Abstract
-
Background
In 2019, the International Agency for Research on Cancer re-evaluated the carcinogenicity of night-shift work and reported that there is limited evidence that night-shift work is carcinogenic for the development of prostate cancer. Therefore, in 2020 and 2021, the Korean Epidemiologic Investigation Evaluation Committee concluded that 2 cases of prostate cancer were occupational diseases related to the night-shift work. Here, we report the 2 cases of prostate cancer in night-shift workers which were first concluded as occupational diseases by the Korean Epidemiologic Investigation Evaluation Committee.
-
Case presentation
Patient A: A 61-year-old man worked as a city bus driver for approximately 17 years, from 2002 to 2019, and was exposed to night-shift work during this period. In March 2017, the patient was diagnosed with high-grade prostate cancer through core-needle biopsy after experiencing stinging pain lasting for 2 months. Patient B: A 56-year-old man worked as an electrician and an automated equipment operator in a cement manufacturing plant for 35 years from 1976 to 2013 and was exposed to night-shift work during this period. In 2013, the patient was diagnosed with high-grade prostate cancer through core needle biopsy at a university hospital because of dysuria that lasted for 6 months.
-
Conclusions
The 2 workers were diagnosed with high-grade prostate cancer after working night shifts for 17 and 35 years respectively. Additionally, previous studies have reported that high-grade prostate cancer has a stronger relationship with night-shift work than low or medium-grade prostate cancer. Therefore, the Korean Epidemiologic Investigation Evaluation Committee concluded that night-shift work in these 2 patients contributed to the development of their prostate cancer.
-
Keywords: Shift work schedule; Prostatic neoplasms; Neoplasm grading; Workers’ compensation
BACKGROUND
Prostate cancer is the second most common cancer in men worldwide, while in the United States and United Kingdom, it is the most common cancer in men.
1 In Korea, the incidence of prostate cancer has more than doubled over the past 15 years due to the westernization of diet and aging of the population. Currently, it ranks fourth in the incidence of male cancer after gastric, lung, and colon and rectal cancers.
2 Major risk factors for prostate cancer include age, race, obesity, and family history.
3,4,5,6 Most prostate cancers occur in people over 50 years of age. However, prostate cancer occurring in younger people is known to be more aggressive.
7 The ‘Gleason scoring system’ is employed to grade the aggressiveness of prostate cancer histologically.
8 Unlike other methods of grading carcinomas, the Gleason scores are calculated based on tissue pattern and structure rather than the properties of each cell. The score is calculated by adding the grades of the most and second-most dominant regions of the cancer tissue. The grades range from 1 (closest to the normal gland) to 5 (no glandular pattern). The Gleason score is first divided into 5 groups according to the prognosis ascribed by the International Society of Urological Pathology in 2014.
9 The groups with higher scores have a worse prognosis.
10
The International Agency for Research on Cancer (IARC) defined night-shift work as work that includes work done during the regular sleeping hours of the general population.
11 Night-shift work is essential for 24-hour production and activity in various industries, and it is common for workers to work night-shifts in health, manufacturing, exercise, retail, and service spheres, and approximately one in 5 people worldwide work on night-shifts.
12 According to the report of 5th Korean Working Conditions Survey conducted by the Occupational Safety and Health Institute (OSHRI) in 2017, about 9.7% of workers in Korea are night-shift workers.
13 In 2019, IARC re-evaluated the carcinogenicity of night-shift work and reported that a positive association was observed between prostate cancer and night-shift work.
11 Additionally, recent meta-analysis studies have reported that night-shift work is associated with the risk of prostate cancer, particularly in a group of Asian countries.
14,15 A well-designed case-control study reported that permanent night work increased the risk of prostate cancer, and particularly the risk of prostate cancer with high Gleason scores.
16
The OSHRI of the Republic of Korea has conducted epidemiologic investigations on diseases of workers’ whose work relatedness is unclear. In the process of the epidemiologic investigation, the conclusion on work relatedness was confirmed after a meeting of the Epidemiologic Investigation Evaluation Committee (Box 1). In 2020 and 2021, the Korean Epidemiologic Investigation Evaluation Committee confirmed that 2 cases of prostate cancer with high Gleason scores were occupational diseases related to night-shift work. Here we report 2 cases of prostate cancer in night-shift workers in whom prostate cancer was first concluded to be an occupational disease in Korea.
Box 1. Role and members of the Korean Epidemiologic Investigation Evaluation Committee
In the republic of Korea, workers’ compensation is administered by the Korea Workers’ Compensation & Welfare Service (KWCWS). In the process of reviewing whether a worker has a work-related illness, if the KWCWS determines that an epidemiologic investigation is necessary, such as a rare disease or a new hazard, it will refer the case to the OSHRI.
The evaluation committee consists of no more than 30 members, including one chairperson. The members shall include experts such as occupational and environmental medicine specialists and industrial hygienists with practical experience. The chairperson is appointed by the Minister of Employment and Labor from among the members. The committee deliberates on the planning, conduct, and evaluation of epidemiologic investigations.
CASE PRESENTATION
Patient A
Patient information
The patient was a 61-year-old male.
Chief complaints
Stinging sensation in the lower urinary tract
Social history, family history and past history
He was a current smoker of 6.7 pack-years (1/3 pack *20 years) and a nondrinker. He had no family history of prostate cancer and no significant medical history.
Present illness
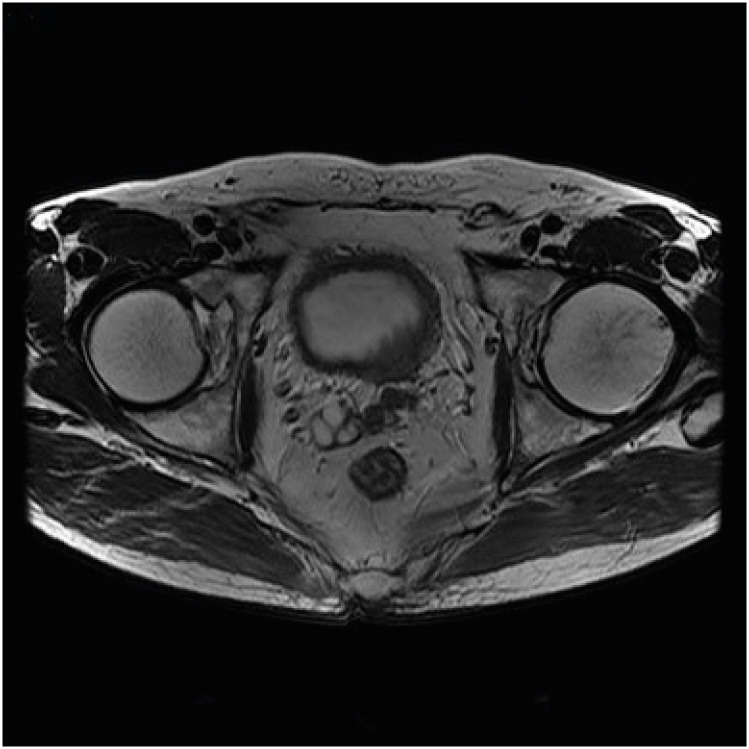
Patient A visited the urology clinic on March 16 and 21, 2017, complaining of a stinging sensation in the lower urinary tract that had lasted for 2 months. An increased prostate-specific antigen (PSA) level of 81.33 ng/mL was observed, and the patient was referred to a university hospital. A core needle biopsy of the prostate performed on March 24, 2017, followed by histopathological examination led to a diagnosis of acinar type of adenocarcinoma, with a Gleason score of 9 (4 + 5). In April 2017, he was diagnosed to have bone metastasis from the prostate cancer by a bone scan, abdominal and pelvic computed tomography (CT), and pelvic magnetic resonance imaging (MRI). Pelvic MRI images revealed prostate cancer protruding into the bladder (
Fig. 1), enlargement of iliac lymph nodes, and multiple metastatic boney lesions. In conclusion, the stage of his prostate cancer was T4N1M1b.
Fig. 1
MRI image of the pelvis of patient A. Transverse T2-weighted MRI image showing cancerous lesion in prostate gland, protruding left bladder base with multiple enhancing nodules in the pelvis.
MRI: magnetic resonance imaging.
Occupational history
Patient A held several jobs, which are summarized in
Table 1. He worked as a bus driver in 2 city bus companies for 17 years, from 2002 to 2006 and from December 2006 to February 2019. He also worked as a truck driver for 6 years from 1986 to 1991. Therefore, he has been driving buses and trucks for the past total of 23 years.
Table 1Occupational history of patient A
|
Year |
Job |
Task |
|
1976 (1 year) |
Military supplementary service |
Grass planting, waste disposal |
|
1977–1985 (10 years) |
Day laborer |
Carrying flowerpots |
|
1986–1991 (6 years) |
Cargo truck driver |
Driving 2.5-ton cargo truck |
|
1992–2001 (10 years) |
Dry-cleaning laundry |
Dry-Cleaning, Ironing, Delivery |
|
2002–2006 (5 years) |
Bus driver |
Driving bus in city bus company A |
|
2006–2019 (12 years) |
Bus driver |
Driving bus in city bus company B |
Exposure assessment
1) Assessment of night shift work
According to the interview with patient A, and work schedules provided by bus companies A and B where he had worked, the work schedule of patient A at the 2 bus companies was as follows: At city bus company A from 2002 to 2006, he worked during the morning and afternoon shifts every other week. He worked 6 days a week; and the morning and afternoon shifts were from 04:00 to 14:00, and 13:00 to 03:00 the next day, respectively. In city bus company B from December 2006 to February 2019, he worked 5 to 6 days a week and his earliest shift was 04:00 to 23:00. The shift was delayed by 10 min every day, and by the end of his tenure there, the last shift started at 07:00 and ended at 01:00. Therefore, patient A had been exposed to night-shift work for approximately 17 years. Summarized features of Patient A’s night-shift work schedule are shown in
Table 2.
Table 2Patient A’s work schedule
|
Features |
Bus company A (for 4 years) |
Bus company B (for 13 years) |
|
With or without night work |
With night work |
With night work |
|
Continuous or discontinuous |
Discontinuous |
Discontinuous |
|
Permanent or rotating |
Rotating |
Rotating |
|
Length of the shift cycle |
2 weeks |
19 weeks |
|
Duration of individual shifts |
Morning shift: 10 hours |
18–19 hours |
|
Afternoon shift: 14 hours |
|
Start and end time of individual shifts |
Morning shift: 04:00 to 14:00 |
Earliest shift: 04:00 to 23:00 |
|
Afternoon shift: 13:00 to 03:00 |
Latest shift: 07:00 to 01:00 |
|
Number of consecutive shifts |
6 shifts |
1 shift |
|
Direction of shift rotation |
Forward |
Forward |
|
Number of rest days |
2 days every week |
1–2 days every week |
|
Regularity |
Regular |
Regular |
2) Other exposures
Considering the occupational history of patient A, he may have been exposed to diesel engine exhaust (DEE) generated by buses and trucks. Although an exposure indicator for DEE has not been clearly established, elemental carbon (EC) is the most reported surrogate indicator for estimating DEE exposure.
17 According to Jung,
18 the exposure level to DEE was measured by an EC estimation every day for one week in the summer and autumn for 5 out of a total of 16 diesel-engine buses in Seoul, and the exposure range of EC at the bus driver’s seat was 1.7–67.2 mcg/m
3 and the geometric mean of EC was 23.0 ± 2.2 mcg/m
3. The Occupational Lung Disease Institute (2018) assessed the level of EC concentration in individual industries and reported that the EC exposure levels in the city bus transportation industry were the arithmetic mean of 2.45 mcg/m
3, geometric mean of 2.14 mcg/m
3, and demonstrated a minimum of 0.29, and maximum of 6.52 mcg/m
3.
19 The measured value at the bus driver’s seat exceeded the exposure standard withdrawn in 2003, after a prior notice by the American Conference of Governmental Industrial Hygienists at 20 mcg/m
3 in 2001 and the diesel smoke exposure limit of 20 mcg/m
3 in California, USA.
We concluded that the patient had been exposed DEE for up to 18 years while operating cargo trucks and buses until he was diagnosed with prostate cancer.
The Committee decision
The Committee concluded that 17 years of night-shift work and some exposure to DEE contributed to the development of high-grade prostate cancer.
Patient B
Patient information
The patient was a 57-year-old male.
Chief complaints
Difficulty in voiding
Past medical history
The patient stopped smoking and alcohol drinking 15 years prior. He has no family history of prostate cancer. However, he has been on medication for hypertension and dyslipidemia since 2003.
Present illness
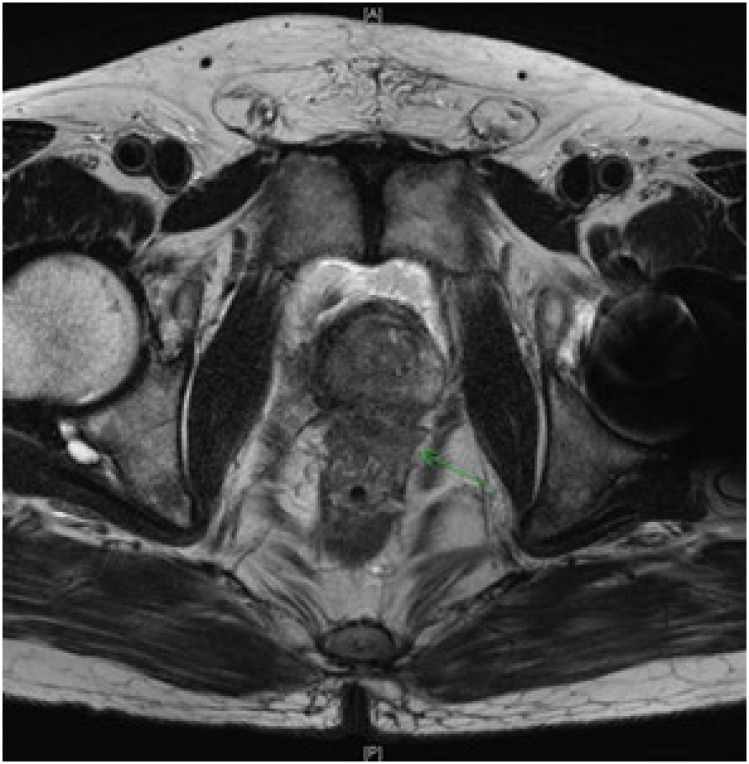
Patient B had voiding difficulty that had lasted for 6 months and was treated for benign prostatic hypertrophy at the urology clinic, however the symptoms did not improve. Therefore, he visited the university hospital on April 8, 2013, and an elevated PSA level (7.9 ng/mL) was observed. He was diagnosed with prostate cancer with a Gleason score of 10 (5 + 5), after undergoing transrectal ultrasonography and prostate core needle biopsy. Extracapsular extension (
Fig. 2) and enlarged lymph nodes were observed and prostate cancer was confirmed by a pelvic MRI and abdominal and pelvic CT. The prostate cancer was T4N1M0 and the patient was treated with androgen deprivation therapy. On July 29, 2013, he underwent palliative cystoprostatectomy, and the histologic type of the prostate cancer was found to be adenocarcinoma.
Fig. 2
MRI image of the pelvis of patient B. Transverse T2-weighted MRI image showing cancerous lesions of prostate with extracapsular extension.
MRI: magnetic resonance imaging.

Occupational history
The patient’s work history is summarized in
Table 3. Patient B worked for approximately 35 years from 1974 to 2013 as an electrician and power distribution engineer at the same workplace.
Table 3Occupational history of patient B
|
Date |
Duration |
Job |
|
1974.07.21.–1977.04.30. |
2 years and 9 monthsa
|
Power distribution engineer |
|
1977.05.01.–1980.02.29 |
2 years and 10 months |
Military service |
|
1980.03.01.–1983.09.15. |
3 years and 6 monthsa
|
Power distribution engineer |
|
1983.09.16.–1992.09.15. |
9 yearsa
|
Instrument repairman |
|
1992.09.16.–1997.11.30. |
5 years and 3 monthsa
|
Electrician |
|
1997.12.01.–2001.07.11. |
3 years and 7 monthsa
|
Manager (field general management) |
|
2001.07.12.–2002.04.15. |
9 monthsa
|
Sick leave (fracture) |
|
2002.04.16.–2003.06.15. |
1 year and 2 monthsa
|
Power distribution engineer |
|
2003.06.16.–2011.03.15. |
7 years and 9 monthsa,b
|
Manager (field general management) |
|
2011.03.16.–2013.05.28. |
2 years and 2 monthsb
|
Power distribution engineer |
Exposure assessment
1) Assessment of night shift work
His working hours are recorded in a computerized format since 1999. From 1999 to 2004, he worked 80 hours at night per month in 3 groups, 3-shifts, and 5-day cycles. From 2004, he worked 57 hours at night per month in 4-groups and 3-shifts, with 2 days off for every 5 days of work. The schedule for night-shift work was as follows: 08:00 to 16:00 for the day shift, 16:00 to 24:00 for the evening shift; and 00:00 to 08:00 for the night-shift. There were no work records before 1999, but since the workplace is open 24 hours a day, it is highly likely that the same work schedule had been maintained before, and the management of the company agreed to this. Therefore, we concluded that patient B had performed night-shift work for approximately 35 years. Summarized features of patient A’s night-shift work schedule are shown in
Table 4.
Table 4Patient B’s work schedule
|
Features |
Year 1974 to 2004 |
Year 2004 to 2013 |
|
With or without night work |
With night work |
With night work |
|
Continuous or discontinuous |
Continuous |
Continuous |
|
Permanent or rotating |
Rotating |
Rotating |
|
Length of the shift cycle |
15 days |
1 week |
|
Duration of individual shifts |
8 hours |
8 hours |
|
Start and end time of individual shifts |
Morning shift: 08:00 to 16:00 |
|
Evening shift: 16:00 to 00:00 |
|
Night shift: 00:00 to 08:00 |
|
Number of consecutive shifts |
5 shifts |
7 shifts |
|
Direction of shift rotation |
Forward |
Forward |
|
Number of rest days |
1 day every shift cycle |
2 days every week |
|
Regularity |
Regular |
Regular |
2) Other exposures
Most of the practices performed by Patient B are summarized as tasks such as measurement and management practices, facility operations, and repair plans through equipment or electrical devices. In particular, he worked as an instrument repairman and an electrician to solve problems, such as repairing devices at the site. However, most maintenance tasks are assigned to and performed by subcontractors. Patient B’s work was checking the operation status of electrical equipment facilities, such as facilities and lines, during repair work. Therefore, the business of dismantling old equipment and replacing it with new equipment was carried out by subcontractors.
Patient B was responsible for the maintenance and repair of the internal electrical facilities of the cement plant. The period of work that he was presumed to have been engaged in on-site inspection or maintenance activities was 5 years and 3 months as an electrician. No arsenic, cadmium, iron, aluminum, nickel, zinc, lead, or any of the 16 types of polycyclic aromatic hydrocarbons (PAHs) were detected in the measured air of the indoor and outdoor working lines. Even when checking the work environment measurement results for the manufacturing process of the plant from 2002 to 2013, most cases were below detectable limit. The DEE was evaluated by measuring the EC. In the case of EC, in the office the level was 0.11 mcg/m3 while it was not detected in other areas.
The Committee decision
The Committee concluded that 35 years of night-shift work to the development of high-grade prostate cancer.
Ethics statement
This study was approved by the Institutional Review Board (IRB) of the Occupational Safety and Health Research Institute (IRB No. OSHRI-202105-HR-017), and written informed consent was obtained from the patient or his family for the publication of this report and any accompanying data.
DISCUSSION AND CONCLUSION
In June 2019, the Working Group of the IARC re-evaluated night-shift work as Group 2A ‘probably carcinogenic to humans’ based on the limited evidence from epidemiological studies in humans, the sufficient evidence from animal studies, and the strong evidence for biological mechanisms in animal studies.
11The Working Group of the IARC stated that there is sufficient evidence of carcinogenicity from changes in light and dark schedules in animal studies. Results from several well-designed chronic animal bioassays were central to this evaluation. The incidence of lung adenocarcinoma, malignant melanoma, and total tumor was increased compared to control rats stably maintained on a 12-hour light and 12-hour dark schedule.
20 An in vivo study, which employed xenografted human prostate cancer cells, demonstrated that a 24-hour light schedule significantly increased tumor size in comparison to a 12-hour light/dark cycle.
21 Another in vivo study using mouse prostate cancer cells similarly found that long photoperiods and light interference markedly increased tumor size.
22 There is solid evidence from both epidemiologic and animal studies that changes in light and dark schedules lead to changes in serum melatonin and the expression of core circadian genes. Moreover, evidence for the biological mechanism was provided by the results of studies confirming the effects of light and dark schedule changes on immunosuppression, chronic inflammation, and cell proliferation.
23,24,25 The IARC evaluated the carcinogenicity of night-shift work twice, in 2007 and in 2019. In 2007, several epidemiologic studies reported their results on the carcinogenicity of night-shift work, but they focused mainly on female breast cancer. At that time, only one cohort study
26 and one case-control study
27 regarding the association between night-shift work and prostate cancer were reported. Both studies reported significant results, however they had several limitations, including weak statistical power. Therefore, in 2007 the IARC Working Group did not draw a conclusion regarding the association between night-shift work and prostate cancer. Since 2007, additional epidemiologic studies
16,28,29,30,31,32 have reported the association between night-shift work and prostate cancer. Based on the epidemiological evidence provided by these studies, the IARC in 2019 published a document mentioning that there is evidence suggestive of a quantitative association between the risk of prostate cancer and night-shift work.
In addition, recent meta-analyses have demonstrated consistent results regarding the association between the risk of prostate cancer and night-shift work. A meta-analysis of prostate cancer and various occupational risk factors was conducted covering 168 documents by searching the literature from 1966 to 2015. In the study, night-shift work was significantly associated with prostate cancer (relative risk [RR]: 1.25; 95% confidence interval [CI]: 1.05–1.49).
14 Another meta-analysis of 9 cohort studies regarding the risk of prostate cancer and night-shift, conducted through February 4, 2017, found a marginally significant association between night-shift work and prostate cancer (RR: 1.05; 95% CI: 1.00–1.11).
15 In the study, when subgroup analysis was performed by dividing the subgroups into Western countries and Asian countries, no significant association was observed in Western countries. However, significant association between the risk of prostate cancer and night-shift work was observed in the Asian countries group (RR: 2.45; 95% CI: 1.19–5.04). These findings suggest that night-shift work increases the risk of prostate cancer, particularly in Asians. A recent cohort study supports these findings. A Korean cohort study analyzed 6 years of health examination data and reported an association between night-shift work and elevated PSA.
33 In the study, compared to the daytime workers, the hazard ratio (HR) of shift workers increased significantly to 1.37 (95% CI: 1.04–1.80), and especially, the HR of rotating shift workers was 1.47 (95% CI: 1.06–2.03). In addition, in the most recently reported meta-analysis study, the following 4 epidemiological studies were evaluated as high-quality studies.
34 First, in 2016 a cohort study on a group of Finnish twins prospectively investigated the association between sleep and circadian factors in middle age and prostate cancer risk and mortality.
35 This study did not find a significant association. However, this study was conducted without an exposure assessment of duration and intensity of night-shift work. Second, a cohort study on male twins registered in the Swedish Twin Registry was conducted in 2017.
36 This study showed no significant associations between night work and prostate cancer, or length of night work and prostate cancer. However, the intensity of exposure was not considered in this study either. Third, a case-control study evaluated several potential risk factors of prostate cancer, including lifelong occupational history of participants in 2018.
16 In this study, the night-shift work was defined as working from 21:00 to 06:00 the next day in accordance with the French legal definition. The analysis revealed that night-shift work was not significantly associated with prostate cancer when the intensity of night-shift work, or the aggressiveness of prostate cancer were not considered. However, regardless of the total duration of night-shift work, the risk of prostate cancer was significantly increased when the shift length exceeded 10 hours and the number of cumulative night shifts were 1,314 days or more (odds ratio [OR]: 1.76; 95% CI: 1.03–3.03). In addition, the risk of prostate cancer was further increased when workers worked on night-shifts permanently (OR: 2.36; 95% CI: 1.21–4.56). Especially, when subgroup analysis was performed with Gleason score, permanent night-shift work for at least 20 years increased the risk of aggressive prostate cancer (Gleason score ≥ 7) (OR: 1.76; 95% CI: 1.13–2.75). Among them, the risk of aggressive prostate cancer was higher when the shift length was > 10 hours (OR: 4.64; 95% CI: 1.78–12.13). In addition, the risk of aggressive prostate cancer was also increased if the shift length was > 10 hours and permanent night-shift work was performed for more than 1,314 days (OR: 3.79; 95% CI: 1.58–9.12). In this study, long shift lengths or at least 6 consecutive night shifts when accompanied by long and permanent night-shifts were significantly associated particularly with aggressive prostate cancer. Finally, a case-control study investigated the association between night-shift work and the risk of prostate cancer in 2019.
37 No significant association was found between exposure to night-shift work and prostate cancer. This study did not consider the intensity of night-shift work or the aggressiveness of prostate cancer. A recently published case-cohort study using Norwegian Offshore Petroleum Workers cohort also supports an association between night-shift work and aggressive prostate cancer. The analysis showed that the risk of aggressive prostate cancer was significantly increased in the group with more than 19.5 years of rotating shifts (HR: 1.86; 95% CI: 1.18–2.91). Exposure-hazard curves using non-linear model showed a linear increase in risk with 18–26 years of rollover shifts.
38
In summary, these 2 cases meet the Bradford-Hill criteria of strength, consistency, temporality, biological gradient, plausibility, coherence, analogy, and experiment, except for specificity. 1) Strength: A study reported that the risk of aggressive prostate cancer was increased by the shift length with > 10 hours and permanent night-shift work for at least 20 years (OR: 4.64; 95% CI: 1.78–12.13). In addition, the risk of aggressive prostate cancer was also increased if the shift length was > 10 hours and permanent night-shift work was performed for more than 1,314 days (OR: 3.79; 95% CI: 1.58–9.12).
16 Another study reported that the risk of aggressive prostate cancer was significantly increased in the group with more than 19.5 years of rotating shifts (HR: 1.86; 95% CI: 1.18–2.91).
38 2) Consistency: Increased risk of prostate cancer in night-shift workers has been consistently observed in several epidemiological studies of various population and work schedules.
16,28,29,30,31,32 3) Temporality: The 2 workers were diagnosed with prostate cancer after doing night shift work for 17 and 35 years, respectively. 4) Biological gradient: Exposure-response curves using non-linear model showed a linear increase in risk of aggressive prostate cancer with 18–26 years of rollover shifts.
38 5) Plausibility: The biological mechanism was provided by the results of studies confirming the effects of light and dark schedule changes on immunosuppression, chronic inflammation, and cell proliferation
23,24,25 and also increased risk of cancer incidence was reported in animal studies.
20 6) Coherence: This epidemiological association between night-shift work and prostate cancer does not contradict natural history and biology of prostate cancer. 7) Analogy: IARC suggested that disruption to the circadian rhythm due to night shift work may increase the risk of breast, colon, and rectal cancer as well as prostate cancer.
11 8) Experiment: Two distinct in vivo studies, utilizing either human or mouse-derived prostate cancer cells, revealed a correlation between prolonged photoperiods or disruption to the circadian rhythm and an increase in tumor size.
21,22 9) Specificity: Specificity is not satisfied. Because night shift-work is associated with an increased risk of different types of cancers, as well as a range of other health consequences, including cardiovascular disease, obesity, and mental illnesses.
39
There are many different types of night shift work schedules, and many features of the night shift work appear to influence the intensity of circadian disruption. Hence, it seems improper to establish an absolute criterion that fits all types of night shift work schedule. Therefore, when evaluating whether a worker’s prostate cancer is work-related, several factors must be considered. These may include the length of their shifts, the duration of exposure to night work, the type of work schedule and the severity of the prostate cancer. It is important to evaluate these factors comprehensively to determine if there is a causal connection between the worker’s employment and the development of their cancer.
In patients A and B, the Gleason scores of prostate cancer were as high as 9 (4 + 5) and 10 points (5 + 5), respectively. The prognosis of prostate cancer differs depending on whether the score is greater or less than 7 points (3 + 4, 4 + 3). In addition, the definition of night-shift work varies from country to country. In a study conducted in France, it was defined as the time between 21:00 and 6:00, which is similar to that of night work hours in Korea. Considering this, we thought that the study conducted in France could best explain the relationship between the 2 cases and night-shift work.
Patient A was a bus driver for a city bus company for 5 years, from 2002 to 2006, and went to work approximately 6 days a week in the morning or afternoon shift on alternate weeks. From December 2006 to February 2019, he transferred to City Bus Company B and worked for an average of 17.5 hours, 5 to 6 days a week, operating a diesel bus for 6 to 7 years. He also operated 2.5 ton cargo trucks during the past 6 years. Patient A was classified as a night worker according to the general definition of night-shift work presented by the IARC and the Korean Labor Standards Act. Therefore, it was estimated that he had been exposed to night-shift work for approximately 17 years and to DEE during bus and freight truck operations for approximately 17 to 18 years. Several meta-analyses have demonstrated that night-shift work is significantly associated with prostate cancer, and this is particularly seen in men in Asian countries. Patient A had long working hours of 17.5 hours per day, including 3 hours of night-shift work every day for 12 out of 17 years of working as a bus driver. As mentioned earlier, long working hours and a large number of cumulative night-shifts are associated with highly aggressive prostate cancer. In addition, a previous study has demonstrated that there is a significant association between DEE and prostate cancer. One report describes a case-control study of the association between diesel exposure and prostate cancer, and the analysis showed a statistically significant association between occupational exposure to diesel fuel or diesel fumes and prostate cancer.
40 Although there is a limitation that his work schedule did not completely meet the standards for night work recommended by the IARC, the possibility that his work schedule contributed to the development of prostate cancer could not be excluded. We conclude that patient A’s 17 years of night-shift work and some exposure to DEE contributed to the development of prostate cancer.
Patient B worked at a cement manufacturing plant from 1974 to 2013, for a total of 35 years. Heavy metals such as arsenic, and PAHs were not detected in Patient B’s work environment measurement results. A previous review of the Material Safety Data Sheet from 2002 to 2013 found that Patient B was less likely to have been exposed. The amount of exposure to DEE is thought to have been very small because the working area is an outdoor field and workers are only exposed during the circuit inspection of facilities. In fact, DEE’s exposure levels were very low even in the work environment measurement results. He was exposed to approximately 80 hours of night work per month for 26 years out of a total of 35 years of work, and approximately 57 hours of night work for 9 years. We conclude that night-shift work may have contributed to the development of prostate cancer, given that he was exposed to a significant period of night-shift work and his biopsy results showed a high level of aggression (Gleason score 5 + 5 = 10).
In 2019, the IARC re-evaluated the carcinogenicity of night-shift work and reported that there is limited evidence that night-shift work is carcinogenic for the development of prostate cancer.
11 Additionally, recent meta-analysis studies have reported that night-shift work is associated with the risk of prostate cancer, particularly in a group of Asian countries.
14,15 A well-designed case-control study reported that night work increased the risk of prostate cancer, especially the risk of prostate cancer with high Gleason scores supported by recently published case-cohort study.
16,38 Based on the scientific evidences, the Epidemiologic Investigation Evaluation Committee recognized 2 cases in 2020 and 2021 based on the association between night-shift work and prostate cancer. These 2 cases have expanded the scope of industrial accident compensation for prostate cancer related to night-shift work. Special health examinations are currently being conducted for night-shift workers; however prostate cancer is not the target disease. To control the risks associated with night-shifts, it is necessary to regulate work schedules and implement appropriate health examinations.
Acknowledgements
The present study utilized workers’ data that were formally obtained from the Occupational Safety and Health Research Institute (OSHRI), and the Korean Occupational Safety and Health Agency (KOSHA) and did not include identifiable personal information.
Abbreviations
International Agency for Research on Cancer
Korea Workers’ Compensation & Welfare Service
magnetic resonance imaging
Occupational Safety and Health Institute
polycyclic aromatic hydrocarbon
prostate-specific antigen
NOTES
-
Competing interests: The authors declare that they have no competing interests.
-
Author Contributions:
Conceptualization: Ye S, Lee J.
Data curation: Park S.
Investigation: Park S, Ma S, Seo H, Lee SG.
Writing - original draft: Park S.
Writing - review & editing: Park S, Ye S, Lee J.
REFERENCES
REFERENCES
- 1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin 2021;71(1):7–33. 33433946.ArticlePubMedPDF
- 2. Jung KW, Won YJ, Hong S, Kong HJ, Lee ES. Prediction of cancer incidence and mortality in Korea, 2020. Cancer Res Treat 2020;52(2):351–358. 32178488.ArticlePubMedPMCPDF
- 3. Platz EA, Rimm EB, Willett WC, Kantoff PW, Giovannucci E. Racial variation in prostate cancer incidence and in hormonal system markers among male health professionals. J Natl Cancer Inst 2000;92(24):2009–2017. 11121463.ArticlePubMed
- 4. Delongchamps NB, Singh A, Haas GP. The role of prevalence in the diagnosis of prostate cancer. Cancer Contr 2006;13(3):158–168.ArticlePDF
- 5. Allott EH, Masko EM, Freedland SJ. Obesity and prostate cancer: weighing the evidence. Eur Urol 2013;63(5):800–809. 23219374.ArticlePubMedPMC
- 6. Bratt O, Drevin L, Akre O, Garmo H, Stattin P. Family history and probability of prostate cancer, differentiated by risk category: a nationwide population-based study. J Natl Cancer Inst 2016;108(10):djw110. 27400876.ArticlePubMed
- 7. Salinas CA, Tsodikov A, Ishak-Howard M, Cooney KA. Prostate cancer in young men: an important clinical entity. Nat Rev Urol 2014;11(6):317–323. 24818853.ArticlePubMedPMCPDF
- 8. Gleason DF, Mellinger GT. Prediction of prognosis for prostatic adenocarcinoma by combined histological grading and clinical staging. J Urol 1974;111(1):58–64. 4813554.ArticlePubMed
- 9. Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA. Grading Committee. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol 2016;40(2):244–252. 26492179.PubMed
- 10. Carter HB, Partin AW, Walsh PC, Trock BJ, Veltri RW, Nelson WG, et al. Gleason score 6 adenocarcinoma: should it be labeled as cancer? J Clin Oncol 2012;30(35):4294–4296. 23032616.ArticlePubMedPMC
- 11. IARC. Night Shift Work: IARC Monographs on the Identification of Carcinogenic Hazards to Humans. Vol. 124: Lyon, France: IARC; 2020.
- 12. National Toxicology Program. NTP Cancer Hazard Assessment Report on Night Shift Work and Light at Night. Updated 2021]. Accessed August 2, 2021].
http://www.ncbi.nlm.nih.gov/books/NBK571598/
.
- 13. Ko J, Jang E, Shin C, Park D, Kim H, Lee J. 5th Korean Working Conditions Survey. Incheon, Korea: Occupational Safety and Health Research Institute; 2017.
- 14. Krstev S, Knutsson A. Occupational risk factors for prostate cancer: a meta-analysis. J Cancer Prev 2019;24(2):91–111. 31360689.ArticlePubMedPMC
- 15. Du HB, Bin KY, Liu WH, Yang FS. Shift work, night work, and the risk of prostate cancer: a meta-analysis based on 9 cohort studies. Medicine (Baltimore) 2017;96(46):e8537. 29145258.PubMedPMC
- 16. Wendeu-Foyet MG, Bayon V, Cénée S, Trétarre B, Rébillard X, Cancel-Tassin G, et al. Night work and prostate cancer risk: results from the EPICAP Study. Occup Environ Med 2018;75(8):573–581. 29921728.ArticlePubMedPMC
- 17. Lee KH, Jung HJ, Park DU, Ryu SH, Kim B, Ha KC, et al. Occupational exposure to diesel particulate matter in municipal household waste workers. PLoS One 2015;10(8):e0135229. 26248196.ArticlePubMedPMC
- 18. Jung J. Bus driver exposure assessment of particulate matter and gases. Bull Nat Sci 2008;13(1):125–133.
- 19. Shin J. Analysis of Diesel Exhaust Exposure Level of Workers in Korea by Industry and Job. Incheon, Korea: Occupational Lung Disease Institute; 2018.
- 20. Anisimov VN, Baturin DA, Popovich IG, Zabezhinski MA, Manton KG, Semenchenko AV, et al. Effect of exposure to light-at-night on life span and spontaneous carcinogenesis in female CBA mice. Int J Cancer 2004;111(4):475–479. 15239122.ArticlePubMed
- 21. Yasuniwa Y, Izumi H, Wang KY, Shimajiri S, Sasaguri Y, Kawai K, et al. Circadian disruption accelerates tumor growth and angio/stromagenesis through a Wnt signaling pathway. PLoS One 2010;5(12):e15330. 21203463.ArticlePubMedPMC
- 22. Haim A, Yukler A, Harel O, Schwimmer H, Fares F. Effects of chronobiology on prostate cancer cells growth in vivo. Sleep Sci 2010;3(1):32–35.
- 23. Logan RW, Zhang C, Murugan S, O’Connell S, Levitt D, Rosenwasser AM, et al. Chronic shift-lag alters the circadian clock of NK cells and promotes lung cancer growth in rats. J Immunol 2012;188(6):2583–2591. 22308312.ArticlePubMedPMCPDF
- 24. Castanon-Cervantes O, Wu M, Ehlen JC, Paul K, Gamble KL, Johnson RL, et al. Dysregulation of inflammatory responses by chronic circadian disruption. J Immunol 2010;185(10):5796–5805. 20944004.ArticlePubMedPMCPDF
- 25. Bedrosian TA, Fonken LK, Walton JC, Nelson RJ. Chronic exposure to dim light at night suppresses immune responses in Siberian hamsters. Biol Lett 2011;7(3):468–471. 21270021.ArticlePubMedPMCPDF
- 26. Kubo T, Ozasa K, Mikami K, Wakai K, Fujino Y, Watanabe Y, et al. Prospective cohort study of the risk of prostate cancer among rotating-shift workers: findings from the Japan collaborative cohort study. Am J Epidemiol 2006;164(6):549–555. 16829554.ArticlePubMed
- 27. Conlon M, Lightfoot N, Kreiger N. Rotating shift work and risk of prostate cancer. Epidemiology 2007;18(1):182–183. 17179764.ArticlePubMed
- 28. Parent MÉ, El-Zein M, Rousseau MC, Pintos J, Siemiatycki J. Night work and the risk of cancer among men. Am J Epidemiol 2012;176(9):751–759. 23035019.ArticlePubMed
- 29. Hammer GP, Emrich K, Nasterlack M, Blettner M, Yong M. Shift work and prostate cancer incidence in industrial workers: a historical cohort study in a German chemical company. Dtsch Arztebl Int 2015;112(27-28):463–470. 26214232.PubMedPMC
- 30. Papantoniou K, Castaño-Vinyals G, Espinosa A, Aragonés N, Pérez-Gómez B, Burgos J, et al. Night shift work, chronotype and prostate cancer risk in the MCC-Spain case-control study. Int J Cancer 2015;137(5):1147–1157. 25530021.PubMed
- 31. Behrens T, Rabstein S, Wichert K, Erbel R, Eisele L, Arendt M, et al. Shift work and the incidence of prostate cancer: a 10-year follow-up of a German population-based cohort study. Scand J Work Environ Health 2017;43(6):560–568. 28879368.ArticlePubMed
- 32. Tse LA, Lee PM, Ho WM, Lam AT, Lee MK, Ng SS, et al. Bisphenol A and other environmental risk factors for prostate cancer in Hong Kong. Environ Int 2017;107:1–7. 28644961.ArticlePubMed
- 33. Lee Y, Lee W, Kim HR. A longitudinal study of the relationship between shift work and prostate-specific antigen in healthy male workers. Int J Environ Res Public Health 2021;18(14):7458. 34299909.ArticlePubMedPMC
- 34. Rivera-Izquierdo M, Martínez-Ruiz V, Castillo-Ruiz EM, Manzaneda-Navío M, Pérez-Gómez B, Jiménez-Moleón JJ. Shift work and prostate cancer: an updated systematic review and meta-analysis. Int J Environ Res Public Health 2020;17(4):1345. 32093096.ArticlePubMedPMC
- 35. Dickerman BA, Markt SC, Koskenvuo M, Hublin C, Pukkala E, Mucci LA, et al. Sleep disruption, chronotype, shift work, and prostate cancer risk and mortality: a 30-year prospective cohort study of Finnish twins. Cancer Causes Control 2016;27(11):1361–1370. 27734240.ArticlePubMedPMCPDF
- 36. Åkerstedt T, Narusyte J, Svedberg P, Kecklund G, Alexanderson K. Night work and prostate cancer in men: a Swedish prospective cohort study. BMJ Open 2017;7(6):e015751.ArticlePubMedPMC
- 37. Barul C, Richard H, Parent ME. Night-shift work and risk of prostate cancer: results from a Canadian case-control study, the prostate cancer and environment study. Am J Epidemiol 2019;188(10):1801–1811. 31360990.ArticlePubMedPMCPDF
- 38. Berge LA, Liu FC, Grimsrud TK, Babigumira R, Støer NC, Kjærheim K, et al. Night shift work and risk of aggressive prostate cancer in the Norwegian Offshore Petroleum Workers (NOPW) cohort. Int J Epidemiol 2023;52(4):1003–1014. 36548214.ArticlePubMed
- 39. Costa G. Shift work and health: current problems and preventive actions. Saf Health Work 2010;1(2):112–123. 22953171.ArticlePubMedPMC
- 40. Seidler A, Heiskel H, Bickeböller R, Elsner G. Association between diesel exposure at work and prostate cancer. Scand J Work Environ Health 1998;24(6):486–494. 9988091.ArticlePubMed
 , Seongwon Ma1
, Seongwon Ma1 , Hoekyeong Seo1
, Hoekyeong Seo1 , Sang Gil Lee1
, Sang Gil Lee1 , Jihye Lee1
, Jihye Lee1 , Shinhee Ye2
, Shinhee Ye2


 KSOEM
KSOEM

 Cite
Cite

