Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 32; 2020 > Article
- Research Article Association between green areas and allergic disease in Korean adults: a cross-sectional study
- Hyun-Jin Kim1, Jin-young Min2, Hye-Jin Kim3, Kyoung-bok Min3
-
Annals of Occupational and Environmental Medicine 2020;32:e5.
DOI: https://doi.org/10.35371/aoem.2020.32.e5
Published online: January 22, 2020
1National Cancer Control Institute, National Cancer Center, Goyang, South Korea.
2Institute of Health and Environment, Seoul National University, Seoul, Korea.
3Department of Preventive Medicine, College of Medicine, Seoul National University, Seoul, Korea.
- Correspondence: Kyoung-Bok Min. Department of Preventive Medicine, Colleague of Medicine, Seoul National University, 103 Daehak-ro, Jongno-gu, Seoul 03080, Korea. minkb@snu.ac.kr
- †These authors contributed equally to this work.
Copyright © 2020 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background Although many epidemiological studies have reported the inverse associations between greenness and health outcomes, inconsistent associations in allergic diseases remain an issue. We aimed to identify associations between greenness and allergic diseases among Korean adults.
-
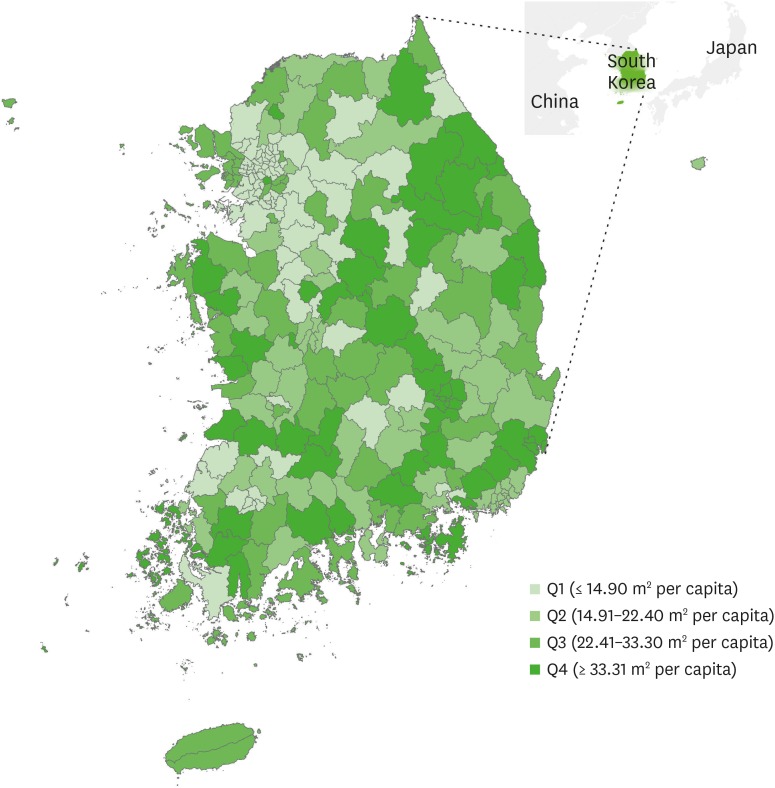
Methods In total, 219,298 adults from the 2009 Korea Community Health Survey were included in this study. Individuals' allergy-related conditions, such as atopic dermatitis and allergic rhinitis, were evaluated. To identify the amount of green areas (m2) per capita in each administrative region, we used the 2009 data for green areas from the Korean Statistical Information Service.
-
Results The risk for atopic dermatitis in the highest quartile of green areas was significantly lower compared with that of the lowest quartile. Physician's diagnosis and current treatment of odds ratios (ORs) with 95% confidence intervals (CIs) were 0.82 (0.73–0.91) and 0.77 (0.64–0.92), respectively. Similarly, the association results for allergic rhinitis showed that the highest level of green areas was significantly associated with a decreased risk of allergic rhinitis in full-adjustment model quartiles. Physician's diagnosis and current treatment of OR (95% CI) were 0.94 (0.89–0.99) and 0.91 (0.82–1.00), respectively.
-
Conclusions We observed inverse associations of green areas with atopic dermatitis and allergic rhinitis in Korean adults.
BACKGROUND
METHODS
RESULTS
Characteristics of study population
Prevalence odds ratio (95% confidence interval) for atopic dermatitis by the level green areas
Prevalence odds ratio (95% confidence interval) for allergic rhinitis by the level of green areas
Prevalence odds ratio (95% CI) for atopic dermatitis and allergic rhinitis by the level of green areas, stratified by moderate physical activity
DISCUSSION
CONCLUSIONS
Abbreviations
BMI
CI
KOSIS
KCHS
OR
-
Funding: This work was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (grant number, Grant No. 2018R1D1A1A09083190 and 2019R1A2C1004966).
-
Competing interests: The authors declare that they have no competing interests.
-
Authors contributions:
Conceptualization: Kim HJ1, Min JY, Min KB.
Formal analysis: Kim HJ1, Min JY, Kim HJ2.
Project administration: Min KB.
Supervision: Min KB.
Writing - original draft: Kim HJ1, Min JY.
Writing - review & editing: Min KB.
1Kim HJ, Hyun-Jin Kim; 2Kim HJ, Hye-Jin Kim
NOTES
- 1. Bodicoat DH, O'Donovan G, Dalton AM, Gray LJ, Yates T, Edwardson C, et al. The association between neighbourhood greenspace and type 2 diabetes in a large cross-sectional study. BMJ Open 2014;4(12):e006076.ArticlePubMedPMC
- 2. Dadvand P, Villanueva CM, Font-Ribera L, Martinez D, Basagaña X, Belmonte J, et al. Risks and benefits of green spaces for children: a cross-sectional study of associations with sedentary behavior, obesity, asthma, and allergy. Environ Health Perspect 2014;122(12):1329–1335. 25157960.ArticlePubMedPMC
- 3. Dzhambov AM, Dimitrova DD, Dimitrakova ED. Association between residential greenness and birth weight: systematic review and meta-analysis. Urban For Urban Green 2014;13(4):621–629.Article
- 4. Gascon M, Triguero-Mas M, Martínez D, Dadvand P, Forns J, Plasència A, et al. Mental health benefits of long-term exposure to residential green and blue spaces: a systematic review. Int J Environ Res Public Health 2015;12(4):4354–4379. 25913182.ArticlePubMedPMC
- 5. Tamosiunas A, Grazuleviciene R, Luksiene D, Dedele A, Reklaitiene R, Baceviciene M, et al. Accessibility and use of urban green spaces, and cardiovascular health: findings from a Kaunas cohort study. Environ Health 2014;13(1):20. 24645935.ArticlePubMedPMCPDF
- 6. World Health Organization. Urban green spaces and health: a review of evidence. Geneva: World Health Organization; 2016.
- 7. Rook GA. Regulation of the immune system by biodiversity from the natural environment: an ecosystem service essential to health. Proc Natl Acad Sci U S A 2013;110(46):18360–18367. 24154724.ArticlePubMedPMC
- 8. Fuertes E, Markevych I, von Berg A, Bauer CP, Berdel D, Koletzko S, et al. Greenness and allergies: evidence of differential associations in two areas in Germany. J Epidemiol Community Health 2014;68(8):787–790. 24862831.ArticlePubMedPMC
- 9. Hanski I, von Hertzen L, Fyhrquist N, Koskinen K, Torppa K, Laatikainen T, et al. Environmental biodiversity, human microbiota, and allergy are interrelated. Proc Natl Acad Sci U S A 2012;109(21):8334–8339. 22566627.ArticlePubMedPMC
- 10. Lynch SV, Wood RA, Boushey H, Bacharier LB, Bloomberg GR, Kattan M, et al. Effects of early-life exposure to allergens and bacteria on recurrent wheeze and atopy in urban children. J Allergy Clin Immunol 2014;134(3):593–601.e12. 24908147.ArticlePubMedPMC
- 11. Ruokolainen L, von Hertzen L, Fyhrquist N, Laatikainen T, Lehtomäki J, Auvinen P, et al. Green areas around homes reduce atopic sensitization in children. Allergy 2015;70(2):195–202. 25388016.ArticlePubMedPMCPDF
- 12. Sbihi H, Tamburic L, Koehoorn M, Brauer M. Greenness and incident childhood asthma: a 10-year follow-up in a population-based birth cohort. Am J Respir Crit Care Med 2015;192(9):1131–1133. 26517419.ArticlePubMed
- 13. Andrusaityte S, Grazuleviciene R, Kudzyte J, Bernotiene A, Dedele A, Nieuwenhuijsen MJ. Associations between neighbourhood greenness and asthma in preschool children in Kaunas, Lithuania: a case-control study. BMJ Open 2016;6(4):e010341.ArticlePubMedPMC
- 14. Fuertes E, Markevych I, Bowatte G, Gruzieva O, Gehring U, Becker A, et al. Residential greenness is differentially associated with childhood allergic rhinitis and aeroallergen sensitization in seven birth cohorts. Allergy 2016;71(10):1461–1471. 27087129.ArticlePubMedPDF
- 15. Lovasi GS, O'Neil-Dunne JP, Lu JW, Sheehan D, Perzanowski MS, Macfaden SW, et al. Urban tree canopy and asthma, wheeze, rhinitis, and allergic sensitization to tree pollen in a New York City birth cohort. Environ Health Perspect 2013;121(4):494–500. 23322788.ArticlePubMedPMC
- 16. Park HS, Choi GS, Cho JS, Kim YY. Epidemiology and current status of allergic rhinitis, asthma, and associated allergic diseases in Korea: ARIA Asia-Pacific workshop report. Asian Pac J Allergy Immunol 2009;27(2-3):167–171. 19839504.PubMed
- 17. Liebhart J, Dobek R, Małolepszy J, Wojtyniak B, Pisiewicz K, Płusa T, et al. The prevalence of allergic diseases in Poland - the results of the PMSEAD study in relation to gender differences. Adv Clin Exp Med 2014;23(5):757–762. 25491690.ArticlePubMed
- 18. Kang YW, Ko YS, Kim YJ, Sung KM, Kim HJ, Choi HY, et al. Korea community health survey data profiles. Osong Public Health Res Perspect 2015;6(3):211–217. 26430619.ArticlePubMedPMC
- 19. Lovasi GS, Quinn JW, Neckerman KM, Perzanowski MS, Rundle A. Children living in areas with more street trees have lower prevalence of asthma. J Epidemiol Community Health 2008;62(7):647–649. 18450765.ArticlePubMedPMC
- 20. Maas J, Verheij RA, de Vries S, Spreeuwenberg P, Schellevis FG, Groenewegen PP. Morbidity is related to a green living environment. J Epidemiol Community Health 2009;63(12):967–973. 19833605.ArticlePubMed
- 21. DellaValle CT, Triche EW, Leaderer BP, Bell ML. Effects of ambient pollen concentrations on frequency and severity of asthma symptoms among asthmatic children. Epidemiology 2012;23(1):55–63. 22082997.ArticlePubMedPMC
- 22. Font-Ribera L, Kogevinas M, Zock JP, Nieuwenhuijsen MJ, Heederik D, Villanueva CM. Swimming pool attendance and risk of asthma and allergic symptoms in children. Eur Respir J 2009;34(6):1304–1310. 19443529.ArticlePubMed
- 23. Kilpeläinen M, Terho EO, Helenius H, Koskenvuo M. Body mass index and physical activity in relation to asthma and atopic diseases in young adults. Respir Med 2006;100(9):1518–1525. 16503404.ArticlePubMed
- 24. Alves A, Martins C, Delgado L, Fonseca J, Moreira A. Exercise-induced rhinitis in competitive swimmers. Am J Rhinol Allergy 2010;24(5):e114–7. 21244727.ArticlePubMedPDF
- 25. Helenius IJ, Tikkanen HO, Sarna S, Haahtela T. Asthma and increased bronchial responsiveness in elite athletes: atopy and sport event as risk factors. J Allergy Clin Immunol 1998;101(5):646–652. 9600502.ArticlePubMed
- 26. Dadvand P, de Nazelle A, Triguero-Mas M, Schembari A, Cirach M, Amoly E, et al. Surrounding greenness and exposure to air pollution during pregnancy: an analysis of personal monitoring data. Environ Health Perspect 2012;120(9):1286–1290. 22647671.ArticlePubMedPMC
- 27. Nowak DJ, Crane DE, Stevens JC. Air pollution removal by urban trees and shrubs in the United States. Urban For Urban Green 2006;4(3-4):115–123.Article
- 28. Nowak DJ, Heisler GM. Air quality effects of urban trees and parks. Ashburn: National Recreation and Parks Association; 2010.
- 29. Nowak DJ, Crane DE. Carbon storage and sequestration by urban trees in the USA. Environ Pollut 2002;116(3):381–389. 11822716.ArticlePubMed
- 30. Ahn K. The role of air pollutants in atopic dermatitis. J Allergy Clin Immunol 2014;134(5):993–999. 25439225.ArticlePubMed
- 31. Hwang BF, Jaakkola JJ, Lee YL, Lin YC, Guo YL. Relation between air pollution and allergic rhinitis in Taiwanese schoolchildren. Respir Res 2006;7(1):23. 16469096.ArticlePubMedPMCPDF
- 32. Kim HO, Kim JH, Cho SI, Chung BY, Ahn IS, Lee CH, et al. Improvement of atopic dermatitis severity after reducing indoor air pollutants. Ann Dermatol 2013;25(3):292–297. 24003270.ArticlePubMedPMC
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Association Between Urban Green Space and Acute Exacerbations of COPD in Korea: A Nationwide Study Using the NHIS-NSC Cohort
Hae In Jung, Ju Won Lee, Hyochan Kim, Hoyoung Cha, Jongjin Baik, Kyoung Min Moon, Changhyun Jun, Sun-Young Jung, Kang-Mo Gu
International Journal of Chronic Obstructive Pulmonary Disease.2025; Volume 20: 3035. CrossRef - Association between residential greenness and allergic diseases among adolescents in South Korea: A nationwide representative study
Jeongmin M. Lee, Juyeong Kim, Kyeongeun Kim, Yesol Yim, Yerin Hwang, Selin Woo, Dong Keon Yon
Pediatric Allergy and Immunology.2025;[Epub] CrossRef - EAACI Guidelines on the Importance of Green Space in Urban Environments for Allergy and Asthma Prevention
Tari Haahtela, Liam O'Mahony, Claudia Traidl‐Hoffmann, Mubeccel Akdis, Ozlem Ceylan, Panagiotis Chaslaridis, Athanasios Damialis, Stefano Del Giacco, Antti Lauerma, Kari C. Nadeau, Inês Paciência, Isabella Pali‐Schöll, Oscar Palomares, Harald Renz, Jurgen
Allergy.2025;[Epub] CrossRef - Association of Soda Drinks and Fast Food with Allergic Diseases in Korean Adolescents: A Nationwide Representative Study
Jinyoung Jeong, Hyesu Jo, Yejun Son, Sooji Lee, Kyeongmin Lee, Yujin Choi, Hayeon Lee, Soeun Kim, Louis Jacob, Lee Smith, Jun Hyuk Lee, Sang Youl Rhee, Sunyoung Kim, Jiseung Kang, Jiyoung Hwang, Jaeyu Park, Selin Woo, Dong Keon Yon
International Archives of Allergy and Immunology.2024; 185(12): 1190. CrossRef - Association of residential greenness with incident allergic rhinitis among adults: A prospective analysis of UK Biobank
Xueqiong Weng, Gengze Liao, Feng Wang, Wenzhen Li, Mei-Po Kwan, Victoria H. Arrandale, Lap Ah Tse
Science of The Total Environment.2024; 946: 174184. CrossRef - Greenness and its composition and configuration in association with allergic rhinitis in preschool children
Han Chen, Xia Meng, Yongfu Yu, Jin Sun, Zhiping Niu, Jing Wei, Ling Zhang, Chan Lu, Wei Yu, Tingting Wang, Xiaohong Zheng, Dan Norbäck, Magnus Svartengren, Xin Zhang, Zhuohui Zhao
Environmental Research.2024; 251: 118627. CrossRef - Environmental justice and allergic disease: A Work Group Report of the AAAAI Environmental Exposure and Respiratory Health Committee and the Diversity, Equity and Inclusion Committee
Allison J. Burbank, Michelle L. Hernandez, Akilah Jefferson, Tamara T. Perry, Wanda Phipatanakul, Jill Poole, Elizabeth C. Matsui
Journal of Allergy and Clinical Immunology.2023; 151(3): 656. CrossRef - Greenness and chronic respiratory health issues: a systematic review and meta-analysis
Mingcheng Tang, Wei Liu, Haifang Li, Fengyi Li
Frontiers in Public Health.2023;[Epub] CrossRef - Association between exposure to greenness and atopic march in children and adults—A systematic review and meta-analysis
Xue Wang, Nan Zhou, Yuxiang Zhi
Frontiers in Public Health.2023;[Epub] CrossRef - Effect of indoor house dust mite concentration on canine atopic dermatitis
Jihee Kim, Ji-Hye Lee, Yunji Song, Ha-Jung Kim
Frontiers in Veterinary Science.2023;[Epub] CrossRef - Early-immune development in asthma: A review of the literature
Maria V. Medeleanu, Yu Chen Qian, Theo J. Moraes, Padmaja Subbarao
Cellular Immunology.2023; 393-394: 104770. CrossRef - Exposure to urban greenspace and pathways to respiratory health: An exploratory systematic review
William Mueller, James Milner, Miranda Loh, Sotiris Vardoulakis, Paul Wilkinson
Science of The Total Environment.2022; 829: 154447. CrossRef - The associations between residential greenness and allergic diseases in Chinese toddlers: A birth cohort study
Lizi Lin, Yujing Chen, Jing Wei, Shengchi Wu, Shu Wu, Jin Jing, Guanghui Dong, Li Cai
Environmental Research.2022; 214: 114003. CrossRef - Exposure to green space and pollen allergy symptom severity: A case-crossover study in Belgium
Michiel Stas, Raf Aerts, Marijke Hendrickx, Andy Delcloo, Nicolas Dendoncker, Sebastien Dujardin, Catherine Linard, Tim Nawrot, An Van Nieuwenhuyse, Jean-Marie Aerts, Jos Van Orshoven, Ben Somers
Science of The Total Environment.2021; 781: 146682. CrossRef
- Figure
- Related articles
-
- Association between sudden work recall and psychological health issues: a cross-sectional analysis of the 6th Korean Working Conditions Survey
- Association between serum iron levels and low-frequency hearing loss in Korean females
- Sex difference in musculoskeletal disabilities among Korean fishers: a cross-sectional study
- Association between multiple jobs and physical and psychological symptoms among the Korean working population
- The association of shift work and TyG index among male workers in a chemical plant of Korea: a cross-sectional study
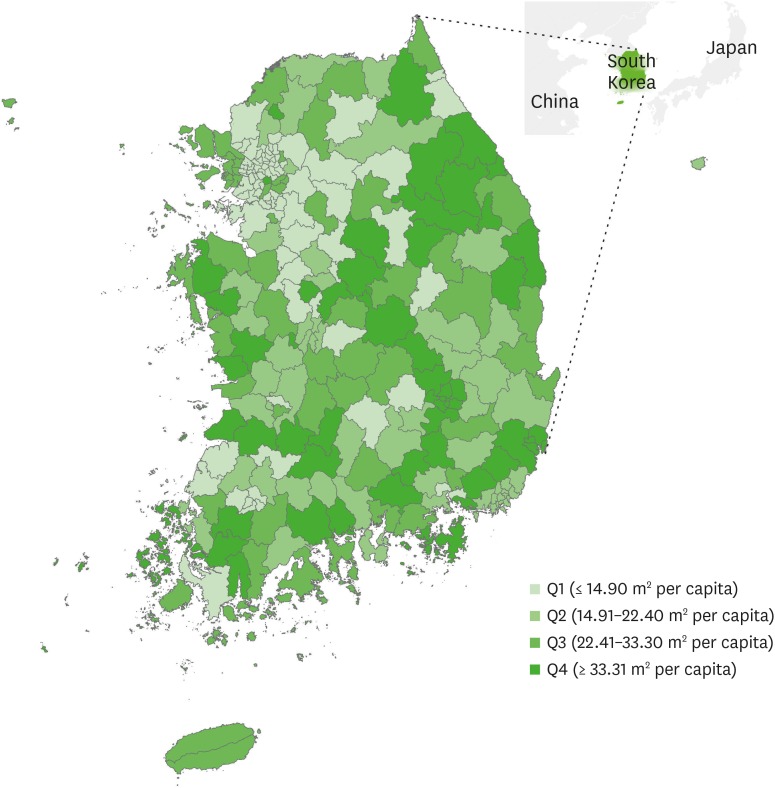
Fig. 1
| Characteristics | Values | |
|---|---|---|
| Age (years) | 49.37 ± 16.24 | |
| Sex | ||
| Male | 100,302 (47.15) | |
| Female | 112,422 (52.85) | |
| Marital status | ||
| Married | 152,531 (71.7) | |
| Divorced/widowed | 28,247 (13.28) | |
| Never married | 31,946 (15.02) | |
| Education | ||
| Elementary or less | 55,659 (26.16) | |
| Middle-High school | 91,839 (43.17) | |
| College or higher | 65,226 (30.66) | |
| Monthly income (1,000 KRW) | ||
| Q1 (≤ 1,000) | 54,378 (25.56) | |
| Q2 (1,001–2,000) | 51,633 (24.27) | |
| Q3 (2,001–3,500) | 46,299 (21.76) | |
| Q4 (≥ 3,501) | 60,414 (28.4) | |
| Job categories | ||
| White-collar | 40,398 (18.99) | |
| Pink-collar | 28,031 (13.18) | |
| Blue-collar | 62,133 (29.21) | |
| Military | 1,043 (0.49) | |
| No economic act | 81,119 (38.13) | |
| Cigarette smoking | ||
| Current smoker | 51,530 (24.22) | |
| Former smoker | 29,283 (13.77) | |
| Never smoker | 131,911 (62.01) | |
| Alcohol drinking | ||
| Drinker | 108,520 (51.01) | |
| Non-drinker | 104,204 (48.99) | |
| Moderate activity | ||
| Yes | 62,448 (29.36) | |
| No | 150,276 (70.64) | |
| Self-reported stress | ||
| High | 56,424 (26.52) | |
| Low | 156,300 (73.48) | |
| Urbanity | ||
| Urban | 97,923 (46.03) | |
| Rural | 114,801 (53.97) | |
| BMI (kg/m2) | 22.95 ± 3.04 | |
| Variables | Two times increase in green areas | Quartiles of green areas (m2 per capita) | Trend p-valuea | ||||
|---|---|---|---|---|---|---|---|
| Q1 (≤ 14.90) | Q2 (14.91–22.40) | Q3 (22.41–33.30) | Q4 (≥ 33.31) | ||||
| Physician's diagnosis | |||||||
| Unadjusted model | 0.88 (0.84–0.92) | Reference | 1.24 (1.13–1.36) | 0.97 (0.86–1.10) | 0.81 (0.73–0.91) | < 0.0001 | |
| Model 1 | 0.90 (0.86–0.94) | Reference | 1.15 (0.99–1.34) | 1.01 (0.83–1.23) | 0.76 (0.63–0.91) | < 0.0001 | |
| Model 2 | 0.90 (0.86–0.95) | Reference | 1.14 (1.09–1.20) | 0.92 (0.86–0.98) | 0.95 (0.90–1.00) | < 0.0001 | |
| Model 3 | 0.91 (0.87–0.95) | Reference | 1.13 (1.04–1.23) | 1.01 (0.91–1.12) | 0.91 (0.83–1.00) | < 0.0001 | |
| Model 4 | 0.94 (0.90–0.98) | Reference | 1.17 (1.07–1.29) | 1.00 (0.88–1.12) | 0.82 (0.73–0.91) | < 0.0001 | |
| Current treatment | |||||||
| Unadjusted model | 0.89 (0.83–0.95) | Reference | 1.14 (0.97–1.33) | 1.03 (0.85–1.25) | 0.77 (0.64–0.92) | < 0.0001 | |
| Model 1 | 0.90 (0.83–0.97) | Reference | 1.06 (1.01–1.11) | 0.92 (0.86–0.98) | 0.94 (0.89–0.99) | < 0.0001 | |
| Model 2 | 0.90 (0.84–0.97) | Reference | 1.07 (0.98–1.16) | 1.01 (0.91–1.12) | 0.90 (0.82–0.99) | 0.0021 | |
| Model 3 | 0.90 (0.84–0.97) | Reference | 1.17 (1.06–1.29) | 1.00 (0.89–1.13) | 0.82 (0.73–0.91) | < 0.0001 | |
| Model 4 | 0.92 (0.85–0.99) | Reference | 1.14 (0.97–1.33) | 1.03 (0.85–1.25) | 0.77 (0.64–0.92) | < 0.0001 | |
| Variables | Two times increase in green areas | Quartiles of green areas (m2 per capita) | Trend p-valuea | ||||
|---|---|---|---|---|---|---|---|
| Q1 (≤ 14.90) | Q2 (14.91–22.40) | Q3 (22.41–33.30) | Q4 (≥ 33.31) | ||||
| Physician's diagnosis | |||||||
| Unadjusted model | 0.91 (0.89–0.93) | Reference | 1.06 (1.01–1.11) | 0.92 (0.86–0.98) | 0.94 (0.89–0.99) | < 0.0001 | |
| Model 1 | 0.94 (0.92–0.96) | Reference | 1.07 (0.98–1.16) | 1.01 (0.91–1.12) | 0.90 (0.82–0.99) | 0.0019 | |
| Model 2 | 0.94 (0.92–0.96) | Reference | 1.16 (1.06–1.28) | 1.01 (0.89–1.14) | 0.82 (0.73–0.92) | < 0.0001 | |
| Model 3 | 0.94 (0.92–0.96) | Reference | 1.12 (0.96–1.31) | 1.04 (0.85–1.26) | 0.77 (0.64–0.93) | 0.0002 | |
| Model 4 | 0.99 (0.96–1.01) | Reference | 1.05 (1.00–1.10) | 0.93 (0.87–0.99) | 0.94 (0.89–0.99) | < 0.0001 | |
| Current treatment | |||||||
| Unadjusted model | 0.94 (0.91–0.98) | Reference | 1.06 (0.98–1.15) | 1.02 (0.91–1.13) | 0.90 (0.82–0.99) | 0.0036 | |
| Model 1 | 0.96 (0.93–1.00) | Reference | 1.14 (1.04–1.26) | 1.07 (0.94–1.21) | 0.85 (0.76–0.95) | < 0.0001 | |
| Model 2 | 0.96 (0.93–1.00) | Reference | 1.12 (0.95–1.31) | 1.06 (0.86–1.30) | 0.78 (0.65–0.94) | 0.0005 | |
| Model 3 | 0.97 (0.93–1.01) | Reference | 1.03 (0.98–1.08) | 1.00 (0.94–1.07) | 0.99 (0.93–1.04) | 0.4570 | |
| Model 4 | 0.98 (0.94–1.02) | Reference | 1.06 (0.97–1.15) | 1.03 (0.93–1.15) | 0.91 (0.82–1.00) | 0.0104 | |
| Variables | Moderate physical activity | |||
|---|---|---|---|---|
| Yes | No | |||
| Atopic dermatitis (Physician's diagnosis) | ||||
| Two time increase in green areas | 0.90 (0.83–0.98) | 0.96 (0.90–1.01) | ||
| Quartiles of green areas | ||||
| Q1 (≤ 14.90) | Reference | Reference | ||
| Q2 (14.90–22.40) | 0.69 (0.58–0.84) | 0.96 (0.86–1.07) | ||
| Q3 (22.41–33.30) | 0.86 (0.69–1.06) | 0.96 (0.84–1.11) | ||
| Q4 (≥ 33.31) | 0.70 (0.58–0.85) | 0.76 (0.67–0.86) | ||
| Trend p-valuea | < 0.0001 | 0.0001 | ||
| Atopic dermatitis (Current treatment) | ||||
| Two time increase in green areas | 0.79 (0.68–0.91) | 0.97 (0.89–1.06) | ||
| Quartiles of green areas | ||||
| Q1 (≤ 14.90) | Reference | Reference | ||
| Q2 (14.90–22.40) | 0.54 (0.40–0.73) | 1.07 (0.89–1.28) | ||
| Q3 (22.41–33.30) | 0.64 (0.46–0.89) | 1.09 (0.86–1.39) | ||
| Q4 (≥ 33.31) | 0.56 (0.41–0.77) | 0.76 (0.62–0.93) | ||
| Trend p-valuea | < 0.0001 | 0.0046 | ||
| Allergic rhinitis (Physician's diagnosis) | ||||
| Two time increase in green areas | 0.99 (0.95–1.03) | 0.99 (0.96–1.02) | ||
| Quartiles of green areas | ||||
| Q1 (≤ 14.90) | Reference | Reference | ||
| Q2 (14.90–22.40) | 0.98 (0.90–1.07) | 0.97 (0.92–1.03) | ||
| Q3 (22.41–33.30) | 1.05 (0.95–1.17) | 0.94 (0.88–1.02) | ||
| Q4 (≥ 33.31) | 0.97 (0.88–1.06) | 0.96 (0.90–1.02) | ||
| Trend p-valuea | 0.4428 | 0.3789 | ||
| Allergic rhinitis (Current treatment) | ||||
| Two time increase in green areas | 0.99 (0.92–1.07) | 0.97 (0.92–1.02) | ||
| Quartiles of green areas | ||||
| Q1 (≤ 14.90) | Reference | Reference | ||
| Q2 (14.90–22.40) | 1.04 (0.89–1.22) | 0.91 (0.83–1.01) | ||
| Q3 (22.41–33.30) | 1.15 (0.97–1.36) | 0.92 (0.81–1.04) | ||
| Q4 (≥ 33.31) | 0.90 (0.77–1.06) | 0.85 (0.76–0.94) | ||
| Trend p-valuea | 0.0882 | 0.0215 | ||
Values are expressed as mean±standard deviation or number (%).
KRW: Korea Won; BMI: body mass index.
Model 1 was adjusted by age, sex, marriage, education, monthly income, and job categories; Model 2 was further adjusted for smoking and alcohol; Model 3 was further adjusted for physical activity and self-reported stress; Model 4 was further adjusted for urbanity and body mass index.
aTrend
Model 1 was adjusted by age, sex, marriage, education, monthly income, and job categories; Model 2 was further adjusted for smoking and alcohol; Model 3 was further adjusted for physical activity and self-reported stress; Model 4 was further adjusted for urbanity and body mass index.
aTrend
The results were adjusted by age, sex, marriage, education, monthly income, job categories, smoking, alcohol, self-reported stress, urbanity, and body mass index.
aTrend
 KSOEM
KSOEM

 Cite
Cite

