Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 33; 2021 > Article
- Original Article Association between sleep disturbance and occupational injury among Korean employees
-
Jongwoo Lee1
 , Seong-Sik Cho2,3
, Seong-Sik Cho2,3 , JungIl Kim2
, JungIl Kim2 , Mo-yeol Kang4
, Mo-yeol Kang4 , Suhwan Ju1
, Suhwan Ju1 , Byoung Gwon Kim2
, Byoung Gwon Kim2 , Young Seoub Hong3
, Young Seoub Hong3
-
Annals of Occupational and Environmental Medicine 2021;33:e29.
DOI: https://doi.org/10.35371/aoem.2021.33.e29
Published online: September 10, 2021
1Department of Occupational and Environmental Medicine, Dong-A University Hospital, Busan, Korea.
2Department of Occupational and Environmental Medicine, College of Medicine, Dong-A University, Busan, Korea.
3Department of Preventive Medicine, College of Medicine, Dong-A University, Busan, Korea.
4Department of Occupational and Environmental Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- Correspondence: Seong-Sik Cho. Department of Occupational and Environmental Medicine, Dong-A University Hospital, College of Medicine, Dong-A University, 32 Daesingongwon-ro, Seo-gu, Busan 49201, Korea. sscho@dau.ac.kr
Copyright © 2021 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background Occupational injury has been a serious social problem steadily. Sleep disturbance is a risk factor for occupational injury. However, there were few researches studied on the linking between sleep disturbance and occupational injury in general working population of Korea. Therefore, we explored the association between sleep disturbance and occupational injury among Korean workers.
-
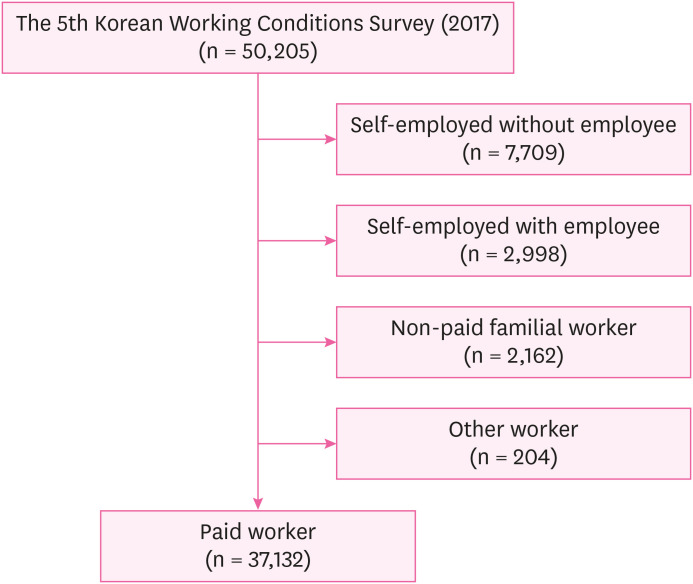
Methods This study used data from the 5th Korean Working Conditions Survey. Occupational injury was assessed by asking work related injury for 12 months prior to the point of the survey. Sleep disturbance was assessed using the Minimal Insomnia Symptoms Scale (MISS). To analyze the association between sleep disturbance and occupational injury, multiple logistic regression analysis was conducted.
-
Results The odds ratio (OR) of sleep disturbance group for occupational injury was 2.57 (95% confidence interval [CI]: 1.68–3.93) in the fully adjusted model. For the association between MISS score and occupational injury, it showed increasing trend that ORs increase from the 1st to the 4th quartiles. The OR of 2nd quartile was 1.10 (95% CI: 0.60–2.01), the OR of 3rd quartile was 2.27 (95% CI: 1.53–3.38) and the OR of 4th quartile was 2.80 (95% CI: 1.84–4.26).
-
Conclusions Sleep disturbance was associated with occupational injury. In addition, increasing trend was observed between MISS score and occupational injury. These findings imply that developing of intervention programs to manage sleep disturbance and fatigue may be necessary to prevent occupational injury.
BACKGROUND
METHOD
Sleep disturbance
Occupational injury
Covariates
RESULTS
Characteristics of the study population by sleep disturbance
Occupational injury and related factors
Association between sleep disturbance and occupational injury by subgroups
Association between sleep disturbance and occupational injury by logistic regression analysis
Association between sleep-related symptoms and occupational injury by logistic regression analysis
DISCUSSION
CONCLUSIONS
ACKNOWLEDGEMENTS
-
Funding: This research is supported by national research fund of Korea (NRF-2021R1C1C1007796).
-
Competing interests: The authors declare that they have no competing interest.
-
Author contributions:
NOTES
- 1. Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Basta M, et al. Insomnia with short sleep duration and mortality: the Penn State cohort. Sleep 2010;33(9):1159–1164. 20857861.ArticlePubMedPMC
- 2. Rod NH, Vahtera J, Westerlund H, Kivimaki M, Zins M, Goldberg M, et al. Sleep disturbances and cause-specific mortality: results from the GAZEL cohort study. Am J Epidemiol 2011;173(3):300–309. 21193534.ArticlePubMedPMC
- 3. Yaggi HK, Araujo AB, McKinlay JB. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care 2006;29(3):657–661. 16505522.ArticlePubMedPDF
- 4. Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG, et al. Sleep duration as a risk factor for diabetes incidence in a large U.S. sample. Sleep 2007;30(12):1667–1673. 18246976.ArticlePubMedPMC
- 5. Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care 2011;14(4):402–412. 21659802.ArticlePubMedPMC
- 6. Panossian LA, Veasey SC. Daytime sleepiness in obesity: mechanisms beyond obstructive sleep apnea--a review. Sleep (Basel) 2012;35(5):605–615.ArticlePubMedPMC
- 7. Morin CM, Bélanger L, LeBlanc M, Ivers H, Savard J, Espie CA, et al. The natural history of insomnia: a population-based 3-year longitudinal study. Arch Intern Med 2009;169(5):447–453. 19273774.ArticlePubMed
- 8. McCall WV. A psychiatric perspective on insomnia. J Clin Psychiatry 2001;62(Suppl 10):27–32.
- 9. Broman JE, Smedje H, Mallon L, Hetta J. The Minimal Insomnia Symptom Scale (MISS): a brief measure of sleeping difficulties. Ups J Med Sci 2008;113(2):131–142. 18509808.PubMed
- 10. Vallières A, Azaiez A, Moreau V, LeBlanc M, Morin CM. Insomnia in shift work. Sleep Med 2014;15(12):1440–1448. 25277664.ArticlePubMed
- 11. Chung S, Cho SW, Jo MW, Youn S, Lee J, Sim CS. The prevalence and incidence of insomnia in Korea during 2005 to 2013. Psychiatry Investig 2020;17(6):533–540.ArticlePubMedPMCPDF
- 12. Korea Occupational Safety and Health Agency. Occurrence of industrial accidents in 2019. Updated 2020]. Accessed May 28, 2021]. https://www.kosha.or.kr/kosha/data/industrialAccidentStatus.do?mode=view&boardNo=229&articleNo=412099&attachNo= .
- 13. Survey on industrial accident coverage and direction of improvement of system: 2014 state audit and processing results evaluation report 2015-3. Updated 2015]. Accessed July 13, 2021]. https://www.nars.go.kr/report/view.do?cmsCode=CM0018&brdSeq=17121 .
- 14. Wilkins K, Mackenzie SG. Work injuries. Health Rep 2007;18(3):25–42. 17892250.PubMed
- 15. Kachan D, Fleming LE, LeBlanc WG, Goodman E, Arheart KL, Caban-Martinez AJ, et al. Worker populations at risk for work-related injuries across the life course. Am J Ind Med 2012;55(4):361–366. 22170632.ArticlePubMedPMC
- 16. Shi J, Wheeler KK, Lu B, Bishai DM, Stallones L, Xiang H. Medical expenditures associated with nonfatal occupational injuries among U.S. workers reporting persistent disabilities. Disabil Health J 2015;8(3):397–406. 25573252.ArticlePubMed
- 17. Salminen S, Oksanen T, Vahtera J, Sallinen M, Härmä M, Salo P, et al. Sleep disturbances as a predictor of occupational injuries among public sector workers. J Sleep Res 2010;19(1 Pt 2):207–213. 19840241.ArticlePubMed
- 18. Chau N, Mur JM, Touron C, Benamghar L, Dehaene D. Correlates of occupational injuries for various jobs in railway workers: a case-control study. J Occup Health 2004;46(4):272–280. 15308826.ArticlePubMedPDF
- 19. Uehli K, Mehta AJ, Miedinger D, Hug K, Schindler C, Holsboer-Trachsler E, et al. Sleep problems and work injuries: a systematic review and meta-analysis. Sleep Med Rev 2014;18(1):61–73. 23702220.ArticlePubMed
- 20. Hyun SH. Associations between working conditions and occupational injury of Korean employees. J Digit Converg 2018;16(12):523–531.
- 21. Shin DS. Characteristics of taxi, bus and truck drivers in industrial and traffic accidents databases, and sleep disorder and depression in working conditions survey [dissertation]. Seoul, Korea: Hansung University; 2019.
- 22. Shin SH, Kim DH, Ahn JH, Kim HD, Kim JH, Kang HM, et al. Factors associated with occupational injuries of ship-building supply workers in Busan. Korean J Occup Environ Med 2008;20(1):15–24.ArticlePDF
- 23. Grandner MA. Sleep and Health. Oxford, UK: Academic Press; 2019.
- 24. Occupational Safety and Health Research Institute. User guide of raw data for the 5the Korean Working Conditions Survey. Updated 2017]. Accessed May 27, 2021]. https://oshri.kosha.or.kr/eoshri/resources/KWCSDownload.do .
- 25. Rosekind MR, Gregory KB, Mallis MM, Brandt SL, Seal B, Lerner D. The cost of poor sleep: workplace productivity loss and associated costs. J Occup Environ Med 2010;52(1):91–98. 20042880.ArticlePubMed
- 26. Goel N, Rao H, Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Semin Neurol 2009;29(4):320–339. 19742409.ArticlePubMedPMC
- 27. Chau N, Mur JM, Benamghar L, Siegfried C, Dangelzer JL, Français M, et al. Relationships between certain individual characteristics and occupational injuries for various jobs in the construction industry: a case-control study. Am J Ind Med 2004;45(1):84–92. 14691972.ArticlePubMed
- 28. Gauchard GC, Mur JM, Touron C, Benamghar L, Dehaene D, Perrin P, et al. Determinants of accident proneness: a case-control study in railway workers. Occup Med (Lond) 2006;56(3):187–190. 16452131.ArticlePubMed
- 29. Lavie P, Kremerman S, Wiel M. Sleep disorders and safety at work in industry workers. Accid Anal Prev 1982;14(4):311–314.Article
- 30. Pérez-Chada D, Videla AJ, O'Flaherty ME, Palermo P, Meoni J, Sarchi MI, et al. Sleep habits and accident risk among truck drivers: a cross-sectional study in Argentina. Sleep 2005;28(9):1103–1108. 16268379.ArticlePubMed
- 31. Hägg SA, Torén K, Lindberg E. Role of sleep disturbances in occupational accidents among women. Scand J Work Environ Health 2015;41(4):368–376. 25830787.ArticlePubMed
- 32. AlGhanim N, Comondore VR, Fleetham J, Marra CA, Ayas NT. The economic impact of obstructive sleep apnea. Lung 2008;186(1):7–12. 18066623.ArticlePubMedPDF
- 33. Hirsch Allen AJ, Peres B, Ayas NT. Obstructive sleep apnea severity and the risk of occupational injury: a prospective observational cohort. Lung 2020;198(2):283–287. 31965242.ArticlePubMedPDF
- 34. Robb G, Sultana S, Ameratunga S, Jackson R. A systematic review of epidemiological studies investigating risk factors for work-related road traffic crashes and injuries. Inj Prev 2008;14(1):51–58. 18245316.ArticlePubMed
- 35. Connor J, Whitlock G, Norton R, Jackson R. The role of driver sleepiness in car crashes: a systematic review of epidemiological studies. Accid Anal Prev 2001;33(1):31–41. 11189120.ArticlePubMed
- 36. Bayon V, Léger D, Philip P. Socio-professional handicap and accidental risk in patients with hypersomnias of central origin. Sleep Med Rev 2009;13(6):421–426. 19493688.ArticlePubMed
- 37. Stevenson MR, Elkington J, Sharwood L, Meuleners L, Ivers R, Boufous S, et al. The role of sleepiness, sleep disorders, and the work environment on heavy-vehicle crashes in 2 Australian states. Am J Epidemiol 2014;179(5):594–601. 24352592.ArticlePubMed
- 38. Chen GX, Fang Y, Guo F, Hanowski RJ. The influence of daily sleep patterns of commercial truck drivers on driving performance. Accid Anal Prev 2016;91:55–63. 26954762.ArticlePubMedPMC
- 39. Ward KL, Hillman DR, James A, Bremner AP, Simpson L, Cooper MN, et al. Excessive daytime sleepiness increases the risk of motor vehicle crash in obstructive sleep apnea. J Clin Sleep Med 2013;9(10):1013–1021. 24127145.ArticlePubMedPMC
- 40. Anund A, Fors C, Kecklund G, van Leeuwen W, Åkerstedt T. Countermeasures for Fatigue in Transportation: a Review of Existing Methods for Drivers on Road, Rail, Sea and in Aviation. Linköping, Sweden: Swedish National Road and Transport Research Institute; 2015.
- 41. European Aviation Safety Agency. Notice of Proposed Amendment (NPA) No 2009-02d. Implementing rules for air operations of community operators. Updated 2009]. Accessed May 28, 2021]. http://easa.europa.eu/rulemaking/docs/npa/2009/NPA%202009-02D.pdf .
- 42. Hersman DA, Whitcomb EA. Fatigue risk management in high-risk environments: a call to action. Prehosp Emerg Care 2018;22(sup1):1–2.Article
- 43. Sullivan JP, O'Brien CS, Barger LK, Rajaratnam SM, Czeisler CA, Lockley SW. Randomized, prospective study of the impact of a sleep health program on firefighter injury and disability. Sleep 2017;40(1):zsw001.ArticlePubMedPMC
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Exploring β-caryophyllene: a non-psychotropic cannabinoid's potential in mitigating cognitive impairment induced by sleep deprivation
Cher Ryn Lim, Satoshi Ogawa, Yatinesh Kumari
Archives of Pharmacal Research.2025; 48(1): 1. CrossRef - Do work stress and sleep problems mediate the link between occupational injury and psychological distress? Evidence from a cross-sectional study of Ghanaian small-scale miners
Emmanuel Nyaaba, Pius W. Kudeto, Vanessa F. Epis, Patrick Azong
Geopsychiatry.2025; 2: 100023. CrossRef - Sleep Disturbance Among Workers: Interaction and Mediation of Job Satisfaction and Social Support
Jian Lee, Jongmin Lee, Juyeon Oh, Hyejin Kim, Subin Kim, Heejoo Park, Juho Sim, Byungyoon Yun, Jin-Ha Yoon
Journal of Korean Medical Science.2025;[Epub] CrossRef - The role of sleep disorder and disturbance in the occurrence of occupational injuries among industry workers in Ethiopia: A systematic review and meta-analysis
Anmut Endalkachew Bezie, Asmare Asrat Yirdaw, Eyob Tilahun Abeje, Lamrot Yohannes, Giziew Abere, Awoke Keleb
Sage Open Medicine.2025;[Epub] CrossRef - The changing dynamics of work from home and its association with sleep disturbance through work–family conflict during the COVID-19 pandemic
Jaehyuk Jung, Jiyoung Lim, Yong Hyuk Cho, Jae Bum Park, Inchul Jeong
Journal of Occupational Health.2024;[Epub] CrossRef - Sleep quality and hypertension in an indigenous African population: a cross-sectional investigation from the COMBAT-CVDs study
Oluwafemi Gbolahan Aremu, Osahon Jeffery Asowata, David Kadan Danladi, Akinkunmi Paul Okekunle, Onoja Matthew Akpa
Journal of Human Hypertension.2024;[Epub] CrossRef - Exploring Clinical Trials to Manage Firefighters’ Sleep Quality: A PRISMA Compliant Systematic Review
Sara Alves, Josiana Vaz, Adília Fernandes
International Journal of Environmental Research and Public Health.2023; 20(5): 3862. CrossRef - Economic costs and Predictors of occupation-related Injuries in Ethiopian sugar industries from the Employer’s perspective: top-down approach and friction method
Mitiku Bonsa Debela, Muluken Azage, Negussie Deyessa, Achenef Motbainor Begosaw
BMC Public Health.2022;[Epub] CrossRef - Changes in the Health Indicators of Hospital Medical Residents During the Four-Year Training Period in Korea
Ji-Sung Ahn, Seunghyeon Cho, Won-Ju Park
Journal of Korean Medical Science.2022;[Epub] CrossRef - Shiftwork Is Associated with Higher Food Insecurity in U.S. Workers: Findings from a Cross-Sectional Study (NHANES)
Maximilian Andreas Storz, Gianluca Rizzo, Mauro Lombardo
International Journal of Environmental Research and Public Health.2022; 19(5): 2847. CrossRef
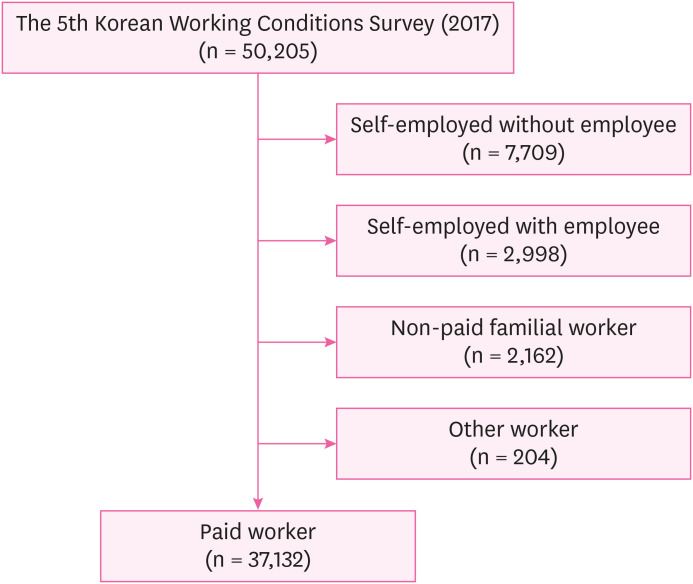
Fig. 1
| Characteristics | Total | Sleep disturbance (−)a | Sleep disturbance (+)a | |
|---|---|---|---|---|
| Sex | ||||
| Male | 21,083 (56.8) | 19,747 (93.7) | 1,336 (6.3) | |
| Female | 16,037 (43.2) | 14,881 (92.8) | 1,156 (7.2) | |
| Age | ||||
| 15–39 | 16,160 (43.5) | 15,167 (93.9) | 993 (6.1) | |
| 40–49 | 9,386 (25.2) | 8,763 (93.4) | 624 (6.6) | |
| 50–59 | 7,450 (20.0) | 6,879 (92.3) | 571 (7.7) | |
| ≥ 60 | 4,124 (11.1) | 3,820 (92.6) | 304 (7.4) | |
| Education | ||||
| College or higher | 22,306 (60.1) | 20,923 (93.8) | 1,382 (6.2) | |
| High school | 11,575 (31.2) | 10,706 (92.5) | 869 (7.5) | |
| Middle school or lower | 3,209 (8.7) | 2,970 (92.6) | 239 (7.5) | |
| Income | ||||
| Lowest | 7,277 (20.9) | 6,774 (93.1) | 503 (6.9) | |
| Low middle | 8,153 (23.4) | 7,576 (92.9) | 577 (7.1) | |
| High middle | 9,463 (27.2) | 8,914 (94.2) | 549 (5.8) | |
| Highest | 9,909 (28.5) | 9,292 (93.8) | 617 (6.2) | |
| Employment status | ||||
| Regular | 30,063 (81.0) | 28,056 (93.3) | 2,007 (6.7) | |
| Temporary | 5,132 (13.8) | 4,767 (92.9) | 364 (7.1) | |
| Daily | 1,926 (5.2) | 1,805 (93.7) | 121 (6.3) | |
| Occupation | ||||
| Professional & managerial | 8,797 (23.8) | 8,249 (93.8) | 548 (6.2) | |
| Clerical | 9,061 (24.5) | 8,517 (94.0) | 544 (6.0) | |
| Sales & service | 7,479 (20.2) | 6,913 (92.4) | 566 (7.6) | |
| Manual | 11,664 (31.5) | 10,839 (92.9) | 825 (7.1) | |
| Weekly working hours | ||||
| 1–34 | 3,857 (10.4) | 3,586 (93.0) | 271 (7.0) | |
| 35–40 | 18,168 (48.9) | 17,115 (94.2) | 1,053 (5.8) | |
| 41–52 | 10,146 (27.3) | 9,419 (92.8) | 727 (7.2) | |
| 53–60 | 3,647 (9.8) | 3,355 (92.0) | 293 (8.0) | |
| ≥ 61 | 1,301 (3.5) | 1,154 (88.7) | 147 (11.3) | |
| Shift work | ||||
| No | 32,715 (88.2) | 30,616 (93.6) | 2,099 (6.4) | |
| Yes | 4,394 (11.8) | 4,002 (91.1) | 391 (8.9) | |
| Perceived risk at work | ||||
| Risk (−) | 33,050 (89.1) | 30,906 (93.5) | 2,144 (6.5) | |
| Risk (+) | 4,028 (10.9) | 3,681 (91.4) | 346 (8.6) | |
| Factors | Occupational injury (−) | Occupational injury (+) | |
|---|---|---|---|
| Sleep disturbancea | |||
| (−) | 34,298 (99.1) | 322 (0.9) | |
| (+) | 2,433 (97.7) | 56 (2.3) | |
| MISS scoreb | |||
| 1Q | 18,264 (99.4) | 103 (0.6) | |
| 2Q | 4,399 (99.3) | 32 (0.7) | |
| 3Q | 8,288 (98.4) | 137 (1.6) | |
| 4Q | 5,781 (98.2) | 106 (1.8) | |
| Difficulty falling asleep | |||
| (−) | 35,053 (99.0) | 362 (1.0) | |
| (+) | 1,687 (99.1) | 16 (0.9) | |
| Waking up repeatedly during the sleep | |||
| (−) | 35,345 (99.0) | 341 (1.0) | |
| (+) | 1,393 (97.4) | 38 (2.6) | |
| Waking up with a feeling of exhaustion and fatigue | |||
| (−) | 35,306 (99.1) | 336 (0.9) | |
| (+) | 1,428 (97.1) | 42 (2.9) | |
| Sex | |||
| Female | 20,784 (98.6) | 297 (1.4) | |
| Male | 15,959 (99.5) | 81 (5.0) | |
| Age | |||
| 15–39 | 16,044 (92.3) | 118 (7.3) | |
| 40–49 | 9,268 (98.7) | 121 (1.3) | |
| 50–59 | 7,362 (98.8) | 87 (1.2) | |
| ≥ 60 | 4,069 (98.7) | 52 (1.3) | |
| Education | |||
| College or higher | 22,151 (99.3) | 163 (0.7) | |
| High school | 11,410 (98.6) | 160 (1.4) | |
| Middle school or lower | 3,151 (98.3) | 54 (1.7) | |
| Income | |||
| Lowest | 7,227 (99.3) | 48 (6.6) | |
| Low middle | 8,082 (99.2) | 68 (8.4) | |
| High middle | 9,357 (98.9) | 107 (1.1) | |
| Highest | 9,781 (98.7) | 128 (1.3) | |
| Employment status | |||
| Regular | 29,787 (99.1) | 279 (0.9) | |
| Temporary | 5,087 (99.1) | 45 (0.9) | |
| Daily | 1,869 (97.2) | 54 (2.8) | |
| Occupation | |||
| Professional & managerial | 8,744 (99.4) | 57 (0.6) | |
| Clerical | 9,041 (99.8) | 22 (0.2) | |
| Sales & service | 7,417 (99.2) | 60 (0.8) | |
| Manual | 11,423 (98.0) | 239 (2.0) | |
| Weekly working hours | |||
| 1–34 | 3,836 (99.5) | 21 (5.4) | |
| 35–40 | 18,048 (99.3) | 127 (0.7) | |
| 41–52 | 10,029 (98.9) | 111 (1.1) | |
| 53–60 | 3,571 (97.9) | 77 (2.1) | |
| ≥ 60 | 1,259 (96.7) | 42 (3.3) | |
| Shift work | |||
| No | 32,390 (99.0) | 325 (1.0) | |
| Yes | 4,345 (98.9) | 49 (1.1) | |
| Company size | |||
| 1–4 | 7,220 (99.2) | 57 (0.8) | |
| 5–49 | 17,133 (98.9) | 197 (1.1) | |
| 50–499 | 7,323 (99.1) | 67 (0.9) | |
| ≥ 500 | 4,803 (99.0) | 48 (1.0) | |
| Working hours type | |||
| Full-time | 32,523 (98.9) | 346 (1.1) | |
| Part-time | 4,197 (99.2) | 32 (0.8) | |
| Sleep disturbancea | Total | Occupational injury (−) | Occupational injury (+) | OR (95% CI) | ||
|---|---|---|---|---|---|---|
| Sex | ||||||
| Male | (−) | 19,743 (93.7) | 19,486 (98.7) | 256 (1.3) | 1 | |
| (+) | 1,334 (6.3) | 1,293 (96.9) | 41 (3.1) | 2.40 (1.47–3.92) | ||
| Female | (−) | 14,877 (92.8) | 14,812 (99.6) | 65 (0.4) | 1 | |
| (+) | 1,156 (7.2) | 1,140 (98.7) | 16 (1.4) | 3.10 (1.60–6.01) | ||
| Age | ||||||
| 15–39 | (−) | 15,165 (93.9) | 15,077 (99.4) | 88 (0.6) | 1 | |
| (+) | 991 (6.1) | 961 (97.0) | 30 (3.0) | 5.30 (2.84–9.87) | ||
| 40–49 | (−) | 8,760 (93.4) | 8,645 (98.7) | 115 (1.3) | 1 | |
| (+) | 624 (6.6) | 617 (99.0) | 7 (1.0) | 0.79 (0.27–2.35) | ||
| 50–59 | (−) | 6,878 (92.3) | 6,800 (98.9) | 78 (1.1) | 1 | |
| (+) | 571 (7.7) | 562 (98.4) | 9 (1.6) | 1.43 (0.33–3.08) | ||
| ≥ 60 | (−) | 3,817 (92.6) | 3,777 (98.9) | 41 (1.1) | 1 | |
| (+) | 304 (7.3) | 293 (96.4) | 11 (3.6) | 3.50 (1.33–9.25) | ||
| Employment status | ||||||
| Regular | (−) | 28,052 (93.3) | 27,814 (99.2) | 238 (0.8) | 1 | |
| (+) | 2,004 (6.7) | 1,963 (98.0) | 41 (2.0) | 2.43 (1.49–3.96) | ||
| Temporary | (−) | 4,765 (92.9) | 4,729 (99.2) | 36 (0.8) | 1 | |
| (+) | 364 (7.1) | 355 (97.5) | 9 (2.5) | 3.32 (1.25–8.86) | ||
| Daily | (−) | 1,802 (93.7) | 1,755 (97.4) | 48 (2.6) | 1 | |
| (+) | 121 (6.3) | 114 (94.6) | 7 (5.4) | 2.12 (0.83–5.43) | ||
| Occupation | ||||||
| Professional & managerial | (−) | 8,249 (93.8) | 8,206 (99.5) | 43 (0.5) | 1 | |
| (+) | 545 (6.2) | 532 (97.5) | 13 (2.5) | 4.75 (1.83–12.40) | ||
| Clerical | (−) | 8,515 (94.0) | 8,495 (99.8) | 20 (0.2) | 1 | |
| (+) | 544 (6.0) | 541 (99.5) | 3 (0.5) | 2.18 (0.45–10.68) | ||
| Sales & service | (−) | 7,416 (99.2) | 6,854 (99.2) | 562 (99.2) | 1 | |
| (+) | 60 (0.8) | 56 (0.8) | 4 (0.8) | 0.96 (0.33–2.83) | ||
| Manual | (−) | 10,835 (92.9) | 10,632 (98.1) | 203 (1.9) | 1 | |
| (+) | 825 (7.1) | 789 (95.6) | 36 (4.4) | 2.39 (1.44–3.94) | ||
| Weekly working hours | ||||||
| 1–34 | (−) | 3,583 (92.9) | 3,569 (99.6) | 14 (0.4) | 1 | |
| (+) | 271 (7.0) | 265 (97.6) | 7 (2.4) | 6.18 (2.08–18.35) | ||
| 35–40 | (−) | 17,113 (94.2) | 16,999 (99.3) | 114 (0.7) | 1 | |
| (+) | 1,053 (5.8) | 1,040 (98.8) | 12 (1.2) | 1.77 (0.85–3.70) | ||
| 41–52 | (−) | 9,414 (92.8) | 9,323 (99.0) | 92 (1.0) | 1 | |
| (+) | 725 (7.2) | 706 (97.4) | 19 (2.6) | 2.71 (1.27–5.77) | ||
| 53–60 | (−) | 3,355 (92.0) | 3,288 (98.0) | 67 (2.0) | 1 | |
| (+) | 293 (8.0) | 283 (96.5) | 10 (3.5) | 1.77 (0.71–4.40) | ||
| ≥ 61 | (−) | 1,154 (88.7) | 1,120 (97.1) | 34 (2.9) | 1 | |
| (+) | 147 (11.3) | 139 (94.3) | 8 (5.7) | 2.01 (0.66–6.13) | ||
| Shift work | ||||||
| No | (−) | 30,608 (93.6) | 30,324 (99.1) | 284 (0.9) | 1 | |
| (+) | 2,096 (6.4) | 2,055 (98.0) | 41 (2.0) | 2.15 (1.36–3.39) | ||
| Yes | (−) | 4,002 (91.0) | 3,967 (99.1) | 35 (0.9) | 1 | |
| (+) | 391 (8.9) | 378 (96.6) | 13 (3.4) | 3.96 (1.61–9.75) | ||
| Company size | ||||||
| 1–4 | (−) | 6,732 (92.5) | 6,681 (99.2) | 51 (0.8) | 1 | |
| (+) | 542 (7.5) | 536 (98.9) | 6 (1.1) | 1.48 (0.45–4.84) | ||
| 5–49 | (−) | 16,150 (93.2) | 15,985 (99.0) | 165 (1.0) | 1 | |
| (+) | 1,175 (6.8) | 1,143 (97.2) | 33 (2.8) | 2.76 (1.64–4.65) | ||
| 50–499 | (−) | 6,927 (93.7) | 6,868 (99.1) | 59 (0.9) | 1 | |
| (+) | 462 (6.3) | 455 (98.4) | 8 (1.6) | 1.92 (0.67–5.51) | ||
| ≥ 500 | (−) | 4,575 (94.4) | 4,537 (99.2) | 39 (0.8) | 1 | |
| (+) | 271 (5.6) | 262 (96.7) | 9 (33.0) | 4.01 (1.28–12.53) | ||
| Variables | Total | Occupational injury (−) | Occupational injury (+) | Unadjusted | Model 1a | Model 2b | Model 3c | |
|---|---|---|---|---|---|---|---|---|
| No. (%: column percent) | No. (%: row percent) | No. (%: row percent) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Sleep disturbanced | ||||||||
| (−) | 34,620 (93.3) | 34,298 (99.1) | 322 (0.9) | 1 | 1 | 1 | 1 | |
| (+) | 2,489 (6.7) | 2,433 (97.7) | 56 (2.3) | 2.47 (1.66–3.69) | 2.91 (1.93–4.39) | 2.72 (1.79–4.12) | 2.57 (1.68–3.93) | |
| MISS scoree | ||||||||
| 1Q | 18,367 (49.5) | 18,264 (99.4) | 103 (0.6) | 1 | 1 | 1 | 1 | |
| 2Q | 4,430 (11.9) | 4,399 (99.3) | 32 (0.7) | 1.28 (0.72–2.28) | 1.27 (1.81–2.29) | 1.23 (0.68–2.23) | 1.10 (0.60–2.01) | |
| 3Q | 8,425 (22.7) | 8,288 (98.4) | 137 (1.6) | 2.93 (2.00–4.28) | 2.68 (1.81–3.97) | 2.61 (1.76–3.87) | 2.27 (1.53–3.38) | |
| 4Q | 5,887 (15.9) | 5,781 (98.2) | 106 (1.8) | 3.26 (2.19–4.86) | 3.39 (2.24–5.12) | 3.14 (2.07–4.77) | 2.80 (1.84–4.26) | |
| Sleep-related symptoms | Total | Occupational injury (−) | Occupational injury (+) | Unadjusted | Model 1a | Model 2b | Model 3c | |
|---|---|---|---|---|---|---|---|---|
| No. (%: column percent) | No. (%: row percent) | No. (%: row percent) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | ||
| Difficulty falling asleep | ||||||||
| (−) | 35,415 (95.4) | 35,053 (99.0) | 362 (1.0) | 1 | 1 | 1 | 1 | |
| (+) | 1,702 (4.6) | 1,687 (99.1) | 16 (0.9) | 0.91 (0.45–1.82) | 1.09 (0.54–2.22) | 1.09 (0.54–2.21) | 1.15 (0.57–2.35) | |
| Waking up repeatedly during sleep | ||||||||
| (−) | 35,685 (96.1) | 35,345 (99.0) | 341 (1.0) | 1 | 1 | 1 | 1 | |
| (+) | 1,430 (3.9) | 1,393 (97.4) | 38 (2.6) | 2.80 (1.68–4.67) | 3.41 (2.01–5.77) | 3.33 (1.96–5.67) | 3.28 (1.92–5.62) | |
| Waking up with a feeling of exhaustion and fatigue | ||||||||
| (−) | 35,641 (96.0) | 35,306 (99.1) | 336 (0.9) | 1 | 1 | 1 | 1 | |
| (+) | 1,470 (4.0) | 1,428 (97.1) | 42 (2.9) | 3.13 (2.04–4.79) | 3.19 (2.06–4.94) | 3.03 (1.96–4.68) | 2.64 (1.69–4.11) | |
Values are presented as number (%: row percent).
aPatients with ≥ 6 points were considered to have sleep disturbance and those with < 6 points were considered to have normal sleep using the Minimal Insomnia Symptoms Scale (MISS).
Values are presented as number (%).
aPatients with ≥ 6 points were considered to have sleep disturbance and those with < 6 points were considered to have normal sleep using the Minimal Insomnia Symptoms Scale (MISS).
bMISS score was categorized into quartiles as follows (1st quartile:1 point; 2nd quartile: 2 points; 3rd quartile: 3–4 points; and 4th quartile: > 4 points).
MISS: Minimal Insomnia Symptoms Scale.
ORs are estimated by univariable logistic regression analysis.
OR: odds ratio; CI: confidence interval.
aPatients with ≥ 6 points were considered to have sleep disturbance and those with < 6 points were considered to have normal sleep using the Minimal Insomnia Symptoms Scale (MISS).
OR: odds ratio; CI: confidence interval; MISS: Minimal Insomnia Symptoms Scale.
aModel 1: adjusted for age, sex, education, income, occupation, and employment status. bModel 2: adjusted for age, sex, education, income, occupation, employment status, shift work, and working hours. cModel 3: adjusted for age, sex, education, income, occupation, employment status, shift work, working hours, and perceived risk at work. dPatients with ≥ 6 points were considered to have sleep disturbance and those with < 6 points were considered to have normal sleep using the Minimal Insomnia Symptoms Scale (MISS). eMISS score was categorized into quartiles as follows (1st quartile:1 point; 2nd quartile: 2 points; 3rd quartile: 3–4 points; and 4th quartile: > 4 points).
OR: odds ratio; CI: confidence interval.
aModel 1: adjusted for age, sex, education, income, occupation, and employment status. bModel 2: adjusted for age, sex, education, income, occupation, employment status, shift work, and working hours. cModel 3: adjusted for age, sex, education, income, occupation, employment status, shift work, working hours, and perceived risk at work.
 KSOEM
KSOEM

 Cite
Cite

