Abstract
-
Background
Antimony is used in catalysts, pesticides, brake systems, pharmaceuticals, and synthetic fire retardants in the plastic, paint, and rubber industries. Accumulation of trivalent antimony compounds in the body can cause cardiotoxic effects and increase the risk of electrocardiogram (ECG) abnormalities and sudden death. Antimony exposure can result in action potential prolongation, causing a cardiac repolarization delay, which appears as QTc prolongation and T-wave abnormalities on the ECG. There are no studies on antimony-associated cardiac toxicity in Korea.
-
Case presentation
Accordingly, the present study reports cases of ECG abnormalities in workers handling antimony trisulfide at a company located in the Gyeongsangbuk-do region. Nineteen workers employed at an automobile brake lining manufacturer were exposed to antimony trisulfide dust through thermoforming, grinding, and drilling processes. In 2020, the workers were reported to work 12-hour shifts, 5 days a week. The time-weighted average (TWA) of antimony trisulfide exposure measured in workers was 0.0028 mg/m3. Two workers were excluded from the analysis due to pre-existing medical conditions (cardiovascular disease). Of the remaining 17 workers, ECG abnormalities were found in 41% (seven out of 17: four with QTc prolongation and T-wave abnormalities; two with only T-wave abnormalities; and one with only QTc prolongation).
-
Conclusions
This case report outlines the first few cases in Korea in which potential cardiac toxicity caused by occupational exposure to antimony was identified. However, data regarding cardiac toxicity caused by antimony exposure are still lacking in Korea; thus, additional studies are needed to identify causal relationships.
-
Keywords: Antimony poisoning; QTc prolongation; Arrhythmia; Occupational exposure
BACKGROUND
Antimony is a brittle, silver-white metalloid ubiquitous in the terrestrial environment as a product of natural phenomena (volcanic eruptions, typhoons, forest fires), typically found in sulfide and stibnite (mineral) forms. It is usually alloyed with lead or tin as a hardener in lead-acid batteries, solder, bearings, and ammunition because it lacks flexibility. Antimony trioxide, the most commonly used antimony compound, is used in catalysts, pesticides, brake systems, pharmaceuticals, and as a synthetic fire retardant in the plastic, paint, and rubber industries.
1 Increased industrial use has resulted in > 50% increase in antimony concentration in the natural environment over the past three decades.
2
According to the work environment survey conducted every 5 years by the Korea Occupational Safety and Health Agency, 11,600 tons of antimony were produced from three companies, and 28,383 tons were handled by 149 companies in 2004. In 2019, four companies produced 4,079 t, and 537 companies handled 55,557 t of antimony. Although the amount produced nationally decreased, the amount handled nearly doubled between 2004 and 2019 due to an increase in the imported volume of antimony. The US and EU environmental protection agencies consider antimony a priority pollutant. Korea has also designated antimony as harmful, subject to special medical examination and antimony trioxide as special management material.
Accumulation of trivalent antimony compounds inside the body can cause cardiotoxic effects and increase the risk of hypertension, electrocardiogram (ECG) abnormalities and sudden death.
3 In addition, it can negatively affect the respiratory, reproductive, and integumentary systems as well as the eyes, nasal cavity, and pharynx. In numerous in vitro studies, cardiac toxicity, particularly cardiac myocyte damage induced by trivalent antimony compounds, was observed, which can cause cell apoptosis, transformation, and ECG abnormalities. Tirmenstein et al. identified that exposure to trivalent antimony compounds could disrupt intracellular thiol homeostasis.
4
Wey et al. found that a gradual increase in resting (or diastolic) calcium concentration can lead to cardiac activity cessation and cell apoptosis.
5 The researchers mentioned that changes in myocardial calcium homeostasis could explain the ECG changes observed in the in vivo studies.
6 Meanwhile, other studies reported that trivalent antimony compounds caused action potential prolongation by increasing calcium currents in cardiac myocytes.
7
In antimony exposure cases in America, among 75 workers in the metal polishing industry exposed to antimony trisulfide dust for 8–24 months, sudden death occurred in eight workers, and ECG abnormalities were found in 37 workers.
8 Moreover, heart disease and ECG changes were observed in 14 workers exposed to antimony trioxide or antimony trisulfide dust.
9 In a mortality study in a cohort of antimony smelter workers, increased mortality caused by ischemic heart disease was observed.
10 Such findings were supported by the results from a study on ECG abnormalities that appeared after repeated injections of antimony in patients with leishmaniasis and an animal study with the administration of trivalent antimony compounds.
11,12
Studies in Korea have reported contact dermatitis and pneumoconiosis caused by antimony exposure, but no reports have been published on cardiac toxicity. Furthermore, in introducing the concept of target organ special health examination items, the ECG test, which originally was optional, was later 2009 deemed the primary screening method, but studies on the association between antimony and cardiac toxicity are still lacking in Korea. Accordingly, the present study reports cases of ECG abnormalities in workers handling antimony trisulfide at a company located in the Gyeongsangbuk-do region.
CASE PRESENTATION
The case study setting was an automobile brake lining manufacturer where antimony trisulfide is used as a lubricant. The workers are exposed to antimony trisulfide dust through the following processes: First, the workers are exposed to dust when placing the solid raw material into the thermoforming machine to form the product shape. Later, dust is produced during the grinding and drilling needed to polish the brake lining surface and couple it to the brake system. This study was approved by the Institutional Review Board (IRB) of Soonchunhyang University Hospital in Gumi (IRB No. 2022-01).
In 2020, this company had 19 antimony trisulfide-exposed employees who worked 12-hour shifts, five days a week. The company was using an exterior upward suction-type local exhaust hood. Measurements of the work environment, i.e., the mass of heavy metals present in the air (filtration sampling: inductively coupled plasma), showed that the time-weighted average (TWA) of antimony trisulfide exposure was 0.0028 mg/m3. The Work Environment Measurement (WEM) results from 2018 to 2021 did not differ significantly (0.0025–0.0029 mg/m3). Workers wore regular face masks until early 2021 before changing to level 1 dust masks.
Among the 19 workers, 2 who had received a percutaneous coronary artery intervention for myocardial infarction before joining the company were excluded; thus, the ECG findings of the remaining 17 workers assessed after joining the company were compared and analyzed. Employment duration varied between 5 and 15 years. There were 13 males and 4 females in the study group, where 8, 6, and 3 workers performed thermoforming, grinding, and drilling work, respectively. A standard 12-lead ECG was used for the measurement. The paper speed was 25 mm/s, and the calibration was 10 mm/mV. The ECG system automatically measured the heart rate (HR), PR interval, QRS, QTc, and P-axis. Since QT interval is affected by heart rate, QTc interval corrected based on heart rate is generally used. The Bazett formula was used for QTc correction (QTc(B) = QT/
RR.) QTc prolongation was defined as ≥ 450 ms for males and ≥ 460 ms for females in accordance with the definition given by the American Heart Association, American College of Cardiology Foundation, and Heart Rhythm Society.
13
Among the 17 antimony trisulfide-exposed workers, ECG abnormalities were found in 7 (41%) (4 workers with QTc prolongation and T-wave abnormalities; 2 with only T-wave abnormalities; and 1 with only QTc prolongation). A review of statements provided by these seven workers and their medical records revealed no prior work history of handling antimony. Only worker C took medication for hypertension; no other worker had any chronic disease. There was no prior history of coronary or cerebrovascular disorders, chronic kidney disease, chronic liver disease, or hypothyroidism. The workers were not taking any medication that would prolong the QTc interval and had no prior or current history of palpitations, dizziness, syncope, or seizures. Moreover, the workers had no history of heart diseases, such as congestive heart failure, cardiomyopathy, myocardial infarction, or arrhythmia before joining the company, and their families’ medical histories showed no heart disease or long QT syndrome.
Worker A: 62-year-old female who worked in the thermoforming process for 6 years, starting in 2015. Her ECG findings were normal until 2020, 5 years after she joined the company, where her results showed QTc prolongation (473 ms, which is a 43 ms increase since 2016) and a T-wave abnormality. Results for 2021 are unavailable as she has since resigned.
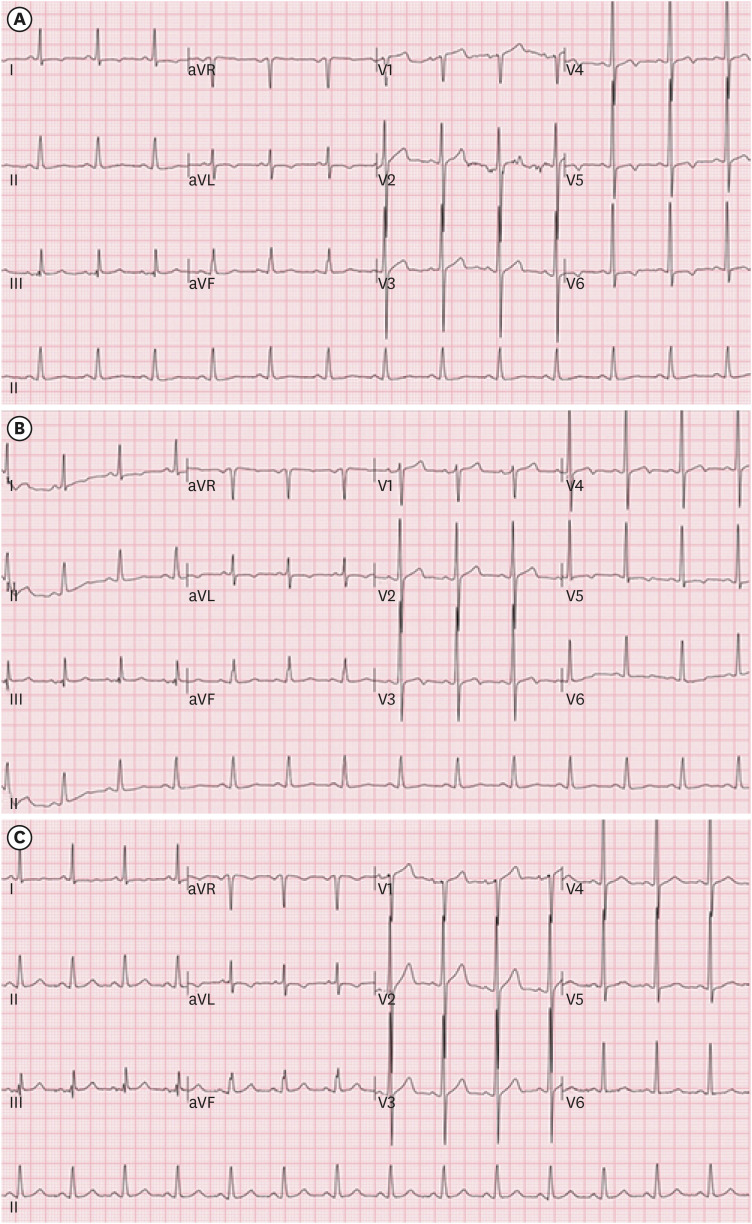
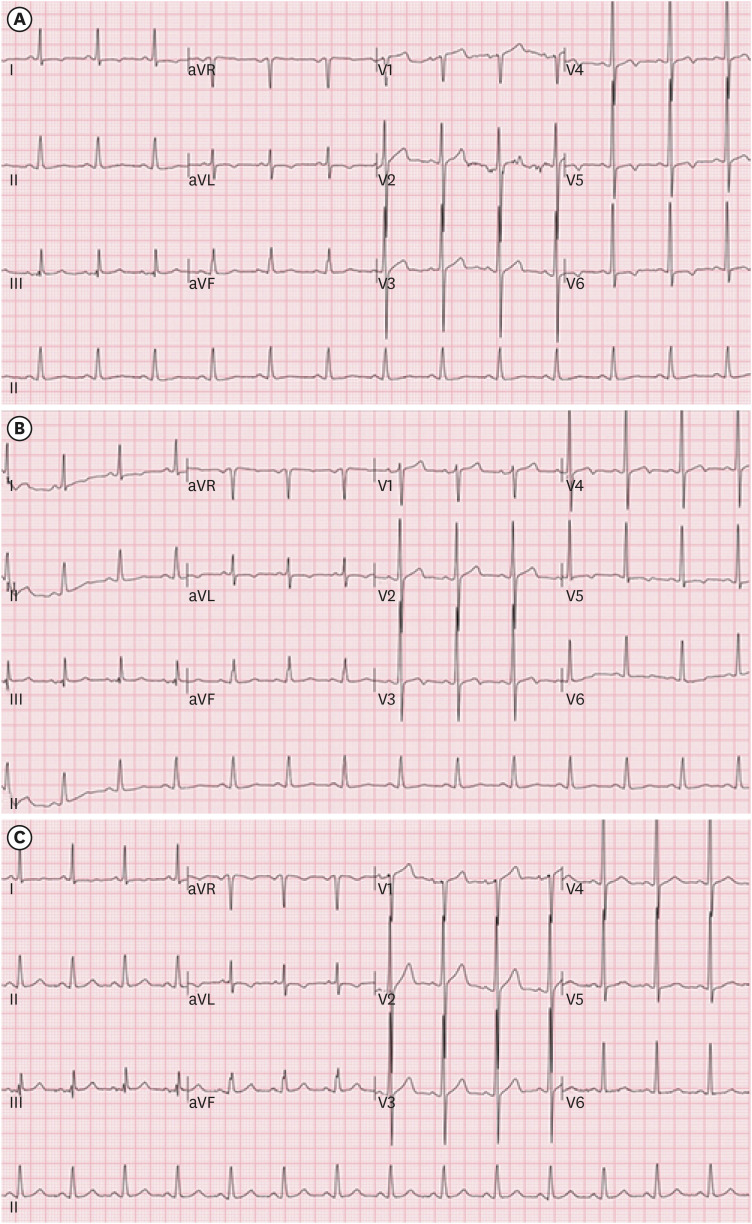
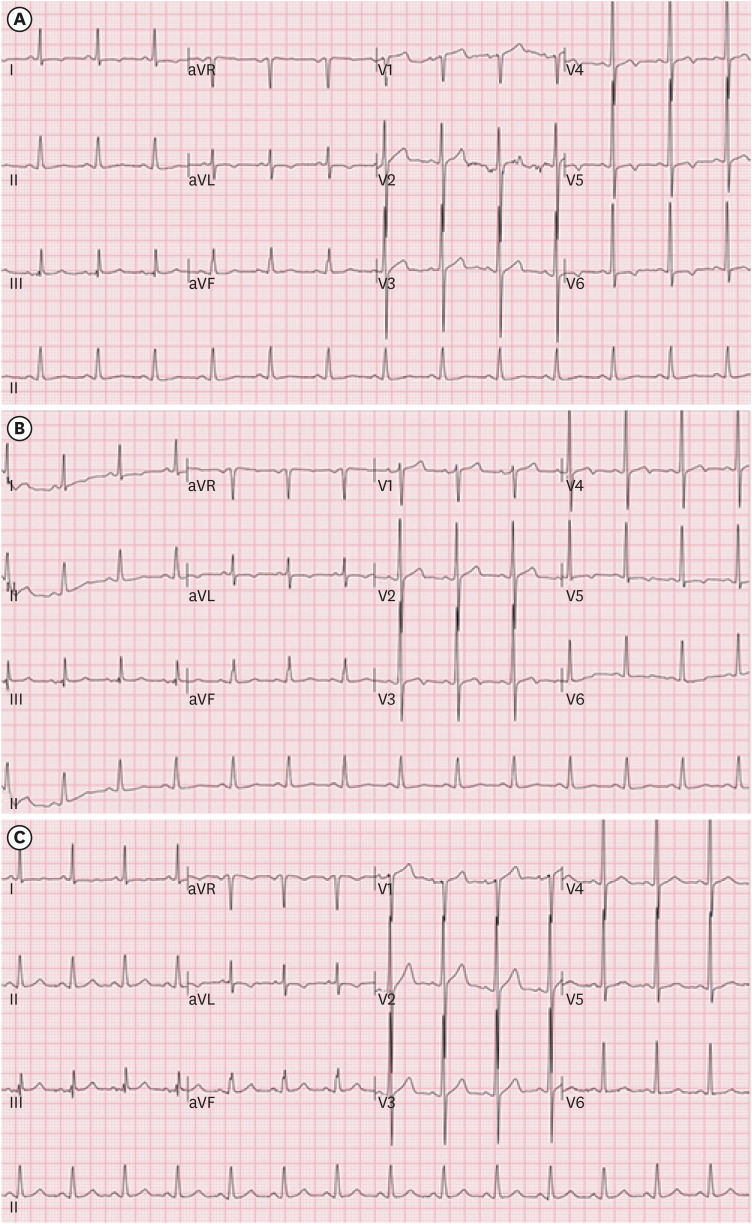
Worker B: 61-year-old male who worked in the thermoforming process for five years, starting in 2016. ECG findings three years later in 2019 showed QTc prolongation and a T-wave abnormality. His ECG findings in 2018 showed a normal QTc interval, which subsequently increased to 468 ms in 2019 and 490 ms in 2020 (
Fig. 1). QTc had significantly increased by the end of 2020, warranting worker B to undergo additional tests and treatment in 2021, which ultimately decreased his QTc interval to 473 ms.
Fig. 1
ECG changes in a 61-year-old male working in the thermoforming process. (A) 2018 ECG findings showed a normal QTc interval of 449 ms; (B) 2019 ECG findings showed an increased QTc interval to 468 ms; (C) 2020 ECG findings showed an increased QTc interval to 490 ms.
ECG: electrocardiogram.
Worker C: 61-year-old male who worked in the drilling process for 7 years, from 2014. ECG findings were normal until 2016, but in 2018, 4 years after being employed, results showed QTc prolongation (487 ms) and a T-wave abnormality, causing him to start treatment for arrhythmia in addition to taking blood pressure medication.
Worker D, 57-year-old male who worked in the drilling process for 6 years, from 2015. His ECG findings were normal until 2018, but in 2019, four years after joining the company, results showed QTc prolongation (464 ms) and a T-wave abnormality. At the end of 2021, the QTc interval increased significantly to 524 ms, warranting worker D to receive additional tests and start treatment at the cardiology department in 2022.
Worker E: 58-year-old male who worked in the drilling process for 3 years, starting in 2018. His ECG findings were normal until 2019, but 2 years after being hired, ECG findings in 2020 showed a T-wave abnormality.
Worker F: 49-year-old female who worked in the grinding process for 5 years, starting in 2016. Her ECG findings were normal up to 2018, but ECG findings in 2020, her fifth year of employment, showed QTc prolongation (462 ms). This is a 32 ms increase from the QTc interval in 2016.
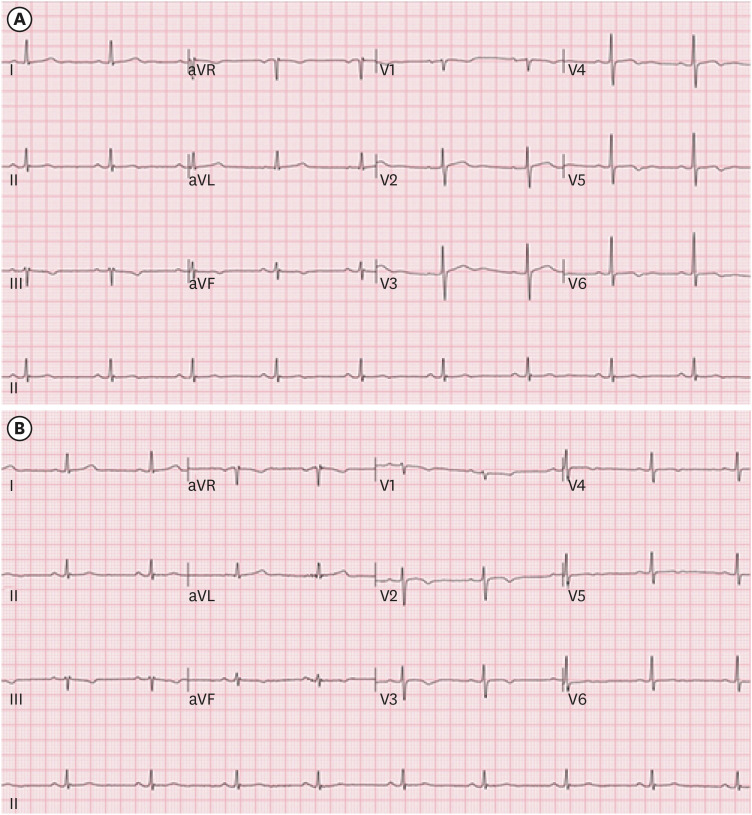
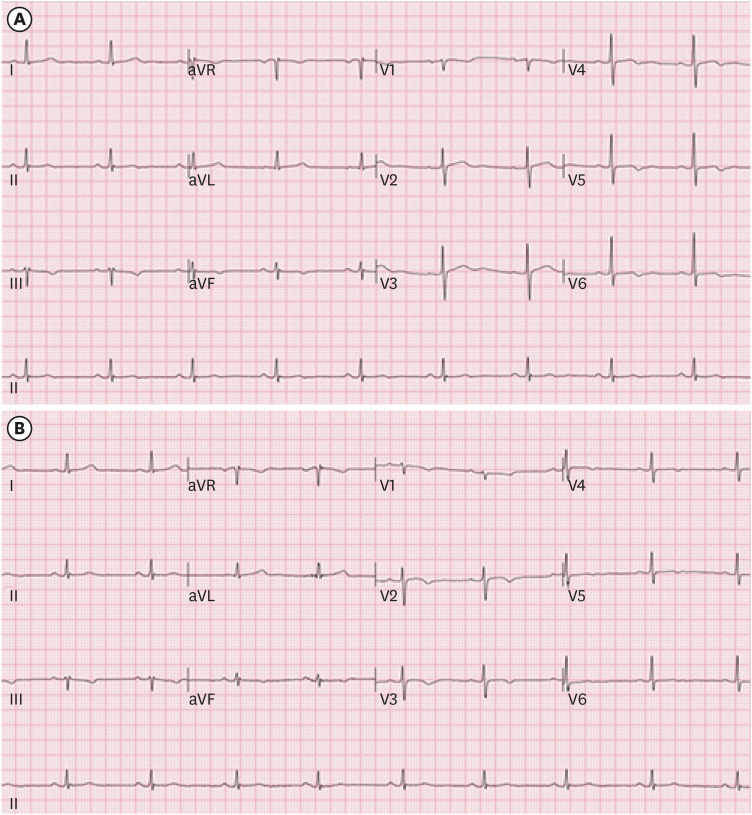
Worker G: 64-year-old female who worked in the grinding process for 6 years, starting in 2015. Her ECG findings were normal until 2018, but four years later, ECG findings in 2019 showed a T-wave abnormality (
Fig. 2,
Table 1).
Fig. 2
ECG changes in a 64-year-old female working in grinding process. (A) Normal ECG findings in 2018; (B) 2019 ECG findings showing inverted T wave in V2-V3 leads.
ECG: electrocardiogram.
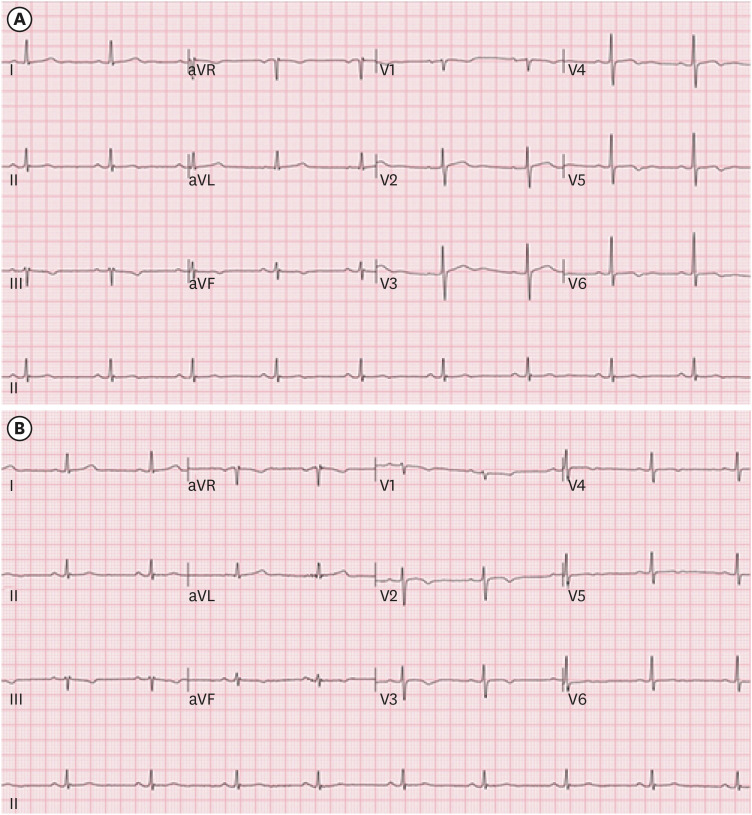
Table 1 Data on work process and ECG findings in workers
|
Worker |
Age/Sex |
Process |
Year of entry |
Working period |
ECG findings |
Mask worn |
|
A |
62/F |
Thermoforming |
2015 |
6y |
(2016) Normal ECG (QTc 430 ms) |
Yes |
|
(2018) Normal ECG (QTc 433 ms) |
|
(2019) Normal ECG (QTc 440 ms) |
|
(2020)a,b Prolonged QTc (473 ms), Nonspecific T-wave abnormality |
|
(2021) Resigned |
|
B |
61/M |
Thermoforming |
2016 |
5y |
(2018)b Nonspecific T-wave abnormality (QTc 449 ms) |
Yes |
|
(2019)a Prolonged QTc (468 ms), T-wave abnormality |
|
(2020) Prolonged QTc (490 ms), T-wave abnormality |
|
(2021) Prolonged QTc (473 ms), T-wave abnormality |
|
C |
61/M |
Drilling |
2014 |
7y |
(2016) Normal ECG (QTc 445 ms) |
Yes |
|
(2018)a,b Prolonged QTc (487 ms), Nonspecific T-wave abnormality |
|
(2019) Prolonged QTc (485 ms), Nonspecific T-wave abnormality |
|
(2020) Prolonged QTc (469 ms), 1°AV-block |
|
(2021) Prolonged QTc (475 ms) |
|
D |
57/M |
Drilling |
2015 |
6y |
(2018) Normal ECG (QTc 438 ms) |
Yes |
|
(2019)a,b Prolonged QTc (464 ms), T-wave abnormality |
|
(2020) Prolonged QTc (454 ms) |
|
(2021) Prolonged QTc (524 ms) |
|
E |
58/M |
Drilling |
2018 |
3y |
(2019) Normal ECG |
Yes |
|
(2020)b T-wave abnormality |
|
(2021) T-wave abnormality |
|
F |
49/F |
Grinding |
2016 |
5y |
(2016) Normal ECG |
Yes |
|
(2018) Normal ECG (QTc 456 ms) |
|
(2020)a Prolonged QTc (462 ms) |
|
(2021) Normal ECG (QTc 442 ms) |
|
G |
64/F |
Grinding |
2015 |
6y |
(2016) Normal ECG |
Yes |
|
(2018) Normal ECG |
|
(2019)b T wave abnormality (inversion) |
|
(2020) T wave abnormality (inversion) |
|
(2021) T wave abnormality (inversion) |
Currently, the workers are receiving education regarding personal hygiene care, and the department of cardiology monitors their symptoms following a consultation about the abnormal ECG findings.
Several studies have shown that antimony exposure causes an increase in blood pressure.
14 A comparison of the trends in blood pressure of 17 workers recorded at the initial and final examinations showed that 11 (64.7%) had elevated blood pressure, 7 (41.2%) had a systolic blood pressure of ≥ 140, a diastolic blood pressure of ≥ 90, or were taking antihypertensives. The remaining 6 (35.3%) had decreased blood pressure. Of the 5 workers with a prolonged QTc interval, 4 had elevated blood pressure. This is consistent with the results of previous studies, which showed that increased exposure to antimony increases blood pressure. In 2021, a test on urinary antimony, a biological exposure index, was included as a secondary test for screening workers with ECG abnormalities. The concentration of antimony in each worker was as follows: no results for worker A (resigned), 8.6 ug/L for worker B, 2.3 ug/L for worker C, 3.1 ug/L for worker D, 1.0 ug/L for worker E, 0.3 ug/L for worker F, and 0.7 ug/L for worker G.
DISCUSSION AND CONCLUSION
Among the 17 antimony-exposed workers in the present study, 16 were aged 40–65 years, and all were apparently healthy without chronic or history of heart diseases, except for worker C, who was receiving treatment for hypertension. The prevalence of QTc prolongation among workers aged 40–65 was 4 of 15 cases and increased to 6 of 15 cases with T-wave abnormalities. The workers showed a relatively higher prevalence of QTc prolongation and T-wave abnormality than healthy Korean adults of the same age group.
Occupational exposure to trivalent antimony compounds occurs primarily by inhalation in antimony smelting facilities, coal-fired power plants, and antimony treatment or processing facilities. Antimony compounds are ocular, mucosal, and skin irritants, with skin disorders and eye irritation reported among workers exposed to airborne antimony compounds.
15 Dermatitis appears more frequently during summer and among workers exposed to high temperatures due to antimony dissolving in sweat and penetrating the skin through the sweat glands. In Korea, skin disorders, such as pustules and papules, caused by trivalent antimony compound exposure were reported in seven foreign workers employed in compounding or packaging processes in a plastic manufacturing plant (4–13 months of work.)
There is currently no consensus on the criteria for QTc prolongation and the upper limits of change from the baseline QT. Lowering the threshold increases the false-positive rate, raising the threshold is making it more difficult to identify arrhythmia symptoms. “The Clinical Evaluation of QT/QTc Interval Prolongation and Proarrhythmic Potential for Non-Antiarrhythmic Drugs (E14),” created at the International Conference on Harmonization (ICH), recommends classifying QTc prolongation into categories depending on the upper limit used when evaluating drugs and comparing the rates of the experimental and control groups that exceed each respective standard. The various upper limits are as follows: > 450, > 480, or > 500 for the absolute QTc interval and > 30 or > 60 for the increase in the QTc interval from the baseline. This is currently being implemented in Europe and countries like the United States and Japan. In addition, according to the 2015 Ministry of Food and Drug Safety guidelines based on the E14 guidelines, drugs that extend the baseline QTc interval for more than 20 ms significantly increase the risk of arrhythmia. Thus, these drugs must be used with caution, as there may have been cases of arrhythmia reported during the drug development process.
When QTc prolongation was defined as > 450 ms for males and > 460 ms for females, the prevalence rates from the ECG data from Ajou University Hospital and Soonchunhyang University Seoul Hospital were similar at 8% and 6%, respectively. This company alone had a prevalence rate of 26.6%, especially because it was measured based on the same standards.
QTc interval prolongation could lead to ventricular arrhythmia known as TdP, which can cause ventricular fibrillation and sudden cardiac death. Moreover, a study on the general population reported that QTc interval prolongation positively correlated with cardiovascular death and sudden death.
16 Risk factors for QTc interval prolongation include female sex, age ≥ 65 years, genetic factors (congenital long QT syndrome), family history of sudden cardiac death, history of taking medication for QTc prolongation, prior history of prolonged QTc arrhythmia, bradycardia, structural heart disease (left ventricular dysfunction), liver/kidney disease, and electrolyte abnormalities associated with nutritional problems (hypokalemia, hypomagnesemia).
17
The raw materials received by the manufacturer in the present study consisted of calcium carbonate, phenolic resin, iron, graphite, aramid, and antimony trisulfide. Based on a review of epidemiological reports, the possibility of ECG changes caused by these raw materials other than antimony trisulfide was reasonably dismissed. Although this study relied solely on workers’ statements, other personal risk factors, such as age and sex, that may have contributed to patients’ risk were not considered. In addition, QTc interval prolongation is an incomplete predictor of TdP, accurate measurements of QTc are difficult to obtain, and errors in measurement of QTc interval and correction of speed may occur at times. Many factors, including demographic variability between individuals, daily fluctuation in QTc interval, and HR, may influence QTc interval measurements. Daily fluctuation in the QTc interval is limited to up to 100 ms.
18
Trivalent antimony compounds have a long biological half-life, and their potential to cause ECG changes after continued exposure, even in trace amounts, has been identified in animal experiments and following parenteral treatments.
11 A study on lung tissue from deceased antimony smelter workers reported no significant differences in the antimony concentration in lung tissue according to retirement period, from discontinuation of exposure immediately after retirement to 20 years after retirement. Such results demonstrate the long biological half-life due to the insolubility of antimony particles.
19 In a study on mice exposed to antimony by inhalation, the half-life and lung burden increased. A study by Newton on chronic inhalation exposure of antimony in rats reported a minimal risk level (MRL) of 0.0003 mg/m
3.
20 Antimony often causes cellular and organic damage to highly vascularized organs, particularly the heart. Trace element content analysis on patients with idiopathic dilated cardiomyopathy showed a 12,000-fold increase in antimony concentration in the cardiac muscle tissue compared to the control group.
21 The fact that chronic exposure to antimony can cause cardiovascular disease can be ascertained from studies based on the National Health and Nutrition Examination Survey of the general US population.
22 In a study on the association between lung cancer and antimony exposure, Schildroth et al.
23 suggested that the occupational exposure level of antimony should be lowered since the level comparable to the current US regulatory standard poses a significant lung cancer risk.
The urinary antimony concentration for the company’s workers was all less than 10 μg/L, which is within the normal range. However, there are currently no antimony biological exposure standards in Korea, and biomarkers are also difficult to use because of low reliability. Studies in Korea showed that serum and urine concentrations did not correlate with occupational exposure.
14,24 Among antimony-exposed workers, those with an increase in QTc intervals above baseline had worked for an average of four years. A new QTc interval anomaly was found for each year since 2018 (2018: 1 person, 2019: 2 people, 2020: 2 people). The average number of years worked for those with T-wave abnormalities was also four years, and a new ECG abnormality was found in each year after 2018 as well (2018: 2 people, 2019: 2 people, and 2020: 2 people). After recognizing that the ECG abnormalities were caused by antimony, the Department of Occupational and Environmental Medicine conducted personal interviews and overall workplace surveys on the workers at the end of 2020 and early 2021.
Despite the low concentration of antimony (TWA: 0.0028 mg/m3, Ministry of Employment and Labor exposure level: 0.5 mg/m3) from work environment measurements, the workers were vulnerable to a high level of direct exposure due to the significant amount of dust created while moving the raw material exacerbated. The following items revealed that the workers were exposed to antimony dust continuously, which further worsened their health: “Stored raw materials in an opened state,” “Neglected to maintain the upkeep of the exhaust system,” “No set times to ventilate factory,” “Wore regular masks,” “Did not store work clothes separately from everyday clothes,” “Did not wash face or work clothes after work,” “Not receiving appropriate treatment for elevated blood pressure, blood sugar, and cholesterol levels,” and “Not seeing a cardiologist despite hearing about arrhythmias.” The results also indicated high levels of exposure to antimony in the past. It is estimated that the prevalence rate in 2020 would have significantly increased as the number of workers with new ECG abnormalities increases with the number of years they work at the company. Workers with ECG abnormalities were ultimately classified as C2 (work compatibility assessment category ‘Na’) because Work Environment Assessment and biological monitoring results are not high. These workers were further grouped into category ‘Na’ in the work compatibility assessment as a detailed cardiac exam and follow-ups were deemed necessary for treating the underlying causes of the ECG abnormalities.
In terms of follow-up care for workers with ECG abnormalities, we first provided health counseling and education was provided in 2021. We helped modify risk factors that can be controlled and taught them what to do when they experienced arrhythmia symptoms such as dizziness, loss of consciousness, palpitations. A balanced diet was recommended, especially potassium-rich foods, to prevent electrolyte imbalance and moderate exercise to prevent cardiovascular problems. Those with blood pressure, blood sugar, and cholesterol level abnormalities were more thoroughly managed through drug treatment. Workers with a QTc interval of 480 ms or more were referred to a cardiologist to receive periodic ECGs and additional tests and moved to work in an area less exposed to antimony.
Furthermore, we instructed workers to switch their protective gear to be more suitable for the work environment and abide by the dress code. Masks were changed to level 1 dust masks, and puncture-resistant gloves and shoes were added to their gear to protect their skin. Contaminated work clothes were now separately stored from everyday clothes, and the workers were advised to wash and change their work clothes periodically. Changes were made to the work environment as well. The workers were instructed to periodically clean the hood, duct, air purifier, and exhaust port of the local exhaust ventilation system. The capture velocity of the external upward-suction-type hood was set above 1.2 m/s to allow for undisturbed ventilation. We made sure that the packaging of the raw materials was sturdy to prevent leaks or being diffused and that workers would go outside during breaks to breathe uncontaminated air. Eating and drinking were prohibited in the workplace, and the possibility of being exposed to dust was minimized by having workers wash their faces before their meals and dusting off before leaving work.
The special health examination in late 2021 showed that the QTc interval of workers B and F decreased while that of workers C and D increased. Worker D, who was referred to a cardiologist, has since been receiving periodic drug treatment and is being closely monitored. No additional ECG abnormalities were found for the other workers.
This case presentation reports the first cases in Korea in which potential cardiac toxicity caused by occupational exposure to antimony was identified. However, data regarding cardiac toxicity caused by antimony exposure are still lacking in Korea; thus, additional studies are needed to identify causal relationships.
Abbreviations
International Conference on Harmonization
Work Environment Measurement
NOTES
-
Funding: This work was supported by the Soonchunhyang University Research Fund and by the Environmental Health Center, Soonchunhyang University Hospital, Gumi, South Korea.
-
Competing interests: The authors declare that they have no competing interests.
-
Author Contributions:
Conceptualization: Jo HR, Yoon S.
Data curation: Jo HR, Kim J, An JM.
Formal analysis: Jo HR, Cho SY.
Investigation: Kim G.
Methodology: Kim G.
Software: Jo HR, Yoon S.
Validation: Kim J.
Writing - original draft: Jo HR, Yoon S, Kim J, An JM.
Writing - review & editing: Jo HR, Cho SY, Yoon S, Kim G.
REFERENCES
REFERENCES
- 1. Tirmenstein MA, Plews PI, Walker CV, Woolery MD, Wey HE, Toraason MA. Antimony-induced oxidative stress and toxicity in cultured cardiac myocytes. Toxicol Appl Pharmacol 1995;130(1):41–47. 7839369.ArticlePubMed
- 2. Krachler M, Zheng J, Koerner R, Zdanowicz C, Fisher D, Shotyk W. Increasing atmospheric antimony contamination in the northern hemisphere: snow and ice evidence from Devon Island, Arctic Canada. J Environ Monit 2005;7(12):1169–1176. 16307068.ArticlePubMed
- 3. Sullivan JB. Hazardous Materials Toxicology–Clinical Principles of Environmental Health. 1st ed. Baltimore, MD, USA: Williams and Wilkins; 1992, 75.
- 4. Tirmenstein MA, Mathias PI, Snawder JE, Wey HE, Toraason M. Antimony-induced alterations in thiol homeostasis and adenine nucleotide status in cultured cardiac myocytes. Toxicology 1997;119(3):203–211. 9152016.ArticlePubMed
- 5. Wey HE, Richards D, Tirmenstein MA, Mathias PI, Toraason M. The role of intracellular calcium in antimony-induced toxicity in cultured cardiac myocytes. Toxicol Appl Pharmacol 1997;145(1):202–210. 9221838.ArticlePubMed
- 6. Toraason M, Wey HE, Richards DE, Mathias PI, Krieg E. Altered Ca2+ mobilization during excitation-contraction in cultured cardiac myocytes exposed to antimony. Toxicol Appl Pharmacol 1997;146(1):104–115. 9299602.ArticlePubMed
- 7. Kuryshev YA, Wang L, Wible BA, Wan X, Ficker E. Antimony-based antileishmanial compounds prolong the cardiac action potential by an increase in cardiac calcium currents. Mol Pharmacol 2006;69(4):1216–1225. 16418337.ArticlePubMed
- 8. Brieger H, Semisch CW 3rd, Stasney J, Piatnek DA. Industrial antimony poisoning. Ind Med Surg 1954;23(12):521–523. 13211006.PubMed
- 9. Klucik I, Ulrich L. Electrocardiographic examination of workers in an antimony plant. Prac Lek 1960;12:236–243. 14409994.PubMed
- 10. Schnorr TM, Steenland K, Thun MJ, Rinsky RA. Mortality in a cohort of antimony smelter workers. Am J Ind Med 1995;27(5):759–770. 7611310.ArticlePubMed
- 11. Honey M. The effects of sodium antimony tartrate on the myocardium. Br Heart J 1960;22(5):601–616. 13715657.ArticlePubMedPMC
- 12. Alvarez M, Malécot CO, Gannier F, Lignon JM. Antimony-induced cardiomyopathy in guinea-pig and protection by L-carnitine. Br J Pharmacol 2005;144(1):17–27. 15644865.PubMed
- 13. Rautaharju PM, Surawicz B, Gettes LS, Bailey JJ, Childers R, Deal BJ, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part IV: the ST segment, T and U waves, and the QT interval: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society . Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 2009;53(11):982–991. 19281931.PubMed
- 14. Kim KW, Choi BS, Kang SK, Seo KB, Lee JS, Cho YS, Chung HK. A study on the urine antimony concentration of workers exposed to antimony trioxide. Proceedings of 45th Meeting of Korean Society for Preventive Medicine; 1993 Oct 1; Seoul. Seoul: Korean Society for Preventive Medicine; 1993;p. 199–200.
- 15. Stevenson CJ. Antimony spots. Trans St Johns Hosp Dermatol Soc 1965;51(1):40–48. 4220643.PubMed
- 16. Nielsen JB, Graff C, Rasmussen PV, Pietersen A, Lind B, Olesen MS, et al. Risk prediction of cardiovascular death based on the QTc interval: evaluating age and gender differences in a large primary care population. Eur Heart J 2014;35(20):1335–1344. 24603310.ArticlePubMedPMC
- 17. Gupta A, Lawrence AT, Krishnan K, Kavinsky CJ, Trohman RG. Current concepts in the mechanisms and management of drug-induced QT prolongation and torsade de pointes. Am Heart J 2007;153(6):891–899. 17540188.ArticlePubMed
- 18. Yap YG, Camm AJ. Drug induced QT prolongation and torsades de pointes. Heart 2003;89(11):1363–1372. 14594906.ArticlePubMedPMC
- 19. Gerhardsson L, Brune D, Nordberg GF, Wester PO. Antimony in lung, liver and kidney tissue from deceased smelter workers. Scand J Work Environ Health 1982;8(3):201–208. 7156939.ArticlePubMed
- 20. Newton PE, Bolte HF, Daly IW, Pillsbury BD, Terrill JB, Drew RT, et al. Subchronic and chronic inhalation toxicity of antimony trioxide in the rat. Fundam Appl Toxicol 1994;22(4):561–576. 8056203.ArticlePubMed
- 21. Frustaci A, Magnavita N, Chimenti C, Caldarulo M, Sabbioni E, Pietra R, et al. Marked elevation of myocardial trace elements in idiopathic dilated cardiomyopathy compared with secondary cardiac dysfunction. J Am Coll Cardiol 1999;33(6):1578–1583. 10334427.ArticlePubMed
- 22. Guo J, Su L, Zhao X, Xu Z, Chen G. Relationships between urinary antimony levels and both mortalities and prevalence of cancers and heart diseases in general US population, NHANES 1999-2010. Sci Total Environ 2016;571:452–460. 27396316.ArticlePubMed
- 23. Schildroth S, Osborne G, Smith AR, Yip C, Collins C, Smith MT, et al. Occupational exposure to antimony trioxide: a risk assessment. Occup Environ Med 2020;78(6):413–418.ArticlePubMedPMC
- 24. Kim KW, Choi BS, Kang SK, Kim HY, Park SS, Cho YS, et al. Assessment of workers’ exposure to antimony trioxide in Korea. J Occup Health 1997;39(4):345–348.ArticlePDF
 , Seongyong Yoon
, Seongyong Yoon , Jinseok Kim
, Jinseok Kim , Seong-yong Cho
, Seong-yong Cho , Jong-min An
, Jong-min An , Gayoung Kim
, Gayoung Kim

 KSOEM
KSOEM

 Cite
Cite

