Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 32; 2020 > Article
- Research Article Multidimensional sleep quality of dependent self-employment workers
-
Sang Ha Lee1
 , Dukyun Kang1
, Dukyun Kang1 , Junhyeong Lee1
, Junhyeong Lee1 , Uijin Kim1, Seunghon Ham2
, Uijin Kim1, Seunghon Ham2 , Wanhyung Lee2
, Wanhyung Lee2 , Won-Jun Choi2
, Won-Jun Choi2 , Seong-Kyu Kang2
, Seong-Kyu Kang2
-
Annals of Occupational and Environmental Medicine 2020;32:e6.
DOI: https://doi.org/10.35371/aoem.2020.32.e6
Published online: January 22, 2020
1Department of Occupational and Environmental Medicine, Gil Medical Center, Gachon University, Incheon, Korea.
2Department of Occupational and Environmental Medicine, Gachon University College of Medicine, Incheon, Korea.
- Correspondence: Seong-Kyu Kang. Department of Occupational and Environmental Medicine, Gachon University College of Medicine, 21 Namdong-daero 774 beon-gil, Namdong-gu, Incheon 21565, Korea. sk.kang@gachon.ac.kr
Copyright © 2020 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background The number of workers in non-standard employment (NSE) is increasing due to industrial change and technological development. Dependent self-employment (DSE), a type of NSE, was created decades ago. Despite the problems associated with this new type of employment, few studies have been conducted on the effects by DSE on health, especially sleep quality. This study aims to determine the relationship between DSE and sleep quality.
-
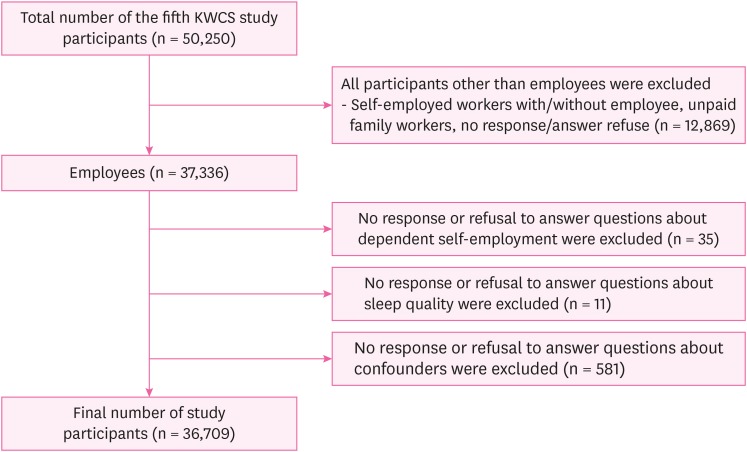
Methods This study analyzed data of 50,250 wage workers from the fifth Korean Working Conditions Survey. Workers that did not respond or refused to answer any questions related to variables were excluded, and finally 36,709 participants were included in this study. A total of 2,287 workers (6.2%) were compared with non-DSE (34,422; 93.8%) workers, and multiple logistic regression analyses were applied.
-
Results DSE status had a significant association with difficulty falling asleep (odds ratio [OR]: 1.331, 95% confidence interval [CI]: 1.178–1.504), difficulty maintaining sleep (OR: 1.279; 95% CI: 1.125–1.455), and extreme fatigue after waking up (OR: 1.331; 95% CI: 1.184–1.496). A multiple logistic regression of the variables for sleep quality in DSE showed a significant association with exposure to physical factors for all types of poor sleep quality as well as shift work for difficulty maintaining sleep with extreme fatigue after waking up. Long working hours and emotional labor were also associated with extreme fatigue after waking up.
-
Conclusions This study shows a significant association between DSE and poor sleep quality, especially when workers were exposed to physical risk factors (noise, vibration, abnormal temperature, etc.) and shift work.
BACKGROUND
METHODS
RESULTS
General characteristics of participants based on dependent self-employment
ORs of dependent self-employment associated with sleep quality
ORs of variables associated with sleep quality in a group of dependent self-employment
DISCUSSION
CONCLUSIONS
Abbreviations
NSE
DSE
OR
CI
ILO
EWCS
OSH
OSHRI
KWCS
KRW
REM
-
Competing interests: The authors declare that they have no competing interest.
-
Author Contributions:
NOTES
- 1. International Labour Office. Non-standard employment around the world: understanding challenges, shaping prospects. Geneva: International Labour Office; 2016.
- 2. International Labour Organization. Non-standard forms of employment: report for discussion at the meeting of experts on non-standard forms of employment. Geneva: International Labour Organization; 2015.
- 3. Quinlan M. The effects of non-standard forms of employment on worker health and safety. Geneva: International Labour Office; 2015.
- 4. Kim IH, Muntaner C, Khang YH, Paek D, Cho SI. The relationship between nonstandard working and mental health in a representative sample of the South Korean population. Soc Sci Med 2006;63(3):566–574. 16580108.ArticlePubMed
- 5. Williams CC, Lapeyre F. Dependent self-employment: trends, challenges and policy responses in the EU. Geneva: International Labour Organization; 2017.
- 6. Seon JJ, Lim YJ, Lee HW, Yoon JM, Kim SJ, Choi S, et al. Cardiovascular health status between standard and nonstandard workers in Korea. PLoS One 2017;12(6):e0178395. 28570650.ArticlePubMedPMC
- 7. Ahn J, Kim NS, Lee BK, Park J, Kim Y. Non-standard workers have poorer physical and mental health than standard workers. J Occup Environ Med 2019;61(10):e413–21. 31348413.ArticlePubMed
- 8. Williams CC, Horodnic IA. Evaluating the prevalence and distribution of dependent self-employment: some lessons from the European Working Conditions Survey. Ind Relat J 2018;49(2):109–127.ArticlePDF
- 9. Kim YS, Rhee KY, Oh MJ, Park J. The validity and reliability of the second Korean working conditions survey. Saf Health Work 2013;4(2):111–116. 23961335.ArticlePubMedPMC
- 10. Seo HJ. Development of a tailored analysis system for Korean working conditions survey. Saf Health Work 2016;7(3):201–207. 27630788.ArticlePubMedPMC
- 11. Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH. The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Med Rev 2015;22:23–36. 25454674.ArticlePubMedPMC
- 12. Drake C, Richardson G, Roehrs T, Scofield H, Roth T. Vulnerability to stress-related sleep disturbance and hyperarousal. Sleep 2004;27(2):285–291. 15124724.ArticlePubMed
- 13. Suen LK, Tam WW, Hon KL. Association of sleep hygiene-related factors and sleep quality among university students in Hong Kong. Hong Kong Med J 2010;16(3):180–185. 20519753.PubMed
- 14. Zee PC, Vitiello MV. Circadian rhythm sleep disorder: irregular sleep wake rhythm type. Sleep Med Clin 2009;4(2):213–218. 20160950.PubMedPMC
- 15. Lu BS, Zee PC. Circadian rhythm sleep disorders. Chest 2006;130(6):1915–1923. 17167016.ArticlePubMed
- 16. Kang JH, Chen SC. Effects of an irregular bedtime schedule on sleep quality, daytime sleepiness, and fatigue among university students in Taiwan. BMC Public Health 2009;9(1):248. 19615098.ArticlePubMedPMCPDF
- 17. Mai QD, Hill TD, Vila-Henninger L, Grandner MA. Employment insecurity and sleep disturbance: evidence from 31 European countries. J Sleep Res 2019;28(1):e12763. 30156336.ArticlePubMedPMCPDF
- 18. Costa G. Shift work and health: current problems and preventive actions. Saf Health Work 2010;1(2):112–123. 22953171.ArticlePubMedPMC
- 19. Fortier-Brochu E, Beaulieu-Bonneau S, Ivers H, Morin CM. Insomnia and daytime cognitive performance: a meta-analysis. Sleep Med Rev 2012;16(1):83–94. 21636297.ArticlePubMed
- 20. Swanson LM, Arnedt JT, Rosekind MR, Belenky G, Balkin TJ, Drake C. Sleep disorders and work performance: findings from the 2008 National Sleep Foundation Sleep in America poll. J Sleep Res 2011;20(3):487–494. 20887396.ArticlePubMed
- 21. Giraudo M, Bena A, Leombruni R, Costa G. Occupational injuries in times of labour market flexibility: the different stories of employment-secure and precarious workers. BMC Public Health 2016;16(1):150. 26874687.ArticlePubMedPMCPDF
- 22. Fruhstorfer B, Fruhstorfer H, Grass P. Daytime noise and subsequent night sleep in man. Eur J Appl Physiol Occup Physiol 1984;53(2):159–163. 6542514.ArticlePubMedPDF
- 23. Gitanjali B, Ananth R. Effect of acute exposure to loud occupational noise during daytime on the nocturnal sleep architecture, heart rate, and cortisol secretion in healthy volunteers. J Occup Health 2003;45(3):146–152. 14646289.ArticlePubMedPDF
- 24. Legault G. Sleep and heat related changes in the cognitive performance of underground miners: a possible health and safety concern. Minerals (Basel) 2011;1(1):49–72.Article
- 25. Cagnacci A, Elliott JA, Yen SS. Melatonin: a major regulator of the circadian rhythm of core temperature in humans. J Clin Endocrinol Metab 1992;75(2):447–452. 1639946.ArticlePubMed
- 26. Aoki K, Stephens DP, Zhao K, Kosiba WA, Johnson JM. Modification of cutaneous vasodilator response to heat stress by daytime exogenous melatonin administration. Am J Physiol Regul Integr Comp Physiol 2006;291(3):R619–24. 16690775.ArticlePubMed
- 27. Ishibashi K, Arikura S, Kozaki T, Higuchi S, Yasukouchi A. Thermoregulatory effect in humans of suppressed endogenous melatonin by pre-sleep bright-light exposure in a cold environment. Chronobiol Int 2010;27(4):782–806. 20560711.ArticlePubMed
- 28. Kazemi R, Motamedzade M, Golmohammadi R, Mokarami H, Hemmatjo R, Heidarimoghadam R. Field study of effects of night shifts on cognitive performance, salivary melatonin, and sleep. Saf Health Work 2018;9(2):203–209. 29928535.ArticlePubMedPMC
- 29. Yong LC, Li J, Calvert GM. Sleep-related problems in the US working population: prevalence and association with shiftwork status. Occup Environ Med 2017;74(2):93–104. 27609325.ArticlePubMed
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Teleworking Is Significantly Associated with Anxiety Symptoms and Sleep Disturbances among Paid Workers in the COVID-19 Era
Minji Kim, Inho Park, Hyojin An, Byungyoon Yun, Jin-Ha Yoon
International Journal of Environmental Research and Public Health.2023; 20(2): 1488. CrossRef - Self-employment and health inequality of migrant workers
Deshui Zhou, Xin Wen
BMC Health Services Research.2022;[Epub] CrossRef - Mental health symptoms among dependent contractors in Korea: a cross-sectional study based on the Fifth Korean Working Condition Survey
Seong-Uk Baek, Sung-Shil Lim, Sehyun Yun, Won-Tae Lee, Min-Seok Kim, Jin-Ha Yoon, Jong-Uk Won
Annals of Occupational and Environmental Medicine.2022;[Epub] CrossRef - The Effect of Job Demands, Job Resources, and Musculoskeletal Complaints on Presenteeism Among the Dependent Self-employment Workers in Korea
Jiyun Kim, Sookja Choi
Journal of Occupational & Environmental Medicine.2022; 64(9): 719. CrossRef - Association between physical risk factors and sleep disturbance among workers in Korea: The 5th Korean Working Conditions Survey
Inho Park, Seunghan Kim, Yangwook Kim, Byungyoon Yun, Jin-Ha Yoon
Sleep Medicine.2022; 100: 157. CrossRef - The Impact of Mandate Contract and Self-Employment on Workers’ Health—Evidence from Poland
Katarzyna Piwowar-Sulej, Dominika Bąk-Grabowska
International Journal of Environmental Research and Public Health.2021; 18(6): 3138. CrossRef
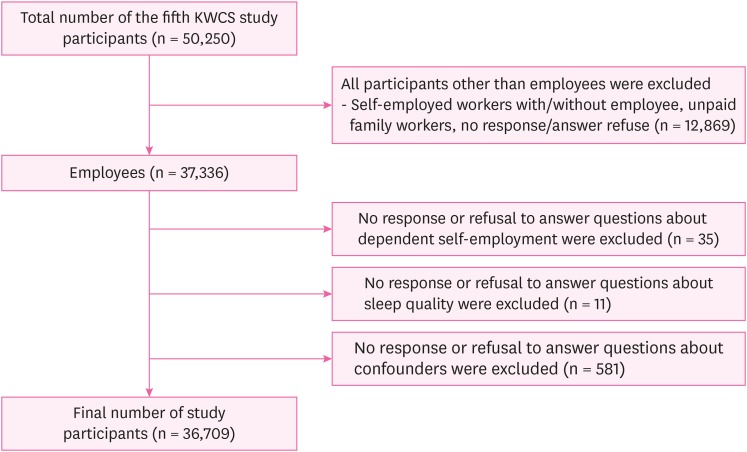
Fig. 1
| Characteristics | Total | Dependent self-employment | |||
|---|---|---|---|---|---|
| Yes | No | p-value | |||
| Total | 36,709 (100.0) | 2,287 (6.2) | 34,422 (93.8) | ||
| Sex | < 0.001 | ||||
| Male | 20,792 (56.6) | 1,110 (48.5) | 19,682 (57.2) | ||
| Female | 15,917 (43.4) | 1,177 (51.5) | 14,740 (42.8) | ||
| Age (years) | < 0.001 | ||||
| < 40 | 15,932 (43.4) | 797 (34.8) | 15,135 (44.0) | ||
| 40–49 | 9,284 (25.3) | 627 (27.4) | 8,657 (25.1) | ||
| 50–59 | 7,382 (20.1) | 605 (26.4) | 6,777 (19.7) | ||
| ≥ 60 | 4,113 (11.2) | 259 (11.3) | 3,854 (11.2) | ||
| Monthly income (10,000 won) | < 0.001 | ||||
| < 200 | 12,406 (33.8) | 648 (28.3) | 11,758 (34.2) | ||
| 200–300 | 10,473 (28.5) | 773 (33.8) | 9,700 (28.2) | ||
| 300–400 | 7,734 (21.1) | 536 (23.4) | 7,198 (20.9) | ||
| ≥ 400 | 6,096 (16.6) | 330 (14.4) | 5,766 (16.8) | ||
| Occupational classification | < 0.001 | ||||
| White-collar | 17,072 (46.5) | 539 (23.6) | 16,533 (48.0) | ||
| Yellow-collar | 8,830 (24.1) | 1,197 (52.3) | 7,633 (22.2) | ||
| Blue-collar | 10,808 (29.4) | 552 (24.1) | 10,256 (29.8) | ||
| Working hours per week (> 52 hours) | < 0.001 | ||||
| No | 31,959 (87.1) | 1,874 (81.9) | 30,085 (87.4) | ||
| Yes | 4,750 (12.9) | 413 (18.1) | 4,337 (12.6) | ||
| Shift work | < 0.001 | ||||
| No | 32,367 (88.2) | 2,125 (92.9) | 30,242 (87.9) | ||
| Yes | 4,340 (11.8) | 162 (7.1) | 4,180 (12.1) | ||
| Exposure to physical factors | 0.346 | ||||
| No | 23,329 (63.5) | 1,475 (64.5) | 21,854 (63.5) | ||
| Yes | 13,381 (36.5) | 813 (35.5) | 12,568 (36.5) | ||
| Emotional labor | < 0.001 | ||||
| No | 15,986 (43.5) | 424 (18,5) | 15,562 (45.2) | ||
| Yes | 20,723 (56.5) | 1,863 (81.5) | 18,860 (54.8) | ||
| Difficulty falling asleep | < 0.001 | ||||
| No | 32,489 (88.5) | 1,933 (84.5) | 30,556 (88.8) | ||
| Yes | 4,220 (11.5) | 354 (15.5) | 3,866 (11.2) | ||
| Difficulty maintaining sleep | < 0.001 | ||||
| No | 32,831 (89.4) | 1,976 (86.4) | 30,855 (89.6) | ||
| Yes | 3,880 (10.6) | 312 (13.6) | 3,568 (10.4) | ||
| Extreme fatigue after waking up | < 0.001 | ||||
| No | 31,977 (87.1) | 1,888 (82.6) | 30,089 (87.4) | ||
| Yes | 4,732 (12.9) | 399 (17.4) | 4,333 (12.6) | ||
| Variables | Difficulty falling asleep | Difficulty maintaining sleep | Extreme fatigue after waking up | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | CI | p-value | OR | CI | p-value | OR | CI | p-value | ||
| Dependent self-employment | ||||||||||
| No | Ref. | Ref. | Ref. | |||||||
| Yes | 1.331 | 1.178–1.504 | < 0.001 | 1.279 | 1.125–1.455 | < 0.001 | 1.331 | 1.184–1.496 | < 0.001 | |
| Sex (female) | ||||||||||
| Male | Ref. | Ref. | Ref. | |||||||
| Female | 1.109 | 1.026–1.199 | 0.009 | 1.245 | 1.147–1.350 | < 0.001 | 1.180 | 1.095–1.272 | < 0.001 | |
| Age (years) | ||||||||||
| < 40 | Ref. | Ref. | Ref. | |||||||
| 40–49 | 1.045 | 0.960–1.138 | 0.305 | 1.143 | 1.046–1.249 | 0.003 | 1.103 | 1.017–1.195 | 0.017 | |
| 50–59 | 1.164 | 1.064–1.274 | 0.001 | 1.296 | 1.180–1.423 | < 0.001 | 1.151 | 1.056–1.255 | 0.001 | |
| ≥ 60 | 1.219 | 1.088–1.367 | 0.001 | 1.454 | 1.295–1.631 | < 0.001 | 1.177 | 1.056–1.312 | 0.003 | |
| Monthly income (10,000 won) | ||||||||||
| < 200 | Ref. | Ref. | Ref. | |||||||
| 200–300 | 0.807 | 0.740–0.880 | < 0.001 | 0.832 | 0.760–0.911 | < 0.001 | 0.915 | 0.841–0.994 | 0.036 | |
| 300–400 | 0.775 | 0.698–0.861 | < 0.001 | 0.766 | 0.686–0.856 | < 0.001 | 0.930 | 0.842–1.028 | 0.154 | |
| ≥ 400 | 0.892 | 0.795–1.002 | 0.053 | 1.011 | 0.898–1.138 | 0.858 | 1.058 | 0.947–1.182 | 0.315 | |
| Occupational classification | ||||||||||
| White-collar | Ref. | Ref. | Ref. | |||||||
| Yellow-collar | 0.947 | 0.867–1.035 | 0.231 | 0.824 | 0.750–0.906 | < 0.001 | 0.924 | 0.847–1.008 | 0.074 | |
| Blue-collar | 0.825 | 0.749–0.908 | < 0.001 | 0.853 | 0.773–0.942 | 0.002 | 1.025 | 0.936–1.121 | 0.597 | |
| Working hours per week (> 52 hours) | ||||||||||
| No | Ref. | Ref. | Ref. | |||||||
| Yes | 1.219 | 1.110–1.339 | < 0.001 | 1.387 | 1.261–1.524 | < 0.001 | 1.471 | 1.350–1.602 | < 0.001 | |
| Shift work | ||||||||||
| No | Ref. | Ref. | Ref. | |||||||
| Yes | 1.261 | 1.146–1.386 | < 0.001 | 1.210 | 1.095–1.336 | < 0.001 | 1.266 | 1.157–1.385 | < 0.001 | |
| Exposure to physical factors | ||||||||||
| No | Ref. | Ref. | Ref. | |||||||
| Yes | 1.398 | 1.302–1.501 | < 0.001 | 1.702 | 1.582–1.831 | < 0.001 | 1.836 | 1.717–1.964 | < 0.001 | |
| Emotional labor | ||||||||||
| No | Ref. | Ref. | Ref. | |||||||
| Yes | 1.465 | 1.361–1.576 | < 0.001 | 1.438 | 1.333–1.550 | < 0.001 | 1.564 | 1.459–1.678 | < 0.001 | |
| Variables | Difficulty falling asleep | Difficulty maintaining sleep | Extreme fatigue after waking up | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | CI | p-value | OR | CI | p-value | OR | CI | p-value | ||
| Sex (female) | ||||||||||
| Male | Ref. | Ref. | Ref. | |||||||
| Female | 0.917 | 0.699–1.203 | 0.533 | 1.262 | 0.971–1.641 | 0.082 | 1.051 | 0.806–1.371 | 0.713 | |
| Age (years) | ||||||||||
| < 40 | Ref. | Ref. | Ref. | |||||||
| 40–49 | 0.816 | 0.606–1.100 | 0.182 | 0.825 | 0.595–1.145 | 0.250 | 1.397 | 1.045–1.866 | 0.024 | |
| 50–59 | 0.874 | 0.647–1.181 | 0.381 | 1.070 | 0.780–1.468 | 0.676 | 1.186 | 0.877–1.603 | 0.268 | |
| ≥ 60 | 0.613 | 0.389–0.965 | 0.034 | 1.088 | 0.709–1.671 | 0.699 | 1.181 | 0.787–1.771 | 0.422 | |
| Monthly income (10,000 won) | ||||||||||
| < 200 | Ref. | Ref. | Ref. | |||||||
| 200–300 | 0.811 | 0.595–1.106 | 0.186 | 0.828 | 0.601–1.140 | 0.247 | 0.990 | 0.739–1.328 | 0.948 | |
| 300–400 | 0.855 | 0.603–1.214 | 0.383 | 0.947 | 0.658–1.365 | 0.771 | 1.217 | 0.892–1.662 | 0.216 | |
| ≥ 400 | 1.402 | 0.956–2.055 | 0.083 | 1.208 | 0.798–1.828 | 0.371 | 1.636 | 1.159–2.309 | 0.005 | |
| Occupational classification | ||||||||||
| White-collar | Ref. | Ref. | Ref. | |||||||
| Yellow-collar | 1.102 | 0.824–1.472 | 0.514 | 0.870 | 0.646–1.172 | 0.360 | 0.867 | 0.651–1.155 | 0.329 | |
| Blue-collar | 0.816 | 0.549–1.213 | 0.315 | 0.661 | 0.454–0.964 | 0.032 | 0.806 | 0.558–1.164 | 0.250 | |
| Working hours per week (> 52 hours) | ||||||||||
| No | Ref. | Ref. | Ref. | |||||||
| Yes | 1.203 | 0.887–1.632 | 0.235 | 1.357 | 0.993–1.855 | 0.055 | 1.603 | 1.232–2.086 | < 0.001 | |
| Shift work | ||||||||||
| No | Ref. | Ref. | Ref. | |||||||
| Yes | 1.023 | 0.649–1.613 | 0.922 | 1.703 | 1.122–2.584 | 0.012 | 1.604 | 1.096–2.346 | 0.015 | |
| Exposure to physical factors | ||||||||||
| No | Ref. | Ref. | Ref. | |||||||
| Yes | 1.474 | 1.151–1.886 | 0.002 | 1.781 | 1.379–2.301 | < 0.001 | 2.234 | 1.784–2.798 | < 0.001 | |
| Emotional labor | ||||||||||
| No | Ref. | Ref. | Ref. | |||||||
| Yes | 1.132 | 0.822–1.557 | 0.448 | 1.012 | 0.729–1.404 | 0.944 | 1.373 | 1.019–1.850 | 0.037 | |
Values are presented as number (%).
Statistical estimated from a multivariate logistic model that adjusted for all other covariates excluding an interesting variant.
OR: odds ration; CI: confidence interval.
Statistical estimated from a multivariate logistic model that adjusted for all other covariates excluding an interesting variant.
OR: odds ration; CI: confidence interval.
 KSOEM
KSOEM

 Cite
Cite

