Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 30; 2018 > Article
- Research Article Association between serum ferritin and hypertension according to the working type in Korean men: the fifth Korean National Health and nutrition examination survey 2010–2012
-
Dong-Hoon Lee1, Seong-Kyu Kang1,2
 , Won-Jun Choi1,2, Kyeong Min Kwak1, Dukyun Kang1, Sang Ha Lee1, Jun-Hyung Lee1
, Won-Jun Choi1,2, Kyeong Min Kwak1, Dukyun Kang1, Sang Ha Lee1, Jun-Hyung Lee1 -
Annals of Occupational and Environmental Medicine 2018;30:40.
DOI: https://doi.org/10.1186/s40557-018-0251-y
Published online: June 11, 2018
1Department of Occupational and Environmental Medicine, Gachon University Gil Medical Center, 21 Namdong-daero 774 beon-gil, Namdong-gu, Incheon, 21565 Republic of Korea
2Department of Occupational and Environmental Medicine, College of Medicine, Gachon University, 38-13 Dokjeom-ro 3 beon-gil, Namdongogu, Incheon, 21565 Republic of Korea
© The Author(s). 2018
Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Abstract
-
Background Several studies suggest that serum ferritin concentrations reflect systemic inflammation, and high ferritin levels can increase the risk of hypertension in adult men. Shift work is also known to increase the risk of hypertension; however, there has been no study about the relationship between serum ferritin levels and the prevalence of hypertension according to the working type.
-
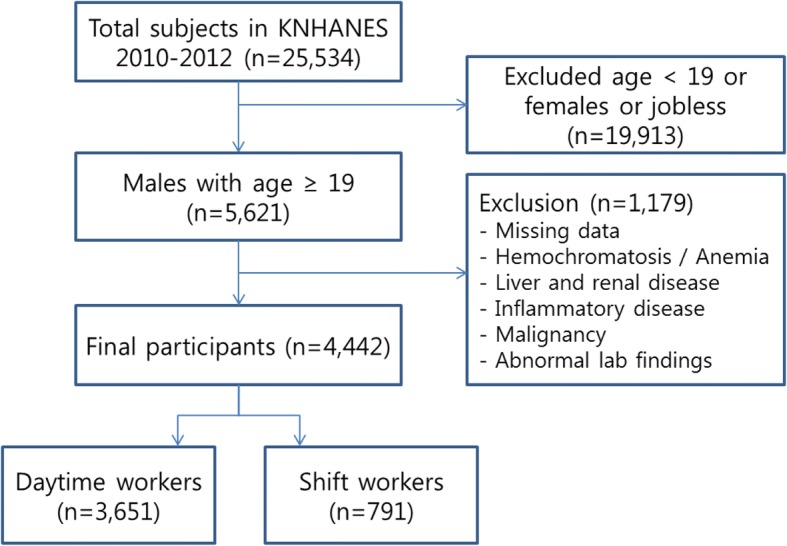
Methods This cross-sectional study included 4,442 male participants (3,651 daytime workers and 791 shift workers) who participated in the fifth Korean National Health and Nutrition Examination Survey. Hypertension was defined as a systolic blood pressure greater than or equal to 140 mmHg, a diastolic blood pressure greater than or equal to 90 mmHg or the current use of antihypertensive medications regardless of blood pressure values. For the statistical analyses, serum ferritin levels were reclassified into quartiles, and complex sample analyses were used to evaluate the relationship between serum ferritin levels and the prevalence of hypertension according to the working type in this study.
-
Results Serum ferritin and shift work were positively associated with the prevalence of hypertension. The effect of interaction was above multiplicative. When compared to participants in the lowest serum ferritin quartile, the odds ratio for hypertension for participants in the highest serum ferritin quartile was 1.372 (1.027–1.833) in daytime workers and 2.009 (1.042–3.873) in shift workers after adjustment.
-
Conclusions The prevalence of hypertension increased as ferritin levels increased in individuals, especially in shift workers.
Background
Methods
Results
| Variables | Odds ratio (95% confidence intervals)a | |
|---|---|---|
| Quartile 1 (≤ 66.82) | Quartile 4 (> 149.13) | |
| Daytime workers | 1.000 (ref.) | 1.426 (1.066–1.906) |
| Shift workers | 1.035 (0.680–1.576) | 1.696 (1.083–2.658) |
Discussion
Conclusions
Abbreviations
ALT
AST
BMI
CI
DBP
FBS
Hb
KNHANES
OR
SBP
TC
TIBC
VitD
WBC
WC
- 1. Naito Y, Hirotani S, Sawada H, Akahori H, Tsujino T, Masuyama T. Dietary iron restriction prevents hypertensive cardiovascular remodeling in dahl salt-sensitive rats. Hypertension 2011;57:497–504. 10.1161/HYPERTENSIONAHA.110.159681. 21263124.ArticlePubMed
- 2. Dominguez-Rodriguez A, Tome MC-P, Hernandez-Garcia C, Arroyo-Ucar E, Juarez-Prera R, Blanco-Palacios G, et al. Serum ferritin and acute coronary syndrome: a strong prognostic factor? Int J Cardiol 2011;152:129–130. 10.1016/j.ijcard.2011.07.052. 21856027.ArticlePubMed
- 3. Whittington C, Kowdley K. Haemochromatosis. Aliment Pharmacol Ther 2002;16:1963–1975. 10.1046/j.1365-2036.2002.01371.x. 12452931.ArticlePubMedPDF
- 4. Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 1999;340:448–454. 10.1056/NEJM199902113400607. 9971870.ArticlePubMed
- 5. Kalantar-Zadeh K, Don BR, Rodriguez RA, Humphreys MH. Serum ferritin is a marker of morbidity and mortality in hemodialysis patients. Am J Kidney Dis 2001;37:564–572. 10.1053/ajkd.2001.22433. 11228181.ArticlePubMed
- 6. Kalender B, Mutlu B, Ersöz M, Kalkan A, Yilmaz A. The effects of acute phase proteins on serum albumin, transferrin and haemoglobin in haemodialysis patients. Int J Clin Pract 2002;56:505–508. 12296612.ArticlePubMed
- 7. Jiang R, Manson JE, Meigs JB, Ma J, Rifai N, Hu FB. Body iron stores in relation to risk of type 2 diabetes in apparently healthy women. JAMA 2004;291:711–717. 10.1001/jama.291.6.711. 14871914.ArticlePubMed
- 8. Park SK, Choi WJ, Oh CM, Kim MG, Ham WT, Choi JM, et al. Clinical significance of serum ferritin level as an independent predictor of insulin resistance in Korean men. Diabetes Res Clin Pract 2015;107:187–193. 10.1016/j.diabres.2014.08.022. 25438938.ArticlePubMed
- 9. Lee BK, Kim Y, Kim YI. Association of serum ferritin with metabolic syndrome and diabetes mellitus in the south Korean general population according to the Korean National Health and nutrition examination survey 2008. Metabolism 2011;60:1416–1424. 10.1016/j.metabol.2011.02.008. 21489582.ArticlePubMed
- 10. Kang HT, Linton JA, Shim JY. Serum ferritin level is associated with the prevalence of metabolic syndrome in Korean adults: the 2007–2008 Korean National Health and nutrition examination survey. Clin Chim Acta 2012;413:636–641. 10.1016/j.cca.2011.12.011. 22212623.ArticlePubMed
- 11. Yoo KD, Ko SH, Park JE, Ahn YB, Yim HW, Lee WC, et al. High serum ferritin levels are associated with metabolic risk factors in non-obese Korean young adults: Korean National Health and nutrition examination survey (KNHANES) IV. Clin Endocrinol 2012;77:233–240. 10.1111/j.1365-2265.2011.04248.x.Article
- 12. Williams MJ, Poulton R, Williams S. Relationship of serum ferritin with cardiovascular risk factors and inflammation in young men and women. Atherosclerosis 2002;165:179–184. 10.1016/S0021-9150(02)00233-2. 12208485.ArticlePubMed
- 13. Gillum R. Association of serum ferritin and indices of body fat distribution and obesity in Mexican American men—the third National Health and nutrition examination survey. Int J Obes 2001;25:639. 10.1038/sj.ijo.0801561.ArticlePDF
- 14. Lecube A, Hernandez C, Pelegri D, Simo R. Factors accounting for high ferritin levels in obesity. Int J Obes 2008;32:1665–1669. 10.1038/ijo.2008.154.ArticlePDF
- 15. Choi B, Yeum KJ, Park SJ, Kim KN, Joo NS. Elevated serum ferritin and mercury concentrations are associated with hypertension; analysis of the fourth and fifth Korea national health and nutrition examination survey (KNHANES IV-2, 3, 2008–2009 and V-1, 2010). Environ Toxicol 2015;30:101–108. 10.1002/tox.21899. 23929718.ArticlePubMed
- 16. Kim MK, Baek KH, Song K-H, Kang MI, Choi JH, Bae JC, et al. Increased serum ferritin predicts the development of hypertension among middle-aged men. Am J Hypertens 2012;25:492–497. 10.1038/ajh.2011.241. 22278211.ArticlePubMed
- 17. Piperno A, Trombini P, Gelosa M, Mauri V, Pecci V, Vergani A, et al. Increased serum ferritin is common in men with essential hypertension. J Hypertens 2002;20:1513–1518. 10.1097/00004872-200208000-00013. 12172312.ArticlePubMed
- 18. Ryoo JH, Kim SY, Oh CM, Park SK, Kim E, Park SJ, et al. The incidental relationship between serum ferritin levels and hypertension. Int J Cardiol 2015;183:258–262. 10.1016/j.ijcard.2014.10.152. 25704911.ArticlePubMed
- 19. Ha MN, Kim JY, Park JS, Chung HK. Influence of shiftwork duration on blood pressure and heart rate variability in short rotating 8-hour shiftworkers. Korean J Occup Environ Med 2001;13:180–189.ArticlePDF
- 20. Suwazono Y, Nogawa K. Effect of shift work on blood pressure. Nihon rinsho Jap J Clin Med 2014;72:1497–1502.
- 21. Suwazono Y, Dochi M, Sakata K, Okubo Y, Oishi M, Tanaka K, et al. Shift work is a risk factor for increased blood pressure in Japanese men: a 14-year historical cohort study. Hypertension 2008;52:581–586. 10.1161/HYPERTENSIONAHA.108.114553. 18625889.ArticlePubMed
- 22.
- 23. Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med 2005;352:1685–1695. 10.1056/NEJMra043430. 15843671.ArticlePubMed
- 24. Haupt CM, Alte D, Dörr M, Robinson DM, Felix SB, John U, et al. The relation of exposure to shift work with atherosclerosis and myocardial infarction in a general population. Atherosclerosis 2008;201:205–211. 10.1016/j.atherosclerosis.2007.12.059. 18321520.ArticlePubMed
- 25. Puttonen S, Kivimäki M, Elovainio M, Pulkki-Råback L, Hintsanen M, Vahtera J, et al. Shift work in young adults and carotid artery intima–media thickness: the cardiovascular risk in young Finns study. Atherosclerosis 2009;205:608–613. 10.1016/j.atherosclerosis.2009.01.016. 19215924.ArticlePubMed
- 26. https://knhanes.cdc.go.kr/knhanes/sub03/sub03_02_02.do.
- 27. Sun L, Franco OH, Hu FB, Cai L, Yu Z, Li H, et al. Ferritin concentrations, metabolic syndrome, and type 2 diabetes in middle-aged and elderly chinese. J Clin Endocrinol Metab 2008;93:4690–4696. 10.1210/jc.2008-1159. 18796516.ArticlePubMed
- 28. Fearon IM, Faux SP. Oxidative stress and cardiovascular disease: novel tools give (free) radical insight. J Mol Cell Cardiol 2009;47:372–381. 10.1016/j.yjmcc.2009.05.013. 19481547.ArticlePubMed
- 29. Wang H, Li H, Hou Z, Pan L, Shen X, Li G. Role of oxidative stress in elevated blood pressure induced by high free fatty acids. Hypertens Res 2009;32:152–158. 10.1038/hr.2008.35. 19262475.ArticlePubMedPDF
- 30. Costa G. The problem: shiftwork. Chronobiol Int 1997;14:89–98. 10.3109/07420529709001147. 9095370.ArticlePubMed
- 31. Åkerstedt T. Shift work and disturbed sleep/wakefulness. Occup Med 2003;53:89–94. 10.1093/occmed/kqg046.Article
- 32. Knutsson A. Health disorders of shift workers. Occup Med 2003;53:103–108. 10.1093/occmed/kqg048.Article
- 33. Roh SC. Shiftwork duration and metabolic risk factors of cardiovascular disease. Korean J Occup Environ Med. 2003;15:132–139.ArticlePDF
- 34. Yeom JH, Sim CS, Lee J, Yun SH, Park SJ, Yoo CI, et al. Effect of shift work on hypertension: cross sectional study. Ann Occup Environ Med 2017;29:11. 10.1186/s40557-017-0166-z. 28400961.ArticlePubMedPMCPDF
REFERENCES
Notes
Figure & Data
REFERENCES
Citations

- Biochemical Profiles in Hypertension: Ferritin, Antioxidant Enzymes, and Mineral Levels in Blood Serum
Mohamed Salem, James Robenson
Cureus.2025;[Epub] CrossRef - Higher serum ferritins are associated with higher blood pressure: A cross-sectional study
Shaoli Li, Feilong Chen, Tao Li, Yijing Cheng, Guimin Huang, Dongqing Hou, Wenqian Liu, Tao Xu, Junting Liu
Medicine.2024; 103(12): e37485. CrossRef - Associations Between Genetically Predicted Iron Status and Cardiovascular Disease Risk: A Mendelian Randomization Study
Alexa Barad, Andrew G. Clark, Eva K. Pressman, Kimberly O. O'Brien
Journal of the American Heart Association.2024;[Epub] CrossRef - Is iron status associated with markers of non-communicable disease in adolescent Indian children?
S. Ghosh, T. Thomas, A. Kurpad, H. S. Sachdev
European Journal of Clinical Nutrition.2023; 77(2): 173. CrossRef - A proposed method for defining the required fortification level of micronutrients in foods: An example using iron
Santu Ghosh, Tinku Thomas, Raghu Pullakhandam, Krishnapillai Madhavan Nair, Harshpal S. Sachdev, Anura V. Kurpad
European Journal of Clinical Nutrition.2023; 77(4): 436. CrossRef - The associations between hematological parameters and the incidence of prehypertension and hypertension in children and adolescents: a prospective cohort study
Lan Huang, Cui Song, Qin Liu, Xiaoyue Liang, Yanling Ren, Daochao Huang, Xianmin Guan, Xizhou An, Xiaohua Liang
Hypertension Research.2023; 46(9): 2085. CrossRef - Dietary intakes of total, nonheme, and heme iron and hypertension risk: a longitudinal study from the China Health and Nutrition Survey
Shangling Wu, Peiyan Chen, Jingjing He, Zhaoyan Liu, Yi Sui, Keji Li, Aiping Fang
European Journal of Nutrition.2023; 62(8): 3251. CrossRef - Association between soluble transferrin receptor and systolic hypertension in adults: National Health and Nutrition Examination Survey (2007–2010 and 2015–2018)
Haoran Wang, Qianjin Qi, Shuaihua Song, Di Zhang, Li Feng
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - The association between serum ferritin and blood pressure in adult women: a large cross-sectional study
Andong He, Xiaofeng Yang, Yuzhen Ding, Lu Sun, Meiting Shi, Ruiman Li
Clinical and Experimental Hypertension.2022; 44(6): 523. CrossRef - Influence of serum ferritin combined with blood cadmium concentrations on blood pressure and hypertension: From the Korean National Health and Nutrition Examination Survey
Jeoung A. Kwon, Eunjung Park, Seyoung Kim, Byungmi Kim
Chemosphere.2022; 288: 132469. CrossRef - Role of Iron‐Related Oxidative Stress and Mitochondrial Dysfunction in Cardiovascular Diseases
Fang Yan, Kaifeng Li, Wenjuan Xing, Mingqing Dong, Mingliang Yi, Haifeng Zhang, Tao Li
Oxidative Medicine and Cellular Longevity.2022;[Epub] CrossRef - Appraising the Causal Association between Systemic Iron Status and Heart Failure Risk: A Mendelian Randomisation Study
Xingchen Wang, Xizhi Wang, Yingchao Gong, Xiaoou Chen, Danfeng Zhong, Jun Zhu, Lenan Zhuang, Jing Gao, Guosheng Fu, Xue Lu, Dongwu Lai
Nutrients.2022; 14(16): 3258. CrossRef - Maternal Iron Status in Early Pregnancy and Blood Pressure Throughout Pregnancy, Placental Hemodynamics, and the Risk of Gestational Hypertensive Disorders
Minerva J Taeubert, Clarissa J Wiertsema, Marijn J Vermeulen, Hugo G Quezada-Pinedo, Irwin K Reiss, Martina U Muckenthaler, Romy Gaillard
The Journal of Nutrition.2022; 152(2): 525. CrossRef - Correlation of Serum Ferritin and Adenosine Deaminase with Body Mass Index in Children: A cross-sectional study
Suchanda Sahu, Medha Menon, Joseph John
Indian Journal of Physiology and Pharmacology.2021; 65: 109. CrossRef - Telomere Length and Oxidative Stress and Its Relation with Metabolic Syndrome Components in the Aging
Graciela Gavia-García, Juana Rosado-Pérez, Taide Laurita Arista-Ugalde, Itzen Aguiñiga-Sánchez, Edelmiro Santiago-Osorio, Víctor Manuel Mendoza-Núñez
Biology.2021; 10(4): 253. CrossRef - Osmotic fragility in essential hypertension revisited: A correlation with Iron status and lipid profile
Z H Alhillawi, S R M Al-Ani, H K Al-Hakeim
Journal of Physics: Conference Series.2021; 1853(1): 012032. CrossRef - Iron in Cardiovascular Disease: Challenges and Potentials
Shizhen Li, Xiangyu Zhang
Frontiers in Cardiovascular Medicine.2021;[Epub] CrossRef - Evaluation of serum ferritin levels in patients of hypertension
Divmehar Kaur, Harvinder Singh, Maninder Kaur, G K Bedi, R P S Sibia
International Journal of Clinical Biochemistry and Research.2020; 7(3): 317. CrossRef - WITHDRAWN: Can Traditional Chinese Medicine provide insights into controlling the COVID-19 pandemic: Serpentinization-induced lithospheric long-wavelength magnetic anomalies in Proterozoic bedrocks in a weakened geomagnetic field mediate the aberrant tran
Moses Turkle Bility, Yash Agarwal, Sara Ho, Isabella Castronova, Cole Beatty, Shivkumar Biradar, Vanshika Narala, Nivitha Periyapatna, Yue Chen, Jean Nachega
Science of The Total Environment.2020; : 142830. CrossRef - Measuring plasma ferritin levels with two different methods: A comparison of roche cobas E601 versus roche cobas C501 (integrated modular system roche cobas 6000)
Durmuş Ayan, Sibel Soylemez
Journal of Medical Biochemistry.2019;[Epub] CrossRef - Markers of iron status, blood pressure and incident hypertension among Chinese adults
Yongjian Zhu, Gaiyun Chen, Yacong Bo, Yanhua Liu
Nutrition, Metabolism and Cardiovascular Diseases.2019; 29(8): 830. CrossRef - The Moderating Effect of Shift Work on Lipid Pathway: An Application of Multi-Group Path Analysis Model
Shokofeh Maleki, Mohammad Gholami Fesharaki, Mohsen Rowzati
Iranian Red Crescent Medical Journal.2018;[Epub] CrossRef
- Figure
- Related articles
-
- Relationship between long-term PM2.5 exposure and myopia prevalence in adults: analysis of the Korea National Health and Nutrition Examination Survey–Air Pollution Linked Data, 2020
- Association between single-person household wage workers in South Korea and insomnia symptoms: the 6th Korean Working Conditions Survey (KWCS)
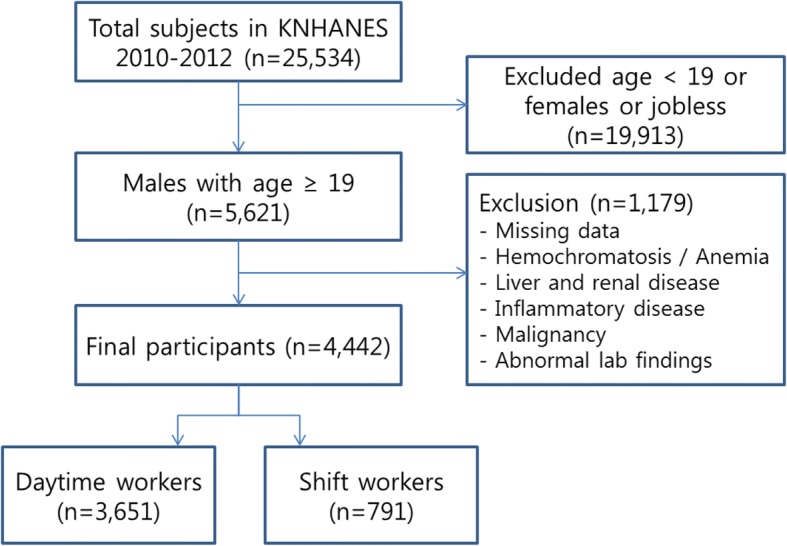
Fig. 1
| Variables | Quartiles of serum ferritin (ng/mL) | ||||
| Quartile 1 (≤ 66.82) | Quartile 2 (66.83–100.78) | Quartile 3 (100.79–149.13) | Quartile 4 (> 149.13) | P for trend | |
| N | 1111 | 1110 | 1111 | 1110 | |
| Age (year) | 43.87 (0.512) | 42.10 (0.486) | 42.34 (0.459) | 42.31 (0.443) | 0.025 |
| SBP (mm Hg) | 119.58 (0.503) | 119.15 (0.553) | 119.26 (0.545) | 120.95 (0.522) | 0.083 |
| DBP (mm Hg) | 78.96 (0.411) | 79.41 (0.422) | 79.65 (0.392) | 81.58 (0.400) | < 0.001 |
| WC (cm) | 82.29 (0.311) | 83.97 (0.376) | 84.11 (0.338) | 86.05 (0.377) | < 0.001 |
| BMI (kg/m2) | 23.56 (0.106) | 24.14 (0.132) | 24.20 (0.116) | 24.82 (0.141) | < 0.001 |
| FBS (mg/dL) | 95.48 (0.613) | 96.63 (0.673) | 98.33 (0.893) | 101.28 (0.878) | < 0.001 |
| TC (mg/dL) | 184.81 (1.204) | 188.77 (1.180) | 191.67 (1.301) | 193.25 (1.396) | < 0.001 |
| Triglyceride (mg/dL) | 130.68 (3.151) | 143.87 (3.559) | 155.31 (4.443) | 182.03 (6.145) | < 0.001 |
| AST (IU/L) | 21.08 (0.245) | 21.89 (0.228) | 23.00 (0.292) | 24.38 (0.305) | < 0.001 |
| ALT (IU/L) | 20.72 (0.371) | 23.47 (0.433) | 24.78 (0.441) | 28.70 (0.548) | < 0.001 |
| Hb (g/dL) | 15.23 (0.039) | 15.45 (0.036) | 15.49 (0.033) | 15.60 (0.041) | < 0.001 |
| TIBC (μg/dL) | 320.41 (1.401) | 309.24 (1.316) | 306.42 (1.266) | 302.56 (1.539) | < 0.001 |
| Cr (mg/dL) | 0.95 (0.004) | 0.96 (0.005) | 0.96 (0.004) | 0.96 (0.004) | 0.011 |
| WBC (103/uL) | 6.20 (0.050) | 6.29 (0.054) | 6.31 (0.050) | 6.43 (0.051) | 0.001 |
| VitD (ng/mL) | 18.36 (0.249) | 18.35 (0.243) | 18.45 (0.243) | 18.13 (0.234) | 0.540 |
| Variables | Quartiles of serum ferritin (ng/mL) | ||||
| Quartile 1 (≤ 66.82) | Quartile 2 (66.83–100.78) | Quartile 3 (100.79–149.13) | Quartile 4 (> 149.13) | p-value | |
| Smoking status (%) | |||||
| Quit smoker or non-smoker | 681 (58.7) | 635 (52.5) | 586 (46.9) | 605 (50.7) | < 0.001 |
| Current smoker | 430 (41.3) | 473 (47.5) | 524 (53.1) | 504 (49.3) | |
| Alcohol intake (%) | |||||
| Less than once a month | 445 (37.1) | 339 (29.5) | 307 (28.3) | 258 (20.6) | < 0.001 |
| More than twice a month | 664 (62.9) | 764 (70.5) | 797 (71.7) | 845 (79.4) | |
| Hypertension (%) | |||||
| Hypertension (−) | 770 (74.8) | 760 (73.7) | 779 (73.0) | 723 (68.5) | 0.029 |
| Hypertension (+) | 341 (25.2) | 350 (26.3) | 332 (27.0) | 387 (31.5) | |
| Variables | Odds ratio (95% confidence intervals)a | |
|---|---|---|
| Quartile 1 (≤ 66.82) | Quartile 4 (> 149.13) | |
| Daytime workers | 1.000 (ref.) | 1.426 (1.066–1.906) |
| Shift workers | 1.035 (0.680–1.576) | 1.696 (1.083–2.658) |
| Odds ratio (95% confidence intervals) | ||||
|---|---|---|---|---|
| Variables | Daytime workers | Shift workers | ||
| Unadjusted | Adjusteda | Unadjusted | Adjusteda | |
| Quartiles of ferritin (ng/mL) | ||||
| Quartile 1 (≤ 66.82) | Ref. | Ref. | Ref. | Ref. |
| Quartile 2 (66.83–100.78) | 1.037 (0.811–1.327) | 1.125 (0.853–1.484) | 1.168 (0.690–1.976) | 1.364 (0.738–2.518) |
| Quartile 3 (100.79–149.13) | 1.127 (0.865–1.469) | 1.274 (0.959–1.691) | 0.958 (0.571–1.608) | 1.088 (0.582–2.031) |
| Quartile 4 (> 149.13) | 1.297 (1.015–1.657) | 1.372 (1.027–1.833) | 1.726 (1.015–2.935) | 2.009 (1.042–3.873) |
Data are presented as the mean (standard deviation), or numbers (percentages)
aLogistic regression analysis after adjusting for age, FBS, TC, TIBC, BMI, alcohol intake and smoking status
aAdjusted for age, FBS, TC, TIBC, BMI, alcohol intake and smoking status
 KSOEM
KSOEM

 Cite
Cite

