Abstract
-
Background
This study was conducted to identify the success rate for smoking cessation over time after participation in a therapeutic smoking cessation camp, and to identify how participant characteristics, including a supportive workplace environment for smoking cessation (SWESC), affect the success rate for smoking cessation.
-
Methods
In all, 296 participants at smoking cessation camps in Ulsan between 2015 and 2020 were investigated. The success rates of smoking cessation after weeks 4, 6, 12, and 24 at camp were investigated. The participants were grouped as workers with an SWESC, and workers without an SWESC, and variables (age, education, household income, marital status, drinking, exercise, body mass index, morbidity, job, number of counseling sessions, cigarettes smoked per day and smoking initiation age) were investigated. Multiple logistic regression analysis was conducted at each time point. In addition, Cox regression analysis was performed to evaluate the variables affecting the success rate for smoking cessation over time.
-
Results
The smoking cessation success rate of workers with an SWESC at week 24 (90.7%) was higher than that for workers without an SWESC (60.5%). Multiple logistic regression was performed to determine the relationship between each variable and the success rates for smoking cessation at week 6, 12, and 24. SWESC was confirmed as significant (p < 0.05) variables for increased success rate for smoking cessation at all 3 time points. After adjusting for all variables, the Cox proportional hazards survival analysis showed a hazard ratio of 6.17 for SWESC (p < 0.001,; 95% confidence interval: 3.08–12.38).
-
Conclusions
At a professional treatment smoking cessation camp, participants with an SWESC showed a significantly higher success rate for smoking cessation. Supportive workplace environment for workers’ health is expected to be an important factor for smoking cessation projects as well as other health promotion projects at workplace.
-
Keywords: smoking cessation; smoking cessation camp; supportive workplace environment; heavy smoker; workplace health promotion
BACKGROUND
Smoking is a leading cause of preventable deaths,
1,2,3 one of the greatest public health threats facing the world. Smoking imposes a huge social and economic burden, including the payment of medical expenses and the loss of human resources due to disease morbidity and death.
4,5 The cessation of smoking leads to instant, long-term health benefits at all ages.
6,7 Previous study has shown that smoking cessation reduces anxiety, depression, and stress; improves mental health; and does not negatively affect social relationships.
8 Thus, the importance of promoting smoking cessation in national health policy cannot be overemphasized.
The smoking rate for Korean adults was 35.1% in 1998, relatively higher than that of other countries.
9 Since then, the government has implemented a range of anti-smoking policies, including the creation of smoking cessation clinics, and the smoking rate has continued to decrease, reaching 22.3% in 2017.
10 However, the trend of decline in smoking rates has slowed since the 2010s.
10 This indicated the need for a new smoking-cessation policy, and in 2015, the Korean Ministry of Health and Welfare established smoking cessation support centers across 18 regions nationwide and introduced specialized treatment-type smoking cessation camps.
A ‘specialized smoking cessation’ camp is a 4-night, 5-day smoking cessation program. Its main targets are heavy smokers (having smoked for more than 20 years), those who have difficulty to ceasing smoking, and those who continue to smoke even after being diagnosed with smoking-related disease. During the course of the camp, the participants maintain their non-smoking status; and are provided with smoking cessation-related education, psychological counseling, and medications and supplements for smoking cessation. The counseling is provided for all 5 the days of the camp. As a follow-up the camp, telephone counseling is provided once a month. The participants can receive additional counseling to maintain smoking cessation.
A smoking cessation center in Ulsan, Korea, has been running smoking cessation camp since 2015. Most participants came to the camp through advertisements or recommendations from medical staff; some camp participants were registered through a major company that promotes smoking cessation as part of a workplace health policy. If employees who participate in a smoking cessation camp succeed in smoking cessation as measured by a cotinine test 24 weeks after camp participation, the company provides compensation and has a workplace environment that is supportive of smoking cessation.
We posited that these characteristics of camp participants would contribute to the higher smoking cessation rate. The supportive individual environment around a person who tried to quit smoking, including family and colleagues, influences smoking cessation success rates.
11 However, little research has been conducted on how a supportive policy at the workplace level would affect the success of smoking cessation. This study evaluates the effect of workplace-level supportive policies for smoking cessation on the success rate for smoking cessation and identifies other factors related to the smoking cessation, to improve the effectiveness of smoking cessation services.
METHODS
Study design and participants
We conducted a survey targeting 568 male subjects who agreed to participate in the study from the participants in the smoking cessation camp hosted at the smoking cessation support center in Ulsan, Korea, from October 2015 to December 2020.
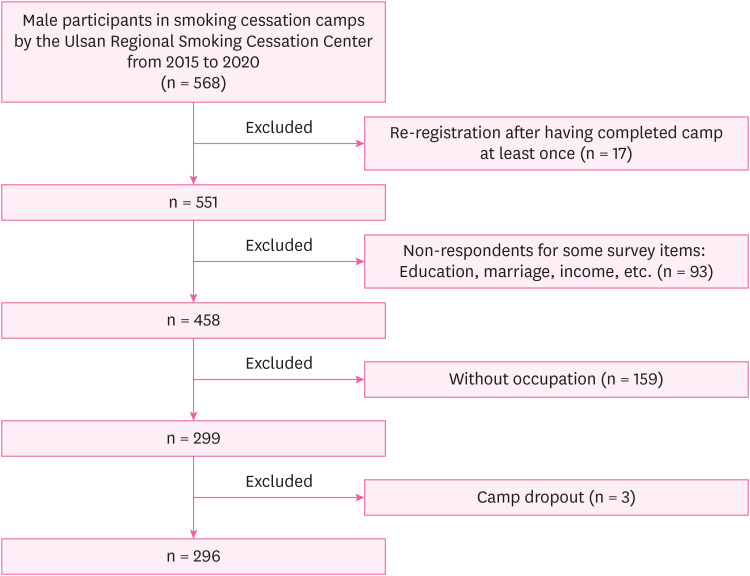
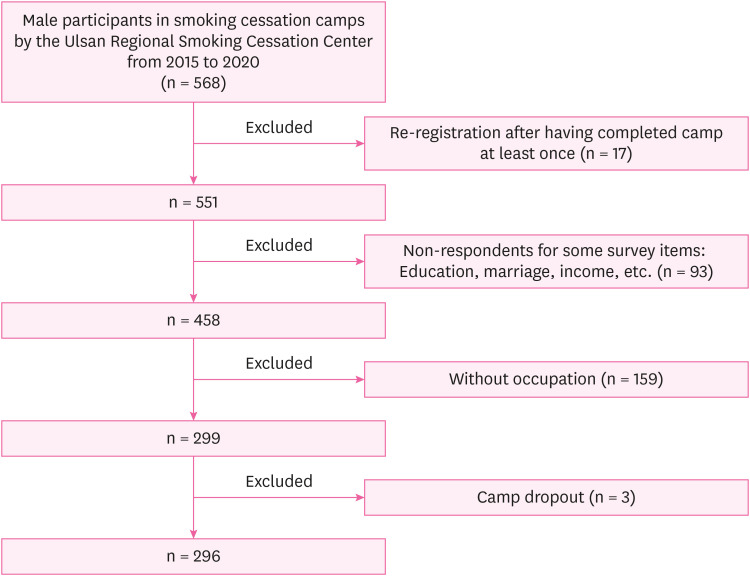
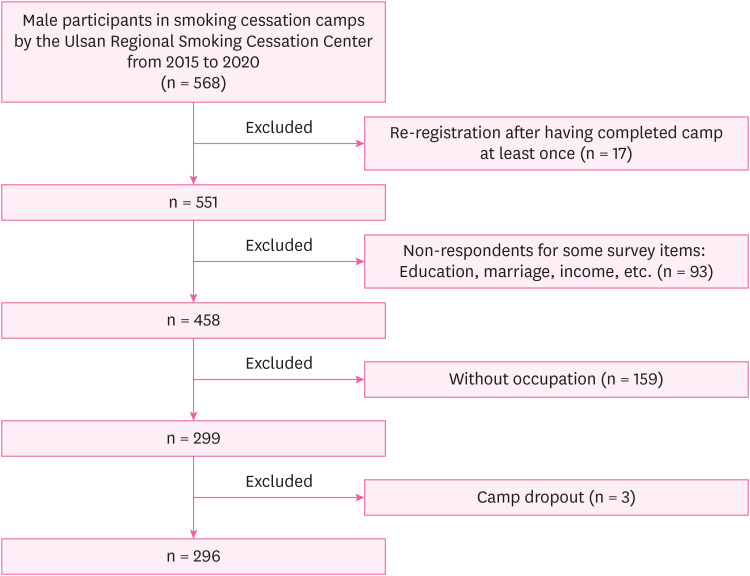
Fig. 1 illustrates the process of selecting study participants. Among the male participants in smoking cessation camps by the Ulsan Regional Smoking Cessation Center from 2015 to 2020, some participants had not succeeded in quitting smoking after participating in their first time at the camp and participated in the smoking cessation camp more than one time. Previous camp participation experience could affect subsequent experiences, leading to differences in the success rate for smoking cessation from that of first-time participants.
12 Therefore, for the homogeneity of the data, the statistics were processed as the result obtained in the first participation (failure) regardless of the ultimate success or failure after re-registration. For the analysis of occupational factor, participants without occupation were excluded. Those who did not respond to any survey item (including education, marriage, income, and so on) and those who dropped out of camp for personal reasons were excluded. A total of 296 participants were analyzed for statistics finally.
Fig. 1Flow chart of selecting study subjects of smoking cessation camp (2015–2020).
Measurement
On the first day of camp, data on the demographic and socioeconomic characteristics of the participants were collected, including age, education level, marital status, and monthly income. Age was classified as young (< 44 years old), middle-aged (45–64 years old), and old (> 64 years old) at time of registration, in accordance with the seniority standards of the Elderly Welfare Act of Korea. For marital status, the group was divided into those that could receive emotional support for smoking cessation due to currently living with a spouse; and others (not married, separated, divorced, or widowed). Household incomes were classified into more than and less than 4,000,000 KRW/month.
Among health-related factors, alcohol drinking, exercise, body mass index (BMI), and morbidity of participants were collected. Drinking alcohol was assessed by drinking at least once per week for the past year. Exercise was based on exercising at least once a week for the past year. BMI was classified based on the obesity diagnosis criterion of 25 kg/m
2.
13 Morbidity was defined as diagnosed by a doctor with one or more of hypertension, diabetes, hyperlipidemia, cancer, lung disease, and cardiovascular disease.
Work-related factors included a supportive workplace environment for smoking cessation (SWESC) and occupation. Workers with a SWESC were defined as an employee of their aforementioned company, and who benefited from the company’s policy of smoking cessation camp. The company adjusts work hours to allow workers to utilize their annual leaves and participate in smoking cessation camps. If the participants are found to have successfully quit smoking through a cotinine test after 24 weeks of participating in a smoking cessation camp, their used annual leaves will be replaced with additional paid leaves. The company provides work replacement helpers during the camp period to reduce the burden on the employee on returning to work. The participants’ occupations were classified according to the Korean Standard Occupational Classification
14: white-collar (manager, professional, clerk), service/sales (service worker, sales worker), blue-collar (skilled agricultural and fishery worker, craft and related trades worker, plant and machine operator and assembler, elementary occupation).
The camp-related factor (number of counseling sessions during and after participation in the smoking cessation camp) was counted and classified into 2 groups: 11 or more sessions and less than 11 sessions. Counselors specialized in smoking cessation provided counseling for approximately 30 minutes, covering recommendations for quitting smoking depending on the participant’s type of smoking and coping with the stress of quitting smoking. Counseling session had been conducted once a day for 5 days of camp, and phone counseling was provided once a month after the camp ended. If the participants wish, participants can receive additional counseling by visiting a smoking cessation center or by phone. Therefore, participants who receive follow-up counseling for 6 months will receive at least 11 counseling sessions.
Smoking-related factors included age of smoking initiation and number of cigarettes smoked per day. The age of smoking initiation was classified based on 20 years of age. The cigarettes smoked per day was divided into smoking more than 1 pack (20 cigarettes) per day and smoking less than 1 pack.
Follow-up to determine whether smoking cessation was successful
The follow-ups after camp were conducted by visits to the smoking cessation center located at the hospital conducting the smoking cessation camp or phone call at week 4, 6, 12, and 24. Smoking cessation success was assessed by conducting the test using the camp participant’s preferred method, including self-report by the phone, expiratory carbon monoxide (CO) test, or urine cotinine test. Urine cotinine was considered positive or negative using an immunoassay dipstick with a cutoff of 20 ng/mL (cotinine urine rapid test),
15 and the cutoff for expiratory CO was 5 ppm.
16 Smoking cessation is considered successful if the urine cotinine test result is negative, exhaled CO is detected as less than 5 ppm, or if the self-report indicates that the participant is continuing to quit smoking.
To encourage objective measurement rather than self-report, free gifts are provided when participants visit and take an exhaled CO or cotinine test. If participants choose to self-report, they will not receive benefits provided by the company as compensation for their success in quitting smoking, even if they respond that they have succeeded in quitting smoking. Therefore, it is believed that workers with an SWESC will be deterred from falsely reporting success in quitting smoking due to reward motivation.
Statistical analysis
Participants were classified as workers with an SWESC and workers without an SWESC, and their categorical variables (age, education, household income, marital status, alcohol, exercise, BMI, morbidity, job, number of counseling sessions, cigarettes smoked per day, and smoking initiation age) were given as percentages. The smoking cessation success rates for workers with an SWESC and workers without an SWESC according to time points were counted and compared by cross sectional analysis.
Multiple logistic regression analysis was conducted at each time point to determine the relationship between the variables (age, education, household income, marital status, drinking, exercise, BMI, morbidity, occupation, SWESC, number of counseling, cigarettes smoked per day, and smoking initiation age) and smoking cessation success.
From the study results, Cox proportional hazards regression analysis was performed to evaluate difference in smoking cessation rate according to having an SWESC. The hazard ratio (HR) was estimated using data measuring smoking cessation at 4 time points following the camp, up to week 24. Model 1 showed univariate analysis including only the effects of an SWESC. In Model 2, multivariate analysis was performed by adjusting all the factors investigated in this study, namely, age, marital status, education, household income, alcohol drinking, exercise, BMI, occupation, morbidity, number of counseling sessions, daily smoking amount, and smoking initiation age. In addition, multivariate analysis was conducted in Model 3 for the factors with a significant effect on the smoking cessation in the results of Model 2.
Data were analyzed using the Statistical Package for Social Sciences for Windows, Version 24.0 (IBM Corp., Armonk, NY, USA). The confidence interval (CI) was set at 95%, and the level of significance was set at p < 0.05 in all statistical analysis.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board (IRB) of Ulsan University Hospital before implementation (IRB File No. 2021-07-019).
RESULTS
Table 1 presents the method of measuring smoking cessation success at each time point. More than 60% of participants were confirmed to have successfully quit smoking using objective measures such as CO and urine cotinine at weeks 4, 12 and 24. The final success rate at week 24 was 73.6%.
Table 1 Smoking cessation rate according to measurement method
|
Week |
Failure |
Self-report |
CO |
Urine cotinine |
CO and urine cotinine |
Total |
|
Week 4 |
5 (1.7) |
85 (28.7) |
54 (18.2) |
17 (5.7) |
135 (45.6) |
296 |
|
Week 6 |
19 (6.4) |
187 (63.2) |
24 (8.1) |
10 (3.4) |
56 (18.9) |
296 |
|
Week 12 |
33 (11.1) |
77 (26.0) |
7 (2.4) |
25 (8.4) |
154 (52.0) |
296 |
|
Week 24 |
78 (26.4) |
30 (10.1) |
2 (0.7) |
31 (10.5) |
155 (52.4) |
296 |
Table 2 classifies the participants into workers without an SWESC (n = 167) and workers with an SWESC (n = 129), and the ratio of each variable was analyzed using chi-square analysis or Fisher’s exact test. Workers with an SWESC were mostly blue-collar workers (94.6%). The percentage of blue-collar workers among workers without an SWESC was 50.3%, which was not as high as in workers with an SWESC, but blue-collar workers were still more than a half.
Table 2 General characteristics, health-related characteristics, work-related characteristic, camp-related characteristic and smoking-related characteristics of camp participants
|
Variables |
Workers without an SWESC (n = 167) |
Workers with an SWESC (n = 129) |
Total (n = 296) |
p-value |
|
General characteristics |
|
|
|
|
|
Age (years) |
|
|
|
< 0.001***
|
|
|
< 45 |
32 (19.2) |
14 (10.9) |
46 (15.5) |
|
|
45–64 |
121 (72.5) |
115 (89.1) |
236 (79.7) |
|
|
> 64 |
14 (8.4) |
0 (0) |
14 (4.7) |
|
Education |
|
|
|
< 0.001***
|
|
|
< High school |
8 (4.8) |
2 (1.6) |
10 (3.4) |
|
|
High school |
69 (41.3) |
92 (71.3) |
161 (54.4) |
|
|
≥ College |
90 (53.9) |
35 (27.1) |
125 (42.2) |
|
Household income (KRW) |
|
|
|
0.001**
|
|
|
≥ 4,000,000 |
76 (45.5) |
34 (26.4) |
110 (37.2) |
|
|
< 4,000,000 |
91 (54.5) |
95 (73.6) |
186 (62.8) |
|
Marital status |
|
|
|
0.075 |
|
|
With spouse |
138 (82.6) |
116 (89.9) |
254 (85.8) |
|
|
Without spouse |
29 (17.4) |
13 (10.1) |
42 (14.2) |
|
Health-related characteristics |
|
|
|
|
|
Alcohol drinking (last year) |
|
|
|
0.048*
|
|
|
Yes |
118 (70.7) |
77 (59.7) |
195 (65.9) |
|
|
No |
49 (29.3) |
52 (40.3) |
101 (34.1) |
|
Exercise (last year) |
|
|
|
0.002**
|
|
|
Yes |
95 (56.9) |
50 (38.8) |
145 (49.0) |
|
|
No |
72 (43.1) |
79 (61.2) |
151 (51.0) |
|
BMI (kg/m2) |
|
|
|
0.691 |
|
|
≥ 25 |
62 (37.1) |
45 (34.9) |
107 (36.1) |
|
|
< 25 |
105 (62.9) |
84 (65.1) |
189 (63.9) |
|
Morbidity |
|
|
|
< 0.001***
|
|
|
Yes |
61 (36.5) |
22 (17.1) |
83 (28.0) |
|
|
No |
106 (63.5) |
107 (82.9) |
213 (72.0) |
|
Work-related characteristics |
|
|
|
|
|
Job |
|
|
|
< 0.001***
|
|
|
White-collar |
52 (31.1) |
7 (5.4) |
59 (19.9) |
|
|
Service/Sales |
31 (18.6) |
0 (0) |
31 (10.5) |
|
|
Blue-collar |
84 (50.3) |
122 (94.6) |
206 (69.6) |
|
Camp-related characteristic |
|
|
|
|
|
Number of counseling sessions |
|
|
|
< 0.001***
|
|
|
≥ 11 |
85 (50.9) |
28 (21.7) |
113 (38.2) |
|
|
< 11 |
82 (49.1) |
101 (78.3) |
183 (61.8) |
|
Smoking-related characteristics |
|
|
|
|
|
Cigarettes smoked per day |
|
|
|
0.797 |
|
|
≥ 20 |
129 (77.2) |
98 (76.0) |
227 (76.7) |
|
|
< 20 |
38 (22.8) |
31 (24.0) |
69 (23.3) |
|
Smoking initiation age (years) |
|
|
|
0.092 |
|
|
≥ 20 |
98 (58.7) |
88 (68.2) |
186 (62.8) |
|
|
< 20 |
69 (41.3) |
41 (31.8) |
110 (37.2) |
Table 3 presents the success rate for smoking cessation for workers without an SWESC, and workers with an SWESC, by time. The success rate of workers with an SWESC was 100% at week 4, and remained high at week 6 (98.4%) and week 12 (97.7%). At week 24, the success rate for smoking cessation for workers without an SWESC (60.5%) was significantly lower than that of and workers with an SWESC (90.7%).
Table 3 Smoking cessation rate of workers without an SWESC and workers with an SWESC
|
Week |
Variable |
Workers without an SWESC |
Workers with an SWESC |
|
Week 4 |
Success |
162 |
129 |
|
Failure |
5 |
0 |
|
Success rate (%) |
97.0 |
100.0 |
|
pa
|
0.071 |
|
Week 6 |
Success |
150 |
127 |
|
Failure |
17 |
2 |
|
Success rate (%) |
89.8 |
98.4 |
|
p
|
0.003**
|
|
|
Week 12 |
Success |
136 |
126 |
|
Failure |
31 |
3 |
|
Success rate (%) |
81.4 |
97.7 |
|
p
|
< 0.001***
|
|
Week 24 |
Success |
101 |
117 |
|
Failure |
66 |
12 |
|
Success rate (%) |
60.5 |
90.7 |
|
p
|
< 0.001***
|
Table 4 presents the odds ratios (ORs) of multiple logistic regression tests at 3 time points (weeks 6, 12, and 24) to examine the relationship between the variables and success rates for smoking cessation. In week 4, no participant had failed to quit smoking among workers with an SWESC. Therefore, an error occurred in the logistic regression analysis calculation, so the result for week 4 was excluded. At week 6, SWESC (OR: 11.13; CI: 2.05–60.37) was significantly related to the success rate for smoking cessation. At week 12, SWESC (OR: 13.29; CI: 3.40–51.91), marital status (OR: 2.94; CI: 1.15–7.52), were significantly related to success rate for smoking cessation. At week 24, SWESC (OR: 9.95; CI: 4.31–22.97), marital status (OR: 2.97; CI: 1.36–6.52) were found to be significant variables. The variable with a significant relationship with the success rate for smoking cessation at 3 time points was having an SWESC.
Table 4 Association of characteristics of smoking cessation camp participants and smoking cessation at each time point
|
Variables |
Week 6 |
Week 12 |
Week 24 |
|
General characteristics |
|
|
|
|
Age (years) |
|
|
|
|
|
< 45 (ref.) |
1.00 |
1.00 |
1.00 |
|
|
45–64 |
0.91 (0.25–3.41) |
1.05 (0.39–2.86) |
1.97 (0.90–4.31) |
|
|
> 64 |
0.56 (0.06–4.97) |
1.53 (0.23–10.13) |
4.24 (0.87–20.62) |
|
Marital status |
|
|
|
|
|
With spouse |
2.81 (0.89–8.91) |
2.94 (1.15–7.52) |
2.97 (1.36–6.52) |
|
|
Without spouse (ref.) |
|
|
|
|
Household income (KRW/month) |
|
|
|
|
|
≥ 4,000,000 |
0.76 (0.53–2.867) |
0.72 (0.28–1.80) |
0.95 (0.49–1.88) |
|
|
< 4,000,000 (ref.) |
|
|
|
|
Education |
|
|
|
|
|
< High school (ref.) |
1.00 |
1.00 |
1.00 |
|
|
High school |
0.56 (0.04–7.67) |
0.44 (0.04–4.41) |
0.49 (0.08–2.83) |
|
|
≥ College |
1.31 (0.08–22.12) |
0.63 (0.06–7.15) |
0.73 (0.12–4.53) |
|
Health-related characteristics |
|
|
|
|
Alcohol drinking (last year) |
|
|
|
|
|
Yes |
0.67 (0.20–2.20) |
1.09 (0.45–2.63) |
0.99 (0.51–1.92) |
|
|
No (ref.) |
|
|
|
|
Exercise (last year) |
|
|
|
|
|
Yes |
1.26 (0.42–3.82) |
1.47 (0.62–3.49) |
1.16 (0.61–2.21) |
|
|
No (ref.) |
|
|
|
|
BMI (kg/m2) |
|
|
|
|
|
≥ 25 |
0.66 (0.22–2.03) |
1.41 (0.58–3.42) |
1.06 (0.56–2.03) |
|
|
< 25 (ref.) |
|
|
|
|
Morbidity |
|
|
|
|
|
Yes |
0.82 (0.27–2.48) |
0.82 (0.34–1.97) |
0.76 (0.39–1.46) |
|
|
No (ref.) |
|
|
|
|
Work-related characteristics |
|
|
|
|
SWESC |
|
|
|
|
|
Participants with an SWESC |
11.13 (2.05–60.37) |
13.29 (3.40–51.91) |
9.95 (4.31–22.97) |
|
|
Participants without an SWESC (ref.) |
|
|
|
|
Job |
|
|
|
|
|
White-collar (ref.) |
1.00 |
1.00 |
1.00 |
|
|
Service/Sales |
0.45 (0.05–3.75) |
0.64 (0.16–2.55) |
1.47 (0.49–4.42) |
|
|
Blue-collar |
0.40 (0.06–2.46) |
0.76 (0.23–2.48) |
0.85 (0.35–2.04) |
|
Camp-related characteristic |
|
|
|
|
Number of counseling sessions |
|
|
|
|
|
≥ 11 |
1.87 (0.60–5.84) |
1.52 (0.65–3.52) |
1.80 (0.95–3.41) |
|
|
< 11 (ref.) |
|
|
|
|
Smoking-related characteristics |
|
|
|
|
Cigarettes smoked per day |
|
|
|
|
|
≥ 20 |
1.41 (0.42–4.78) |
0.79 (0.29–2.16) |
0.87 (0.41–1.83) |
|
|
< 20 (ref.) |
|
|
|
|
Smoking initiation age (years) |
|
|
|
|
|
≥ 20 |
1.84 (0.63–5.41) |
1.77 (0.76–4.13) |
0.93 (0.49–1.74) |
|
|
< 20 (ref.) |
|
|
|
Table 5 presents the results of Cox regression analysis, adjusting confounding variables, to determine the success rate for smoking cessation over time and the effects of variables on it. Cox survival analysis was performed for a period of 24 weeks after the camp. In Model 1, the HR for SWESC was 4.83 (
p < 0.001; 95% CI: 2.61–8.93). In Model 2, the HR was 6.17 (
p < 0.001; 95% CI: 3.08–12.38). Marital status was found to be significant factors other than SWESC for smoking cessation in Model 2. The HR for the marital status was 2.10 (
p = 0.008; 95% CI: 1.21–3.63). In Model 3, which was adjusted for marital status, the HR for the workers with an SWESC was 4.55 (
p < 0.001; 95% CI: 2.45–8.42). The HR for marital status was 2.41 (
p < 0.001; 95% CI: 1.47–3.96).
Table 5 Cox proportional hazard regression analysis of SWESC and smoking cessation rate after 24 weeks of camp
|
Group |
HR of participants with an SWESC |
HR of participants without an SWESC (ref.) |
|
Model 1a
|
4.83 (2.61–8.93) |
1.00 |
|
Model 2b
|
6.17 (3.08–12.38) |
1.00 |
|
Model 3c
|
5.15 (2.74–9.67) |
1.00 |
DISCUSSION
Having an SWESC was significantly related to smoking cessation success at weeks 6, 12, and 24 in the logistic regression analysis. In addition, in the Cox survival analysis conducted with all variables adjusted, SWESC was found to be significantly related to the success rate for smoking cessation. Marital status was also variable with significant effects in the Cox analysis.
Previous studies investigated the success rate for smoking cessation can increase when there is support at the individual level. Van den Putte et al.
17 showed that the behaviors of supportive family or peer can be strong incentive for smoking cessation. In addition, some studies showed positive effects of financial incentives on the success rate for smoking cessation.
18,19 However, to the best of our knowledge, no study evaluated the association between non-financial supportive environment for smoking cessation at workplace and the success rate for smoking cessation.
The overall success rate of a professional treatment smoking cessation camps in Korea at week 24 was 61.2% in 2017. It was a superior rate than those of other smoking cessation methods, such as smoking cessation clinics at public health centers (34.4%) and phone counseling for smoking cessation (27.5%).
20 The success rate for smoking cessation camp in this study at week 24 was 73.6%, showing a higher success rate than the average of previous nationwide camps. Considering that most camp participants were heavy smokers who had difficulty ceasing smoking, smoking cessation camp can be considered as one of the most effective ways for smoking cessation.
The success rate for smoking cessation among workers with an SWESC at week 24 (90.7%) was significantly higher (p < 0.001) than that of workers without an SWESC (60.5%). Workers with an SWESC appear to maintained a high success rate over time, due to their company’s supportive environment and compensation motives.
Previous studies have shown a difference in the success rate for smoking cessation between men and women.
21 Women accounted for less than 10% of the camp participants during that period, and a small number of gender factors could confound the statistics. For this reason, only male participants were selected as the study subjects.
For marital status, a significant result was obtained at week 24 in the logistic regression analysis and the Cox survival analysis. The result that the presence of a spouse is related to smoking cessation is consistent with the study of Yeom et al.
22
Previous studies have shown that age,
23 education level,
22,24 drinking alcohol,
25 income,
26 morbidity,
27 daily smoking amount,
28 and smoking initiation age
29 are related to smoking cessation. However, these factors did not show sufficient relevance to smoking cessation in this study. Smoking cessation camp programs are intensive interventions, including psychotherapy and pharmacotherapy, so they appear to reduce the influence of other factors.
Among this study’s limitations were that the variables were investigated at the beginning of the camp, and changes of variables during the smoking cessation period (6 months) were not reflected in the analysis. To control the withdrawal symptoms of the participants and improve the smoking cessation rate, participants were recommended to take a medicine such as Varenicline. There was a lack of medication-related data before the camp, and there was no medication-related follow-up data after the camp, so it was excluded in the analysis. Participants in the smoking cessation camp are people who are already willing to quit smoking, and there is a limitation that it is difficult to generalize the results of this study to smokers who are less willing to quit smoking. It was not possible to determine what the ultra-long-term success rate for smoking cessation after week 24 would be, and additional research is required on this. In addition, among the methods taken to evaluate smoking cessation success, the results of the self-interview were not objective data. However, cessation status was evaluated at 4 points, up to week 24, and among 218 participants assessed as having successfully quit smoking at week 24, 188 (86.2%) were tested through objective measurement. Among workers with an SWESC, only those who succeeded in quitting smoking through objective measurement could receive compensation from their workplace, so the possible distortion of results due to self-report is limited.
Among the strengths of this study is that it analyzed data collected over 5 years in the integrated information system of the Ministry of Health and Welfare. As noted, this study is significant in that it is, to the best of our knowledge, the first analysis to identify the quantitative effect for non-financial compensation and supportive environment at the workplace level on the success rate for smoking cessation. Smoking cessation projects for the future can improve their cost-efficiency by effectively increasing the success rate for smoking cessation while consuming lower amount of financial cost in connection with the workplace. In addition, previous studies have been conducted to measure the success rate for smoking cessation for workers at small and medium-sized workplaces.
30 But it is difficult to find studies other than this study that focus on smoking cessation among employees of large-sized company. The survival analysis used, in addition to the advantage of adjusting the effects of variables for the smoking cessation success, had the advantage of reflecting the passage of time, showing a higher causal relationship.
A supportive workplace environment for workers’ health can contribute to improvement of workers’ health.
31,32 The result of this study shows a specific example of this. Since the supportive workplace environment has been shown to be effective even in smoking cessation, which is not easy to succeed, supportive workplace environment is expected to be an important factor in the success of not only smoking cessation but also other health projects in workplace, and additional research is required on this. In addition, most workers with an SWESC in this study were blue-collar workers (94.6%), and blue-collar workers are known to be exposed to a higher smoking risk than office workers.
33,34 This study suggests that the smoking cessation policy at the workplace level is effective for the smoking cessation of blue-collar workers in the blind spot of smoking.
Smokers take more sick leaves compared to the non-smokers, and the cost of their health care is 50% higher than that of non-smokers; these factors reduce corporate competitiveness.
35 The results of this study can be used as a reference for designing better workplace-based smoking cessation policies designed in relation to the government’s smoking cessation projects, to improve workers’ health and productivity. It is necessary to actively inform the health policy makers that SWESC is an effective factor in workers’ success for smoking cessation. Larger portion of the smoking cessation project budget should be allocated to strengthening SWESC in conjunction with the Ministry of Health and Welfare and the Ministry of Employment and Labor. Similar to the compensatory policy mentioned in this study, a higher success rate for smoking cessation is expected by developing and implementing other smoking cessation policies at workplace, which is attractive to workers who try to quit smoking.
CONCLUSIONS
Among the participants at a professional treatment smoking cessation camp, those with an SWESC showed a significantly higher success rate for smoking cessation. A supportive workplace environment for worker’s health should be evaluated as an important factor for the success of future smoking cessation and other health projects in workplace.
Acknowledgements
The authors thank Ms. Heejung Lee, from Ulsan Regional Smoking Cessation Center, for her informational assistance for this study.
Abbreviations
supportive workplace environment for smoking cessation
NOTES
-
Funding: This study was supported by Health Promotion Fund, Ministry of Health & Welfare, Republic of Korea (RTCC2021FH004).
-
Competing interests: The authors declare that they have no competing interests.
-
Authors contributions:
Conceptualization: Yoo C.
Data curation: Kim W.
Formal analysis: Kim W, Kim D, Yoo C.
Investigation: Kim W.
Methodology: Kim W, Ock M, Yoo C.
Visualization: Kim W.
Writing - original draft: Kim W.
Writing - review & editing: Jeon YJ, Ock M, Lee H, Kim AR, Kim M, Yoo C.
REFERENCES
REFERENCES
- 1. Lee EH, Park SK, Ko KP, Cho IS, Chang SH, Shin HR, et al. Cigarette smoking and mortality in the Korean Multi-center Cancer Cohort (KMCC) study. J Prev Med Public Health 2010;43(2):151–158. 20383048.ArticlePubMed
- 2. Cahn Z, Drope J, Hamill S, Islami F, Liber A, Nargis N, et al. The Tobacco Atlas: Sixth Edition. Atlanta, GA, USA: American Cancer Society and Vital Strategies; 2018.
- 3. Cummings KM. Health policy and smoking and tobacco use. In: Gochman DS, editor. Handbook of Health Behavior Research IV: Relevance for Professionals and Issues for the Future. Boston, MA, USA: Springer US; 1997, 231–232.
- 4. GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet 2021;397(10292):2337–2360. 34051883.PubMedPMC
- 5. Centers for Disease Control and Prevention (CDC). Cigarette smoking among adults--United States, 2007. MMWR Morb Mortal Wkly Rep 2008;57(45):1221–1226. 19008790.PubMed
- 6. Samet JM. Health benefits of smoking cessation. Clin Chest Med 1991;12(4):669–679. 1747986.ArticlePubMed
- 7. Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years’ observations on male British doctors. BMJ 2004;328(7455):1519. 15213107.ArticlePubMedPMC
- 8. Taylor GM, Lindson N, Farley A, Leinberger-Jabari A, Sawyer K, Te Water Naudé R, et al. Smoking cessation for improving mental health. Cochrane Database Syst Rev 2021;3(3):CD013522. 33687070.ArticlePubMedPMC
- 9. Organisation for Economic Co-operation and Development (OECD). Health at a Glance 2019: OECD Indicators. Paris, France: OECD Publishing; 2019.
- 10. Korea Disease Control and Prevention Agency. Korea National Health and Nutrition Examination Survey: current smoking rate trend, 1998–2019. Updated 2023]. Accessed April 1, 2023].
https://kosis.kr/statHtml/statHtml.do?orgId=177&tblId=DT_11702_N001&conn_path=I2
.
- 11. van den Brand FA, Nagtzaam P, Nagelhout GE, Winkens B, van Schayck CP. The association of peer smoking behavior and social support with quit success in employees who participated in a smoking cessation intervention at the workplace. Int J Environ Res Public Health 2019;16(16):2831. 31398854.ArticlePubMedPMC
- 12. Lee KH, Chung YC, Kim KH. Success factors of smoking cessation among new enrollees and re-enrollees in smoking cessation clinics at public health centers. J Digital Convergence 2014;12(1):445–455.Article
- 13. Smith KB, Smith MS. Obesity statistics. Prim Care 2016;43(1):121–135. 26896205.Article
- 14. Statistics Korea. 7th Korean Standard Occupational Classification. Updated 2018]. Accessed April 1, 2023].
http://kssc.kostat.go.kr/ksscNew_web/kssc/common/ClassificationContent.do?gubun=1&strCategoryNameCode=002&categoryMenu=007&addGubun=no
.
- 15. Kang YH, Lee YJ, Kong SY, Lee DH, Yun YH. Usefulness of urinary cotinine test to discriminate between smokers and nonsmokers in Korean adolescents. Korean J Lab Med 2004;24(3):155–159.
- 16. Park SS, Lee JY, Cho SI. Validity of expired carbon monoxide and urine cotinine using dipstick method to assess smoking status. J Prev Med Public Health 2007;40(4):297–304. 17693733.ArticlePubMed
- 17. van den Putte B, Yzer MC, Brunsting S. Social influences on smoking cessation: a comparison of the effect of six social influence variables. Prev Med 2005;41(1):186–193. 15917010.ArticlePubMed
- 18. Notley C, Gentry S, Livingstone-Banks J, Bauld L, Perera R, Hartmann-Boyce J. Incentives for smoking cessation. Cochrane Database Syst Rev 2019;7(7):CD004307. 31313293.
- 19. van den Brand FA, Nagelhout GE, Winkens B, Chavannes NH, van Schayck OC. Effect of a workplace-based group training programme combined with financial incentives on smoking cessation: a cluster-randomised controlled trial. Lancet Public Health 2018;3(11):e536–e544. 30342875.ArticlePubMed
- 20. Lim MK, Kim YH, Kim HS, Baek YJ, Oh JK, Park JJ, et al. Evaluation of the Result of the Smoking Cessation Support Project and Plans for Operational Advancement. Goyang, Korea: National Cancer Center; 2019.
- 21. Kim B. Workplace smoking ban policy and smoking behavior. J Prev Med Public Health 2009;42(5):293–297. 19806001.ArticlePubMed
- 22. Yeom H, Lim HS, Min J, Lee S, Park YH. Factors affecting smoking cessation success of heavy smokers registered in the intensive care smoking cessation camp (data from the National Tobacco Control Center). Osong Public Health Res Perspect 2018;9(5):240–247. 30402379.ArticlePubMedPMCPDF
- 23. Ha MW, Lee DH. Predictors of quitting smoking-results of smoking cessation campaign in workplace of a steel manufacturing industry-. Korean J Occup Environ Med 2000;12(2):170–178.ArticlePDF
- 24. Zhuang YL, Gamst AC, Cummins SE, Wolfson T, Zhu SH. Comparison of smoking cessation between education groups: findings from 2 US National Surveys over 2 decades. Am J Public Health 2015;105(2):373–379. 25521868.ArticlePubMedPMC
- 25. Lynch KL, Twesten JE, Stern A, Augustson EM. Level of alcohol consumption and successful smoking cessation. Nicotine Tob Res 2019;21(8):1058–1064. 29986105.ArticlePubMedPMC
- 26. Smith CE, Hill SE, Amos A. Impact of population tobacco control interventions on socioeconomic inequalities in smoking: a systematic review and appraisal of future research directions. Tob Control 2020;30:e87–e95. 32994297.ArticlePubMedPMC
- 27. Lindsay HG, Wamboldt FS, Holm KE, Make BJ, Hokanson J, Crapo JD, et al. Impact of a medical diagnosis on decision to stop smoking and successful smoking cessation. Chronic Obstr Pulm Dis 2021;8(3):360–370. 34010545.ArticlePubMedPMC
- 28. Lee ES, Seo HG. The factors associated with successful smoking cessation in Korea. J Korean Acad of Fam Med 2007;28(1):39–44.
- 29. Khuder SA, Dayal HH, Mutgi AB. Age at smoking onset and its effect on smoking cessation. Addict Behav 1999;24(5):673–677. 10574304.ArticlePubMed
- 30. Ryu IH, Park KS. Successful factors of smoking cessation for male workers from small and medium enterprises registered with local tobacco control center. J Agric Med Community Health 2021;46(4):253–265.
- 31. Goetzel RZ, Henke RM, Tabrizi M, Pelletier KR, Loeppke R, Ballard DW, et al. Do workplace health promotion (wellness) programs work? J Occup Environ Med 2014;56(9):927–934. 25153303.PubMed
- 32. O’Donnel MP. Health Promotion in the Workplace. 5th ed. Littleton, CO, USA: Art & Science of Health Promotion Institute; 2017.
- 33. Ham DC, Przybeck T, Strickland JR, Luke DA, Bierut LJ, Evanoff BA. Occupation and workplace policies predict smoking behaviors: analysis of national data from the current population survey. J Occup Environ Med 2011;53(11):1337–1345. 21988795.PubMedPMC
- 34. Albertsen K, Hannerz H, Borg V, Burr H. Work environment and smoking cessation over a five-year period. Scand J Public Health 2004;32(3):164–171. 15204176.ArticlePubMedPDF
- 35. Jang TW, Kim HR, Choi SE, Yim HW, Lee HE, Myong JP, et al. Smoking rate trends in Korean occupational groups: analysis of KNHANES 1998-2009 data. J Occup Health 2012;54(6):452–458. 23060030.ArticlePubMedPDF
 , A Ram Kim1
, A Ram Kim1 , Minsu Ock3
, Minsu Ock3 , Young-Jee Jeon4
, Young-Jee Jeon4 , Heun Lee1
, Heun Lee1 , Daehwan Kim5
, Daehwan Kim5 , Minjun Kim1
, Minjun Kim1 , Cheolin Yoo1,2
, Cheolin Yoo1,2

 KSOEM
KSOEM

 Cite
Cite

