Abstract
-
Background
The coronavirus disease 2019 (COVID-19) pandemic drastically modified the occupational system wherein telecommuting has risen as the major form of work. Few studies have incorporated Karasek’s job demand-control (JDC) model into explaining the health effects of telecommuting. This study aimed to investigate the health risk in South Korean telecommuters during the pandemic, and its distribution according to the job stress-related factors.
-
Methods
A nationwide population-based cross-sectional study of South Korean laborers was conducted, utilizing the 6th Korean Working Conditions Survey (2020–2021). Following the previously described concept of telecommuting, 14,478 white-collar employees were eligible study participants. Telecommuting, job demand, job control, and various health indicators were measured by the responses to the survey. Participants were stratified into 4 job profiles classified by the JDC model. We conducted multiple logistic regression analyses between telecommuting and health-related outcomes to estimate the odds ratio (OR) with a 95% confidence interval (CI).
-
Results
One hundred forty-six low-strain, 223 active, 69 passive, and 148 high-strain workers were screened as telecommuters. Compared to office workers, telecommuters had a higher proportion in high job control groups. Subgroup analysis demonstrated different relationships between telecommuting and health, where only active telecommuters showed a higher prevalence of depression (OR: 1.980, 95% CI: 1.126–3.481), and high-strain telecommuters were affected in most outcomes including insomnia (OR: 2.555, 95% CI: 1.473–4.433), musculoskeletal pain (OR: 2.786, 95% CI: 1.719–4.517), headache/eye strain (OR: 3.074, 95% CI: 1.992–4.745) and presenteeism (OR: 1.932, 95% CI: 1.193–3.131).
-
Conclusions
This study revealed significantly increased odds of multiple health outcomes among South Korean telecommuters during the COVID-19 pandemic era. High-strain job holders were prominently susceptible to the negative health impacts of telecommuting. Occupational health management towards telecommuters should approach mitigating high job demand and low job control.
-
Keywords: Telecommuting; COVID-19; Occupational health; Job demand and control; National population survey
BACKGROUND
Telecommuting or teleworking is a work form where an employed member of an institution interacts remotely with coworkers using information and communication technologies (ICTs), and performs a portion of work hours outside the main workstation.
1,2 Advanced satellite networks and the unprecedented coronavirus disease 2019 (COVID-19) pandemic led to an abrupt transition to working from home.
3 Despite labor market rigidity related to workspaces and work schedules in South Korea, the proportion of telecommuters increased tenfold, from 0.5% in 2019 to 5.4% in 2021.
4
Studies have highlighted the positive aspects of telecommuting, including better work-life balance, lower risk of various unhealthy lifestyles (i.e., alcohol abuse and smoking), and lower work role stress.
5,6,7 However, the World Health Organization (WHO) and International Labour Organization (ILO) Joint Estimates have asserted possible health risks to teleworkers and provided guidelines to protect and promote their physical and mental health and social well-being.
8 Researchers have identified negative aspects of teleworking, such as increased sickness presenteeism (working despite being sick),
9 musculoskeletal pain due to poor ergonomic design and physical inactivity,
10 and depression and sleep disturbances due to overtime work.
11,12,13 Teleworkers are more likely to suffer from various health problems, such as anxiety, insomnia, and fatigue than daily commuters.
14
Inconsistent findings regarding the positive or negative effects of teleworking on health may be due to multidimensional factors, including work-related or familial characteristics. Occupational stress is one of the most critical risk factors for work-related diseases and well-being.
15 Previous studies have revealed the modulating effect of job stress on the relationship between telecommuting and work-related outcomes.
7,16 However, research examining the role of individual job stress factors on telecommuters’ health is limited. The job demand-control (JDC) model is highly influential in research on occupational stress and has provided the theoretical foundation for more empirical studies than any other models.
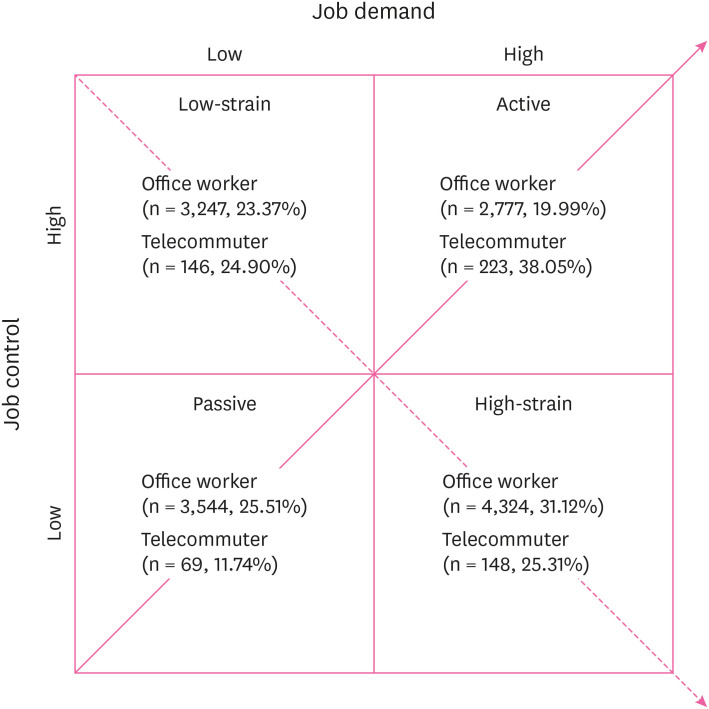
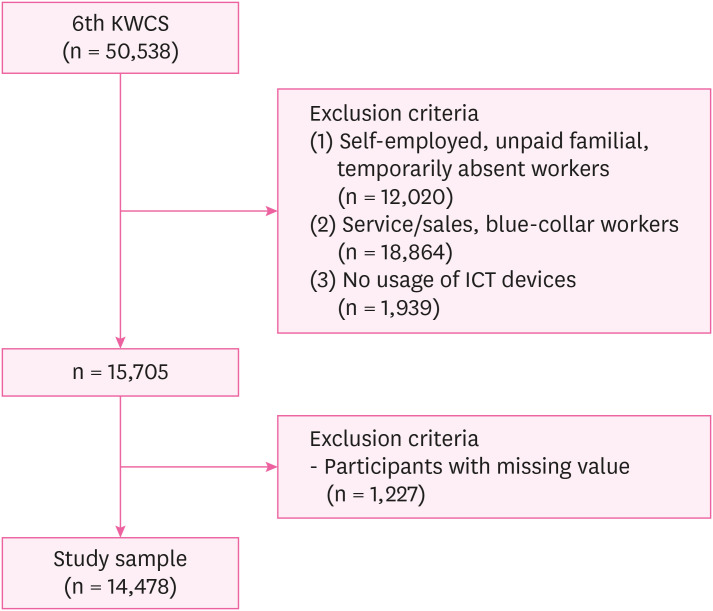
17 Job demands originate from the physical or psychological workload, such as fast pace and conflicting tasks placed on workers, while job control refers to decision authority and skill discretion. Based on these 2 dimensions, occupations can be categorized into 4 groups: (1) low-strain, (2) active, (3) passive, and (4) high-strain (
Fig. 1). The most severe occupational stress and consequent health deterioration are likely to occur among workers with high-strain workers and low flexibility in managing intense job demands.
18,19 Meanwhile, active workers can prevent burnout caused by high job demands by utilizing appropriate resources and coping strategies.
20
Fig. 1 Distribution of study participants stratified by job demand-control model.
Therefore, this study investigated whether occupational stress moderates the effect of teleworking on workers’ health outcomes. We hypothesized that occupational stress, particularly high job demands and low control, combined with hazardous working conditions in telecommuting, exacerbates the health risks of telecommuters. Using nationally representative data from South Korean workers, this study investigated the role of job demands and control in the association between telecommuting and health outcomes.
METHODS
Data source and study population
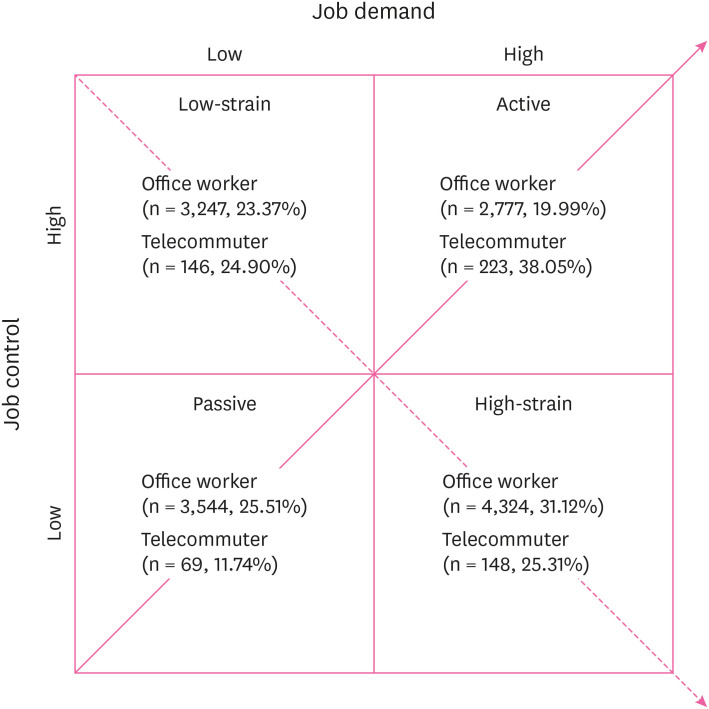
We conducted a population-based cross-sectional study using data from the 6th Korean Working Conditions Survey (KWCS). The KWCS is conducted by the Korea Occupational Safety and Health Research Institute, to explore the multifaceted working conditions and health statuses of South Korean laborers. The questionnaire composition and survey process were derived from the current European Working Conditions Survey.
21 The 6th KWCS was conducted during the COVID-19 pandemic (October 5th, 2020–April 11th, 2021) and included 50,538 workers aged over 15 years.
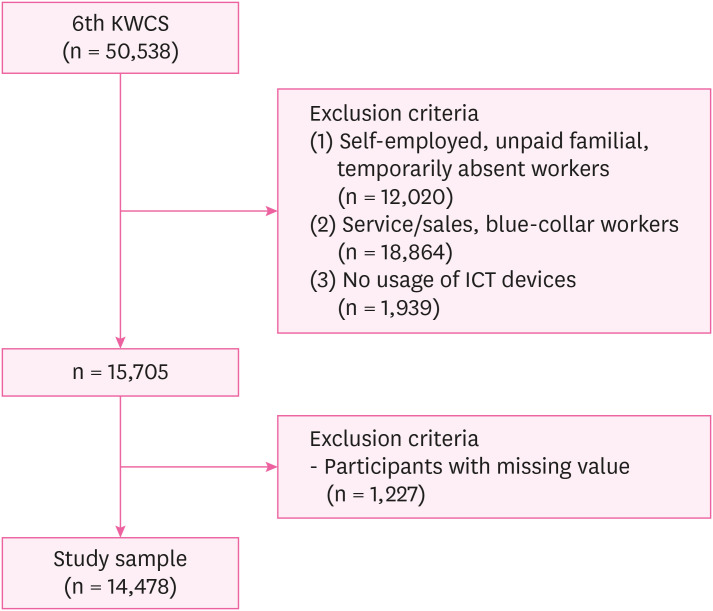
Our study utilized the definition of telecommuting or teleworking described by previous literature, to select an eligible study population.
1,2 Allen et al.
1 stated telecommuting involves members of an organization and ILO specified teleworkers as employees who work for renumeration and are not economically independent workers. Therefore, (1) self-employed, unpaid familial, and temporarily absent workers (n = 12,020) were excluded. Among the 3 types of ‘home workers’ defined by the ILO’s Home Work Convention (No. 177) and Recommendation (No. 184), ILO clarified telework being distinct from industrial home work (goods production undertaken by homeworkers either as part of, or replacing, factory production), and home-based digital platform work (service-sector tasks performed by “crowdworkers” according to the specifications of the employer or intermediary). Thus, (2) blue-collar or service/sales workers (n = 18,864) were excluded. Allen et al.
1 and ILO asserted telecommuters or teleworkers should use ICTs to conduct their tasks and communicate with others remotely. Hence, (3) workers who did not use ICT devices during their tasks (n = 1,939) were excluded. After excluding respondents with missing values (n = 1,227), the final sample included 14,478 participants (
Fig. 2).
Fig. 2
Flow chart of selecting eligible population.
KWCS: Korean Working Conditions Survey; ICT: information and communication technology.
Telecommuting status
The participants’ telecommuting status was investigated by the following question and its subdomains, “During the last 12 months, how often have you worked in any of the following locations: D) Your own home?”. Participants’ answers were rated on a 5-point Likert scale (1 = always; 5 = never). Since telecommuters partly substitute their work hours to work away from a central workplace, participants who answered “occasionally” or more were classified as ‘telecommuters.’
1
Job demands were measured using the following 4 items regarding quantitative workload: “Do you have enough time to get the job done?”, “Does your job involve working at very high speed?”, “Does your job involve working to tight deadlines?” and “How often do you have to interrupt a task you are doing in order to take on an unforeseen task?” The questions were rated on 5-point, 7-point, 7-point, and 4-point Likert scales, respectively. Higher scores indicated higher intensity. The participants with total scores below the median (5) were classified as having low job demands.
22 Cronbach’s alpha of questionnaires was found 0.610.
Job control was measured using a combination of the following 3 items regarding autonomy in decision-making or work schedule: “Are you able to apply your own ideas in your work?”, “Can you influence decisions that are important for your work?” and “Can you take a break when you wish?” Responses were rated on a 5-point Likert scale (0 = never; 4 = always).
23 The participants with total scores that did not exceed the median (7) were coded as having low job control. Cronbach’s alpha of questionnaires was found 0.695.
We measured 6 health-related indicators as outcome variables. The WHO-5 Well-Being Index, which is a validated survey to test depression risk, was used.
24 Responses were rated on a 6-point Likert scale (0 = never; 5 = always). The summed total was multiplied by 4, and scores below 50 were considered to indicate depression. The 3-item Minimal Insomnia Symptom Scale was used to identify participants with sleep disorders. Responses were rated on a 5-point Likert scale (0 = daily; 4 = never). A total score above 6 was considered to indicate insomnia.
25 Participants who reported having experienced pain in the lower back, upper limbs (shoulder, neck, arm, elbow, wrist, hand, etc.), or lower limbs (hip, leg, knee, foot, etc.) in the past 12 months were coded as having musculoskeletal pain. Participants who reported having experienced headaches or eye strain in the past 12 months were coded as having headaches or eye strain. Participants who were absent from work due to illnesses for one or more days were coded as exhibiting absenteeism. Participants who reported having worked while sick in the past 12 months were coded as exhibiting presenteeism.
In addition, we measured the following sociodemographic and occupational factors as variables of interest: sex, age (15–29, 30–39, 40–49, 50–59, or ≥ 60 years), education (below college, college, or graduate school), monthly income (< 200, 200–299, 300–399, or ≥ 400/10,000 Korean Won = 8–10 US dollar), and family composition (single, children aged < 15 years, or others). The ‘Others’ category in family composition indicated married couples, having 15 years of age or older, extended families, or other family members. Weekly working hours (≤ 40, 41–52, or > 52), shiftwork, and occupation type (manager/professional or clerk) were included as occupational factors. As managers were not included in subgroups in our sample, occupation type was coded into 2 categories.
Statistical analysis
Descriptive analysis was performed to determine the distribution of the participants’ sociodemographic and occupational characteristics. Chi-squared test was applied to identify the difference in the prevalence of variables. We conducted multiple logistic regression analyses to estimate the adjusted odds ratios (ORs) with a 95% confidence interval (CI) and to verify the association between telecommuting and health-related outcomes. Three models were used: Model 1: unadjusted ORs; (2) Model 2: adjusted for sociodemographic characteristics; and (3) Model 3: adjusted for all confounding variables. Subgroups were divided into 4 using the JDC model, and a stratified logistic regression analysis was performed. To calculate unbiased estimators for the parameters, all analyses were conducted using the survey weight value assigned to each participant in the 6th KWCS. SAS 9.4 software (SAS Institute, Cary, NC, USA) was used, and statistical significance was set at a p-value value of 0.05.
Sensitivity analysis
Sensitivity analyses with adjustment for additional confounders were conducted to verify the robustness of the primary findings. Visual display terminal (VDT) use (< 75%, 75%–99%, 100% of the work hours), physical activity (low, moderate, high), and employment status (regular, precarious) were considered as other potential confounders. Detailed information on the questionnaire items used to define the variables is introduced in the
Supplementary Data 1. The classification of the employment status was derived from the previous study.
26 We examined whether the estimates altered after further adjustment for each confounder upon Model 3. Finally, 3 additional models (Models 4–6) were constructed to repeat the multiple logistic regression and stratification analysis.
Institutional Review Board (IRB) of Seoul National University Hospital determined to exempt the review of this study and approved the waiver of written informed consent due to the secondary use of anonymous information (IRB No. E-2208-111-1351).
RESULTS
The Sociodemographic and occupational characteristics of the study population are summarized in
Table 1. According to our study criteria, 586 workers (4.05%) were defined as telecommuters. Telecommuters were more likely to be highly educated, non-shift workers, and engaged in managerial/professional careers than office workers. In addition, telecommuters showed a higher proportion in the highest and the lowest income brackets. There were significant differences in the distribution of all variables among the 4 occupational groups based on the JDC profiles. Workers with high job control (low-strain, active) were more likely to be male, over middle-aged (age ≥ 40), highly educated, earning high income, supporting young children, and having managerial/professional jobs compared to low job control groups (passive, high-strain). The weekly working hours of high job demand groups (active, high-strain) were greater than those of their low job demand counterparts (passive, low-strain). Among the 4 subgroups, workers with high-strain had the highest proportion in conducting shiftwork.
Table 1 Sociodemographic and occupational characteristics of the participants according to work arrangement and job demand-control model
|
Characteristics |
Work arrangement |
Job demand-control classification |
|
Telecommuter |
Office worker |
p-value |
Low-strain |
Active |
Passive |
High-strain |
p-value |
|
Total (n = 14,478) |
586 |
13,892 |
|
3,393 |
3,000 |
3,613 |
4,472 |
|
|
Sex |
|
|
0.529 |
|
|
|
|
< 0.001 |
|
Male |
305 (52.03) |
7,520 (54.13) |
2,160 (63.67) |
1,853 (61.76) |
1,652 (45.72) |
2,160 (48.30) |
|
Female |
281 (47.97) |
6,372 (45.87) |
1,233 (36.33) |
1,147 (38.24) |
1,961 (54.28) |
2,312 (51.70) |
|
Age (year) |
|
|
0.368 |
|
|
|
|
< 0.001 |
|
15–29 |
74 (12.69) |
2,437 (17.54) |
451 (13.30) |
368 (12.28) |
668 (18.50) |
1,023 (22.88) |
|
30–39 |
194 (33.06) |
4,403 (31.70) |
960 (28.30) |
973 (32.42) |
1,206 (33.39) |
1,458 (32.60) |
|
40–49 |
192 (32.69) |
4,173 (30.04) |
1,088 (32.07) |
980 (32.67) |
1,064 (29.44) |
1,233 (27.57) |
|
50–59 |
103 (17.65) |
2,431 (17.50) |
734 (21.63) |
580 (19.33) |
558 (15.44) |
662 (14.81) |
|
≥ 60 |
23 (3.91) |
448 (3.22) |
160 (4.70) |
99 (3.29) |
117 (3.23) |
96 (2.15) |
|
Education |
|
|
< 0.001 |
|
|
|
|
< 0.001 |
|
Graduate school |
111 (18.91) |
992 (7.14) |
411 (12.11) |
306 (10.21) |
140 (3.87) |
246 (5.49) |
|
College |
430 (73.33) |
11,514 (82.88) |
2,684 (79.11) |
2,451 (81.69) |
3,054 (84.54) |
3,754 (83.95) |
|
Below high school |
45 (7.77) |
1,386 (9.98) |
298 (8.78) |
243 (8.10) |
419 (11.59) |
472 (10.56) |
|
Income (10,000 KRW/month) |
|
|
0.011 |
|
|
|
|
< 0.001 |
|
< 200 |
85 (14.47) |
1,605 (11.55) |
309 (9.09) |
221 (7.36) |
518 (14.34) |
643 (14.37) |
|
200–299 |
160 (27.35) |
4,663 (33.57) |
936 (27.60) |
762 (25.39) |
1,385 (38.33) |
1,740 (38.92) |
|
300–399 |
129 (21.93) |
3,689 (26.55) |
829 (24.44) |
857 (28.57) |
955 (26.44) |
1,176 (26.29) |
|
≥ 400 |
212 (36.25) |
3,935 (28.32) |
1,319 (38.88) |
1,160 (38.68) |
755 (20.88) |
913 (20.43) |
|
Family member |
|
|
0.252 |
|
|
|
|
< 0.001 |
|
Single |
47 (8.06) |
992 (7.14) |
231 (6.80) |
204 (6.79) |
265 (7.33) |
340 (7.59) |
|
Offspring age < 15 years |
261 (44.49) |
5,609 (40.38) |
1,445 (42.59) |
1,357 (45.22) |
1,421 (39.32) |
1,647 (36.84) |
|
Others |
278 (47.45) |
7,291 (52.48) |
1,717 (50.61) |
1,439 (47.98) |
1,927 (53.35) |
2,485 (55.57) |
|
Working hour (/week) |
|
|
0.689 |
|
|
|
|
< 0.001 |
|
≤ 40 |
476 (81.31) |
10,980 (79.04) |
2,858 (84.23) |
2,350 (78.31) |
2,918 (80.76) |
3,332 (74.50) |
|
41–52 |
97 (16.48) |
2,576 (18.54) |
475 (14.00) |
571 (19.04) |
607 (16.79) |
1,020 (22.80) |
|
> 52 |
13 (2.21) |
336 (2.42) |
60 (1.77) |
79 (2.65) |
89 (2.45) |
120 (2.70) |
|
Shiftwork |
|
|
0.009 |
|
|
|
|
< 0.001 |
|
No |
580 (99.00) |
13,315 (95.85) |
3,295 (97.12) |
2,905 (96.84) |
3,490 (96.59) |
4,205 (94.03) |
|
Yes |
6 (1.00) |
577 (4.15) |
98 (2.88) |
95 (3.16) |
123 (3.41) |
267 (5.97) |
|
Occupation type |
|
|
< 0.001 |
|
|
|
|
< 0.001 |
|
Manager/Professional |
389 (66.32) |
6,941 (49.96) |
1,922 (56.65) |
1,666 (55.54) |
1,611 (44.59) |
2,130 (47.64) |
|
Clerk |
197 (33.68) |
6,951 (50.04) |
1,471 (43.35) |
1,334 (44.46) |
2,002 (55.41) |
2,342 (52.36) |
Table 2 shows the job demands and control levels of telecommuters and office workers. Telecommuters had significantly higher job demand and control than office workers. Concordantly, telecommuters were more often involved in active jobs (high demand, high control) and least often involved in passive jobs (low demand, low control;
Fig. 1).
Table 2 Job demand-control status of the participants according to telecommuting status
|
Job stressors |
Work arrangement |
p-value |
|
Telecommuter (n = 586) |
Office worker (n = 13,892) |
|
Job demand |
|
|
< 0.001 |
|
Low |
215 (36.64) |
6,791 (48.88) |
|
High |
371 (63.36) |
7,101 (51.12) |
|
Job control |
|
|
< 0.001 |
|
Low |
217 (37.05) |
7,868 (56.64) |
|
High |
369 (62.95) |
6,024 (43.36) |
|
JDC classification |
|
|
< 0.001 |
|
Low-strain |
146 (24.90) |
3,247 (23.37) |
|
Active |
223 (38.05) |
2,777 (19.99) |
|
Passive |
69 (11.74) |
3,544 (25.51) |
|
High-strain |
148 (25.31) |
4,324 (31.12) |
The ORs and 95% CI based on the regression analyses of the total population are shown in
Table 3. After adjusting for all confounders, telecommuters had significantly increased odds of illness including insomnia (OR: 1.560, 95% CI: 1.021–2.383), musculoskeletal pain (OR: 1.645, 95% CI: 1.222–2.217), and headaches/eye strain (OR: 1.779, 95% CI: 1.346–2.352) compared with office workers. On the other hand, the OR for depression was not statistically significant in either the unadjusted model (OR: 1.307, 95% CI: 0.956–1.787) or the Model 3 (OR: 1.378, 95% CI: 0.992–1.914). The association between telecommuting and presenteeism was significant after adjusting for all covariates (OR: 1.532, 95% CI: 1.104–2.127); however, the association with absenteeism was not statistically significant (OR: 1.206, 95% CI: 0.723–2.010). The results of the sensitivity analysis after further adjustment are displayed in
Supplementary Table 1. The association between telecommuting and insomnia was attenuated when VDT use (OR: 1.462, 95% CI: 0.957–2.232) and employment status (OR: 1.524, 95% CI: 0.992–2.340) were added as confounders respectively. Unlike the primary finding, telecommuting was significantly associated with depression (OR: 1.454, 95% CI: 1.040–2.033) in the model adjusted for physical activity. Musculoskeletal pain, headache/eye strain, and presenteeism consistently showed significant ORs in the sensitivity analysis.
Table 3 Odds ratios with 95% confidence intervals for health-related outcomes according to telecommuting status
|
Characteristics |
Number (%)a
|
Model 1 |
Model 2b
|
Model 3c
|
|
Depression |
181 (31.26) |
1.307 (0.956–1.787) |
1.331 (0.967–1.832) |
1.378 (0.992–1.914) |
|
Insomnia |
77 (13.20) |
1.881 (1.262–2.802)**
|
1.719 (1.129–2.615)*
|
1.560 (1.021–2.383)*
|
|
Musculoskeletal pain |
261 (44.46) |
1.950 (1.501–2.533)**
|
1.826 (1.383–2.412)**
|
1.645 (1.222–2.217)**
|
|
Headache, eye strain |
252 (43.07) |
2.111 (1.626–2.740)**
|
1.964 (1.498–2.574)**
|
1.779 (1.346–2.352)**
|
|
Absenteeism |
35 (6.01) |
1.519 (0.949–2.430) |
1.418 (0.870–2.311) |
1.206 (0.723–2.010) |
|
Presenteeism |
109 (18.64) |
1.746 (1.274–2.392)**
|
1.655 (1.202–2.278)**
|
1.532 (1.104–2.127)*
|
Table 4 shows the results of the stratification analyses by the JDC classification. Among workers with low-strain and passive occupations, telecommuters had significantly higher odds of musculoskeletal pain than officer workers adjusting for covariates (OR: 1.830, 95% CI: 1.089–3.075; OR: 3.079, 95% CI: 1.446–6.559). The OR for headaches/eye strain among telecommuters with low-strain was significant in the unadjusted model (OR: 1.813, 95% CI: 1.092–3.010) but yet in the adjusted models. The OR for depression in the total sample was not statistically significant; however, active telecommuters showed a significantly higher prevalence of depression after full adjustment (OR: 1.980, 95% CI: 1.126–3.481) compared with active office workers. The analyses of workers with high-strain showed significant ORs for most outcomes including insomnia (OR: 2.555, 95% CI: 1.473–4.433), musculoskeletal pain (OR: 2.786, 95% CI: 1.719–4.517), headaches/eye strain (OR: 3.074, 95% CI: 1.992–4.745) and presenteeism (OR: 1.932, 95% CI: 1.193–3.131) in the Model 3.
Supplementary Table 2 shows the sensitivity analysis of the stratified logistic regression with further adjustment. Identical to the primary result, active workers had a significant association between telecommuting with depression and high-strain group showed the most outcome variables with significant OR.
Table 4 Odds ratios with 95% confidence intervals for health-related outcomes of telecommuters stratified by job demand-control model
|
Characteristics |
Number (%)a
|
Model 1 |
Model 2b
|
Model 3c
|
|
Low-strain |
|
|
|
|
|
Depression |
29 (19.61) |
1.385 (0.747–2.566) |
1.363 (0.728–2.549) |
1.309 (0.699–2.453) |
|
Insomnia |
4 (3.06) |
0.609 (0.190–1.954) |
0.483 (0.146–1.599) |
0.489 (0.147–1.622) |
|
Musculoskeletal pain |
59 (40.65) |
2.037 (1.247–3.326)**
|
1.893 (1.121–3.195)*
|
1.830 (1.089–3.075)*
|
|
Headache, eye strain |
48 (33.15) |
1.813 (1.092–3.010)*
|
1.658 (0.943–2.915) |
1.547 (0.887–2.699) |
|
Absenteeism |
8 (5.39) |
1.806 (0.577–5.659) |
1.543 (0.515–4.628) |
1.570 (0.524–4.704) |
|
Presenteeism |
17 (11.44) |
1.609 (0.782–3.310) |
1.492 (0.721–3.086) |
1.556 (0.745–3.253) |
|
Active |
|
|
|
|
|
Depression |
85 (39.06) |
2.004 (1.157–3.473)*
|
1.906 (1.085–3.348)*
|
1.980 (1.126–3.481)*
|
|
Insomnia |
36 (16.10) |
1.544 (0.757–3.149) |
1.352 (0.620–2.949) |
1.408 (0.648–3.060) |
|
Musculoskeletal pain |
83 (37.44) |
0.987 (0.617–1.578) |
0.928 (0.562–1.532) |
0.919 (0.550–1.535) |
|
Headache, eye strain |
97 (43.48) |
1.499 (0.928–2.423) |
1.408 (0.849–2.336) |
1.395 (0.834–2.334) |
|
Absenteeism |
18 (7.96) |
1.248 (0.602–2.589) |
1.180 (0.537–2.593) |
1.177 (0.524–2.643) |
|
Presenteeism |
46 (20.80) |
1.437 (0.812–2.543) |
1.313 (0.719–2.396) |
1.359 (0.740–2.496) |
|
Passive |
|
|
|
|
|
Depression |
19 (27.53) |
1.072 (0.380–3.022) |
1.014 (0.381–2.699) |
1.013 (0.385–2.667) |
|
Insomnia |
4 (5.38) |
1.638 (0.437–6.135) |
1.431 (0.369–5.554) |
1.488 (0.380–5.831) |
|
Musculoskeletal pain |
32 (46.22) |
3.347 (1.555–7.204)**
|
3.235 (1.450–7.220)**
|
3.079 (1.446–6.559)**
|
|
Headache, eye strain |
19 (27.57) |
1.839 (0.884–3.827) |
1.616 (0.728–3.586) |
1.672 (0.766–3.649) |
|
Absenteeism |
3 (3.78) |
1.547 (0.443–5.398) |
1.566 (0.431–5.684) |
1.570 (0.420–5.871) |
|
Presenteeism |
7 (9.81) |
1.562 (0.619–3.944) |
1.528 (0.591–3.954) |
1.439 (0.517–4.000) |
|
High-strain |
|
|
|
|
|
Depression |
49 (32.94) |
0.927 (0.581–1.479) |
0.941 (0.575–1.539) |
0.953 (0.583–1.556) |
|
Insomnia |
33 (22.46) |
2.472 (1.464–4.173)**
|
2.370 (1.371–4.097)**
|
2.555 (1.473–4.433)**
|
|
Musculoskeletal pain |
86 (57.95) |
2.720 (1.728–4.283)**
|
2.637 (1.632–4.260)**
|
2.786 (1.719–4.517)**
|
|
Headache, eye strain |
88 (59.38) |
2.996 (1.929–4.654)**
|
3.003 (1.933–4.663)**
|
3.074 (1.992–4.745)**
|
|
Absenteeism |
7 (4.72) |
1.053 (0.464–2.388) |
0.954 (0.411–2.214) |
0.961 (0.408–2.264) |
|
Presenteeism |
39 (26.58) |
1.841 (1.129–3.002)*
|
1.745 (1.076–2.830)*
|
1.932 (1.193–3.131)**
|
DISCUSSION
This study demonstrated that telecommuters had higher job demands and control than office workers. Telecommuters were more likely to have health-related problems than office workers. Health-related problems, including insomnia, musculoskeletal pain, headache/eye strain, and presenteeism, were most frequently observed in telecommuters with high-strain workers.
Previous studies have shown that the risk to workers’ well-being posed by telecommuting is mediated by job demands and control. The job satisfaction of European teleworking teachers during the COVID-19 pandemic decreased as the job demands increased (coefficient −0.10,
p-value 0.020).
27 Job control and autonomy of telecommuters were associated with high productivity, low emotional exhaustion, and low cognitive stress.
16,28 A study by Ikegami et al.
29 found that job control was significantly higher among telecommuters, regardless of telecommuting frequency and that the high-frequency telecommuting group showed a negative, although insignificant, association with job demands, which contradicted our findings. However, their study was limited to correlating changes in occupational stress with improvements or degradation of health among telecommuters. To the best of our knowledge, our study was the first to explore the variability in health outcomes of telecommuting based on job demands and control.
Consistent to our findings, previous studies have examined the physical and mental health risks of telecommuting. Tejero et al.
28 reported a significant reduction in workers’ mean sleep quality scores during teleworking in the Philippines. Majumdar et al.
30 conducted an online survey during the COVID-19 wave in India and found that the sleep duration and depressive symptoms of remote workers worsened significantly. One case-control study in Turkey conducted during the lockdown associated with the COVID-19 pandemic identified higher low back pain in the group working from home than office.
31 Steidelmüller et al.
32 explored the relationship between telecommuting frequency and presenteeism and revealed a higher prevalence of presenteeism among telecommuters. However, one Canadian study indicated that telecommuters’ burnout, general mental health problems, and neck/shoulder pain decreased after 6 months of follow-up.
33
The telecommuting work environment contributes to poor health outcomes among telecommuters. As long commute times were linked to multiple medical conditions, our findings suggest that telecommuters are exposed to unique risk factors that differ from those of office workers.
34 Some studies have shown that disengagement from work is difficult to attain among telecommuters, due to work accessibility through remote communication.
28,35 Thus, telecommuters are at a high risk of irregular and night work, which induces insomnia and physical illness.
36 Telecommuters are expected to spend more time before visual devices and connected online, as observed in our study population (
Supplementary Table 3). The prolonged use of VDTs among telecommuters is a predictor of ocular symptoms and insomnia.
37,38 Decreased OR of insomnia and headache/eye strain after adjusted for VDT use from our sensitivity analysis supports such a modulating effect. Moreover, a significant association between increased Internet use for teleworking during COVID-19 and sleep disturbances was revealed.
39 The ergonomic suitability of in-house workstations during VDT use is easily compromised, which negatively affects the musculoskeletal symptoms of telecommuters.
40 Indeed, the effect size of telecommuting on musculoskeletal pain was alleviated in the model including VDT use as a confounder. Unless provided by the employer, teleworkers are not equipped with ergonomic desks or supplies.
41 Compared with office workers who move during the commute or at their workplace, telecommuters have a paucity of exercise and are prone to musculoskeletal pain.
42 Contrarily, telecommuters were more likely to be physically active in our sample, possibly due to the survey questionnaire including leisure and cultural activities simultaneously. Further study is needed to uncover the moderating role of exercise habit in the relationship between telecommuting and musculoskeletal pain. A higher prevalence of presenteeism is related to the minimal physical demand of commuting, which enables telecommuters to continue working under mild-to-moderate disease conditions. Telecommuters who are ill may engage in self-endangering behavior by arranging regular work in the evening after medical treatment.
43
Importantly, our study revealed that the high-strain group had the highest risk of negative health effects from telecommuting. Corresponding result from the sensitivity analysis indicates the robustness of our finding. Correcting high job demands and low job control is the key to minimizing the negative impact of telecommuting on health. Owing to low job control to buffer the heavy workload, workers with high-strain have weak resilience to telecommuting-induced stress. Unlike office workers, whose work terminates as they clock out (reference), high-strain telecommuters are at risk of working overtime to keep up with high workloads or strict deadlines. Extended working hours using communication devices are closely related to insomnia and eye strain. In our study, workers with low job control (passive, high-strain) were more susceptible to musculoskeletal pain due to telecommuting. Job control allows telecommuters to take breaks as needed; thus, ergonomic stress may not exceed the pain threshold. The relatively high proportion of female in the low job control group partially supports these findings. Increased physical load among female telecommuters due to household chores facilitates the onset of musculoskeletal symptoms.
44 Given the freely accessible nature of remote work, telecommuters with high job demands (active, high-strain) may be subject to presenteeism. However, the association between telecommuting and presenteeism was not significant among the active group. We speculated that, regardless of the work location, active workers were flexible in adjusting their work schedules while sick. Surprisingly, active workers were the only subgroup that presented with higher odds of depression due to telecommuting. Active workers exhibited high engagement and motivation toward the job to cope with job-related stress.
45 As the intrinsic motivation of workers declines with continuous telecommuting, prolonged teleworking during the COVID-19 pandemic could trigger depression.
46 Further analysis is required to verify whether other psychological factors, such as social isolation and coworkers’ support, contribute to mental health challenges in active telecommuters.
1,47
Our study used data from a nationwide random sample to achieve external validity. Furthermore, this study used a clear definition of telecommuters in the selection process. We minimized the selection bias by setting up a control group comparable to telecommuters. However, this study had several limitations. The cross-sectional design of this study is a major concern. As we could not determine the temporal antecedents of exposure and outcome, the results were susceptible to reverse causality. Second, all data was collected from participants’ responses; therefore, a recall bias may exist. Especially, the experience of mental or physical illness was not confirmed by a healthcare professional. Third, although our definition of job demands and control was grounded in the existing literature, there is no consensus in the field on the operational definition of parameters using KWCS variables. Multiple studies have attempted to develop job demand and control measures out of KWCS survey questionnaires, yet no research has presented the instrument with optimal validity and reliability.
48,49 Cronbach’s alpha of the items in our study exceeded 0.6, deemed acceptable in terms of reliability.
50 Lastly, the survey did not investigate health-related lifestyles, comorbidities, or telecommuting spontaneity, which could have modulated the relationship between telecommuting and health.
51 Potential confounding effects may not have been completely eliminated.
CONCLUSIONS
This study demonstrated a significant negative association between telecommuting and health outcomes in South Korean workers during the COVID-19 pandemic. Subgroup analysis using the JDC model showed different health effects of telecommuting on workers’ health. Teleworkers with high job demands, low job control, and high-strain had a higher prevalence of insomnia, musculoskeletal pain, headaches/eye strain, and presenteeism. To successfully prevent the public health crisis associated with telecommuters, policies that limit job demands and sustain job control should be implemented.
Acknowledgements
The authors thank the Occupational Safety and Health Research Institute of Korea.
Abbreviations
information and communication technology
International Labour Organization
Korean Working Conditions Survey
World Health Organization
NOTES
-
Funding: This work was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and Technology (grant number, 2022R1A2C2010463).
-
Competing interests: The authors declare that they have no competing interests.
-
Author contributions:
Conceptualization: Ryoo SW, Min KB.
Data curation: Ryoo SW, Son SY.
Formal analysis: Ryoo SW.
Funding acquisition: Min KB.
Methodology: Ryoo SY, Min KB.
Software: Ryoo SW, Choi J.
Validation: Min JY, Min KB.
Visualization: Ryoo SW, Choi BY.
Writing - original draft: Ryoo SW, Min JY.
Writing - review & editing: Min KB, Son SY, Choi BY, Choi J.
SUPPLEMENTARY MATERIALS
Supplementary Data 1
Sensitivity analysis: definition of additional confounders
aoem-36-e14-s001.doc
Supplementary Table 1
Odds ratios with 95% confidence intervals for health-related outcomes according to telecommuting status after further adjustment
aoem-36-e14-s002.xls
Supplementary Table 2
Odds ratios with 95% confidence intervals for health-related outcomes of telecommuters stratified by JDC model after further adjustment
aoem-36-e14-s003.xls
Supplementary Table 3
Distribution of additional confounding factors among the participants according to work arrangement and job demand-control model
aoem-36-e14-s004.xls
REFERENCES
REFERENCES
- 1. Allen TD, Golden TD, Shockley KM. How effective is telecommuting? Assessing the status of our scientific findings. Psychol Sci Public Interest 2015;16(2):40–68. 26403188.ArticlePubMedPDF
- 2. Berg J, Humblet M, Soares S. Working from home: from invisibility to decent work. Updated 2021]. Accessed September 1, 2021].
www.ilo.org/global/publications/books/WCMS_765806/lang--en/index.htm
.
- 3. Belzunegui-Eraso A, Erro-Garcés A. Teleworking in the context of the COVID-19 crisis. Sustainability 2020;12(9):3662.Article
- 4. Ha T. COVID-19 and remote work inequality: evidence from South Korea. Labor Hist 2022;63(3):406–420.Article
- 5. Oakman J, Kinsman N, Stuckey R, Graham M, Weale V. A rapid review of mental and physical health effects of working at home: how do we optimise health? BMC Public Health 2020;20(1):1825. 33256652.ArticlePubMedPMCPDF
- 6. Henke RM, Benevent R, Schulte P, Rinehart C, Crighton KA, Corcoran M. The effects of telecommuting intensity on employee health. Am J Health Promot 2016;30(8):604–612. 26389981.ArticlePubMedPDF
- 7. Gajendran RS, Harrison DA. The good, the bad, and the unknown about telecommuting: meta-analysis of psychological mediators and individual consequences. J Appl Psychol 2007;92(6):1524–1541. 18020794.ArticlePubMed
- 8. Amster Y. Healthy and safe telework: a WHO/ILO technical brief. Saf Health Work 2022;13:S303–S304.Article
- 9. Harpaz I. Advantages and disadvantages of telecommuting for the individual, organization and society. Work Study 2002;51(2):74–80.Article
- 10. Gomez IN, Suarez CG, Sosa KE, Tapang ML. Work from home-related musculoskeletal pain during the COVID-19 pandemic: a rapid review. Int J Osteopath Med 2022;43:49–52. 35401773.ArticlePubMedPMC
- 11. Magnavita N, Tripepi G, Chiorri C. Telecommuting, off-time work, and intrusive leadership in workers’ well-being. Int J Environ Res Public Health 2021;18(7):3330. 33804828.ArticlePubMedPMC
- 12. Noonan MC, Glass JL. The hard truth about telecommuting. Mon Labor Rev 2012;135:38.
- 13. Dahlgren A, Kecklund G, Åkerstedt T. Overtime work and its effects on sleep, sleepiness, cortisol and blood pressure in an experimental field study. Scand J Work Environ Health 2006;32(4):318–327. 16932830.ArticlePubMed
- 14. Ryoo SW, Min JY, Lee DW, Choi BY, Choi J, Kim HY, et al. Telecommuting-related health outcomes during the COVID-19 pandemic in South Korea: a national population-based cross-sectional study. BMC Public Health 2023;23(1):549. 36959592.ArticlePubMedPMCPDF
- 15. Quick JC, Henderson DF. Occupational stress: preventing suffering, enhancing wellbeing. Int J Environ Res Public Health 2016;13(5):459. 27136575.ArticlePubMedPMC
- 16. Vander Elst T, Verhoogen R, Sercu M, Van den Broeck A, Baillien E, Godderis L. Not extent of telecommuting, but job characteristics as proximal predictors of work-related well-being. J Occup Environ Med 2017;59(10):e180–e186. 28820860.ArticlePubMed
- 17. Karasek RA Jr. Job demands, job decision latitude, and mental strain: Implications for job redesign. Adm Sci Q 1979;24(2):285–308.Article
- 18. Hannan LM, Monteilh CP, Gerr F, Kleinbaum DG, Marcus M. Job strain and risk of musculoskeletal symptoms among a prospective cohort of occupational computer users. Scand J Work Environ Health 2005;31(5):375–386. 16273964.ArticlePubMed
- 19. Bonde JP. Psychosocial factors at work and risk of depression: a systematic review of the epidemiological evidence. Occup Environ Med 2008;65(7):438–445. 18417557.ArticlePubMed
- 20. Fernet C, Guay F, Senécal C. Adjusting to job demands: the role of work self-determination and job control in predicting burnout. J Vocat Behav 2004;65(1):39–56.Article
- 21. Parent-Thirion A, Biletta I, Cabrita J, Vargas Llave O, Vermeylen G, Wilczyńska A, et al. Sixth European Working Conditions Survey - Overview Report. Luxembourg: Publications Office of the European Union; 2016.
- 22. Korea Occupational Safety & Health Agency (KOSHA). Sixth Korean Working Conditions Survey, Analysis Report. Ulsan, Korea: KOSHA; 2021.
- 23. Lee J, Kim HR, Lee DW, Kang MY. Interaction between occupational physical burdens and low job control on musculoskeletal pain: analysis of the 5th Korean Working Environment Survey. J Occup Health 2021;63(1):e12244. 34212460.ArticlePubMedPMCPDF
- 24. Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom 2015;84(3):167–176. 25831962.ArticlePubMedPDF
- 25. Broman JE, Smedje H, Mallon L, Hetta J. The Minimal Insomnia Symptom Scale (MISS): a brief measure of sleeping difficulties. Ups J Med Sci 2008;113(2):131–142. 18509808.PubMed
- 26. Yang YJ, Lee J. Association between depressive symptoms and employment type of Korean workers: the Fifth Korean Working Conditions Survey. BMC Public Health 2024;24(1):93. 38178074.ArticlePubMedPMCPDF
- 27. Mahmood F, Ariza-Montes A, Saleem M, Han H. Teachers’ teleworking job satisfaction during the COVID-19 pandemic in Europe. Curr Psychol 2023;42(10):8540–8553. 34690478.ArticlePubMedPDF
- 28. Tejero LM, Seva RR, Fadrilan-Camacho VF. Factors associated with work-life balance and productivity before and during work from home. J Occup Environ Med 2021;63(12):1065–1072. 34560760.ArticlePubMedPMC
- 29. Ikegami K, Baba H, Ando H, Hino A, Tsuji M, Tateishi S, et al. Job stress among workers who telecommute during the coronavirus disease (COVID-19) pandemic in Japan: a cross-sectional study. Int J Occup Med Environ Health 2022;35(3):339–351. 35289338.ArticlePubMedPMCPDF
- 30. Majumdar P, Biswas A, Sahu S. COVID-19 pandemic and lockdown: cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiol Int 2020;37(8):1191–1200. 32660352.ArticlePubMed
- 31. Toprak Celenay S, Karaaslan Y, Mete O, Ozer Kaya D. Coronaphobia, musculoskeletal pain, and sleep quality in stay-at home and continued-working persons during the 3-month COVID-19 pandemic lockdown in Turkey. Chronobiol Int 2020;37(12):1778–1785. 32878506.ArticlePubMed
- 32. Steidelmüller C, Meyer SC, Müller G. Home-based telework and presenteeism across Europe. J Occup Environ Med 2020;62(12):998–1005. 32796258.ArticlePubMedPMC
- 33. Somasundram KG, Hackney A, Yung M, Du B, Oakman J, Nowrouzi-Kia B, et al. Mental and physical health and well-being of Canadian employees who were working from home during the COVID-19 pandemic. BMC Public Health 2022;22(1):1987. 36316683.ArticlePubMedPMCPDF
- 34. Kim S, Kim Y, Lim SS, Ryoo JH, Yoon JH. Long commute time and sleep problems with gender difference in work–life balance: a cross-sectional study of more than 25,000 workers. Saf Health Work 2019;10(4):470–475. 31890330.ArticlePubMedPMC
- 35. Eddleston KA, Mulki J. Toward understanding remote workers’ management of work–family boundaries: the complexity of workplace embeddedness. Group Organ Manage 2017;42(3):346–387.ArticlePDF
- 36. Boivin DB, Tremblay GM, James FO. Working on atypical schedules. Sleep Med 2007;8(6):578–589. 17481949.ArticlePubMed
- 37. Fjaervoll H, Fjaervoll K, Magno M, Moschowits E, Vehof J, Dartt DA, et al. The association between visual display terminal use and dry eye: a review. Acta Ophthalmol 2022;100(4):357–375. 34697901.ArticlePubMedPDF
- 38. Yoshioka E, Saijo Y, Fukui T, Kawaharada M, Kishi R. Association between duration of daily visual display terminal work and insomnia among local government clerks in Japan. Am J Ind Med 2008;51(2):148–156. 18161872.ArticlePubMed
- 39. Costa C, Teodoro M, Mento C, Giambò F, Vitello C, Italia S, et al. Work performance, mood and sleep alterations in home office workers during the COVID-19 pandemic. Int J Environ Res Public Health 2022;19(4):1990. 35206177.ArticlePubMedPMC
- 40. Seva RR, Tejero LM, Fadrilan-Camacho VF. Barriers and facilitators of productivity while working from home during pandemic. J Occup Health 2021;63(1):e12242. 34181307.ArticlePubMedPMCPDF
- 41. Radulović AH, Žaja R, Milošević M, Radulović B, Luketić I, Božić T. Work from home and musculoskeletal pain in telecommunications workers during COVID-19 pandemic: a pilot study. Arh Hig Rada Toksikol 2021;72(3):232–239. 34587664.ArticlePubMedPMC
- 42. Šagát P, Bartík P, Prieto González P, Tohănean DI, Knjaz D. Impact of COVID-19quarantine on low back pain intensity, prevalence, and associated risk factors among adult citizens residing in Riyadh (Saudi Arabia): a cross-sectional study. Int J Environ Res Public Health 2020;17(19):7302. 33036287.ArticlePubMedPMC
- 43. Ruhle SA, Schmoll R. COVID-19, telecommuting, and (virtual) sickness presenteeism: working from home while ill during a pandemic. Front Psychol 2021;12:734106. 34721202.ArticlePubMedPMC
- 44. Dos Santos IN, Pernambuco ML, da Silva AM, Ruela GA, de Oliveira AS. Association between musculoskeletal pain and telework in the context of the COVID 19 pandemic: an integrative review. Rev Bras Med Trab 2021;19(3):342–350. 35774766.ArticlePubMedPMC
- 45. Demerouti E, Bakker AB, de Jonge J, Janssen PP, Schaufeli WB. Burnout and engagement at work as a function of demands and control. Scand J Work Environ Health 2001;27(4):279–286. 11560342.ArticlePubMed
- 46. Jamal MT, Anwar I, Khan NA. Voluntary part-time and mandatory full-time telecommuting: a comparative longitudinal analysis of the impact of managerial, work and individual characteristics on job performance. Int J Manpow 2022;43(6):1316–1337.Article
- 47. Probst T, Budimir S, Pieh C. Depression in and after COVID-19 lockdown in Austria and the role of stress and loneliness in lockdown: a longitudinal study. J Affect Disord 2020;277:962–963. 33065839.ArticlePubMedPMC
- 48. Kim G, Min B, Jung J, Paek D, Cho S. The association of relational and organizational job stress factors with sleep disorder: analysis of the 3rd Korean working conditions survey (2011). Ann Occup Environ Med 2016;28(1):1–11. 26835129.ArticlePubMedPMCPDF
- 49. Jung SW, Lee JH, Lee KJ. Assessing the association between emotional labor and presenteeism among nurses in Korea: cross-sectional study using the 4th Korean Working Conditions Survey. Saf Health Work 2020;11(1):103–108. 32206380.ArticlePubMed
- 50. Shi J, Mo X, Sun Z. Content validity index in scale development. J Cent South Univ Med Sci 2012;37(2):152–155.
- 51. Kaduk A, Genadek K, Kelly EL, Moen P. Involuntary vs. voluntary flexible work: insights for scholars and stakeholders. Community Work Fam 2019;22(4):412–442. 36090310.ArticlePubMedPMC
 , Jin-Young Min2
, Jin-Young Min2 , Seok-Yoon Son1
, Seok-Yoon Son1 , Baek-Yong Choi1
, Baek-Yong Choi1 , Juho Choi1
, Juho Choi1 , Kyoung-Bok Min1
, Kyoung-Bok Min1

 KSOEM
KSOEM

 Cite
Cite

