Rheum 2000;43(11):2543–2549. 11083279.ArticlePubMed
- 13. Tanamas S, Hanna FS, Cicuttini FM, Wluka AE, Berry P, Urquhart DM. Does knee malalignment increase the risk of development and progression of knee osteoarthritis? A systematic review. Arthritis Rheum 2009;61(4):459–467. 19333985.ArticlePubMed
- 14. Brouwer GM, van Tol AW, Bergink AP, Belo JN, Bernsen RMD, Reijman M, et al. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum 2007;56(4):1204–1211. 17393449.ArticlePubMed
- 15. Sharma L, Chmiel JS, Almagor O, Felson D, Guermazi A, Roemer F, et al. The role of varus and valgus alignment in the initial development of knee cartilage damage by MRI: the MOST study. Ann Rheum Dis 2013;72(2):235–240. 22550314.ArticlePubMedPMC
- 16. Hayashi D, Englund M, Roemer FW, Niu J, Sharma L, Felson DT, et al. Knee malalignment is associated with an increased risk for incident and enlarging bone marrow lesions in the more loaded compartments: the MOST study. Osteoarthritis Cartilage 2012;20(11):1227–1233. 22874524.ArticlePubMedPMC
- 17. Sharma L, Song J, Dunlop D, Felson D, Lewis CE, Segal N, et al. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis 2010;69(11):1940–1945. 20511608.ArticlePubMedPMC
- 18. Kim JM, Hong SH, Kim JM, Lee BS, Kim DE, Kim KA, et al. Femoral shaft bowing in the coronal plane has more significant effect on the coronal alignment of TKA than proximal or distal variations of femoral shape. Knee Surg Sports Traumatol Arthrosc 2015;23(7):1936–1942. 24760162.ArticlePubMedPDF
- 19. Park YC, Yoon SP, Yang KH. Localization of atypical femoral fracture on straight and bowed femurs. J Bone Metab 2019;26(2):123–131. 31223609.ArticlePubMedPMCPDF
- 20. Shin WC, Moon NH, Jang JH, Park KY, Suh KT. Anterolateral femoral bowing and loss of thigh muscle are associated with occurrence of atypical femoral fracture: effect of failed tension band mechanism in mid-thigh. J Orthop Sci 2017;22(1):99–104. 27720510.ArticlePubMed
- 21. Chang CB, Choi JY, Koh IJ, Seo ES, Seong SC, Kim TK. What should be considered in using standard knee radiographs to estimate mechanical alignment of the knee? Osteoarthritis Cartilage 2010;18(4):530–538. 20060951.ArticlePubMed
- 22. Sebastian AS, Wilke BK, Taunton MJ, Trousdale RT. Femoral bow predicts postoperative malalignment in revision total knee arthroplasty. J Arthroplasty 2014;29(8):1605–1609. 24704122.ArticlePubMed
- 23. Matsumoto T, Hashimura M, Takayama K, Ishida K, Kawakami Y, Matsuzaki T, et al. A radiographic analysis of alignment of the lower extremities--initiation and progression of varus-type knee osteoarthritis. Osteoarthritis Cartilage 2015;23(2):217–223. 25481289.ArticlePubMed
- 24. Shimosawa H, Nagura T, Harato K, Kobayashi S, Nakamura M, Matsumoto M, et al. Variation of three-dimensional femoral bowing and its relation to physical status and bone mineral density: a study with CT. Surg Radiol Anat 2019;41(12):1489–1495. 31520108.ArticlePubMedPDF
- 25. Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren-Lawrence classification of osteoarthritis. Clin Orthop Relat Res 2016;474(8):1886–1893. 26872913.ArticlePubMedPMCPDF
- 26. Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage 2007;15(Suppl A):A1–A56. 17320422.ArticlePubMed
- 27. Wright RW. MARS Group. Osteoarthritis classification scales: interobserver reliability and arthroscopic correlation. J Bone Joint Surg Am 2014;96(14):1145–1151. 25031368.ArticlePubMedPMC
- 28. Colebatch AN, Hart DJ, Zhai G, Williams FM, Spector TD, Arden NK. Effective measurement of knee alignment using AP knee radiographs. Knee 2009;16(1):42–45. 18790641.ArticlePubMed
- 29. Lasam MP, Lee KJ, Chang CB, Kang YG, Kim TK. Femoral lateral bowing and varus condylar orientation are prevalent and affect axial alignment of TKA in Koreans. Clin Orthop Relat Res 2013;471(5):1472–1483. 23011845.ArticlePubMedPMC
- 30. Jeong CH, Noh JH. Clinical and radiological analysis of angular deformity of lower extremities. J Korean Fract Soc 2017;30(3):156–166.ArticlePDF
- 31. Luo CF, Zeng BF, Koshino T. Transepicondylar line and condylar line as parameters for axial alignment in knee arthroplasty. Knee 2004;11(3):213–217. 15194098.ArticlePubMed
- 32. Cooke D, Scudamore A, Li J, Wyss U, Bryant T, Costigan P. Axial lower-limb alignment: comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis Cartilage 1997;5(1):39–47. 9010877.ArticlePubMed
- 33. Lu Y, Zheng Z, Chen W, Lv H, Lv J, Zhang Y. Dynamic deformation of femur during medial compartment knee osteoarthritis. PLoS One 2019;14(12):e0226795. 31860687.ArticlePubMedPMC
- 34. Song MH, Yoo SH, Kang SW, Kim YJ, Park GT, Pyeun YS. Coronal alignment of the lower limb and the incidence of constitutional varus knee in Korean females. Knee Surg Relat Res 2015;27(1):49–55. 25750894.ArticlePubMedPMC
- 35. Nagamine R, Miura H, Bravo CV, Urabe K, Matsuda S, Miyanishi K, et al. Anatomic variations should be considered in total knee arthroplasty. J Orthop Sci 2000;5(3):232–237. 10982663.ArticlePubMed
- 36. Mullaji AB, Marawar SV, Mittal V. A comparison of coronal plane axial femoral relationships in Asian patients with varus osteoarthritic knees and healthy knees. J Arthroplasty 2009;24(6):861–867. 18701244.ArticlePubMed
- 37. Yau WP, Chiu KY, Tang WM, Ng TP. Coronal bowing of the femur and tibia in Chinese: its incidence and effects on total knee arthroplasty planning. J Orthop Surg (Hong Kong) 2007;15(1):32–36. 17429114.ArticlePubMedPDF
- 38. Esposito S, Leonardi A, Lanciotti L, Cofini M, Muzi G, Penta L. Vitamin D and growth hormone in children: a review of the current scientific knowledge. J Transl Med 2019;17(1):87. 30885216.ArticlePubMedPMCPDF
- 39. Chung YS, Chung DJ, Kang MI, Kim IJ, Koh JM, Min YK, et al. Vitamin D repletion in Korean postmenopausal women with osteoporosis. Yonsei Med J 2016;57(4):923–927. 27189286.ArticlePubMedPMCPDF
- 40. Bhan A, Rao AD, Rao DS. Osteomalacia as a result of vitamin D deficiency. Endocrinol Metab Clin North Am 2010;39(2):321–331. 20511054.ArticlePubMed
- 41. Zhang Y, Hunter DJ, Nevitt MC, Xu L, Niu J, Lui LY, et al. Association of squatting with increased prevalence of radiographic tibiofemoral knee osteoarthritis: the Beijing Osteoarthritis Study. Arthritis Rheum 2004;50(4):1187–1192. 15077301.ArticlePubMed
- 42. Shanb AA, Youssef EF. The impact of adding weight-bearing exercise versus nonweight bearing programs to the medical treatment of elderly patients with osteoporosis. J Family Community Med 2014;21(3):176–181. 25374469.ArticlePubMedPMC
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Normative values of radiographic parameters in coronal plane lower limb alignment in a general Japanese population: A cross‐sectional study in the Iwaki cohort
Ryoto Kura, Eiji Sasaki, Eitaro Sato, Yukiko Sakamoto, Yuka Kimura, Kyota Ishibashi, Eiichi Tsuda, Yasuyuki Ishibashi
Journal of Experimental Orthopaedics.2025;[Epub] CrossRef - Femoral varus deformity predominates in male Chinese osteoarthritis patients with geographic variability in functional knee phenotypes
Songlin Li, Jiaming He, Weibo Zheng, Xuezhou Li, Jie Yang, Zhe Li, Houyi Sun, Zhuang Miao, Wenwei Qian, Peilai Liu, Qunshan Lu
Knee Surgery, Sports Traumatology, Arthroscopy.2025; 33(9): 3310. CrossRef - Relationship Between Magnetic Resonance Imaging-based Knee Cartilage Loss and Work-related Physical Workload in Farmers and Fishers
Hansoo Song, Yong Soo Cho, Hye-min Kim, Soo Hyeong Park, Dong Hwi Kim, Chul Gab Lee
Safety and Health at Work.2025;[Epub] CrossRef - Age‐related varus progression of femoral bowing and its related factors in the Iwaki cohort study
Takamasa Uehara, Eiji Sasaki, Kyota Ishibashi, Ryo Tomita, Ryoto Kura, Yukiko Sakamoto, Yuka Kimura, Sunao Tanaka, Eiichi Tsuda, Yasuyuki Ishibashi
Journal of Experimental Orthopaedics.2025;[Epub] CrossRef - The mediation effects of malalignment on the relation of sex to the risk of incidence tibiofemoral osteoarthritis
Haoyu Xin, Xiaoxiao Li, Yuqing Zhang, Chao Zeng, Guanghua Lei, Tuo Yang, Jie Wei
Osteoarthritis and Cartilage.2024; 32(9): 1134. CrossRef - Gender, BMI, and Age‐Related Variations in Lower Limb Alignment Parameters and CPAK Phenotypes in Chinese Patients with Knee Osteoarthritis
Songlin Li, Xi Chen, Sen Liu, Hongjun Xu, Yang Yu, Shanni Li, Zhaojing Yin, Yiyang Du, Miaomiao Zhang, Peilai Liu, Wenwei Qian
Orthopaedic Surgery.2024; 16(12): 3098. CrossRef - Age and sex differences in coronal lower extremity alignment in a healthy Asian population
Doohyun Hwang, Min Wook Choi, Seong-Hwan Kim, Hyuk-Soo Han, Chong Bum Chang, Myung Chul Lee, Na-Kyoung Lee, Du Hyun Ro
The Knee.2023; 45: 198. CrossRef - Do Individualized Patient-Specific Situations Predict the Progression Rate and Fate of Knee Osteoarthritis? Prediction of Knee Osteoarthritis
Hyun Jin Yoo, Ho Won Jeong, Sung Bae Park, Seung Jae Shim, Hee Seung Nam, Yong Seuk Lee
Journal of Clinical Medicine.2023; 12(3): 1204. CrossRef - Associations between long-term exercise participation and lower limb joint and whole-bone geometry in young and older adults
Matteo Scorcelletti, Jochen Zange, Jonas Böcker, Wolfram Sies, Patrick Lau, Uwe Mittag, Neil D. Reeves, Alex Ireland, Jörn Rittweger
Frontiers in Physiology.2023;[Epub] CrossRef - Chronological Changes in Sagittal Femoral Bowing after Primary Cementless Total Hip Arthroplasty: A Comparative 3D CT Study
Francesco Pardo, Antonino Amedeo La Mattina, Emanuele Diquattro, Stefano Lucchini, Marco Viceconti, Andrea Minerba, Francesco Castagnini, Francesco Traina
Journal of Personalized Medicine.2023; 13(12): 1704. CrossRef - Femoral bowing in the Arab population: A cross-sectional study and literature review
Randa Elsheikh, Abdelrahman M. Makram, Omar Mohamed Makram, Ahmed Tamer, Mahmoud A. Hafez
Translational Research in Anatomy.2022; 26: 100160. CrossRef - Radiographic hand osteoarthritis in women farmers: characteristics and risk factors
Bohyun Sim, Jaehoo Lee, Chul Gab Lee, Hansoo Song
Annals of Occupational and Environmental Medicine.2022;[Epub] CrossRef - Work-related factors of knee osteoarthritis in Korean farmers: a cross-sectional study
Han Soo Song, Dong Hwi Kim, Gwang Chul Lee, Kweon Young Kim, So Yeon Ryu, Chul Gab Lee
Annals of Occupational and Environmental Medicine.2020;[Epub] CrossRef
- Figure
- Related articles
-
- Factors affecting heat-related illness symptoms among school food service workers: a cross-sectional study in Korea
- Sex difference in musculoskeletal disabilities among Korean fishers: a cross-sectional study
- Burnout, stress, and their correlates among bank employees of South India: a cross-sectional study
- Impact of neck posture and insulating stick use on neck disability in Korean line workers: a cross-sectional study
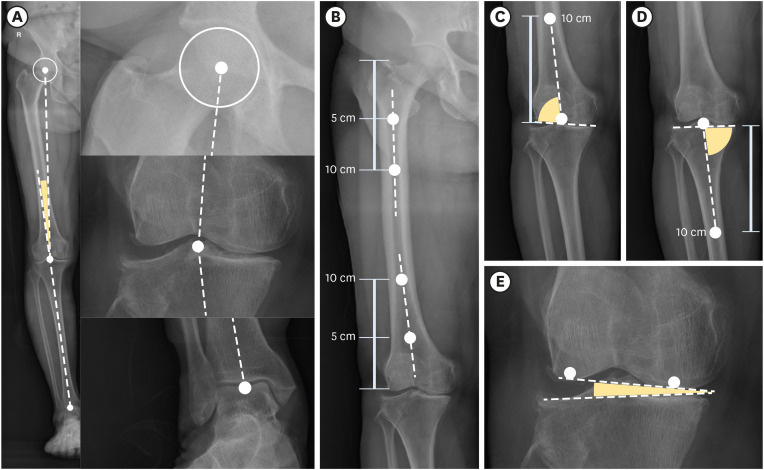
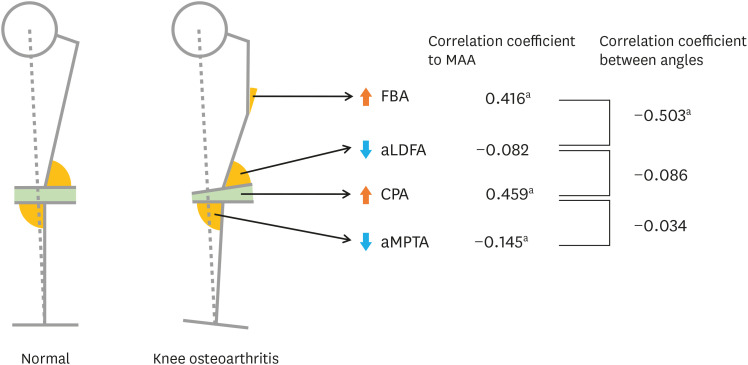
Fig. 1
Fig. 2
| Variables | No. | Minimum | Maximum | Mean | SD | Skewness | |
|---|---|---|---|---|---|---|---|
| Age (years) | 264 | 40.00 | 77.00 | 57.27 | 8.19 | 0.238 | |
| Height (cm) | 264 | 125.10 | 189.20 | 155.57 | 6.36 | 0.064 | |
| Weight (kg) | 264 | 36.00 | 84.10 | 59.01 | 9.08 | 0.270 | |
| BMI (kg/m2) | 264 | 16.64 | 33.49 | 24.34 | 3.15 | 0.363 | |
| BMD(f) (g/cm2) | 264 | 0.45 | 1.31 | 0.92 | 0.14 | −0.099 | |
| Career (years) | 264 | 0.50 | 60.00 | 27.05 | 15.21 | 0.143 | |
| CSWT (1,000 hours) | 264 | 0.00 | 94.08 | 25.76 | 25.03 | 0.893 | |
| Quartile 1 | 43 | 0.00 | 1.41 | 0.41 | |||
| Quartile 2 | 63 | 1.54 | 11.48 | 5.46 | |||
| Quartile 3 | 78 | 11.95 | 34.50 | 22.76 | |||
| Quartile 4 | 80 | 34.78 | 94.08 | 58.29 | |||
| CLWT (1,000 hours) | 264 | 0.00 | 94.08 | 16.74 | 21.23 | 1.495 | |
| Quartile 1 | 75 | 0.00 | 1.04 | 0.27 | |||
| Quartile 2 | 55 | 1.07 | 7.20 | 3.29 | |||
| Quartile 3 | 68 | 7.31 | 25.62 | 14.79 | |||
| Quartile 4 | 66 | 27.32 | 94.08 | 48.67 | |||
| Variables | KL grade | No. | Mean (degree) | SD | p-value | Homogenous subset by post hoc analysis |
|---|---|---|---|---|---|---|
| MAA | Grade 0–1 | 328 | 2.52 | 2.72 | < 0.001 | 1 |
| Grade 2 | 143 | 2.95 | 3.11 | 1 | ||
| Grade 3–4 | 57 | 8.15 | 5.06 | 2 | ||
| Total | 528 | 3.25 | 3.59 | |||
| FBA | Grade 0–1 | 328 | 1.05 | 4.60 | < 0.001 | 1 |
| Grade 2 | 143 | 1.66 | 4.11 | 1 | ||
| Grade 3–4 | 57 | 5.97 | 5.02 | 2 | ||
| Total | 528 | 1.75 | 4.75 | |||
| aLDFA | Grade 0–1 | 328 | 85.13 | 2.83 | < 0.001 | 1 |
| Grade 2 | 143 | 84.49 | 3.14 | 1 | ||
| Grade 3–4 | 57 | 82.72 | 2.77 | 2 | ||
| Total | 528 | 84.69 | 3.00 | |||
| CPA | Grade 0–1 | 328 | 1.43 | 1.02 | < 0.001 | 1 |
| Grade 2 | 143 | 1.86 | 1.26 | 2 | ||
| Grade 3–4 | 57 | 3.42 | 2.09 | 3 | ||
| Total | 528 | 1.76 | 1.38 | |||
| aMPTA | Grade 0–1 | 328 | 92.79 | 4.84 | 0.034 | 1 |
| Grade 2 | 143 | 93.07 | 1.78 | 1/2 | ||
| Grade 3–4 | 57 | 94.31 | 3.09 | 2 | ||
| Total | 528 | 93.03 | 4.08 |
| Variables | Age | Career | CSWT | CLWT | BMI | BMD(f) | MAA | FBA | aLDFA | CPA |
|---|---|---|---|---|---|---|---|---|---|---|
| Career | 0.595b | |||||||||
| CSWT | 0.307b | 0.543b | ||||||||
| CLWT | 0.021 | 0.251b | 0.555b | |||||||
| BMI | −0.144b | −0.062 | −0.013 | 0.055 | ||||||
| BMD(f) | −0.464b | −0.275b | −0.205b | −0.016 | 0.397b | |||||
| MAA | 0.348b | 0.362b | 0.163b | 0.055 | 0.132b | −0.161b | ||||
| FBA | 0.424b | 0.419b | 0.207b | 0.020 | 0.021 | −0.279b | 0.416b | |||
| aLDFA | −0.372b | −0.280b | −0.192b | −0.034 | −0.110 | 0.184b | −0.082 | −0.503b | ||
| CPA | 0.269b | 0.276b | 0.175b | 0.051 | 0.063 | −0.100a | 0.459b | 0.171b | −0.086a | |
| aMPTA | 0.033 | 0.041 | 0.027 | 0.005 | 0.077 | −0.045 | −0.145b | −0.020 | 0.128b | 0.034 |
| Model | Variables | Coefficients | p-value | R2 | ||
|---|---|---|---|---|---|---|
| β (95% CI) | β* | |||||
| 1 | Intercept | 16.49 (5.11, 27.87) | 0.005 | 0.26 | ||
| Internal factors | Age (year) | 0.16 (0.10, 0.21) | 0.27 | < 0.001 | ||
| Height (cm) | −0.16 (−0.22, −0.10) | −0.21 | < 0.001 | |||
| BMI (kg/m2) | 0.18 (0.06, 0.30) | 0.12 | 0.005 | |||
| BMD(f) (g/cm2) | −3.93 (−6.98, −0.87) | −0.12 | 0.012 | |||
| External factors | CSWT (4Q) | 0.58 (0.18, 0.97) | 0.13 | 0.005 | ||
| CLWT (4Q) | −0.46 (−0.81, −0.10) | −0.11 | 0.012 | |||
| 2 | Intercept | 15.73 (4.63, 26.83) | 0.006 | 0.28 | ||
| Internal factors | Age (year) | 0.10 (0.04, 0.16) | 0.17 | 0.001 | ||
| Height (cm) | −0.14 (−0.20, −0.08) | −0.19 | < 0.001 | |||
| BMI (kg/m2) | 0.18 (0.06, 0.30) | 0.12 | 0.004 | |||
| BMD(f) (g/cm2) | −4.22 (−7.22, −1.23) | −0.13 | 0.006 | |||
| External factors | Career (year) | 0.07 (0.04, 0.10) | 0.23 | < 0.001 | ||
SD: standard deviation; BMI: body mass index; BMD(f): femur bone mineral density; Career: the length of agricultural career; CSWT: cumulative squatting working time; CLWT: cumulative heavy lifting working time.
The
KL: Kellgren-Lawrence; SD: standard deviation; MAA: mechanical axis angle; FBA: femoral bowing angle; aLDFA: anatomical lateral distal femoral angle; CPA: condylar plateau angle; aMPTA: anatomical medial tibial angle.
Career: the length of agricultural career; CSWT: cumulative squatting working time; CLWT: cumulative heavy lifting working time; BMI: body mass index; BMD(f): femur bone mineral density; MAA: mechanical axis angle; FBA: femoral bowing angle; aLDFA: anatomical lateral distal femoral angle; CPA: condylar plateau angle; aMPTA: anatomical medial tibial angle.
a
Model 1 variables: age, height, BMI, BMD(f), CSWT, CLWT; model 2 variables: age, height, BMI, BMD(f), career.
β: non-standardized coefficient beta; CI: confidence interval; β*: Standardized coefficient beta; BMI: body mass index; BMD(f): femur bone mineral density; CSWT: cumulative squatting working time; CLWT: cumulative heavy lifting working time; Career: the length of agricultural career.
 KSOEM
KSOEM

 Cite
Cite

