Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 34; 2022 > Article
- Original Article Poor worker’s long working hours paradox: evidence from the Korea National Health and Nutrition Examination Survey, 2013-2018
-
Min Young Park1
 , Jaeyoung Park1
, Jaeyoung Park1 , Jun-Pyo Myong1
, Jun-Pyo Myong1 , Hyoung-Ryoul Kim1
, Hyoung-Ryoul Kim1 , Dong-Wook Lee2
, Dong-Wook Lee2 , Mo-Yeol Kang1
, Mo-Yeol Kang1
-
Annals of Occupational and Environmental Medicine 2022;34:e2.
DOI: https://doi.org/10.35371/aoem.2022.34.e2
Published online: February 14, 2022
1Department of Occupational and Environmental Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
2Public Health Center, Seoul National University Hospital, Seoul, Korea.
- Correspondence: Mo-Yeol Kang. Department of Occupational and Environmental Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, 222 Banpo-daero, Seocho-gu, Seoul 06591, Korea. snaptoon@naver.com
Copyright © 2022 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background Because income and working hours are closely related, the health impact of working hours can vary according to economic status. This study aimed to investigate the relationship between working hours and the risk of poor self-rated health according to household income level.
-
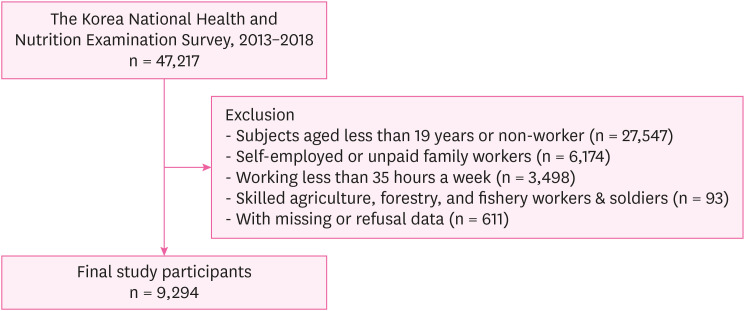
Methods We used the data from the Korea National Health and Nutrition Examination Survey VI and VII. The information on working hours and self-rated health was obtained from the questionnaire. After stratifying by household income level, the risk of poor self-rated health for long working hour group (≥ 52 hours a week), compared to the 35–51 working hour group as a reference, were calculated using multiple logistic regression.
-
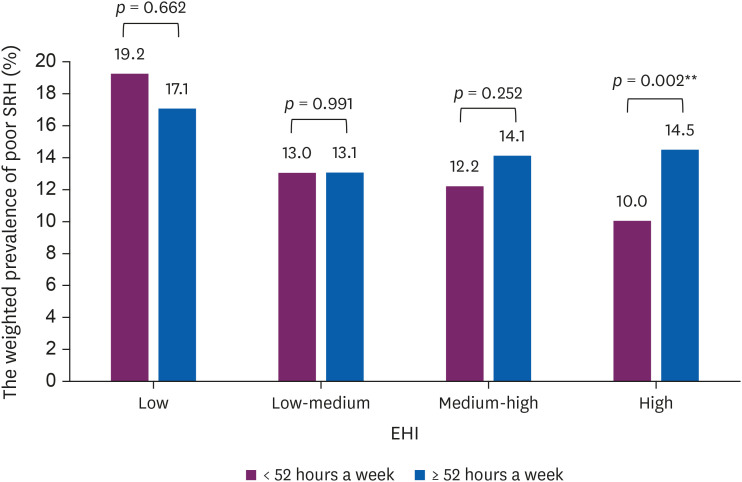
Results Long working hours increased the risk of poor self-rated health in the group with the highest income, but not in the group with the lowest income. On the other hand, the overall weighted prevalence of poor self-rated health was higher in the low-income group.
-
Conclusions The relationship between long working hours and the risk of poor self-rated health varied by household income level. This phenomenon, in which the health effects of long working hours appear to diminish in low-income households can be referred to as the ‘poor worker’s long working hours paradox’. Our findings suggest that the recent working hour restriction policy implemented by the Korean government should be promoted, together with a basic wage preservation to improve workers’ general health and well-being.
BACKGROUND
METHODS
RESULTS
Characteristics of the study participants (n = 9,294)
Self-rated health according to characteristics of the study participants
The odds ratio of poor self-rated health by long working hours stratified by equivalised household incomea
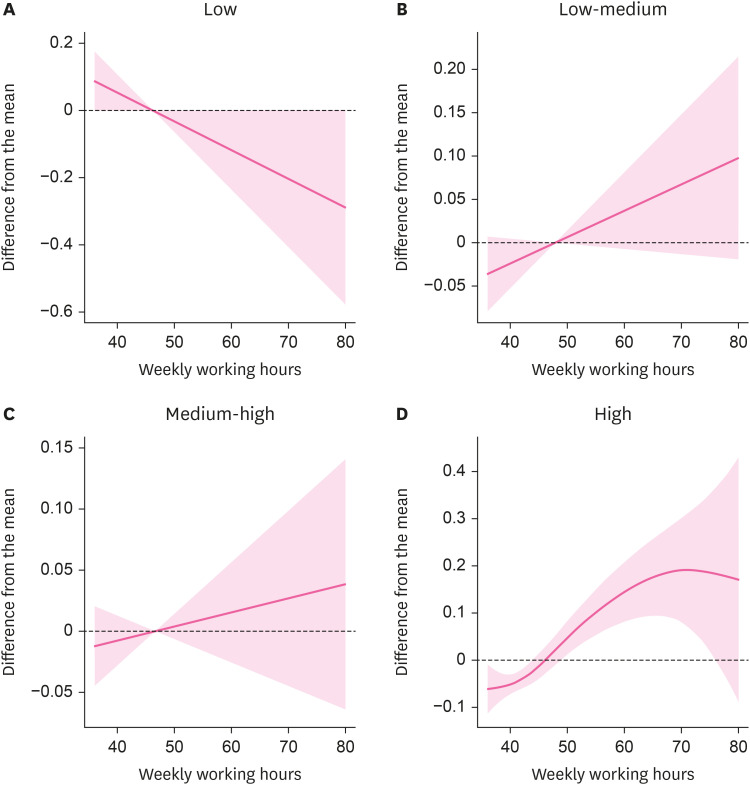
Nonparametric association between weekly working hours and poor self-rated health score in each group of EHI. (A) Low EHI. (B) Low-medium EHI. (C) Medium-high EHI. (D) High EHI.
The weighted prevalence of poor SRH by working hours and EHI.
DISCUSSION
CONCLUSIONS
ACKNOWLEDGMENTS
Abbreviations
CI
EHI
KNHANES
OECD
OR
SRH
STROBE
-
Competing interests: The authors declare that they have no competing interest.
-
Author Contributions:
NOTES
- 1. Organization for Economic Cooperation and Development (OECD). Hours worked (indicator). Paris, France: OECD; 2021.
- 2. Bannai A, Tamakoshi A. The association between long working hours and health: a systematic review of epidemiological evidence. Scand J Work Environ Health 2014;40(1):5–18. 24100465.ArticlePubMed
- 3. Amagasa T, Nakayama T. Relationship between long working hours and depression in two working populations: a structural equation model approach. J Occup Environ Med 2012;54(7):868–874. 22547121.PubMed
- 4. Virtanen M, Jokela M, Nyberg ST, Madsen IE, Lallukka T, Ahola K, et al. Long working hours and alcohol use: systematic review and meta-analysis of published studies and unpublished individual participant data. BMJ 2015;350:g7772. 25587065.ArticlePubMedPMC
- 5. Kobayashi T, Suzuki E, Takao S, Doi H. Long working hours and metabolic syndrome among Japanese men: a cross-sectional study. BMC Public Health 2012;12(1):395. 22651100.ArticlePubMedPMCPDF
- 6. Kang MY, Park H, Seo JC, Kim D, Lim YH, Lim S, et al. Long working hours and cardiovascular disease: a meta-analysis of epidemiologic studies. J Occup Environ Med 2012;54(5):532–537. 22576460.PubMed
- 7. Lee DW, Hong YC, Min KB, Kim TS, Kim MS, Kang MY. The effect of long working hours on 10-year risk of coronary heart disease and stroke in the Korean population: the Korea National Health and Nutrition Examination Survey (KNHANES), 2007 to 2013. Ann Occup Environ Med 2016;28(1):64. 27891238.ArticlePubMedPMCPDF
- 8. Dembe AE, Erickson JB, Delbos RG, Banks SM. The impact of overtime and long work hours on occupational injuries and illnesses: new evidence from the United States. Occup Environ Med 2005;62(9):588–597. 16109814.ArticlePubMedPMC
- 9. McConnell C, Brue S, Macpherson D. Contemporary Labor Economics. 11th ed. New York, NY, USA: McGraw Hill Education; 2016.
- 10. Wilkinson RG, Pickett KE. Income inequality and population health: a review and explanation of the evidence. Soc Sci Med 2006;62(7):1768–1784. 16226363.ArticlePubMed
- 11. Wagstaff A, van Doorslaer E. Income inequality and health: what does the literature tell us? Annu Rev Public Health 2000;21(1):543–567. 10884964.ArticlePubMed
- 12. Pickett KE, Wilkinson RG. Income inequality and health: a causal review. Soc Sci Med 2015;128:316–326. 25577953.ArticlePubMed
- 13. Lee DW, Kim HR, Myong JP, Choi J, Hong YC, Kang MY. Does working long hours increase the risk of cardiovascular disease for everyone? J Occup Health 2019;61(6):431–441. 31237053.ArticlePubMedPMCPDF
- 14. Manor O, Matthews S, Power C. Self-rated health and limiting longstanding illness: inter-relationships with morbidity in early adulthood. Int J Epidemiol 2001;30(3):600–607. 11416091.ArticlePubMed
- 15. Kim SH, Wolde-Tsadik G, Reuben DB. Predictors of perceived health in hospitalized older persons: a cross-sectional and longitudinal study. J Am Geriatr Soc 1997;45(4):420–426. 9100709.ArticlePubMed
- 16. Benyamini Y, Idler EL, Leventhal H, Leventhal EA. Positive affect and function as influences on self-assessments of health: expanding our view beyond illness and disability. J Gerontol B Psychol Sci Soc Sci 2000;55(2):107–116.Article
- 17. Palladino R, Tayu Lee J, Ashworth M, Triassi M, Millett C. Associations between multimorbidity, healthcare utilisation and health status: evidence from 16 European countries. Age Ageing 2016;45(3):431–435. 27013499.ArticlePubMedPMC
- 18. Ryu J, Yoon Y, Kim H, Kang CW, Jung-Choi K. The change of self-rated health according to working hours for two years by gender. Int J Environ Res Public Health 2018;15(9):1984.ArticlePubMedPMC
- 19. Song JT, Lee G, Kwon J, Park JW, Choi H, Lim S. The association between long working hours and self-rated health. Ann Occup Environ Med 2014;26(1):2. 24472333.ArticlePubMedPMCPDF
- 20. Jeon J, Lee W, Choi WJ, Ham S, Kang SK. Association between Working Hours and Self-Rated Health. Int J Environ Res Public Health 2020;17(8):2736.ArticlePubMedPMC
- 21. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ 2007;85(11):867–872. 18038077.ArticlePubMedPMC
- 22. Ministry of Employment and Labor. Chapter IV. Working hours and recess. Labor Standards Act. Sejong, Korea: Ministry of Employment and Labor; 2021.
- 23. Korea Workers’ Compensation & Welfare Services. The Manual of Occupational Disease Adjudication. Ulsan, Korea: Korea Workers’ Compensation & Welfare Services; 2019.
- 24. Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med 2009;69(3):307–316. 19520474.ArticlePubMed
- 25. Wu S, Wang R, Zhao Y, Ma X, Wu M, Yan X, et al. The relationship between self-rated health and objective health status: a population-based study. BMC Public Health 2013;13(1):320. 23570559.ArticlePubMedPMCPDF
- 26. Lorem G, Cook S, Leon DA, Emaus N, Schirmer H. Self-reported health as a predictor of mortality: a cohort study of its relation to other health measurements and observation time. Sci Rep 2020;10(1):4886. 32184429.ArticlePubMedPMCPDF
- 27. Organization for Economic Cooperation and Development (OECD). Divided We Stand: Why Inequality Keeps Rising. Paris, France: OECD Publishing Paris; 2011.
- 28. Lee W, Yeom H, Yoon JH, Won JU, Jung PK, Lee JH, et al. Metabolic outcomes of workers according to the International Standard Classification of Occupations in Korea. Am J Ind Med 2016;59(8):685–694. 27345305.ArticlePubMed
- 29. Geurts SA, Sonnentag S. Recovery as an explanatory mechanism in the relation between acute stress reactions and chronic health impairment. Scand J Work Environ Health 2006;32(6):482–492. 17173204.ArticlePubMed
- 30. Spurgeon A, Harrington JM, Cooper CL. Health and safety problems associated with long working hours: a review of the current position. Occup Environ Med 1997;54(6):367–375. 9245942.ArticlePubMedPMC
- 31. Altonji JG, Paxson CH. Labor supply preferences, hours constraints, and hours-wage trade-offs. J Labor Econ 1988;6(2):254–276.Article
- 32. Stier H, Lewin-Epstein N. Time to work: a comparative analysis of preferences for working hours. Work Occup 2003;30(3):302–326.
- 33. Lu L. Working hours and personal preference among Taiwanese employees. Int J Workplace Health Manag 2011;4(3):244–256.Article
- 34. Lee Y. Analysis of the relationship between working hour mismatch and worker’s health. Health Soc Welf Rev 2015;35(3):135–165.Article
- 35. Smith PM, Glazier RH, Sibley LM. The predictors of self-rated health and the relationship between self-rated health and health service needs are similar across socioeconomic groups in Canada. J Clin Epidemiol 2010;63(4):412–421. 19926448.ArticlePubMed
- 36. Kennedy BP, Kawachi I, Glass R, Prothrow-Stith D. Income distribution, socioeconomic status, and self rated health in the United States: multilevel analysis. BMJ 1998;317(7163):917–921. 9756809.ArticlePubMedPMC
- 37. Weich S, Lewis G, Jenkins SP. Income inequality and self rated health in Britain. J Epidemiol Community Health 2002;56(6):436–441. 12011200.ArticlePubMedPMC
- 38. Yoon BJ. Differential effects on self-rated health by socioeconomic class. J Health Inf Stat 2016;41(1):35–42.ArticlePDF
- 39. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Viera A, Crotty K, et al. Health literacy interventions and outcomes: an updated systematic review. Evid Rep Technol Assess (Full Rep) 2011;(199):1–941.
- 40. Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health 2012;12(1):80. 22276600.PubMedPMC
- 41. Ratzan S, Parker R, Selden C, Zorn M. National Library of Medicine Current Bibliographies in Medicine: Health Literacy. Bethesda, MD, USA: National Institutes of Health, US Department of Health and Human Services; 2000.
- 42. Sørensen K, Brand H. Health literacy lost in translations? Introducing the European Health Literacy Glossary. Health Promot Int 2014;29(4):634–644. 23479322.ArticlePubMed
- 43. Furuya Y, Kondo N, Yamagata Z, Hashimoto H. Health literacy, socioeconomic status and self-rated health in Japan. Health Promot Int 2015;30(3):505–513. 24131729.ArticlePubMed
- 44. Park MY, Lee J, Kim HR, Lee YM, Ahn J, Lee DW, et al. Long working hours and risk of depression by household income level: findings from the Korea National Health and Nutrition Examination Survey (KNHANES). J Occup Environ Med 2022;64(2):99–104. 34723909.PubMed
- 45. Pennycook M. What Price a Living Wage?: Understanding the Impact of a Living Wage on Firm-level Wage Bills. London, UK: Institute for Public Policy Research; 2012.
- 46. Seoul confirms living wage of 10,702 KRWO per hour next year, 1.7% hourly wage increase. Updated September 17, 2020]. Accessed November 4, 2021]. https://news.seoul.go.kr/economy/archives/509472 .
- 47. Choi YH. Is subjective health reliable as a proxy variable for true health? A comparison of self-rated health and self-assessed change in health among middle-aged and older South Koreans. Health Soc Welf Rev 2016;36(4):431–459.Article
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Association between working hours, income, and work-related injury among freelancers in Japan: a cross-sectional study
Kazuhiro Watanabe, Kazuhito Yokoyama, Akizumi Tsutsumi
Journal of Occupational Health.2025;[Epub] CrossRef - Paradox of long working hours: how income levels and satisfaction modify health outcomes
Jeehee MIN, Min-Seok KIM, Dong-Wook LEE, Seong-Sik CHO, Mo-Yeol KANG
Industrial Health.2025; 63(5): 443. CrossRef - Effect of long working hours on psychological distress among young workers in different types of occupation
Seong-Uk Baek, Jin-Ha Yoon
Preventive Medicine.2024; 179: 107829. CrossRef - High levels of anxiety and depression in women farmers from Ecuador: A cross-section study in Coastal and Highlands regions
Aline Siteneski, Viviana Septimia Gómez Mieles, Paola Andrea Romero Riaño, Karime Montes Escobar, German Josuet Lapo-Talledo, Andrea Valeria Dueñas-Rodriguez, María Antonieta Palma Cedeño, Yliana Consuelo Villacis Lascano, Lincon Oliver Echeverria Zurita
International Journal of Social Psychiatry.2024; 70(6): 1138. CrossRef - Association between single-person household wage workers in South Korea and insomnia symptoms: the 6th Korean Working Conditions Survey (KWCS)
Yoon Ho Lee, Yong-Jin Lee, Eun-Chul Jang, Young-Sun Min, Soon-Chan Kwon
Ann Occup Environ Med.2024; 36: e25. CrossRef - Multi-Dimensional Comparison of the Impact Mechanism of the Self-Rated Health Status of Urban and Rural Residents in Chinese Social Environments
Chao Yu, Xinyi Zhang, Junbo Gao
International Journal of Environmental Research and Public Health.2022; 19(17): 10625. CrossRef
- Figure
- Related articles
-
- Relationship between long-term PM2.5 exposure and myopia prevalence in adults: analysis of the Korea National Health and Nutrition Examination Survey–Air Pollution Linked Data, 2020
- Exploring the impact of age and socioeconomic factors on health-related unemployment using propensity score matching: results from Korea National Health and Nutrition Examination Survey (2015–2017)
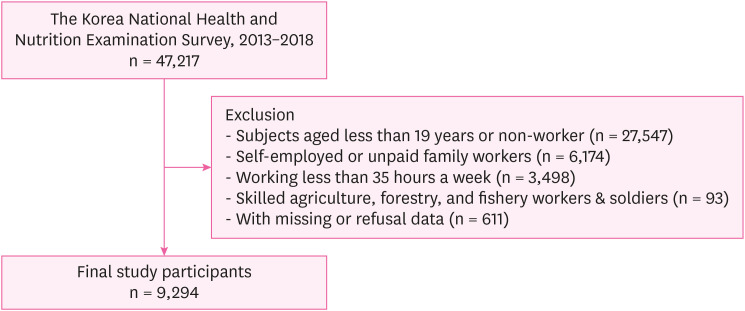
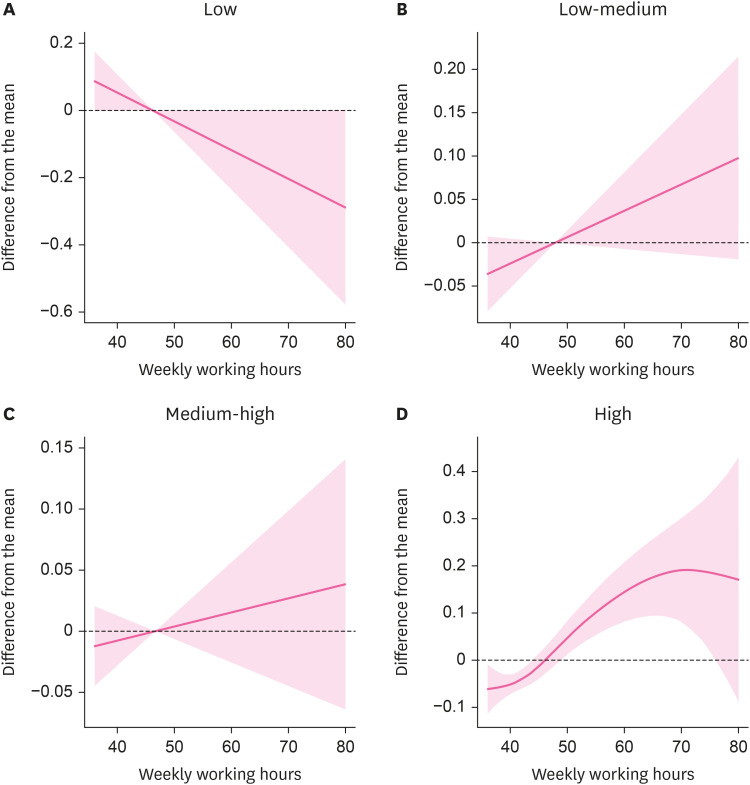
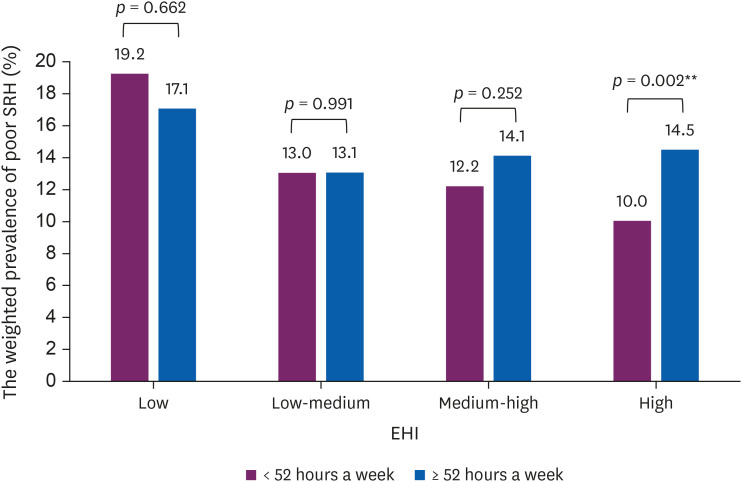
Fig. 1
Fig. 2
Fig. 3
| Characteristics | Long working hours | Total | |||
|---|---|---|---|---|---|
| Yes (≥ 52 hours/week) | No (35–51 hours/week) | ||||
| No. (%) | No. (%) | ||||
| Total | 2,160 (23.8) | 7,134 (76.2) | 9,294 | ||
| Age (years) | < 0.001 | ||||
| 19–39 | 778 (22.0) | 3,029 (78.0) | 3,807 | ||
| 40–54 | 822 (24.6) | 2,739 (75.4) | 3,561 | ||
| 55–64 | 377 (25.4) | 1,099 (74.6) | 1,476 | ||
| ≥ 65 | 183 (38.4) | 267 (61.6) | 450 | ||
| Sex | < 0.001 | ||||
| Male | 1,527 (28.7) | 3,752 (71.3) | 5,279 | ||
| Female | 633 (15.2) | 3,382 (84.8) | 4,015 | ||
| Marital status | < 0.001 | ||||
| Married | 1,571 (24.9) | 4,996 (75.1) | 6,567 | ||
| Unmarried | 395 (20.6) | 1,651 (79.4) | 2,046 | ||
| Othersa | 194 (26.5) | 487 (73.5) | 681 | ||
| Education | < 0.001 | ||||
| Elementary | 245 (37.7) | 418 (62.3) | 663 | ||
| Middle | 254 (39.2) | 413 (60.8) | 667 | ||
| High | 799 (26.8) | 2,268 (73.2) | 3,067 | ||
| ≥ College | 862 (19.0) | 4,035 (81.0) | 4,897 | ||
| Equivalised household incomeb | < 0.001 | ||||
| Low | 111 (25.3) | 322 (74.7) | 433 | ||
| Low-medium | 609 (31.0) | 1,362 (69.0) | 1,971 | ||
| Medium-high | 768 (24.5) | 2,410 (75.5) | 3,178 | ||
| High | 672 (19.4) | 3,040 (80.6) | 3,712 | ||
| Occupation | < 0.001 | ||||
| White collar | 697 (15.3) | 4,201 (84.7) | 4,898 | ||
| Pink collar | 425 (30.0) | 938 (70.0) | 1,363 | ||
| Blue collar | 1,038 (35.4) | 1,995 (64.6) | 3,033 | ||
| Employment status | < 0.001 | ||||
| Permanent | 1,678 (22.7) | 6,007 (77.3) | 7,685 | ||
| Precarious | 482 (29.6) | 1,127 (70.4) | 1,609 | ||
| Self-rated health | |||||
| Good | 1,846 (23.3) | 6,298 (76.7) | 8,144 | ||
| Poor | 314 (27.3) | 836 (72.7) | 1,150 | ||
| Work schedule | < 0.001 | ||||
| Day time | 1,678 (22.1) | 6,299 (77.9) | 7,977 | ||
| Shift workc | 482 (33.8) | 835 (66.2) | 1,317 | ||
| Smoking | < 0.001 | ||||
| No | 918 (18.4) | 4,126 (81.6) | 5,044 | ||
| Current | 757 (32.2) | 1,643 (67.8) | 2,400 | ||
| Past | 485 (25.2) | 1,365 (74.8) | 1,850 | ||
| Problematic drinking | 0.002 | ||||
| Yes | 394 (27.5) | 1,012 (72.5) | 1,406 | ||
| No | 1,766 (23.1) | 6,122 (76.9) | 7,888 | ||
| Hypertension | < 0.001 | ||||
| Yes | 571 (28.2) | 1,434 (71.8) | 2,005 | ||
| No | 1,589 (22.7) | 5,700 (77.3) | 7,289 | ||
| Diabetes Mellitus | 0.002 | ||||
| Yes | 201 (29.6) | 446 (70.4) | 647 | ||
| No | 1,959 (23.5) | 6,688 (76.5) | 8,647 | ||
| Depression | 0.502 | ||||
| Yes | 15 (28.1) | 43 (71.9) | 58 | ||
| No | 2,145 (23.8) | 7,091 (76.2) | 9,236 | ||
| Characteristics | Self-rated health | Total | |||
|---|---|---|---|---|---|
| Poor | Good | ||||
| No. (%) | No. (%) | ||||
| Total | 1,150 (12.3) | 8,144 (87.7) | 9,294 | ||
| Age | 0.322 | ||||
| 19–39 | 447 (12.2) | 3,360 (87.8) | 3,807 | ||
| 40–54 | 426 (11.9) | 3,135 (88.1) | 3,561 | ||
| 55–64 | 204 (13.3) | 1,272 (86.7) | 1,476 | ||
| ≥ 65 | 73 (15.2) | 377 (84.8) | 450 | ||
| Sex | < 0.001 | ||||
| Male | 556 (11.1) | 4,723 (88.9) | 5,279 | ||
| Female | 594 (14.4) | 3,421 (85.6) | 4,015 | ||
| Marital status | < 0.001 | ||||
| Married | 739 (11.0) | 5,828 (89.0) | 6,567 | ||
| Unmarried | 273 (13.7) | 1,773 (86.3) | 2,046 | ||
| Othersa | 138 (20.1) | 543 (79.9) | 681 | ||
| Education | < 0.001 | ||||
| Elementary | 137 (19.5) | 526 (80.5) | 663 | ||
| Middle | 115 (17.7) | 552 (82.3) | 667 | ||
| High | 408 (13.7) | 2,659 (86.3) | 3,067 | ||
| ≥ College | 490 (10.2) | 4,407 (89.8) | 4,897 | ||
| Equivalised household incomeb | < 0.001 | ||||
| Low | 85 (18.7) | 348 (81.3) | 433 | ||
| Low-medium | 275 (13.1) | 1,696 (86.9) | 1,971 | ||
| Medium-high | 393 (12.7) | 2,785 (87.3) | 3,178 | ||
| High | 397 (10.9) | 3,315 (89.1) | 3,712 | ||
| Occupation | 0.017 | ||||
| White collar | 527 (11.3) | 4,371 (88.7) | 4,898 | ||
| Pink collar | 202 (14.1) | 1,161 (85.9) | 1,363 | ||
| Blue collar | 421 (13.2) | 2,612 (86.8) | 3,033 | ||
| Employment status | < 0.001 | ||||
| Permanent | 866 (11.3) | 6,819 (88.7) | 7,685 | ||
| Precarious | 284 (17.2) | 1,325 (82.8) | 1,609 | ||
| Weekly working hour | 0.011 | ||||
| 35–51 | 836 (11.7) | 6,298 (88.3) | 7,134 | ||
| ≥ 52 | 314 (14.1) | 1,846 (85.9) | 2,160 | ||
| Work schedule | 0.138 | ||||
| Day time | 968 (12.1) | 7,009 (87.9) | 7,977 | ||
| Shift workc | 182 (13.7) | 1,135 (86.3) | 1,317 | ||
| Smoking | < 0.001 | ||||
| No | 605 (11.3) | 4,439 (88.7) | 5,044 | ||
| Current | 355 (15.9) | 2,045 (84.1) | 2,400 | ||
| Past | 190 (9.5) | 1,660 (90.5) | 1,850 | ||
| Problematic drinking | 0.007 | ||||
| Yes | 193 (14.9) | 1,213 (85.1) | 1,406 | ||
| No | 957 (11.8) | 6,931 (88.2) | 7,888 | ||
| Hypertension | < 0.001 | ||||
| Yes | 323 (16.3) | 1,682 (83.7) | 2,005 | ||
| No | 827 (11.3) | 6,462 (88.7) | 7,289 | ||
| Diabetes Mellitus | < 0.001 | ||||
| Yes | 154 (23.4) | 493 (76.6) | 647 | ||
| No | 996 (11.6) | 7,651 (23.4) | 8,647 | ||
| Depression | < 0.001 | ||||
| Yes | 25 (40.8) | 33 (59.2) | 58 | ||
| No | 1,125 (12.1) | 8,111 (87.9) | 9,236 | ||
| Equivalised household income | Weighted prevalence of poor self-rated health (%) | Crude ORb | Model 1c | Model 2d | Model 3e | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| < 52 hours a week | ≥ 52 hours a week | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | ||
| Overall | 11.7 | 14.1 | 1.24 | 1.05–1.45 | 1.30 | 1.09–1.54 | 1.22 | 1.017–1.458 | 1.17 | 0.98–1.41 | |
| Subgroups for income | |||||||||||
| Low | 19.2 | 17.1 | 0.86 | 0.44–1.70 | 0.96 | 0.46–1.99 | 0.88 | 0.410–1.896 | 0.88 | 0.41–1.87 | |
| Low-medium | 13.0 | 13.1 | 1.00 | 0.73–1.37 | 1.09 | 0.79–1.50 | 1.05 | 0.753–1.465 | 0.97 | 0.69–1.37 | |
| Medium-high | 12.2 | 14.1 | 1.18 | 0.89–1.57 | 1.28 | 0.95–1.73 | 1.21 | 0.887–1.644 | 1.17 | 0.86–1.59 | |
| High | 10.0 | 14.5 | 1.52 | 1.16–1.99 | 1.58 | 1.19–2.08 | 1.52 | 1.138–2.039 | 1.46 | 1.09–1.97 | |
aWidowed, separated, or divorced.
bGross household income divided by square root of household size. EHI groups were classified according to the standard income quartile of sample households for each year presented by the Korea National Health and Nutrition Examination Survey.
cIncluding evening or night work.
aWidowed, separated, or divorced.
bGross household income divided by square root of household size. EHI groups were classified according to the standard income quartile of sample households for each year presented by the Korea National Health and Nutrition Examination Survey.
cIncluding evening or night work.
aThe participants who worked < 52 hours a week were considered as a reference group.
bCrude odds ratio was calculated by logistic regression.
cModel 1: Adjusted for age, sex, and marrital status.
dModel 2: Adjusted for age, sex, marrital status, education, occupation, employment status, and shiftwork.
eModel 3: Adjusted for age, sex, marrital status, education, occupation, employment status, shiftwork, smoking, drinking, hypertension, diabetes, and depression.
 KSOEM
KSOEM

 Cite
Cite

