Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 34; 2022 > Article
- Original Article Association between sitting-time at work and incidence of erosive esophagitis diagnosed by esophagogastroduodenoscopy: a Korean cohort study
-
Daehoon Kim
 , Yesung Lee
, Yesung Lee , Eunchan Mun
, Eunchan Mun , Eunhye Seo
, Eunhye Seo , Jaehong Lee
, Jaehong Lee , Youshik Jeong
, Youshik Jeong , Jinsook Jeong
, Jinsook Jeong , Woncheol Lee
, Woncheol Lee
-
Annals of Occupational and Environmental Medicine 2022;34:e15.
DOI: https://doi.org/10.35371/aoem.2022.34.e15
Published online: July 21, 2022
Department of Occupational and Environ mental Medicine, Kangbuk Samsung Hospital, School of Medicine, Sungkyunkwan University, Seoul, Korea.
- Correspondence: Woncheol Lee. Department of Occupational and Environmental Medicine, Kangbuk Samsung Hospital, School of Medicine, Sungkyunkwan University, 29 Saemunan-ro, Jongno-gu, Seoul 03181, Korea. doctor.oem@gmail.com
Copyright © 2022 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background Most previous longitudinal studies on lifestyle and gastroesophageal reflux disease (GERD) have focused on physical activity rather than sitting time. The main purpose of this study was to investigate the relationship between prolonged sitting time and the development of erosive esophagitis (EE).
-
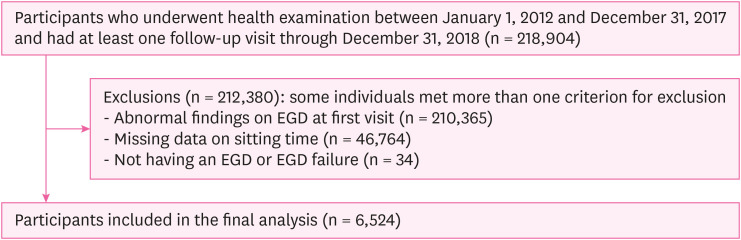
Methods A self-report questionnaire was used for measuring sitting time in the Kangbuk Samsung Health Study. Sitting time was categorized into four groups: ≤ 6, 7–8, 9–10, and ≥ 11 hours/day. Esophagogastroduodenoscopy (EGD) was performed by experienced endoscopists who were unawared of the aims of this study. Hazard ratios (HRs) and 95% confidence intervals (CIs) for the development of EE were estimated using Cox proportional hazards analyses with ≤ 6 hours/day sitting time as the reference.
-
Results There were 6,524 participants included in the study. During a mean follow-up of 3.14 years, 2,048 incident cases developed EE. In age- and sex-adjusted models, the HR in the group sitting ≥ 11 hours per day compared ≤ 6 hours per day was 0.88 (95% CI: 0.76–0.99). After further adjusting for alcohol intake, smoking status, educational level, history of diabetes, and history of dyslipidemia, sitting time was still significantly related to the risk of EE (HR, 0.87; 95% CI: 0.76–0.98). After further adjustment for exercise frequency, this association persisted (HR, 0.86; 95% CI: 0.76–0.98). In subgroup analysis by obesity, the relationship between sitting time and EE was only significant among participants with body mass index < 25 kg/m2 (HR, 0.82; 95% CI: 0.71–0.95).
-
Conclusions Generally, prolonged sitting time is harmful to health, but with regard to EE, it is difficult to conclude that this is the case.
BACKGROUND
METHODS
RESULTS
Baseline characteristics of study population by sitting time per day
HR for the incidence of erosive esophagitis by sitting time per day
Incidence of erosive esophagitis by sitting time per day stratified by obesity
DISCUSSION
Abbreviations
BMI
CI
CPS-II
EE
EGD
GERD
HbA1c
HR
ICD
IPAQ
KNHANES
KSHS
SD
SES
-
Funding: This work was supported by the Korean Society of Occupational and Environmental Medicine (KSOEM).
-
Competing interests: The authors declare that they have no competing interests.
-
Author Contributions:
NOTES
- 1. Dean BB, Crawley JA, Schmitt CM, Wong J, Ofman JJ. The burden of illness of gastro-oesophageal reflux disease: impact on work productivity. Aliment Pharmacol Ther 2003;17(10):1309–1317. 12755844.ArticlePubMedPDF
- 2. Shin WG, Kim HU, Kim SG, Kim GH, Shim KN, Kim JW, et al. Work productivity and activity impairment in gastroesophageal reflux disease in Korean full-time employees: a multicentre study. Dig Liver Dis 2012;44(4):286–291. 22325831.ArticlePubMed
- 3. Park CH, Lee SK. Gastroesophageal reflux disease. Korean J Gastroenterol 2019;73(2):70–76. 30845382.ArticlePubMedPDF
- 4. Kim N, Lee SW, Cho SI, Park CG, Yang CH, Kim HS, et al. The prevalence of and risk factors for erosive oesophagitis and non-erosive reflux disease: a nationwide multicentre prospective study in Korea. Aliment Pharmacol Ther 2008;27(2):173–185. 17973646.ArticlePubMed
- 5. Fock KM, Talley N, Goh KL, Sugano K, Katelaris P, Holtmann G, et al. Asia-Pacific consensus on the management of gastro-oesophageal reflux disease: an update focusing on refractory reflux disease and Barrett’s oesophagus. Gut 2016;65(9):1402–1415. 27261337.ArticlePubMed
- 6. Kim KM, Cho YK, Bae SJ, Kim DS, Shim KN, Kim JH, et al. Prevalence of gastroesophageal reflux disease in Korea and associated health-care utilization: a national population-based study. J Gastroenterol Hepatol 2012;27(4):741–745. 21916988.ArticlePubMed
- 7. Hampel H, Abraham NS, El-Serag HB. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med 2005;143(3):199–211. 16061918.ArticlePubMed
- 8. Chang P, Friedenberg F. Obesity and GERD. Gastroenterol Clin North Am 2014;43(1):161–173. 24503366.ArticlePubMedPMC
- 9. Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut 2018;67(3):430–440. 28232473.ArticlePubMed
- 10. Maret-Ouda J, Markar SR, Lagergren J. Gastroesophageal reflux disease: a review. JAMA 2020;324(24):2536–2547. 33351048.ArticlePubMed
- 11. Ness-Jensen E, Lagergren J. Tobacco smoking, alcohol consumption and gastro-oesophageal reflux disease. Best Pract Res Clin Gastroenterol 2017;31(5):501–508. 29195669.ArticlePubMed
- 12. Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Lifestyle related risk factors in the aetiology of gastro-oesophageal reflux. Gut 2004;53(12):1730–1735. 15542505.ArticlePubMedPMC
- 13. Chirila I, Morariu ID, Barboi OB, Drug VL. The role of diet in the overlap between gastroesophageal reflux disease and functional dyspepsia. Turk J Gastroenterol 2016;27(1):73–80. 26728864.ArticlePubMed
- 14. Shawdon A. Gastro-oesophageal reflux and exercise. Important pathology to consider in the athletic population. Sports Med 1995;20(2):109–116. 7481280.PubMed
- 15. Bi L, Triadafilopoulos G. Exercise and gastrointestinal function and disease: an evidence-based review of risks and benefits. Clin Gastroenterol Hepatol 2003;1(5):345–355. 15017652.ArticlePubMed
- 16. Collings KL, Pierce Pratt F, Rodriguez-Stanley S, Bemben M, Miner PB. Esophageal reflux in conditioned runners, cyclists, and weightlifters. Med Sci Sports Exerc 2003;35(5):730–735. 12750580.ArticlePubMed
- 17. Pandolfino JE, Bianchi LK, Lee TJ, Hirano I, Kahrilas PJ. Esophagogastric junction morphology predicts susceptibility to exercise-induced reflux. Am J Gastroenterol 2004;99(8):1430–1436. 15307855.ArticlePubMed
- 18. Parmelee-Peters K, Moeller JL. Gastroesophageal reflux in athletes. Curr Sports Med Rep 2004;3(2):107–111. 14980140.ArticlePubMed
- 19. Ravi N, Stuart RC, Byrne PJ, Reynolds JV. Effect of physical exercise on esophageal motility in patients with esophageal disease. Dis Esophagus 2005;18(6):374–377. 16336607.ArticlePubMed
- 20. Jóźków P, Waśko-Czopnik D, Dunajska K, Medraś M, Paradowski L. The relationship between gastroesophageal reflux disease and the level of physical activity. Swiss Med Wkly 2007;137(33-34):465–470. 17990130.ArticlePubMedPDF
- 21. Herregods TV, van Hoeij FB, Oors JM, Bredenoord AJ, Smout AJ. Effect of running on gastroesophageal reflux and reflux mechanisms. Am J Gastroenterol 2016;111(7):940–946. 27068716.ArticlePubMedPDF
- 22. Zheng Z, Nordenstedt H, Pedersen NL, Lagergren J, Ye W. Lifestyle factors and risk for symptomatic gastroesophageal reflux in monozygotic twins. Gastroenterology 2007;132(1):87–95. 17241862.ArticlePubMedPMC
- 23. Korea National Health and Nutrition Examination Survey. Updated 2020]. Accessed July 20, 2021]. https://knhanes.kdca.go.kr/knhanes/sub04/sub04_04_01.do .
- 24. Garcia LM, da Silva KS, Del Duca GF, da Costa FF, Nahas MV. Sedentary behaviors, leisure-time physical inactivity, and chronic diseases in Brazilian workers: a cross sectional study. J Phys Act Health 2014;11(8):1622–1634. 24732950.ArticlePubMed
- 25. Stamatakis E, Gale J, Bauman A, Ekelund U, Hamer M, Ding D. Sitting time, physical activity, and risk of mortality in adults. J Am Coll Cardiol 2019;73(16):2062–2072. 31023430.ArticlePubMed
- 26. Bontrup C, Taylor WR, Fliesser M, Visscher R, Green T, Wippert PM, et al. Low back pain and its relationship with sitting behaviour among sedentary office workers. Appl Ergon 2019;81:102894. 31422243.ArticlePubMed
- 27. Citko A, Górski S, Marcinowicz L, Górska A. Sedentary lifestyle and nonspecific low back pain in medical personnel in north-east Poland. BioMed Res Int 2018;2018:1965807. 30271778.ArticlePubMedPMCPDF
- 28. Kumar S, Sharma S, Norboo T, Dolma D, Norboo A, Stobdan T, et al. Population based study to assess prevalence and risk factors of gastroesophageal reflux disease in a high altitude area. Indian J Gastroenterol 2011;30(3):135–143. 21181325.ArticlePubMedPDF
- 29. Chadolias D, Zissimopoulos A, Nena E, Agathokleous MN, Drakopoulos V, Constantinidis TC, et al. Association of occupational exposures and work characteristics with the occurrence of gastrointestinal disorders. Hippokratia 2017;21(2):74–79. 30455559.PubMedPMC
- 30. Patel AV, Maliniak ML, Rees-Punia E, Matthews CE, Gapstur SM. Prolonged leisure time spent sitting in relation to cause-specific mortality in a large US cohort. Am J Epidemiol 2018;187(10):2151–2158. 29947736.ArticlePubMedPMC
- 31. Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35(8):1381–1395. 12900694.ArticlePubMed
- 32. Chun MY. Validity and reliability of Korean version of international physical activity questionnaire short form in the elderly. Korean J Fam Med 2012;33(3):144–151. 22787536.ArticlePubMedPMC
- 33. Khoury T, Mari A, Amara H, Jabaren M, Watad A, Nseir W, et al. Impact of chronic statins use on the development of esophagitis in patients with gastroesophageal reflux disease. Can J Gastroenterol Hepatol 2019;2019:6415757. 30854351.ArticlePubMedPMCPDF
- 34. Hallan A, Bomme M, Hveem K, Møller-Hansen J, Ness-Jensen E. Risk factors on the development of new-onset gastroesophageal reflux symptoms. A population-based prospective cohort study: the HUNT study. Am J Gastroenterol 2015;110(3):393–400. 25665934.ArticlePubMedPDF
- 35. Sun XM, Tan JC, Zhu Y, Lin L. Association between diabetes mellitus and gastroesophageal reflux disease: a meta-analysis. World J Gastroenterol 2015;21(10):3085–3092. 25780309.ArticlePubMedPMC
- 36. Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 2020;54(24):1451–1462. 33239350.ArticlePubMedPMC
- 37. Pyo JH, Kim JW, Kim TJ, Lee H, Min YW, Min BH, et al. Physical activity protects against the risk of erosive esophagitis on the basis of body mass index. J Clin Gastroenterol 2019;53(2):102–108. 29099464.ArticlePubMed
- 38. Murao T, Sakurai K, Mihara S, Marubayashi T, Murakami Y, Sasaki Y. Lifestyle change influences on GERD in Japan: a study of participants in a health examination program. Dig Dis Sci 2011;56(10):2857–2864. 21487772.ArticlePubMedPMC
- 39. Alkhathami AM, Alzahrani AA, Alzhrani MA, Alsuwat OB, Mahfouz ME. Risk factors for gastroesophageal reflux disease in Saudi Arabia. Gastroenterol Res 2017;10(5):294–300.ArticlePubMedPMC
- 40. Zhang M, Hou ZK, Huang ZB, Chen XL, Liu FB. Dietary and lifestyle factors related to gastroesophageal reflux disease: a systematic review. Ther Clin Risk Manag 2021;17:305–323. 33883899.ArticlePubMedPMCPDF
- 41. Corley DA, Kubo A. Body mass index and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Gastroenterol 2006;101(11):2619–2628. 16952280.ArticlePubMed
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Causal links between socioeconomic status, leisure sedentary behaviours and gastro-oesophageal reflux disease: a multivariable two-sample Mendelian randomisation study
Xingji Lian, Yifen Lin, Xiaohui Peng, Yanhui Wang, Ting He, Ziyong He, Wenlong Gu, Hongwu Wang, Feng He, Yuyu Huang
Journal of Epidemiology and Community Health.2023; 77(7): 460. CrossRef
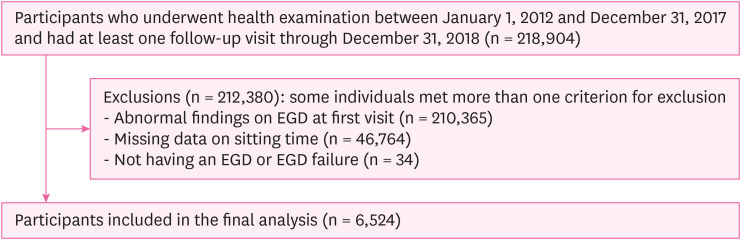
Fig. 1
| Variables | Sitting time (hours/day) | ||||
|---|---|---|---|---|---|
| ≤ 6 | 7–8 | 9–10 | ≥ 11 | ||
| Subjects | 1,641 | 1,307 | 1,908 | 1,668 | |
| Age (years) | 33.0 ± 5.4 | 32.3 ± 5.1 | 32.0 ± 4.5 | 31.5 ± 4.1 | < 0.001 |
| Men (%) | 45.95 | 54.55 | 53.51 | 56.06 | < 0.001 |
| Alcohol intake, ≥ 10 g/day (%) | 33.94 | 34.12 | 33.75 | 32.49 | 0.214 |
| Current smoker (%) | 12.00 | 11.71 | 12.47 | 12.59 | 0.614 |
| Education, ≥ college graduate (%) | 78.61 | 85.62 | 90.62 | 92.81 | < 0.001 |
| Diabetes mellitus (%) | 0.98 | 0.46 | 0.84 | 0.60 | 0.402 |
| Dyslipidemia (%) | 0.43 | 0.69 | 0.21 | 0.96 | 0.177 |
| Exercise, ≥ 3 times/week (%) | 16.03 | 11.25 | 9.80 | 8.33 | < 0.001 |
| BMI (kg/m2) | 22.51 ± 3.11 | 22.54 ± 3.06 | 22.48 ± 3.12 | 22.48 ± 3.15 | 0.663 |
| Obesity, ≥ 25 kg/m2 (%) | 19.38 | 20.66 | 19.71 | 20.02 | 0.800 |
| Sitting time (hours/day) | Person-years | Incident cases | Incidence density (per 10 person-years) | Multivariable-adjusted HRa (95% CI) | |||
|---|---|---|---|---|---|---|---|
| Crude | Model 1 | Model 2 | Model 3 | ||||
| ≤ 6 | 5,097.7 | 533 | 1.046 | 1.00 | 1.00 | 1.00 | 1.00 |
| 7–8 | 4,004.5 | 396 | 0.989 | 0.96 (0.84–1.09) | 0.94 (0.82–1.07) | 0.94 (0.83–1.08) | 0.94 (0.82–1.08) |
| 9–10 | 5,988.4 | 592 | 0.989 | 0.93 (0.82–1.04) | 0.91 (0.80–1.02) | 0.90 (0.80–1.02) | 0.90 (0.80–1.02) |
| ≥ 11 | 5,406.5 | 527 | 0.975 | 0.90 (0.79–1.01) | 0.88 (0.76–0.99) | 0.87 (0.76–0.98) | 0.86 (0.76–0.98) |
| 0.060 | 0.028 | 0.021 | 0.016 | ||||
| Subgroup | Sitting time (hours/day), HRsa (95% CI) | |||||
|---|---|---|---|---|---|---|
| ≤ 6 | 7–8 | 9–10 | ≥ 11 | |||
| BMI | ||||||
| < 25 kg/m2 | 1.00 | 0.96 (0.83–1.12) | 0.93 (0.81–1.07) | 0.82 (0.71–0.95) | 0.009 | |
| ≥ 25 kg/m2 | 1.00 | 0.87 (0.65–1.16) | 0.77 (0.59–1.00) | 0.99 (0.76–1.30) | 0.768 | |
Data are expressed as frequency or mean ± standard deviation.
BMI: body mass index.
GERD: gastroesophageal reflux disease; HR: hazard ratio; CI: confidence interval.
aEstimated from Cox proportional hazards models. Multivariable model 1 was adjusted for age and sex; model 2: model 1 plus adjustment for alcohol intake, smoking status, educational level, history of diabetes, history of dyslipidemia; model 3: model 2 plus adjustment for exercise frequency.
HR: hazard ratio; CI, confidence interval.
aEstimated from Cox proportional hazard models: adjusted for sex, age, alcohol intake, smoking status, educational level, history of diabetes, history of dyslipidemia, and exercise frequency.
 KSOEM
KSOEM

 Cite
Cite

