Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 35; 2023 > Article
- Original Article Association between ambient particulate matter levels and hypertension: results from the Korean Genome and Epidemiology Study
-
Sewhan Na1,2
 , Jong-Tae Park1,3,4
, Jong-Tae Park1,3,4 , Seungbeom Kim1
, Seungbeom Kim1 , Jinwoo Han1
, Jinwoo Han1 , Saemi Jung5
, Saemi Jung5 , Kyeongmin Kwak1,3,4
, Kyeongmin Kwak1,3,4
-
Annals of Occupational and Environmental Medicine 2023;35:e51.
DOI: https://doi.org/10.35371/aoem.2023.35.e51
Published online: December 4, 2023
1Department of Occupational and Environmental Medicine, Korea University Ansan Hospital, Ansan, Korea.
2Department of Environmental Health Sciences, Seoul National University Graduate School of Public Health, Seoul, Korea.
3Department of Occupational and Environmental Medicine, Korea University College of Medicine, Seoul, Korea.
4Department of Environmental and Occupational Health, Korea University Graduate School of Public Health, Seoul, Korea.
5Department of Occupational and Environmental Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea.
- Correspondence: Kyeongmin Kwak. Department of Occupational and Environmental Medicine, Korea University Ansan Hospital, 123 Jeokgeum-ro, Danwon-gu, Ansan 15355, Korea. pathfinder81@korea.ac.kr
Copyright © 2023 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background Recently, there has been increasing worldwide concern about outdoor air pollution, especially particulate matter (PM), which has been extensively researched for its harmful effects on the respiratory system. However, sufficient research on its effects on cardiovascular diseases, such as hypertension, remains lacking. In this study, we examine the associations between PM levels and hypertension and hypothesize that higher PM concentrations are associated with elevated blood pressure.
-
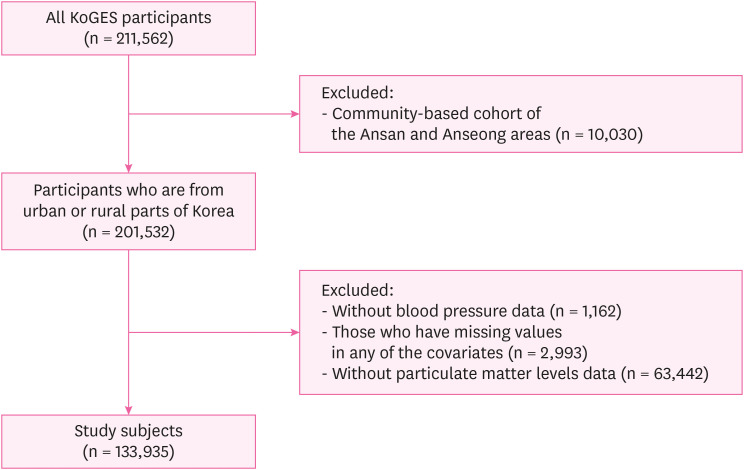
Methods A total of 133,935 adults aged ≥ 40 years who participated in the Korean Genome and Epidemiology Study were analyzed. Multiple linear regression analyses were conducted to investigate the short- (1–14 days), medium- (1 and 3 months), and long-term (1 and 2 years) impacts of PM on blood pressure. Logistic regression analyses were conducted to evaluate the medium- and long-term effects of PM on blood pressure elevation after adjusting for sex, age, body mass index, health-related lifestyle behaviors, and geographic areas.
-
Results Using multiple linear regression analyses, both crude and adjusted models generated positive estimates, indicating an association with increased blood pressure, with all results being statistically significant, with the exception of PM levels over the long-term period (1 and 2 years) in non-hypertensive participants. In the logistic regression analyses on non-hypertensive participants, moderate PM10 (particulate matter with diameters < 10 μm) and PM2.5 (particulate matter with diameters < 2.5 μm) levels over the long-term period and all high PM10 and PM2.5 levels were statistically significant after adjusting for various covariates. Notably, high PM2.5 levels of the 1 year exhibited the highest odds ratio of 1.23 (95% confidence interval: 1.19–1.28) after adjustment.
-
Conclusions These findings suggest that both short- and long-term exposure to PM is associated with blood pressure elevation.
BACKGROUND
METHODS
RESULTS
General characteristics of the subjects
Levels of PM10 regarding characteristics of the subjects
Levels of PM2.5 regarding characteristics of the subjects
Crude and adjusted association between PM concentrations and MAP in the hypertensive and non-hypertensive subjects
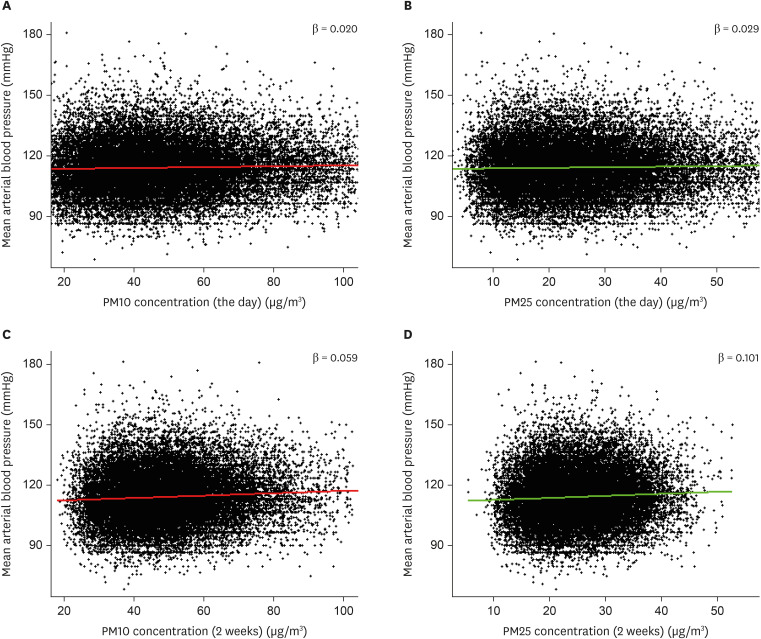
Association between PM concentrations and MAP by scatter plot. Regression lines are displayed. (A, B) Average PM10 and PM2.5 levels of the health examination day and MAP. (C, D) Average PM10 and PM2.5 levels for 2 weeks and MAP.
Crude and adjusted ORs for hypertension of subjects without prior diagnosis in moderate/high PM level groups
DISCUSSION
CONCLUSIONS
Acknowledgements
Abbreviations
ANOVA
BMI
BP
CI
COPD
DALY
DBP
GM
IRB
KoGES
MAP
OR
PM
PM10
PM2.5
SBP
-
Funding: This research was supported by the Inha University Hospital’s Environmental Health Center for Training Environmental Medicine Professionals funded by the Ministry of Environment, Republic of Korea (2023).
-
Competing interests: The authors declare that they have no competing interests.
-
Author contributions:
NOTES
SUPPLEMENTARY MATERIAL
Supplementary Table 1
- 1. Brook RD, Newby DE, Rajagopalan S. The global threat of outdoor ambient air pollution to cardiovascular health: time for intervention. JAMA Cardiol 2017;2(4):353–354. 28241232.ArticlePubMed
- 2. Mukherjee A, Agrawal M. A global perspective of fine particulate matter pollution and its health effects. Rev Environ Contam Toxicol 2018;244:5–51. 28361472.ArticlePubMed
- 3. Kyung SY, Jeong SH. Particulate-matter related respiratory diseases. Tuberc Respir Dis (Seoul) 2020;83(2):116–121. 32185911.ArticlePubMedPMCPDF
- 4. Brook RD. Why physicians who treat hypertension should know more about air pollution. J Clin Hypertens (Greenwich) 2007;9(8):629–635. 17673885.ArticlePubMedPMC
- 5. Sanidas E, Papadopoulos DP, Grassos H, Velliou M, Tsioufis K, Barbetseas J, et al. Air pollution and arterial hypertension. A new risk factor is in the air. J Am Soc Hypertens 2017;11(11):709–715. 28989071.ArticlePubMed
- 6. Vaduganathan M, Mensah GA, Turco JV, Fuster V, Roth GA. The global burden of cardiovascular diseases and risk: a compass for future health. J Am Coll Cardiol 2022;80(25):2361–2371. 36368511.PubMed
- 7. Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol 2020;16(4):223–237. 32024986.ArticlePubMedPMCPDF
- 8. Wang W, Lee ET, Fabsitz RR, Devereux R, Best L, Welty TK, et al. A longitudinal study of hypertension risk factors and their relation to cardiovascular disease: the Strong Heart Study. Hypertension 2006;47(3):403–409. 16432042.ArticlePubMed
- 9. Meissner A. Hypertension and the brain: a risk factor for more than heart disease. Cerebrovasc Dis 2016;42(3-4):255–262. 27173592.ArticlePubMedPDF
- 10. Kannan A, Janardhanan R. Hypertension as a risk factor for heart failure. Curr Hypertens Rep 2014;16(7):447. 24792121.ArticlePubMedPDF
- 11. Chen H, Burnett RT, Kwong JC, Villeneuve PJ, Goldberg MS, Brook RD, et al. Spatial association between ambient fine particulate matter and incident hypertension. Circulation 2014;129(5):562–569. 24190962.ArticlePubMed
- 12. Doulatram-Gamgaram V, Valdés S, Maldonado-Araque C, Lago-Sampedro A, Badía-Guillén R, García-Escobar E, et al. Association between long term exposure to particulate matter and incident hypertension in Spain. Sci Rep 2021;11(1):19702. 34611240.ArticlePubMedPMCPDF
- 13. Huang K, Yang X, Liang F, Liu F, Li J, Xiao Q, et al. Long-term exposure to fine particulate matter and hypertension incidence in China. Hypertension 2019;73(6):1195–1201. 31067193.ArticlePubMedPMC
- 14. Dominici F, Greenstone M, Sunstein CR. Science and regulation. Particulate matter matters. Science 2014;344(6181):257–259. 24744361.ArticlePubMedPMC
- 15. Huang YC. Outdoor air pollution: a global perspective. J Occup Environ Med 2014;56(Suppl 10):S3–S7. 25285972.PubMed
- 16. Kim KH, Kabir E, Kabir S. A review on the human health impact of airborne particulate matter. Environ Int 2015;74:136–143. 25454230.ArticlePubMed
- 17. Hopke PK, Dai Q, Li L, Feng Y. Global review of recent source apportionments for airborne particulate matter. Sci Total Environ 2020;740:140091. 32559544.ArticlePubMedPMC
- 18. Conklin DJ. Beware the air! Why particulate matter matters. Circ Res 2011;108(6):644–647. 21415405.PubMedPMC
- 19. Myong JP. Health effects of particulate matter. Korean J Med 2016;91(2):106–113.ArticlePDF
- 20. Huang W, Wang L, Li J, Liu M, Xu H, Liu S, et al. Short-term blood pressure responses to ambient fine particulate matter exposures at the extremes of global air pollution concentrations. Am J Hypertens 2018;31(5):590–599. 29409056.ArticlePubMedPMCPDF
- 21. Zhao M, Xu Z, Guo Q, Gan Y, Wang Q, Liu JA. Association between long-term exposure to PM2.5 and hypertension: a systematic review and meta-analysis of observational studies. Environ Res 2022;204(Pt D):112352. 34762927.ArticlePubMed
- 22. Kim Y, Han BG. KoGES group. Cohort profile: the Korean Genome and Epidemiology Study (KoGES) consortium. Int J Epidemiol 2017;46(4):1350. 28938752.ArticlePubMedPMC
- 23. Baek TH, Lee HY, Lim NK, Park HY. Gender differences in the association between socioeconomic status and hypertension incidence: the Korean Genome and Epidemiology Study (KoGES). BMC Public Health 2015;15(1):852. 26336067.ArticlePubMedPMCPDF
- 24. Woo HD, Song DS, Choi SH, Park JK, Lee K, Yun HY, et al. Integrated dataset of the Korean Genome and Epidemiology Study cohort with estimated air pollution data. Epidemiol Health 2022;44:e2022071. 36108673.ArticlePubMedPMCPDF
- 25. Kim JH, Woo HD, Choi S, Song DS, Lee JH, Lee K. Long-term effects of ambient particulate and gaseous pollutants on serum high-sensitivity C-reactive protein levels: a cross-sectional study using KoGES-HEXA data. Int J Environ Res Public Health 2022;19(18):11585. 36141854.ArticlePubMedPMC
- 26. Hwang MJ, Sung J, Yoon M, Kim JH, Yun HY, Choi DR, et al. Establishment of the Korea National Health and Nutrition Examination Survey air pollution study dataset for the researchers on the health impact of ambient air pollution. Epidemiol Health 2021;43:e2021015. 33561914.ArticlePubMedPMC
- 27. Jung H, Lee G, Lim K, Shin S. Association of milk consumption with management and incidence of hypertension among South Korean adults: a prospective analysis of the health examinees study cohort. Nutr Metab Cardiovasc Dis 2022;32(11):2515–2525. 36175315.ArticlePubMed
- 28. Ioannidis JP. The proposal to lower p value thresholds to .005. JAMA 2018;319(14):1429–1430. 29566133.ArticlePubMed
- 29. Lee JJ, Kim JH, Song DS, Lee K. Effect of short- to long-term exposure to ambient particulate matter on cognitive function in a cohort of middle-aged and older adults: KoGES. Int J Environ Res Public Health 2022;19(16):9913. 36011565.ArticlePubMedPMC
- 30. Weaver AM, Wang Y, Wellenius GA, Bidulescu A, Sims M, Vaidyanathan A, et al. Long-term air pollution and blood pressure in an African American cohort: the Jackson Heart study. Am J Prev Med 2021;60(3):397–405. 33478866.ArticlePubMedPMC
- 31. Arku RE, Brauer M, Ahmed SH, AlHabib KF, Avezum Á, Bo J, et al. Long-term exposure to outdoor and household air pollution and blood pressure in the Prospective Urban and Rural Epidemiological (PURE) study. Environ Pollut 2020;262:114197. 32146361.ArticlePubMedPMC
- 32. Prabhakaran D, Mandal S, Krishna B, Magsumbol M, Singh K, Tandon N, et al. Exposure to particulate matter is associated with elevated blood pressure and incident hypertension in urban India. Hypertension 2020;76(4):1289–1298. 32816598.ArticlePubMedPMC
- 33. Wu QZ, Li S, Yang BY, Bloom M, Shi Z, Knibbs L, et al. Ambient airborne particulates of diameter ≤1 μm, a leading contributor to the association between ambient airborne particulates of diameter ≤2.5 μm and children’s blood pressure. Hypertension 2020;75(2):347–355. 31838909.ArticlePubMed
- 34. Liu C, Fuertes E, Tiesler CM, Birk M, Babisch W, Bauer CP, et al. The associations between traffic-related air pollution and noise with blood pressure in children: results from the GINIplus and LISAplus studies. Int J Hyg Environ Health 2014;217(4-5):499–505. 24183515.ArticlePubMed
- 35. Yang BY, Qian Z, Howard SW, Vaughn MG, Fan SJ, Liu KK, et al. Global association between ambient air pollution and blood pressure: a systematic review and meta-analysis. Environ Pollut 2018;235:576–588. 29331891.ArticlePubMed
- 36. Niu Z, Duan Z, Yu H, Xue L, Liu F, Yu D, et al. Association between long-term exposure to ambient particulate matter and blood pressure, hypertension: an updated systematic review and meta-analysis. Int J Environ Health Res 2023;33(3):268–283. 34983264.ArticlePubMed
- 37. Chuang KJ, Yan YH, Chiu SY, Cheng TJ. Long-term air pollution exposure and risk factors for cardiovascular diseases among the elderly in Taiwan. Occup Environ Med 2011;68(1):64–68. 20833756.ArticlePubMed
- 38. Li N, Chen G, Liu F, Mao S, Liu Y, Liu S, et al. Associations between long-term exposure to air pollution and blood pressure and effect modifications by behavioral factors. Environ Res 2020;182:109109. 32069739.ArticlePubMedPMC
- 39. Zhang Z, Dong B, Li S, Chen G, Yang Z, Dong Y, et al. Exposure to ambient particulate matter air pollution, blood pressure and hypertension in children and adolescents: a national cross-sectional study in China. Environ Int 2019;128:103–108. 31035113.ArticlePubMed
- 40. Huang W, Wang G, Lu SE, Kipen H, Wang Y, Hu M, et al. Inflammatory and oxidative stress responses of healthy young adults to changes in air quality during the Beijing Olympics. Am J Respir Crit Care Med 2012;186(11):1150–1159. 22936356.ArticlePubMedPMC
- 41. Jiang S, Bo L, Gong C, Du X, Kan H, Xie Y, et al. Traffic-related air pollution is associated with cardio-metabolic biomarkers in general residents. Int Arch Occup Environ Health 2016;89(6):911–921. 27084335.ArticlePubMedPDF
- 42. Zhang Q, Du X, Li H, Jiang Y, Zhu X, Zhang Y, et al. Cardiovascular effects of traffic-related air pollution: a multi-omics analysis from a randomized, crossover trial. J Hazard Mater 2022;435:129031. 35523096.ArticlePubMed
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Long-term joint exposure of outdoor air pollutants and impaired kidney function in Korean adults: A mixture analysis based on a nationwide sample (2007–2019)
Seong-Uk Baek, Jin-Ha Yoon
Environmental Toxicology and Pharmacology.2025; 116: 104712. CrossRef - Long-term exposure to ambient air pollutant mixture and metabolic obesity phenotypes: Results from a nationwide Korean study (2007–2019)
Seong-Uk Baek, Jin-Ha Yoon
Journal of Exposure Science & Environmental Epidemiology.2025;[Epub] CrossRef - Association between exposure to ambient particulate matter and high sensitivity C-reactive protein: A nationwide study in South Korea, 2015–2018
Seong-Uk Baek, Jong-Uk Won, Yu-Min Lee, Jin-Ha Yoon
Atmospheric Environment.2024; 339: 120856. CrossRef
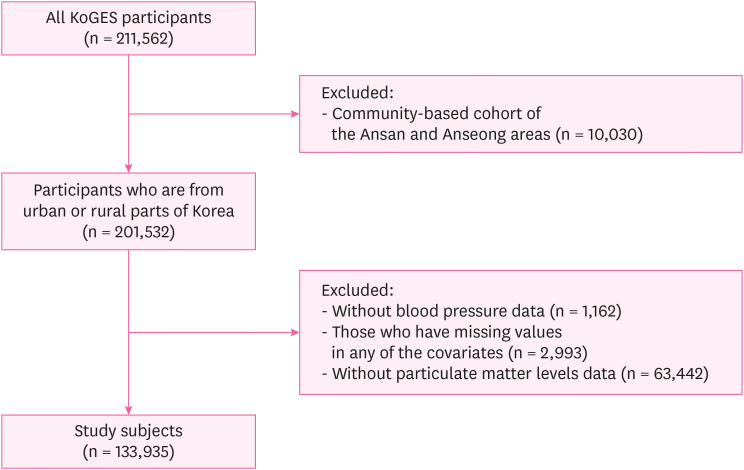
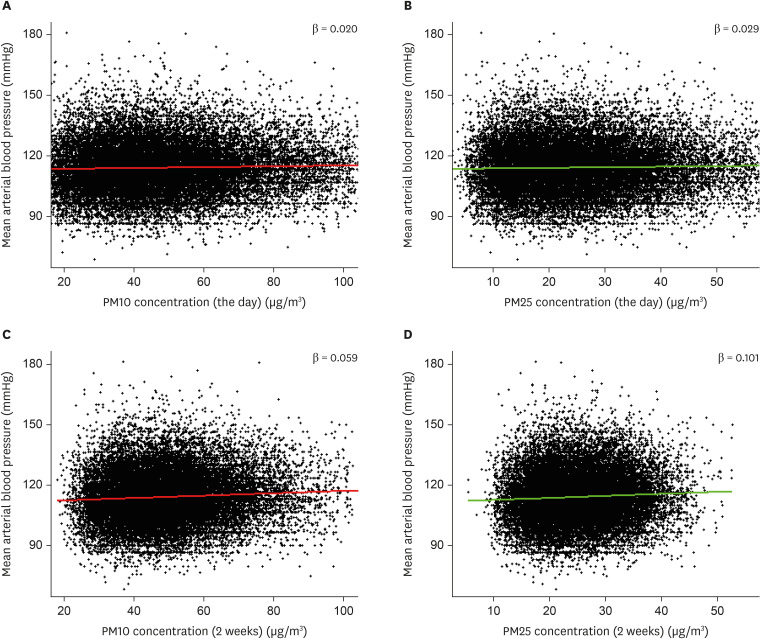
Fig. 1
Fig. 2
| Characteristics | Category | All (n = 133,935) | With HTN (n = 44,936) | Without HTN (n = 88,999) | |
|---|---|---|---|---|---|
| Sex | Male | 47,237 (35.3) | 17,728 (39.5) | 29,509 (33.2) | < 0.001a*** |
| Female | 86,698 (64.7) | 27,208 (60.5) | 59,490 (66.8) | ||
| Age (years) | 40–49 | 45,626 (34.1) | 9,619 (21.4) | 36,007 (40.5) | < 0.001b*** |
| 50–59 | 51,936 (38.8) | 17,405 (38.7) | 34,531 (38.8) | ||
| ≥ 60 | 36,373 (27.2) | 17,912 (39.9) | 18,461 (20.7) | ||
| BMI (kg/m2) | ≤ 23 | 52,801 (39.4) | 13,272 (29.5) | 39,529 (44.4) | < 0.001b*** |
| 23–25 | 36,760 (27.4) | 11,907 (26.5) | 24,853 (27.9) | ||
| ≥ 25 | 44,374 (33.1) | 19,757 (44.0) | 24,617 (27.7) | ||
| Family history | Yes | 94,986 (70.9) | 28,406 (63.2) | 66,580 (74.8) | < 0.001a*** |
| No | 38,949 (29.1) | 16,530 (36.8) | 22,419 (25.2) | ||
| Smoking | Never | 96,447 (72.0) | 31,254 (69.6) | 65,193 (73.3) | < 0.001a*** |
| Ex-smoker | 20,367 (15.2) | 8,178 (18.2) | 12,189 (13.7) | ||
| Current | 17,121 (12.8) | 5,504 (12.2) | 11,617 (13.1) | ||
| Drinking | Never | 68,157 (50.9) | 22,734 (50.6) | 45,423 (51.0) | < 0.001a*** |
| Ex-drinker | 5,247 (3.9) | 2,070 (4.6) | 3,177 (3.6) | ||
| Current | 60,531 (45.2) | 20,132 (44.8) | 40,399 (45.4) | ||
| Exercise | Yes | 65,677 (49.0) | 21,544 (47.9) | 44,133 (49.6) | < 0.001a*** |
| No | 68,258 (51.0) | 23,392 (52.1) | 44,866 (50.4) | ||
| Geographical area | Urban | 123,827 (92.5) | 40,355 (89.8) | 83,472 (93.8) | < 0.001a*** |
| Rural | 10,108 (7.5) | 4,581 (10.2) | 5,527 (6.2) |
| Characteristics | Category | Geometric mean (μg/m3) | |||
|---|---|---|---|---|---|
| The day | 1 week | 3 months | 2 years | ||
| All subjects | 45.18 (45.08–45.29) | 46.91 (46.83–46.99) | 48.95 (48.90–49.00) | 52.81 (52.77–52.84) | |
| Sex | Male | 45.29 (45.11–45.47) | 47.09 (46.95–47.22) | 48.88 (48.79–48.97) | 52.91 (52.86–52.97) |
| Female | 45.13 (45.00–45.26) | 46.81 (46.71–46.91) | 48.99 (48.92–49.06) | 52.75 (52.70–52.79) | |
| < 0.001*** | < 0.001*** | < 0.001*** | < 0.001*** | ||
| Age (years) | 40–49 | 45.36 (45.18–45.54) | 47.17 (47.03–47.31) | 48.72 (48.63–48.81) | 53.19 (53.14–53.25) |
| 50–59 | 45.18 (45.01–45.36) | 46.82 (46.69–46.95) | 48.88 (48.80–48.97) | 52.70 (52.64–52.75) | |
| ≥ 60 | 44.97 (44.77–45.17) | 46.71 (46.56–46.87) | 49.34 (49.24–49.44) | 52.48 (52.41–52.54) | |
| 0.001** | < 0.001*** | < 0.001*** | < 0.001*** | ||
| BMI | ≤ 23 | 44.84 (44.68–45.01) | 46.50 (46.38–46.63) | 48.62 (48.54–48.71) | 52.63 (52.58–52.68) |
| 23–25 | 45.12 (44.92–45.32) | 46.82 (46.66–46.97) | 48.98 (48.87–49.08) | 52.77 (52.71–52.83) | |
| ≥ 25 | 45.65 (45.46–45.84) | 47.47 (47.33–47.62) | 49.32 (49.23–49.41) | 53.05 (52.99–53.10) | |
| < 0.001*** | < 0.001*** | < 0.001*** | < 0.001*** | ||
| Family history | Yes | 45.42 (45.22–45.62) | 47.09 (46.94–47.24) | 48.86 (48.76–48.96) | 52.88 (52.82–52.95) |
| No | 45.09 (44.96–45.21) | 46.84 (46.74–46.93) | 48.99 (48.92–49.05) | 52.77 (52.73–52.81) | |
| < 0.001*** | < 0.001*** | < 0.001*** | < 0.001*** | ||
| Smoking | Never | 45.18 (45.06–45.31) | 46.87 (46.77–46.97) | 49.00 (48.94–49.06) | 52.80 (52.76–52.84) |
| Ex-smoker | 45.31 (45.04–45.59) | 46.98 (46.77–47.18) | 48.83 (48.70–48.97) | 52.67 (52.59–52.76) | |
| Current | 45.06 (44.76–45.36) | 47.05 (46.82–47.28) | 48.82 (48.67–48.97) | 53.00 (52.90–53.09) | |
| 0.604 | 0.194 | 0.006** | < 0.001*** | ||
| Drinking | Never | 45.09 (44.94–45.23) | 46.78 (46.67–46.90) | 48.96 (48.89–49.04) | 52.71 (52.66–52.76) |
| Ex-smoker | 45.14 (44.61–45.67) | 47.25 (46.86–47.65) | 49.31 (49.05–49.57) | 52.65 (52.48–52.82) | |
| Current | 45.30 (45.14–45.46) | 47.02 (46.90–47.14) | 48.90 (48.82–48.98) | 52.93 (52.88–52.98) | |
| 0.236 | 0.035* | 0.016* | < 0.001*** | ||
| Exercise | Yes | 45.51 (45.36–45.66) | 47.08 (46.96–47.19) | 49.04 (48.97–49.12) | 52.93 (52.88–52.98) |
| No | 44.85 (44.69–45.00) | 46.74 (46.62–46.85) | 48.85 (48.78–48.93) | 52.68 (52.63–52.73) | |
| < 0.001*** | < 0.001*** | < 0.001*** | < 0.001*** | ||
| Geographical area | Urban | 45.36 (45.25–45.47) | 47.04 (46.96–47.13) | 48.75 (48.70–48.81) | 52.70 (52.66–52.73) |
| Rural | 43.14 (42.75–43.53) | 45.30 (44.99–45.62) | 51.41 (51.23–51.59) | 54.18 (54.05–54.30) | |
| < 0.001*** | < 0.001*** | < 0.001*** | < 0.001*** | ||
| Characteristics | Category | Geometric mean (μg/m3) | |||
|---|---|---|---|---|---|
| The day | 1 week | 3 months | 2 years | ||
| All subjects | 22.43 (22.37–22.48) | 23.56 (23.52–23.60) | 24.41 (24.39–24.44) | 25.95 (25.94–25.97) | |
| Sex | Male | 22.43 (22.33–22.53) | 23.58 (23.51–23.65) | 24.33 (24.28–24.37) | 25.91 (25.88–25.94) |
| Female | 22.43 (22.35–22.50) | 23.55 (23.50–23.60) | 24.46 (24.43–24.49) | 25.98 (25.96–26.00) | |
| < 0.001*** | < 0.001*** | < 0.001*** | < 0.001*** | ||
| Age (years) | 40–49 | 22.41 (22.31–22.51) | 23.59 (23.52–23.66) | 24.25 (24.21–24.30) | 26.00 (25.97–26.02) |
| 50–59 | 22.45 (22.36–22.55) | 23.58 (23.51–23.65) | 24.43 (24.39–24.47) | 25.94 (25.91–25.96) | |
| ≥ 60 | 22.41 (22.30–22.52) | 23.50 (23.42–23.58) | 24.58 (24.54–24.63) | 25.92 (25.89–25.95) | |
| 0.661 | 0.031* | < 0.001*** | < 0.001*** | ||
| BMI | ≤ 23 | 22.28 (22.19–22.37) | 23.38 (23.31–23.44) | 24.27 (24.23–24.31) | 25.89 (25.86–25.91) |
| 23–25 | 22.37 (22.26–22.48) | 23.50 (23.42–23.58) | 24.40 (24.36–24.45) | 25.92 (25.89–25.95) | |
| ≥ 25 | 22.65 (22.54–22.75) | 23.83 (23.76–23.90) | 24.59 (24.54–24.63) | 26.06 (26.03–26.09) | |
| < 0.001*** | < 0.001*** | < 0.001*** | < 0.001*** | ||
| Family history | Yes | 22.60 (22.49–22.71) | 23.73 (23.65–23.81) | 24.47 (24.42–24.51) | 25.99 (25.96–26.02) |
| No | 22.36 (22.29–22.43) | 23.49 (23.44–23.54) | 24.39 (24.36–24.42) | 25.94 (25.92–25.96) | |
| < 0.001*** | < 0.001*** | < 0.001*** | < 0.001*** | ||
| Smoking | Never | 22.43 (22.36–22.50) | 23.55 (23.50–23.60) | 24.44 (24.41–24.47) | 25.98 (25.96–26.00) |
| Ex-smoker | 22.48 (22.33–22.63) | 23.59 (23.48–23.70) | 24.32 (24.26–24.39) | 25.82 (25.78–25.87) | |
| Current | 22.33 (22.17–22.50) | 23.59 (23.47–23.71) | 24.35 (24.29–24.42) | 25.94 (25.90–25.99) | |
| 0.798 | 0.711 | 0.001** | < 0.001*** | ||
| Drinking | Never | 22.42 (22.34–22.50) | 23.55 (23.49–23.61) | 24.47 (24.43–24.50) | 25.99 (25.97–26.02) |
| Ex-smoker | 22.27 (21.99–22.56) | 23.62 (23.41–23.83) | 24.39 (24.27–24.52) | 25.86 (25.78–25.94) | |
| Current | 22.45 (22.36–22.53) | 23.57 (23.51–23.63) | 24.35 (24.31–24.39) | 25.92 (25.89–25.94) | |
| 0.202 | 0.986 | < 0.001*** | < 0.001*** | ||
| Exercise | Yes | 22.58 (22.50–22.66) | 23.64 (23.58–23.69) | 24.41 (24.38–24.45) | 25.97 (25.95–25.99) |
| No | 22.26 (22.18–22.35) | 23.48 (23.42–23.54) | 24.41 (24.38–24.45) | 25.94 (25.91–25.96) | |
| < 0.001*** | < 0.001*** | < 0.001*** | < 0.001*** | ||
| Geographical area | Urban | 22.49 (22.43–22.55) | 23.61 (23.57–23.65) | 24.25 (24.22–24.27) | 25.87 (25.85–25.88) |
| Rural | 21.64 (21.44–21.85) | 22.97 (22.82–23.13) | 26.53 (26.45–26.62) | 27.05 (26.99–27.11) | |
| < 0.001*** | < 0.001*** | < 0.001*** | < 0.001*** | ||
| PM | Period | Crude | Adjusteda | |||
|---|---|---|---|---|---|---|
| β (95% CI) | β (95% CI) | |||||
| With HTN | ||||||
| PM10 | 0 day | 0.020 (0.013–0.026) | < 0.001*** | 0.019 (0.013–0.025) | < 0.001*** | |
| 2 days | 0.029 (0.022–0.036) | < 0.001*** | 0.028 (0.021–0.035) | < 0.001*** | ||
| 1 week | 0.044 (0.035–0.053) | < 0.001*** | 0.042 (0.033–0.051) | < 0.001*** | ||
| 2 weeks | 0.059 (0.049–0.069) | < 0.001*** | 0.056 (0.046–0.067) | < 0.001*** | ||
| 1 month | 0.067 (0.055–0.079) | < 0.001*** | 0.064 (0.052–0.076) | < 0.001*** | ||
| 3 months | 0.036 (0.022–0.050) | < 0.001*** | 0.033 (0.019–0.047) | < 0.001*** | ||
| 1 year | 0.093 (0.070–0.116) | < 0.001*** | 0.084 (0.061–0.107) | < 0.001*** | ||
| 2 years | 0.108 (0.085–0.131) | < 0.001*** | 0.099 (0.076–0.122) | < 0.001*** | ||
| PM2.5 | 0 day | 0.029 (0.017–0.041) | < 0.001*** | 0.028 (0.017–0.040) | < 0.001*** | |
| 2 days | 0.045 (0.031–0.059) | < 0.001*** | 0.044 (0.030–0.058) | < 0.001*** | ||
| 1 week | 0.069 (0.051–0.087) | < 0.001*** | 0.066 (0.049–0.084) | < 0.001*** | ||
| 2 weeks | 0.101 (0.080–0.122) | < 0.001*** | 0.097 (0.076–0.118) | < 0.001*** | ||
| 1 month | 0.121 (0.096–0.146) | < 0.001*** | 0.114 (0.089–0.139) | < 0.001*** | ||
| 3 months | 0.053 (0.023–0.084) | < 0.001*** | 0.047 (0.016–0.077) | < 0.001*** | ||
| 1 year | 0.117 (0.071–0.162) | < 0.001*** | 0.107 (0.061–0.152) | < 0.001*** | ||
| 2 years | 0.164 (0.116–0.212) | < 0.001*** | 0.152 (0.104–0.200) | < 0.001*** | ||
| Without HTN | ||||||
| PM10 | 0 day | 0.013 (0.010–0.016) | < 0.001*** | 0.012 (0.009–0.015) | < 0.001*** | |
| 2 days | 0.017 (0.013–0.020) | < 0.001*** | 0.015 (0.011–0.018) | < 0.001*** | ||
| 1 week | 0.025 (0.021–0.030) | < 0.001*** | 0.023 (0.019–0.027) | < 0.001*** | ||
| 2 weeks | 0.037 (0.031–0.042) | < 0.001*** | 0.032 (0.027–0.037) | < 0.001*** | ||
| 1 month | 0.046 (0.040–0.052) | < 0.001*** | 0.039 (0.033–0.045) | < 0.001*** | ||
| 3 months | 0.021 (0.014–0.028) | < 0.001*** | 0.011 (0.005–0.018) | < 0.001*** | ||
| 1 year | −0.004 (−0.016–0.008) | 0.509 | −0.006 (−0.017–0.005) | 0.250 | ||
| 2 years | 0.009 (−0.003–0.021) | 0.125 | 0.008 (−0.003–0.019) | 0.172 | ||
| PM2.5 | 0 day | 0.024 (0.018–0.030) | < 0.001*** | 0.022 (0.016–0.027) | < 0.001*** | |
| 2 days | 0.030 (0.023–0.038) | < 0.001*** | 0.026 (0.020–0.033) | < 0.001*** | ||
| 1 week | 0.048 (0.039–0.057) | < 0.001*** | 0.043 (0.035–0.051) | < 0.001*** | ||
| 2 weeks | 0.070 (0.060–0.081) | < 0.001*** | 0.062 (0.052–0.072) | < 0.001*** | ||
| 1 month | 0.092 (0.079–0.104) | < 0.001*** | 0.079 (0.067–0.091) | < 0.001*** | ||
| 3 months | 0.038 (0.022–0.053) | < 0.001*** | 0.019 (0.005–0.034) | < 0.001*** | ||
| 1 year | −0.003 (−0.026–0.021) | 0.823 | −0.009 (−0.031–0.013) | 0.404 | ||
| 2 years | 0.034 (0.009–0.058) | 0.007** | 0.026 (0.003–0.049) | 0.028* | ||
| PM | Period | Crude | Adjusteda | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | |||||
| Moderate | ||||||
| PM10 | 1 month | 1.02 (0.98–1.06) | 0.275 | 1.02 (0.98–1.06) | 0.357 | |
| 3 months | 1.03 (0.99–1.07) | 0.212 | 0.99 (0.95–1.03) | 0.483 | ||
| 1 year | 1.10 (1.06–1.14) | < 0.001*** | 1.10 (1.05–1.14) | < 0.001*** | ||
| 2 years | 1.09 (1.05–1.14) | < 0.001*** | 1.10 (1.05–1.14) | < 0.001*** | ||
| PM2.5 | 1 month | 1.01 (0.98–1.06) | 0.466 | 1.01 (0.97–1.05) | 0.502 | |
| 3 months | 1.02 (0.98–1.06) | 0.464 | 0.99 (0.95–1.03) | 0.488 | ||
| 1 year | 1.07 (1.03–1.12) | < 0.001*** | 1.06 (1.02–1.11) | 0.004** | ||
| 2 years | 1.08 (1.04–1.13) | < 0.001*** | 1.08 (1.04–1.12) | < 0.001*** | ||
| High | ||||||
| PM10 | 1 month | 1.07 (1.03–1.11) | 0.001** | 1.07 (1.03–1.11) | 0.001** | |
| 3 months | 1.10 (1.06–1.15) | < 0.001*** | 1.07 (1.03–1.11) | 0.001** | ||
| 1 year | 1.21 (1.17–1.26) | < 0.001*** | 1.20 (1.16–1.25) | < 0.001*** | ||
| 2 years | 1.20 (1.15–1.25) | < 0.001*** | 1.20 (1.16–1.25) | < 0.001*** | ||
| PM2.5 | 1 month | 1.08 (1.03–1.12) | < 0.001*** | 1.07 (1.03–1.11) | < 0.001*** | |
| 3 months | 1.13 (1.08–1.17) | < 0.001*** | 1.08 (1.04–1.12) | < 0.001*** | ||
| 1 year | 1.28 (1.23–1.33) | < 0.001*** | 1.23 (1.19–1.28) | < 0.001*** | ||
| 2 years | 1.26 (1.21–1.31) | < 0.001*** | 1.22 (1.17–1.27) | < 0.001*** | ||
Values are presented as number (%)
HTN: hypertension; BMI: body mass index.
aAnalyzed by χ2 test. bAnalyzed by Cochran-Armitage trend test.
***
Values are geometric mean of average PM concentration of each duration before the test day with 95% confidence interval.
PM10: particulate matter with diameters < 10 μm; PM: particulate matter; BMI: body mass index.
aAnalyzed by Student’s
*
Values are geometric mean of average PM concentration of each duration before the test day with 95% confidence interval.
PM2.5: particulate matter with diameters < 2.5 μm; PM: particulate matter; BMI: body mass index.
aAnalyzed by Student’s
*
Analyzed by multiple linear regression model.
PM: particular matter; MAP: mean arterial blood pressure; CI: confidence interval; HTN: hypertension; PM10: particulate matter with diameters < 10 μm; PM2.5: particulate matter with diameters < 2.5 μm.
aModel was adjusted for sex, age, body mass index, family history, smoking, drinking, exercise, and geographical area.
*
Analyzed by multiple logistic regression model. Groups were determined by tertile of each metabolite (low, moderate, and high); Group with the lowest tertile set as reference group.
PM: particular matter; OR: odds ratio CI: confidence interval; PM10: particulate matter with diameters < 10 μm; PM2.5: particulate matter with diameters < 2.5 μm.
aModel was adjusted for sex, age, body mass index, family history, smoking, drinking, exercise, and geographical area.
**
 KSOEM
KSOEM

 Cite
Cite

