Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 28; 2016 > Article
- Review The impact of fire suppression tasks on firefighter hydration: a critical review with consideration of the utility of reported hydration measures
- Adam Walker1, Rodney Pope2, Robin Marc Orr2
-
Annals of Occupational and Environmental Medicine 2016;28:63.
DOI: https://doi.org/10.1186/s40557-016-0152-x
Published online: November 15, 2016
1Faculty of Health Sciences and Medicine, Bond Institute of Health and Sport, Bond University, Gold Coast, QLD 4226 Australia
2Tactical Research Unit, Bond University, Gold Coast, QLD 4226 Australia
© The Author(s). 2016
Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Abstract
-
Background Firefighting is a highly stressful occupation with unique physical challenges, apparel and environments that increase the potential for dehydration. Dehydration leaves the firefighter at risk of harm to their health, safety and performance. The purpose of this review was to critically analyse the current literature investigating the impact of fighting ‘live’ fires on firefighter hydration.
-
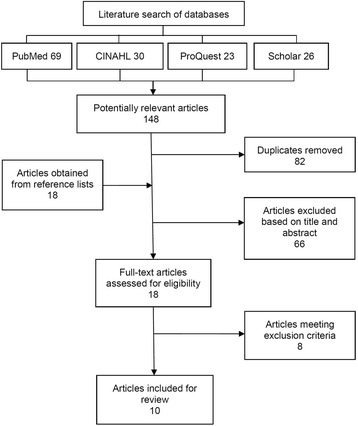
Methods A systematic search was performed of four electronic databases for relevant published studies investigating the impact of live fire suppression on firefighter hydration. Study eligibility was assessed using strict inclusion and exclusion criteria. The included studies were critically appraised using the Downs and Black protocol and graded according to the Kennelly grading system.
-
Results Ten studies met the eligibility criteria for this review. The average score for methodological quality was 55 %, ranging from 50 % (‘fair’ quality) to 61 % (‘good’ quality) with a ‘substantial agreement’ between raters (k = .772). Wildfire suppression was considered in five studies and structural fire suppression in five studies. Results varied across the studies, reflecting variations in outcome measures, hydration protocols and interventions. Three studies reported significant indicators of dehydration resulting from structural fire suppression, while two studies found mixed results, with some measures indicating dehydration and other measures an unchanged hydration status. Three studies found non-significant changes in hydration resulting from wildfire firefighting and two studies found significant improvements in markers of hydration. Ad libitum fluid intake was a common factor across the studies finding no, or less severe, dehydration.
-
Conclusions The evidence confirms that structural and wildfire firefighting can cause dehydration. Ad libitum drinking may be sufficient to maintain hydration in many wildfire environments but possibly not during intense, longer duration, hot structural fire operations. Future high quality research better quantifying the effects of these influences on the degree of dehydration is required to inform policies and procedures that ensure firefighter health and safety.
Background
Methods
Results
| Study | Participants | Outcome measure(s) | Intervention(s) | Major Findings | CAS (%) |
|---|---|---|---|---|---|
| Cuddy et al. [1] |
15 Hot Spot firefighters (12 male, 3 female) Wore PPE |
Water turnover Nude BW |
Live wildland fire suppression over 3 days of work shifts (11.4 ± 0.7 h/day) (hiking, line dragging, laying hose, chain sawing, clearing brush, lookout, and scouting) Ad libitum drinking 27.5 ± 3.2 °C mean ambient temperature |
No significant change (p = 0.12) in morning BW across 3 days (pre 77.3 ± 8.3 kg, post 77.0 ± 8.9 kg) Mean water turnover 9.5 ± 1.7 L/d |
54 (Fair) |
| Raines et al. [2] |
32 firefighters (31 male,1 female) Ad libitum(AD) group (n = 17), pre-shift (PR) group (n = 15) PPE |
Plasma Osm Urine colour USG |
PR group consumed 500 mL fluid bolus pre shift and ad libitum remainder of shift 7 days (9.9 ± 2.2 h/day AD, 9.7 ± 2.3 h/day PR) of wildfire suppression (intense but intermittent work, using chainsaws, applying water, carrying, transit time and briefings) Mild to warm ambient temperatures (15.8–26.4 °C) |
No difference between groups in total fluid intake (3.4 ± 1.6 L AD, 3.7 ± 2.9 L PR, p = 0.730) No significant differences between groups for any hydration marker (urine colour, p = 0.44; USG, p = 0.92; plasma Osm, p = 0.41) Significant decrease in both urine colour (p = 0.001) and USG (p = 0.01) across the shift, but still dehydrated by end, though less than at start Plasma Osm indicates firefighters arrived on shift dehydrated and finish dehydrated (p < 0.0001) |
57 (Fair) |
| Horn et al. [6] |
35 career, volunteer and industrial firefighters (31 male, 4 female) Wore PPE and SCBA |
Nude BW Urine colour USG Urine Osm Salivary Osm |
3 h live fire training exercise in specialised training building. 3–4 evolutions lasting 15–25 min, separated by 10–15 min (obtain water, advance hoses, extinguish fires, forcible entries, search and rescue and ventilation tasks) Encouraged ad libitum drinking (water and sport drink) Cool autumn day |
Significant BW loss of 1.1 ± 0.8 kg (p < 0.001) and 1.9 ± 0.9 kg (2.2 % BW loss) adjusted for fluid intake and voiding Significant (p < 0.001) increase in salivary Osm (pre 78.0 ± 21.5 mOsm/kg, post 49.0 ± 15 mOsm/kg), reflective of dehydration No significant (p > 0.05) changes in Urine Osm (pre 768 ± 260 mOsm/kg, post 712 ± 251 mOsm/kg), urine colour (pre score 5.8 ± 1.5, post score 5.3 ± 1.5), or USG (pre 1.025 ± 0.009, post 1.024 ± 0.009) |
61 (Good) |
| Holsworth et al. [7] |
9 volunteer firefighters (8 males, 1 female) WorePPE and SCBA |
HCT |
2 × 30 min strenuous live structural fires No fluid intake |
Significant (p = 0.0014) change in HCT (pre 43.7 ± 3.1 %, post 46.1 ± 2.3 %), indicating significant dehydration |
61 (Good) |
| Smith et al. [8] |
11 male professional firefighters WorePPE and SCBA (20.4 kg) |
HCT |
3 trials of 5 standardised firefighting drills in a training structure (carrying a hose up 4 flights, hoisting a hose, discharging a pump can, dragging a dummy, chopping a block of wood). 10 min rest between trials No fluid intake Unknown ambient temperature |
Significant (p < 0.001) change in HCT (pre 43.2 ± 0.75 %, post 47.3 ± 0.75 %), indicating significant dehydration |
57 (Fair) |
| Angerer et al. [9] |
49 firefighter trainees (all male) Wore PPE and SCBA (24 kg) |
Nude BW |
30 min fire operation in a large simulation plant (ascending stairs, dragging hoses, fire suppression, dragging 80 kg dummy up and downstairs, crouched progression) No fluid intake Maximum 200 °C at 1.5 m above ground and 700 °C below the ceiling |
BW significantly (p <0.001) reduced by mean 0.6 ± 0.2 kg |
61 (Good) |
| Raines et al. [12] |
34 firefighters (32 male, 2 female) AD group (n = 17) PR group (n = 17) Wore PPE |
Plasma Osm Urine colour USG |
PR group consumed 600mLwater and 600 mL sport drink per hour of shift One day (9.9 ± 2.2 h/day AD, 10.5 ± 2.2 h/day PR) of wildfire suppression (intense but intermittent work, using chainsaws, applying water, carrying, transit time and briefings) Mild to warm ambient temperature (15.8–26.4 °C) |
PR group significantly higher total water intake (7.1 ± 3.1 L PR, 3.4 ± 1.6 L AD, p < 0.001) Both groups began work dehydrated according to USG (1.019 ± 0.007 AD, 1.016 ± 0.005 PR) PR post shift had significantly (p = 0.001) lower USG (1.004 ± 0.002) than AD (1.016 ± 0.008) Change from dehydrated to euhydrated for PR group only Significant (p < 0.01) change in urine colour for both groups (pre score 2.8 ± 0.4 AD, 2.6 ± 0.5 PR, post score 2.3 ± 0.8 AD, 1.4 ± 0.5 PR), but still dehydrated Plasma Osm no different between groups (p = 0.371), both arrived dehydrated and post shift both significantly reduced (p < 0.0001) to achieve similar euhydration |
57 (Fair) |
| Ruby et al. [15] |
14 wildland firefighters Wore PPE |
Water turnover USG Urine Osm |
5 day period of arduous fire suppression (hiking with load and fire line construction) Ad libitum drinking Unspecified ambient temperature |
Water turnover 6.7 ± 4 L/day No significant change in USG (pre 1.016 ± 0.006, post 1.108 ± 0.006) No significant change in urine Osm (pre 562 ± 175 mOsm/L, post 629 ± 216 mOsm/L) |
50 (Fair) |
| Raines et al. [18] |
12 male wildfire firefighters Wore PPE |
Plasma Osm |
2 days of 12 h live fire prescribed operation (controlled fire application, building containment lines with hoe, chasing spot fires and applying water) Ad libitum drinking Hot ambient temperature (30.9 ± 3.6 °C day 1, 32.8 ± 5.7 °C day 2) |
No significant (p = 0.73) change in plasma osmolality (day 1 292 ± 1 mOsm/L, day 2 289 ± 0.5 mOsm/L), indicating euhydration throughout |
57 (Fair) |
| Eglin et al. [28] |
14 firefighter instructors (all male) Wore PPE and SCBA (20.2 kg) |
USG Nude BW (adjusted) Fluid deficit |
30 hot fire (HF) exercises (33 ± 7.9 min, 74 ± 42 °C) 6 fire behaviour (FB) exercises (26.3 ± 5.5 min, 45 ± 12 °C) and 8 fire attack (FA) exercises (7.3 ± 2.6 min, 139 ± 48 °C) performed on same day with 2 h rest in-between Ad libitum drinking |
Mean BW change 0.96 ± 0.41 kg/h, fluid deficit 0.62 ± 0.61 L HF exercises (0.79 ± 0.80 %/h) Mean BW change 1.59 ± 0.57 kg for FB and FA exercises Mild hypohydration at end of exercises with insufficient fluid intake to counteract body weight loss from sweating No significant (p > 0.05) change in USG (pre 1.019 ± 0.08, post 1.021 ± 0.009) |
50 (Fair) |
Discussion
Conclusion
Abbreviations
PPE
SCBA
USG
- 1. Cuddy JS, Sol JA, Hailes WS, Ruby BC. Work patterns dictate energy demands and thermal strain during wildland firefighting. Wilderness Environ Med 2015;26(2):221–226. 10.1016/j.wem.2014.12.010. 25772825.ArticlePubMed
- 2. Raines J, Snow R, Petersen A, Harvey J, Nichols D, Aisbett B. Pre-shift fluid intake: effect on physiology, work and drinking during emergency wildfire fighting. Appl Ergon 2012;43(3):532–540. 10.1016/j.apergo.2011.08.007. 21906723.ArticlePubMed
- 3. Bos J, Mol E, Visser B, Frings-Dresen MH. The physical demands upon (Dutch) fire-fighters in relation to the maximum acceptable energetic workload. Ergonomics 2004;47(4):446–460. 10.1080/00140130310001643283. 14681000.ArticlePubMed
- 4. Rossi R. Fire fighting and its influence on the body. Ergonomics 2003;46(10):1017–1033. 10.1080/0014013031000121968. 12850937.ArticlePubMed
- 5. Smith DL, Manning T, Petruzzello SJ. Effect of strenuous live-fire drills on cardiovascular and psychological responses of recruit firefighters. Ergonomics 2001;44(3):244–254. 10.1080/00140130121115. 11219758.ArticlePubMed
- 6. Horn GP, DeBlois J, Shalmyeva I, Smith DL. Quantifying dehydration in the fire service using field methods and novel devices. Prehosp Emerg Care 2012;16(3):347–355. 10.3109/10903127.2012.664243. 22443314.ArticlePubMed
- 7. Holsworth RE Jr, Cho YI, Weidman J. Effect of hydration on whole blood viscosity in firefighters. Altern Ther Health Med 2013;19(4):44–49. 23981371.PubMed
- 8. Smith DL, Petruzzello SJ, Chludzinski MA, Reed JJ, Woods JA. Effect of strenuous live-fire fire fighting drills on hematological, blood chemistry and psychological measures. J Thermal Biol 2001;26(4):375–379. 10.1016/S0306-4565(01)00047-X.Article
- 9. Angerer P, Kadlez-Gebhardt S, Delius M, Raluca P, Nowak D. Comparison of cardiocirculatory and thermal strain of male firefighters during fire suppression to exercise stress test and aerobic exercise testing. Am J Cardiol 2008;102(11):1551–1556. 10.1016/j.amjcard.2008.07.052. 19026313.ArticlePubMed
- 10. Barr D, Gregson W, Reilly T. The thermal ergonomics of firefighting reviewed. Appl Ergon 2010;41(1):161–172. 10.1016/j.apergo.2009.07.001. 19664755.ArticlePubMed
- 11. Cuddy JS, Ruby BC. High work output combined with high ambient temperatures caused heat exhaustion in a wildland firefighter despite high fluid intake. Wilderness Environ Med 2011;22(2):122–125. 10.1016/j.wem.2011.01.008. 21664560.ArticlePubMed
- 12. Raines J, Snow R, Petersen A, Harvey J, Nichols D, Aisbett B. The effect of prescribed fluid consumption on physiology and work behavior of wildfire fighters. Appl Ergon 2013;44(3):404–413. 10.1016/j.apergo.2012.10.002. 23149116.ArticlePubMed
- 13. Ftaiti F, Duflot JC, Nicol C, Grelot L. Tympanic temperature and heart rate changes in firefighters during treadmill runs performed with different fireproof jackets. Ergonomics 2001;44(5):502–512. 10.1080/00140130118503. 11345493.ArticlePubMed
- 14. Duncan HW, Gardner GW, James BR. Physiological responses of men working in fire fighting equipment in the heat. Ergonomics 1979;22(5):521–527. 10.1080/00140137908924636. 520284.ArticlePubMed
- 15. Ruby BC, Schoeller DA, Sharkey BJ, Burks C, Tysk S. Water turnover and changes in body composition during arduous wildfire suppression. Med Sci Sports Exerc 2003;35(10):1760–1765. 10.1249/01.MSS.0000089348.39312.4D. 14523317.ArticlePubMed
- 16. Hendrie A, Brotherhood J, Budd G, Jeffery S, Beasley F, Costin B, Zhien W, Baker M, Cheney N, Dawson M. Project Aquarius 8. Sweating, drinking, and dehydration in men suppressing wildland fires. Int J Wildland Fire 1997;7(2):145–158. 10.1071/WF9970145.Article
- 17. Cheuvront SN, Carter R, Montain SJ, Stephenson LA, Sawka MN. Influence of hydration and airflow on thermoregulatory control in the heat. J Thermal Biol 2004;29(7):471–477. 10.1016/j.jtherbio.2004.08.016.Article
- 18. Raines J, Snow R, Nichols D, Aisbett B. Fluid intake, hydration, work physiology of wildfire fighters working in the heat over consecutive days. Ann Occup Hyg 2015;59(5):554–565. 10.1093/annhyg/meu113. 25667157.PubMed
- 19. Mclellan TM, Cheung SS, Latzka WA, Sawka MN, Pandolf KB, Millard CE, Withey WR. Effects of dehydration, hypohydration, and hyperhydration on tolerance during uncompensable heat stress. Can J Appl Physiol 1999;24(4):349–361. 10.1139/h99-027. 10470451.ArticlePubMed
- 20. Hew-Butler T, Rosner MH, Fowkes-Godek S, Dugas JP, Hoffman MD, Lewis DP, Maughan RJ, Miller KC, Montain SJ, Rehrer NJ, et al. Statement of the third international exercise-associated hyponatremia consensus development conference, Carlsbad, California, 2015. Clin J Sport Med 2015;25(4):303–320. 10.1097/JSM.0000000000000221. 26102445.ArticlePubMed
- 21. Beltrami FG, Hew-Butler T, Noakes TD. Drinking policies and exercise-associated hyponatraemia: is anyone still promoting overdrinking? Br J Sports Med 2008;42(10):796–501. 10.1136/bjsm.2008.047944. 18400876.ArticlePubMed
- 22. Carlton A, Orr RM. The effects of fluid loss on physical performance: A critical review. J Sport Health Sci. 2015;4:357–63. 10.1016/j.jshs.2014.09.004.Article
- 23. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6(7):e1000097. 10.1371/journal.pmed.1000097. 19621072.ArticlePubMedPMC
- 24. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52(6):377–384. 10.1136/jech.52.6.377. 9764259.ArticlePubMedPMC
- 25. Deeks JJ, Dinnes J, D’amico R, Sowden A, Sakarovitch C, Song F, Petticrew M, Altman D. Evaluating non-randomised intervention studies. Health Technol Assess 2003;7(27):1–179. 10.3310/hta7270.ArticlePDF
- 26. Theis J, Gerdhem P, Abbott A. Quality of life outcomes in surgically treated adult scoliosis patients: a systematic review. Eur Spine J 2015;24(7):1343–1355. 10.1007/s00586-014-3593-3. 25381158.ArticlePubMedPDF
- 27. Kennelly J. Methodological Approach to Assessing the Evidence. Reducing Racial/Ethnic Disparities in Reproductive and Perinatal Outcomes. 2011, New York: Springer; 7–19.Article
- 28. Eglin CM, Coles S, Tipton MJ. Physiological responses of fire-fighter instructors during training exercises. Ergonomics 2004;47(5):483–494. 10.1080/0014013031000107568. 15204300.ArticlePubMed
- 29. Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med 2005;37(5):360–363. 15883903.PubMed
- 30. Graff L. A handbook of routine urinalysis. 1983, New York: Lippincott Williams & Wilkins.
- 31. Casa DJ, Armstrong LE, Hillman SK, Montain SJ, Reiff RV, Rich BS, Roberts WO, Stone JA. National athletic trainers' association position statement: fluid replacement for athletes. J Athl Train 2000;35(2):212–224. 16558633.PubMedPMC
- 32. Cheuvront SN, Ely BR, Kenefick RW, Sawka MN. Biological variation and diagnostic accuracy of dehydration assessment markers. Am J Clin Nutr 2010;92(3):565–573. 10.3945/ajcn.2010.29490. 20631205.ArticlePubMed
- 33. Maughan RJ, Shirreffs SM. Development of individual hydration strategies for athletes. Int J Sport Nutr Exerc Metab 2008;18(5):457–472. 10.1123/ijsnem.18.5.457. 19033609.ArticlePubMed
- 34. Popowski LA, Oppliger RA, Patrick Lambert G, Johnson RF, Kim Johnson A, Gisolf CV. Blood and urinary measures of hydration status during progressive acute dehydration. Med Sci Sports Exerc 2001;33(5):747–753. 10.1097/00005768-200105000-00011. 11323543.ArticlePubMed
- 35. Cheuvront SN, Sawka MN. SSE# 97: Hydration assessment of athletes. Sports Sci Exch 2005;18(2):1–12.
- 36. Kovacs EM, Senden JM, Brouns F. Urine color, osmolality and specific electrical conductance are not accurate measures of hydration status during postexercise rehydration. J Sports Med Phys Fitness 1999;39(1):47–53. 10230169.PubMed
- 37. Armstrong LE, Maresh CM, Castellani JW, Bergeron MF, Kenefick RW, LaGasse KE, Riebe D. Urinary indices of hydration status. Int J Sport Nutr 1994;4(3):265–279. 10.1123/ijsn.4.3.265. 7987361.ArticlePubMed
- 38. Cheuvront SN, Kenefick RW, Charkoudian N, Sawka MN. Physiologic basis for understanding quantitative dehydration assessment. Am J Clin Nutr 2013;97(3):455–462. 10.3945/ajcn.112.044172. 23343973.ArticlePubMed
- 39. Cheuvront SN, Fraser CG, Kenefick RW, Ely BR, Sawka MN. Reference change values for monitoring dehydration. Clin Chem Lab Med 2011;49(6):1033–1037. 10.1515/CCLM.2011.170. 21428854.ArticlePubMed
- 40. Walsh NP, Laing SJ, Oliver SJ, Montague JC, Walters R, Bilzon JL. Saliva parameters as potential indices of hydration status during acute dehydration. Med Sci Sports Exerc 2004;36(9):1535–1542. 10.1249/01.MSS.0000139797.26760.06. 15354035.ArticlePubMed
- 41. NFPA. National Fire Protection Association, Standard on the Rehabilitation Process for Members During Emergency Operations and Training Exercises. 2008, Quincy: National Fire Protection Association.
- 42.
- 43.
- 44. Langridge P, Taylor N, Bermingham A. Hydration on the fireground: experimental trial and interim report. 2003, Melbourne: Country Fire Authority.
REFERENCES
Figure & Data
REFERENCES
Citations

- Hydration Tracking via Saliva Osmolarity in Recruit Firefighters Throughout a 12-Week Fire School
A. Maleah Holland-Winkler, Andrew R. Moore, Steven L. Parish, Tiffany J. Oberther
Fire.2025; 8(2): 39. CrossRef - Determinants of Health and Performance in Wildland Firefighters: A Narrative Review
Fabio García-Heras, Jorge Gutiérrez-Arroyo, Juan Rodríguez-Medina, Belén Carballo-Leyenda, Pilar Sánchez-Collado, Gerardo Villa-Vicente, Jose A. Rodríguez-Marroyo
Journal of Functional Morphology and Kinesiology.2025; 10(1): 80. CrossRef - EVALUATING KNOWLEDGE ABOUT WILDFIRES AMONG FIREFIGHTERS AND FIRE SCHOOL CADETS: A SURVEY-BASED STUDY
Bartłomiej Płeska, Marcin Popielarski
Zeszyty Naukowe SGSP.2025; 2(93): 81. CrossRef - Work Exposome and Related Disorders of Firefighters: An Overview of Systematized Reviews
Alexis Descatha, Hugues Dousseau, Sabrina Pitet, Francis Magnolini, Neil McMillan, Neil Mangelsdorf, Rick Swan, Jean-Marie Steve, Didier Pourret, Marc Fadel
Safety and Health at Work.2025; 16(2): 145. CrossRef - Hydration Strategies in Older Adults
Jacquelyn Pence, Allyson Davis, Ebonie Allen-Gregory, Richard J. Bloomer
Nutrients.2025; 17(14): 2256. CrossRef - The impact of age on firefighters' specific motor abilities
Radivoje Janković, Svetozar Stajkovac, Dragan Mlađan, Nenad Koropanovski
Bezbednost, Beograd.2025; 67(2): 27. CrossRef - Non-malignant kidney diseases in Danish firefighters
Julie Elbaek Pedersen, Kajsa Kirstine Ugelvig Petersen, Maria Helena Guerra Andersen, Anne Thoustrup Saber, Ulla Vogel, Niels Ebbehøj, Jens Peter Bonde, Tina Kold Jensen, Regitze Sølling Wils, Johnni Hansen
Occupational and Environmental Medicine.2025; 82(9): 423. CrossRef - Relationships between job stress, post-traumatic stress and musculoskeletal symptoms in firefighters and the role of job burnout and depression mediators: a bayesian network model
Amir Hossein Khoshakhlagh, Saleh Al Sulaie, Saeid Yazdanirad, Robin Marc Orr, Fereydoon Laal
BMC Public Health.2024;[Epub] CrossRef - Nourishing Physical Productivity and Performance On a Warming Planet - Challenges and Nutritional Strategies to Mitigate Exertional Heat Stress
Alan J. McCubbin, Christopher G. Irwin, Ricardo J. S. Costa
Current Nutrition Reports.2024; 13(3): 399. CrossRef - Wilderness First Responder Medical Clearance – A Scoping Review with Recommendations
Gregory D. King, Erik Pan, Michael G. Millin
Prehospital Emergency Care.2024; 28(1): 50. CrossRef - Health burden of sugarcane burning on agricultural workers and nearby communities
Arthur D. Stem, Matthew Gibb, Carlos A. Roncal-Jimenez, Richard J. Johnson, Jared M. Brown
Inhalation Toxicology.2024; 36(5): 327. CrossRef - Hydration Considerations to Improve the Physical Performance and Health of Firefighters
Angelia M. Holland-Winkler, Blake K. Hamil
Journal of Functional Morphology and Kinesiology.2024; 9(4): 182. CrossRef - RETRACTED: Scottish Firefighters Occupational Cancer and Disease Mortality Rates: 2000-2020
A A Stec, A Robinson, T A M Wolffe, E Bagkeris
Occupational Medicine.2023; 73(1): 42. CrossRef - Biomonitoring of firefighting forces: a review on biomarkers of exposure to health-relevant pollutants released from fires
Bela Barros, Marta Oliveira, Simone Morais
Journal of Toxicology and Environmental Health, Part B.2023; 26(3): 127. CrossRef - Differences in Fitness between Firefighter Trainee Academy Classes and Normative Percentile Rankings
Robert George Lockie, Robin M. Orr, Fernando Montes, Tomas Jason Ruvalcaba, J. Jay Dawes
Sustainability.2022; 14(11): 6548. CrossRef - End‐stage renal disease incidence in a cohort of US firefighters from San Francisco, Chicago, and Philadelphia
Lynne E. Pinkerton, Stephen Bertke, Matthew M. Dahm, Travis L. Kubale, Miriam R. Siegel, Thomas R. Hales, James H. Yiin, Mark P. Purdue, James J. Beaumont, Robert D. Daniels
American Journal of Industrial Medicine.2022; 65(12): 975. CrossRef - Sweat monitoring beneath garments using passive, wireless resonant sensors interfaced with laser-ablated microfluidics
Adam R. Carr, Yash H. Patel, Charles R. Neff, Sadaf Charkhabi, Nathaniel E. Kallmyer, Hector F. Angus, Nigel F. Reuel
npj Digital Medicine.2020;[Epub] CrossRef - Sustainable solutions to mitigate occupational heat strain – an umbrella review of physiological effects and global health perspectives
Nathan B. Morris, Ollie Jay, Andreas D. Flouris, Ana Casanueva, Chuansi Gao, Josh Foster, George Havenith, Lars Nybo
Environmental Health.2020;[Epub] CrossRef - A Profile of Injuries Sustained by Firefighters: A Critical Review
Robin Orr, Vinicius Simas, Elisa Canetti, Ben Schram
International Journal of Environmental Research and Public Health.2019; 16(20): 3931. CrossRef - Effects of Wrist Cooling on Recovery From Exercise-Induced Heat Stress With Firefighting Personal Protective Equipment
Emily Schlicht, Ronald Caruso, Kelsey Denby, Alexs Matias, Monique Dudar, Stephen J. Ives
Journal of Occupational & Environmental Medicine.2018; 60(11): 1049. CrossRef - A Profile of Injuries Sustained by Law Enforcement Officers: A Critical Review
Kate Lyons, Cameron Radburn, Robin Orr, Rodney Pope
International Journal of Environmental Research and Public Health.2017; 14(2): 142. CrossRef
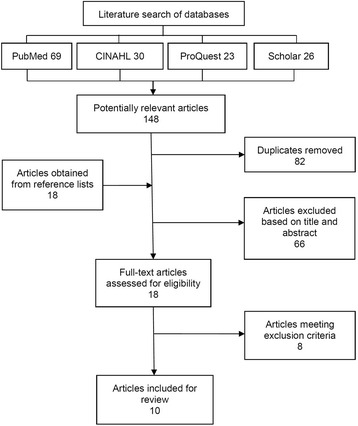
Fig. 1
| Database | Search terms | Filters |
|---|---|---|
| PubMed | (firefighter [Mesh] OR firefighter* OR “fire service” OR “fire fighter*” OR “fire and rescue personnel”) AND (hydration OR dehydration OR rehydration OR physiological* OR thermoregulation OR “thermal strain” OR temperature OR “water turnover” OR “fluid intake” OR drinking OR “fluid consumption”) | 2000–2015 |
| CINAHL | (firefighter [Mesh] OR firefighter* OR “fire service” OR “fire fighter*” OR “fire and rescue personnel”) AND (hydration OR dehydration OR rehydration OR physiological* OR thermoregulation OR “thermal strain” OR temperature OR “water turnover” OR “fluid intake” OR drinking OR “fluid consumption”) | 2000–2015 |
| ProQuest | (firefighter* OR “fire service” OR “fire fighter*” OR “fire and rescue personnel”) AND (hydration OR dehydration OR rehydration OR physiological* OR thermoregulation OR “thermal strain” OR temperature OR “water turnover” OR “fluid intake” OR drinking OR “fluid consumption”) | 2000–2015 |
| Peer reviewed | ||
| Terms in abstract | ||
| Google Scholar | (firefighter* OR fire service OR fire fighter* OR fire and rescue personnel) AND (hydration OR dehydration OR rehydration OR physiological response OR thermoregulation OR body temperature OR water turnover OR fluid intake OR drinking OR fluid consumption) | 2000–2015 |
| Study | Participants | Outcome measure(s) | Intervention(s) | Major Findings | CAS (%) |
|---|---|---|---|---|---|
| Cuddy et al. [1] | 15 Hot Spot firefighters (12 male, 3 female) Wore PPE | Water turnover Nude BW | Live wildland fire suppression over 3 days of work shifts (11.4 ± 0.7 h/day) (hiking, line dragging, laying hose, chain sawing, clearing brush, lookout, and scouting) Ad libitum drinking 27.5 ± 3.2 °C mean ambient temperature | No significant change (p = 0.12) in morning BW across 3 days (pre 77.3 ± 8.3 kg, post 77.0 ± 8.9 kg) Mean water turnover 9.5 ± 1.7 L/d | 54 (Fair) |
| Raines et al. [2] | 32 firefighters (31 male,1 female) Ad libitum(AD) group (n = 17), pre-shift (PR) group (n = 15) PPE | Plasma Osm Urine colour USG | PR group consumed 500 mL fluid bolus pre shift and ad libitum remainder of shift 7 days (9.9 ± 2.2 h/day AD, 9.7 ± 2.3 h/day PR) of wildfire suppression (intense but intermittent work, using chainsaws, applying water, carrying, transit time and briefings) Mild to warm ambient temperatures (15.8–26.4 °C) | No difference between groups in total fluid intake (3.4 ± 1.6 L AD, 3.7 ± 2.9 L PR, p = 0.730) No significant differences between groups for any hydration marker (urine colour, p = 0.44; USG, p = 0.92; plasma Osm, p = 0.41) Significant decrease in both urine colour (p = 0.001) and USG (p = 0.01) across the shift, but still dehydrated by end, though less than at start Plasma Osm indicates firefighters arrived on shift dehydrated and finish dehydrated (p < 0.0001) | 57 (Fair) |
| Horn et al. [6] | 35 career, volunteer and industrial firefighters (31 male, 4 female) Wore PPE and SCBA | Nude BW Urine colour USG Urine Osm Salivary Osm | 3 h live fire training exercise in specialised training building. 3–4 evolutions lasting 15–25 min, separated by 10–15 min (obtain water, advance hoses, extinguish fires, forcible entries, search and rescue and ventilation tasks) Encouraged ad libitum drinking (water and sport drink) Cool autumn day | Significant BW loss of 1.1 ± 0.8 kg (p < 0.001) and 1.9 ± 0.9 kg (2.2 % BW loss) adjusted for fluid intake and voiding Significant (p < 0.001) increase in salivary Osm (pre 78.0 ± 21.5 mOsm/kg, post 49.0 ± 15 mOsm/kg), reflective of dehydration No significant (p > 0.05) changes in Urine Osm (pre 768 ± 260 mOsm/kg, post 712 ± 251 mOsm/kg), urine colour (pre score 5.8 ± 1.5, post score 5.3 ± 1.5), or USG (pre 1.025 ± 0.009, post 1.024 ± 0.009) | 61 (Good) |
| Holsworth et al. [7] | 9 volunteer firefighters (8 males, 1 female) WorePPE and SCBA | HCT | 2 × 30 min strenuous live structural fires No fluid intake | Significant (p = 0.0014) change in HCT (pre 43.7 ± 3.1 %, post 46.1 ± 2.3 %), indicating significant dehydration | 61 (Good) |
| Smith et al. [8] | 11 male professional firefighters WorePPE and SCBA (20.4 kg) | HCT | 3 trials of 5 standardised firefighting drills in a training structure (carrying a hose up 4 flights, hoisting a hose, discharging a pump can, dragging a dummy, chopping a block of wood). 10 min rest between trials No fluid intake Unknown ambient temperature | Significant (p < 0.001) change in HCT (pre 43.2 ± 0.75 %, post 47.3 ± 0.75 %), indicating significant dehydration | 57 (Fair) |
| Angerer et al. [9] | 49 firefighter trainees (all male) Wore PPE and SCBA (24 kg) | Nude BW | 30 min fire operation in a large simulation plant (ascending stairs, dragging hoses, fire suppression, dragging 80 kg dummy up and downstairs, crouched progression) No fluid intake Maximum 200 °C at 1.5 m above ground and 700 °C below the ceiling | BW significantly (p <0.001) reduced by mean 0.6 ± 0.2 kg | 61 (Good) |
| Raines et al. [12] | 34 firefighters (32 male, 2 female) AD group (n = 17) PR group (n = 17) Wore PPE | Plasma Osm Urine colour USG | PR group consumed 600mLwater and 600 mL sport drink per hour of shift One day (9.9 ± 2.2 h/day AD, 10.5 ± 2.2 h/day PR) of wildfire suppression (intense but intermittent work, using chainsaws, applying water, carrying, transit time and briefings) Mild to warm ambient temperature (15.8–26.4 °C) | PR group significantly higher total water intake (7.1 ± 3.1 L PR, 3.4 ± 1.6 L AD, p < 0.001) Both groups began work dehydrated according to USG (1.019 ± 0.007 AD, 1.016 ± 0.005 PR) PR post shift had significantly (p = 0.001) lower USG (1.004 ± 0.002) than AD (1.016 ± 0.008) Change from dehydrated to euhydrated for PR group only Significant (p < 0.01) change in urine colour for both groups (pre score 2.8 ± 0.4 AD, 2.6 ± 0.5 PR, post score 2.3 ± 0.8 AD, 1.4 ± 0.5 PR), but still dehydrated Plasma Osm no different between groups (p = 0.371), both arrived dehydrated and post shift both significantly reduced (p < 0.0001) to achieve similar euhydration | 57 (Fair) |
| Ruby et al. [15] | 14 wildland firefighters Wore PPE | Water turnover USG Urine Osm | 5 day period of arduous fire suppression (hiking with load and fire line construction) Ad libitum drinking Unspecified ambient temperature | Water turnover 6.7 ± 4 L/day No significant change in USG (pre 1.016 ± 0.006, post 1.108 ± 0.006) No significant change in urine Osm (pre 562 ± 175 mOsm/L, post 629 ± 216 mOsm/L) | 50 (Fair) |
| Raines et al. [18] | 12 male wildfire firefighters Wore PPE | Plasma Osm | 2 days of 12 h live fire prescribed operation (controlled fire application, building containment lines with hoe, chasing spot fires and applying water) Ad libitum drinking Hot ambient temperature (30.9 ± 3.6 °C day 1, 32.8 ± 5.7 °C day 2) | No significant (p = 0.73) change in plasma osmolality (day 1 292 ± 1 mOsm/L, day 2 289 ± 0.5 mOsm/L), indicating euhydration throughout | 57 (Fair) |
| Eglin et al. [28] | 14 firefighter instructors (all male) Wore PPE and SCBA (20.2 kg) | USG Nude BW (adjusted) Fluid deficit | 30 hot fire (HF) exercises (33 ± 7.9 min, 74 ± 42 °C) 6 fire behaviour (FB) exercises (26.3 ± 5.5 min, 45 ± 12 °C) and 8 fire attack (FA) exercises (7.3 ± 2.6 min, 139 ± 48 °C) performed on same day with 2 h rest in-between Ad libitum drinking | Mean BW change 0.96 ± 0.41 kg/h, fluid deficit 0.62 ± 0.61 L HF exercises (0.79 ± 0.80 %/h) Mean BW change 1.59 ± 0.57 kg for FB and FA exercises Mild hypohydration at end of exercises with insufficient fluid intake to counteract body weight loss from sweating No significant (p > 0.05) change in USG (pre 1.019 ± 0.08, post 1.021 ± 0.009) | 50 (Fair) |
 KSOEM
KSOEM

 Cite
Cite

