Abstract
-
Background
Sunlight exposure is a major risk factor for eye disorders. Most outdoor workers cannot avoid sunlight exposure. This study aimed to analyze the relationship between outdoor sunlight exposure and eye disorders in an economically active population.
-
Methods
This study analyzed the 2008–2012 Korea National Health and Nutritional Examination Survey data. Sunlight exposure was categorized as < 5 hours and > 5 hours. We also analyzed the dose-dependent relationship between exposure to sunlight and eye disorders (cataracts, pterygium, and age-related macular degeneration [AMD]) using data from 2010 to 2012 by subdividing the exposure groups into < 2 hours, 2–5 hours, and ≥ 5 hours. Eye disorders were diagnosed by an ophthalmologist. The study participants were stratified by sex, and the results were analyzed using the χ2 test and multiple logistic regression analysis.
-
Results
In the female group, the odds ratio of pterygium in the high-level sunlight exposure group was 1.47 (95% confidence interval [CI]: 1.15–1.89). Regarding AMD, the odds ratios were 1.42 (95% CI: 1.16–1.73), 1.33 (95% CI: 1.03–1.73), and 1.58 (95% CI: 1.15–2.16) in the total, male, and female groups, respectively. Analysis of the dose-response relationship revealed that the odds ratios of pterygium in the high-level sunlight exposure subgroups of the total and female groups were 1.62 (95% CI: 1.25–2.08) and 2.00 (95% CI: 1.39–2.88), respectively.
-
Conclusions
This study demonstrated a relationship between sunlight exposure and eye disorders in an economically active population. Women were found to be especially vulnerable to pterygium. However, additional prospective studies to clarify the pathophysiology of pterygium are needed.
-
Keywords: Sunlight; Outdoor working condition; Economically active population; Eye disorder; Pterygium; KNHANES
BACKGROUND
Sunlight is an essential energy source for almost all living organisms on Earth. Humans cannot photosynthesize; however, they synthesize vitamin D
1 through sunlight and regulate the circadian rhythm.
2 However, insufficient, or excessive exposure to sunlight can cause heat-related illnesses
3 and disorders of the skin,
4 sleep,
5 mood,
6 and eye.
7,8,9,10,11,12,13,14,15,16,17,18,19,20
Sunlight is electromagnetic radiation from the sun and is composed of ultraviolet (UV), visible light, and infrared (IR) components.
21 Each of these radiations affects the human body via different mechanisms. UV radiation is a major cause of eye disorders. It induces pterygium and photokeratitis in the anterior chamber of the eye
10 and cataract in the lens via photooxidative stress-induced structural changes.
20 Moreover, UV that is not absorbed by the cornea and surrounding structures can reach the retina and cause macular degeneration.
15 Visible light is composed of wavelengths between 400 and 700 nm, and light of wavelengths ≤ 450 nm can induce solar retinopathy.
22 IR causes vibration in the atomic structure and an increase in temperature
21 and is the main cause of body temperature increase following exposure to sunlight. IR can be absorbed by the iris and lens, causing cataractous changes.
23 Furthermore, heat exposure increases the prevalence of heat-related illnesses, injury, death, and urinary, reproductive, and psychological diseases.
24
In her classic,
Little Women,
25 Louisa May Alcott said, “Some people seemed to get all sunshine, and some all shadow.” Some workers, especially those working outdoors, are unable to avoid direct sunlight exposure and can be classified as a vulnerable population.
26,27
Eye disorders are strongly related to quality of life. According to a study
28 using the National Health and Nutrition Examination Survey Data, the economic burden of blindness and eye disorders in the United States for people under the age of 40 was $27.5 billion, and the loss of quality-adjusted life years was reached 215,000.
Cataract is a disease that causes vision impairment due to clouding of the lens. In general, it is known that there is an epidemiological relationship with age, smoking, diabetes, and UV exposure. According to a recent literature review,
29 smoking, diabetes, asthma, cardiovascular disease, and steroid use are particularly associated with the prevalence of cataracts.
Pterygium is a disease in which triangular fibrovascular tissue proliferates from the inner conjunctiva to the cornea, and the generally accepted common risk factor is ultraviolet rays. Mutation of p53, a stress regulator, is the main pathogenesis, and Human papilloma virus infection, which shares the mechanism, is considered risk factor.
30
Age-related macular degeneration (AMD) is macular degeneration with age growth, which is a major factor of vision loss in older populations. Increasing age, smoking status, previous cataract surgery history and AMD family history, overweight, hypertension and cardiovascular disease history are known to be associated with AMD.
31
The health effects of excessive exposure to sunlight in outdoor workers have recently attracted attention.
32 A systematic review of the health effects of heat exposure in outdoor workers has been conducted; however, only a few reports were related to eye disorders.
24 Therefore, although studies have explored the relationship between sunlight exposure and eye disorders, they did not consider sunlight exposure as the main variable and targeted only the general population.
12,15,16,17 These studies were also limited to specific occupations
7,11,33,34 or diseases.
35,36,37
In the present study, we aimed to establish a policy for preventing and protecting eye diseases by identifying their status and characteristics in the economically active population exposed to sunlight outdoors using data from the Korea National Health and Nutrition Examination Survey (KNHANES).
METHODS
Data collection, study design, and participants
This study was based on the KNHANES data. The KNHANES is a series of cross-sectional, representative, population-based annual surveys to assess the health, nutritional status, and prevalence of chronic diseases in the Korean population. It is conducted by the Korea Disease Control and Prevention Agency.
38 The current study used the 2008–2012 KNHANES data, which included general characteristics such as age, sex, household income, occupational classifications, personal lifestyle and disease, outdoor working conditions, and ophthalmic examinations. This study focused on an economically active population that included wage workers, self-employed workers, employers, and unpaid family workers.
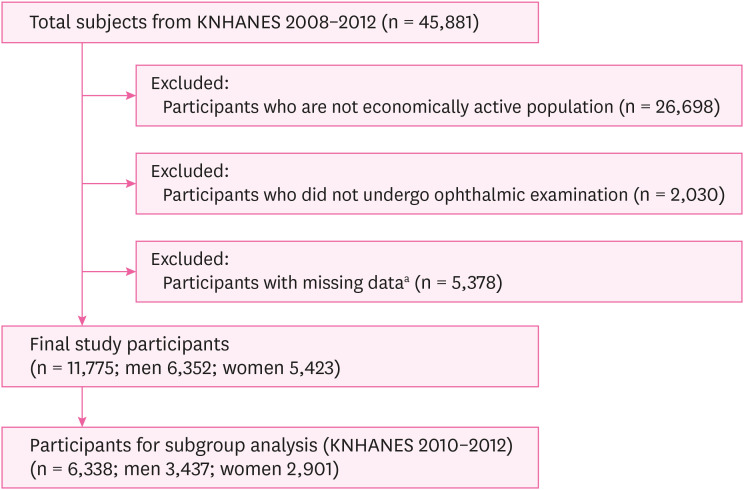
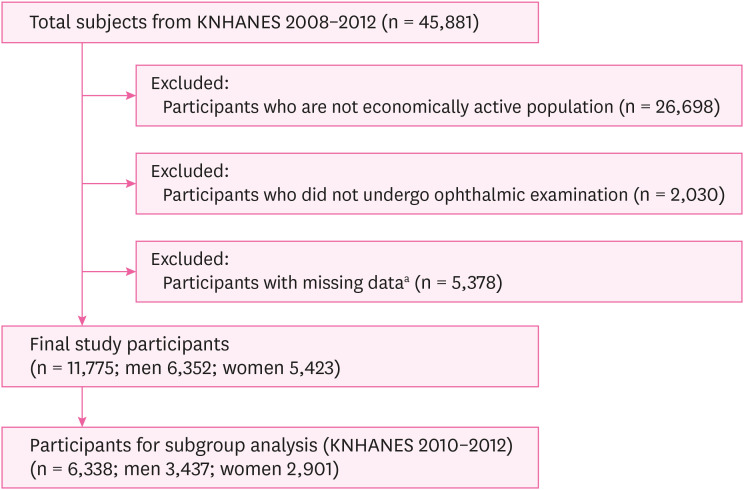
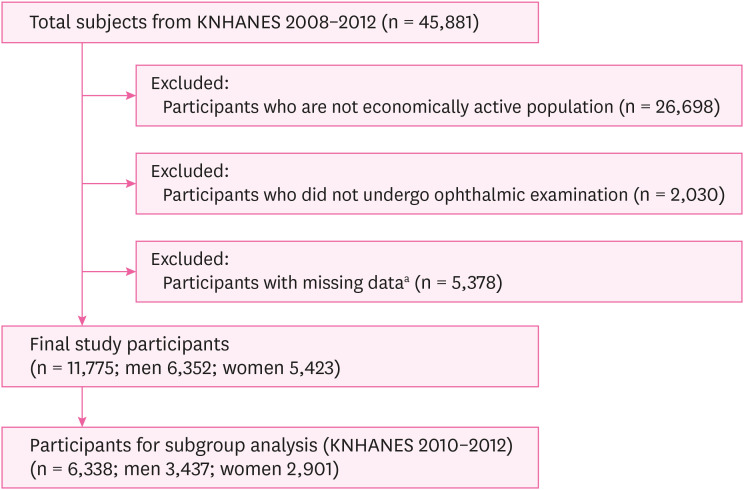
39 The sample size and exclusion criteria are shown in
Fig. 1.
Fig. 1
Study flow chart.
Schematic diagram shows the study design and selection of participants.
KNHANES: Korea National Health and Nutrition Examination Survey.
aSince cataract screening was conducted for those aged 19 and older, all subjects were aged 19 and older.
Outdoor sunlight exposure
Sunlight exposure outdoors was determined using a KNHANES ophthalmic survey questionnaire. The survey was conducted face-to-face by trained interviewers. The specific question was, “On average, how many hours during the day are you exposed directly to sunlight (scorching sun) without wearing sunglasses or a hat?” The responses were i) less than 5 hours and more than 5 hours in the 4th KNHANES (2008–2009) and ii) less than 2 hours, 2–5 hours, and 5 hours or more in the 5th KNHANES (2010–2012). In this study, sunlight exposure was categorized as < 5 hours and ≥ 5 hours. Meanwhile, a subgroup analysis was performed for participants included in the 5th KNHANES database.
General characteristics, socioeconomic, and health behavioral status
Age, sex, household income, education level
40 occupational classification,
41,42,43 alcohol consumption,
44 current smoking status,
43 physical activity,
45,46 and obesity
47 were included as potential confounding factors. Participants were aged 19 years or older, and they underwent all types of ophthalmic examinations. With respect to age, participants were classified as under 40 years, 40–59 years, and 60 years or older. The total household income was divided into 4 quartiles: low, low-middle, middle-high, and high. Education levels were divided into 4 groups: less than elementary, middle school, high school, and college or higher. Excluding armed forces, occupations were classified into four groups based on the International Standard Classification of Occupation (ISCO) and skill similarities as white collar (managers, professionals, technicians, and associate professionals), pink collar (clerical support, service, and sales workers), green collar (agricultural, forestry, and fishery workers), and blue collar (craft and related trades workers, plant and machine operators, assemblers, and elementary occupations).
48,49 Based on alcohol consumption, participants were classified as high risk (drinking two or more times a week, women drinking 5 glasses or more, and men drinking 7 glasses or more), moderate risk (drinking less than 4 times a month), or non-drinkers (did not drink alcohol in the last one year). Smoking status included non-smokers or current smokers. Physical activity was classified as high (3 times a week for more than 20 minutes), moderate (3 times a week for less than 20 minutes) and no activity. Obesity was classified as underweight (body mass index [BMI] < 18.5 kg/m
2), normal, and overweight (BMI > 25.0 kg/m
2).
Hypertension
50 and diabetes mellitus
51 are the major risk factors for eye disorders. Hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, or pharmacological treatment to control blood pressure. Diabetes mellitus was defined as a fasting blood glucose level ≥ 126 mg/dL, a diagnosis of diabetes mellitus by a doctor, or taking medication to control glucose levels.
Ophthalmologists assigned by the Korean Ophthalmological Society performed the ophthalmic examinations for the KNHANES, which included visual acuity tests, noncycloplegic autorefraction, slit-lamp examinations, intraocular pressure measurement, and non-mydriatic fundus photography. Based on the test results, the diagnosis of cataract, pterygium, and AMD was coded for the right and left eyeballs, and if only one eye had a disease, each eye disorder was defined.
Statistical analysis
The χ2 test was used to compare the baseline characteristics between groups based on the hours of sunlight exposure. After sex stratification, the relationship between hours of sunlight exposure and eye disorders was examined using multiple logistic regression analysis. To investigate the dose-dependent relationship between sunlight exposure time and eye diseases, a subgroup (< 2 hours, 2–5 hours, and > 5 hours of sunlight exposure) analysis was performed using the KNHANES 2010–2012 data. All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). For all statistical calculations, a p-value < 0.05 in both tails was considered significant.
Ethics statement
The KNHANES was approved by the Institutional Review Board (IRB) of the Korea Disease Control and Prevention Agency (IRB: 2008-04EXP-01-C, 2009-01CON-03-2C, 2010-02CON-21-C, 2011-02CON-06-C, 2012-01EXP-01-2C).
RESULTS
Baseline characteristics of study participants
We included 11,775 Korean economically active populations (6,352 men and 5,423 women) in the final analysis.
Table 1 presents the basic characteristics of the study participants according to the hours of sunlight exposure. A total of 2,577 (21.9%) participants were exposed to sunlight for ≥ 5 hours and 9,198 (78.1%) were exposed for < 5 hours. Twenty-five percent of men and 18.2% of women were exposed to sunlight ≥ 5 hours.
Table 1Baseline characteristics of study participants according to hours of sunlight exposure
|
Characteristics |
Total (%) |
p-value |
Male (%) |
p-value |
Female (%) |
p-value |
|
Lowa
|
Highb
|
Low |
High |
Low |
High |
|
Total participants |
9,198 (78.1) |
2,577 (21.9) |
- |
4,761 (75.0) |
1,591 (25.0) |
< 0.001
|
4,437 (81.8) |
986 (18.2) |
< 0.001
|
|
Age (years) |
|
|
< 0.001
|
|
|
< 0.001
|
|
|
- |
|
< 40 |
3,310 (83.4) |
658 (16.6) |
1,705 (80.2) |
421 (19.8) |
1,605 (87.1) |
237 (12.9) |
|
40–59 |
4,374 (79.9) |
1,102 (20.1) |
2,253 (76.7) |
685 (23.3) |
2,121 (83.6) |
417 (16.4) |
|
≥ 60 |
1,514 (65.0) |
817 (35.0) |
803 (62.3) |
485 (37.7) |
711 (68.2) |
332 (31.8) |
|
Household income |
|
|
< 0.001
|
|
|
< 0.001
|
|
|
< 0.001
|
|
Low |
1,121 (68.7) |
511 (31.3) |
468 (64.5) |
258 (35.5) |
653 (72.1) |
253 (28.0) |
|
Low-middle |
2,183 (75.0) |
729 (25.0) |
1,115 (70.3) |
471 (29.7) |
1,068 (80.5) |
258 (19.5) |
|
Middle-high |
2,893 (80.1) |
717 (19.9) |
1,537 (76.5) |
472 (23.5) |
1,356 (84.7) |
245 (15.3) |
|
High |
3,001 (82.3) |
620 (17.1) |
1,641 (80.8) |
390 (19.2) |
1,360 (85.5) |
230 (14.5) |
|
Education level |
|
|
< 0.001
|
|
|
< 0.001
|
|
|
< 0.001
|
|
Less than elementary school |
1,651 (68.4) |
762 (31.6) |
573 (63.6) |
328 (36.4) |
1,078 (71.3) |
434 (28.7) |
|
Middle school |
1,011 (73.1) |
373 (27.0) |
514 (68.1) |
241 (31.9) |
497 (79.0) |
132 (21.0) |
|
High school |
3,260 (79.6) |
834 (20.4) |
1,718 (74.4) |
590 (25.6) |
1,542 (86.3) |
244 (13.7) |
|
College or higher |
3,276 (84.4) |
608 (15.7) |
1,956 (81.2) |
432 (18.1) |
1,320 (88.2) |
176 (11.8) |
|
Occupational classification |
|
|
< 0.001
|
|
|
< 0.001
|
|
|
< 0.001
|
|
White collar |
3,414 (86.0) |
558 (14.0) |
1,855 (84.3) |
345 (15.7) |
1,559 (88.0) |
213 (12.0) |
|
Pink collar |
2,071 (81.9) |
458 (18.1) |
769 (76.1) |
242 (23.9) |
1,302 (85.8) |
216 (14.2) |
|
Green collar |
1,037 (59.2) |
716 (40.8) |
526 (56.7) |
402 (43.3) |
511 (61.9) |
314 (38.1) |
|
Blue collar |
2,676 (76.0) |
845 (24.0) |
1,611 (72.8) |
602 (27.2) |
1,065 (81.4) |
243 (18.6) |
|
Alcohol consumption |
|
|
0.055 |
|
|
0.077 |
|
|
0.003
|
|
None |
1,836 (76.7) |
559 (23.3) |
573 (71.8) |
225 (28.2) |
1,263 (79.1) |
334 (20.9) |
|
Moderate |
6,018 (78.8) |
1,621 (21.2) |
3,079 (75.2) |
1,015 (24.8) |
2,939 (82.9) |
606 (17.1) |
|
High-risk |
1,344 (77.2) |
397 (22.8) |
1,109 (76.0) |
351 (24.0) |
235 (83.6) |
46 (16.4) |
|
Current smoking |
|
|
< 0.001
|
|
|
0.169 |
|
|
0.431 |
|
No |
6,802 (79.3) |
1,780 (20.7) |
2,623 (75.6) |
845 (24.4) |
4,179 (81.7) |
935 (18.3) |
|
Yes |
2,396 (75.0) |
797 (25.0) |
2,138 (74.1) |
746 (25.9) |
258 (83.5) |
51 (16.5) |
|
Physical activity |
|
|
0.011
|
|
|
0.018
|
|
|
0.001
|
|
No |
5,752 (77.5) |
1,670 (22.5) |
2,598 (73.7) |
925 (26.3) |
3,154 (80.9) |
745 (19.1) |
|
Moderate |
2,909 (78.6) |
792 (21.4) |
1,836 (76.0) |
580 (24.0) |
1,073 (83.5) |
212 (16.5) |
|
High |
537 (82.4) |
115 (17.6) |
327 (79.2) |
86 (20.8) |
210 (87.9) |
29 (12.1) |
|
Obesity (BMI, kg/m2) |
|
|
0.002
|
|
|
0.979 |
|
|
< 0.001
|
|
Underweight (< 18.5) |
378 (79.1) |
100 (20.9) |
130 (75.1) |
43 (24.9) |
248 (81.3) |
57 (18.7) |
|
Normal |
5,922 (79.0) |
1,569 (21.0) |
2,880 (74.9) |
967 (25.1) |
3,042 (83.5) |
602 (16.5) |
|
Overweight (≥ 25.0) |
2,898 (76.1) |
908 (23.9) |
1,751 (75.1) |
581 (24.9) |
1,147 (77.8) |
327 (22.2) |
|
Hypertension |
|
|
< 0.001
|
|
|
< 0.001
|
|
|
< 0.001
|
|
No |
6,802 (80.3) |
1,669 (19.7) |
3,275 (76.7) |
997 (23.3) |
3,527 (84.0) |
672 (16.0) |
|
Yes |
2,396 (72.5) |
908 (27.5) |
1,486 (71.4) |
594 (28.6) |
910 (74.4) |
314 (25.6) |
|
Diabetes mellitus |
|
|
< 0.001
|
|
|
< 0.001
|
|
|
< 0.001
|
|
No |
8,556 (78.9) |
2,292 (21.1) |
4,356 (75.8) |
1,394 (24.2) |
4,200 (82.4) |
898 (17.6) |
|
Yes |
642 (69.3) |
285 (30.7) |
405 (67.3) |
197 (32.7) |
237 (72.9) |
88 (27.1) |
|
Cataract |
|
|
< 0.001
|
|
|
< 0.001
|
|
|
< 0.001
|
|
No |
7,123 (80.7) |
1,702 (19.3) |
3,661 (77.4) |
1,071 (22.6) |
3,462 (84.6) |
631 (15.4) |
|
Yes |
2,075 (70.3) |
875 (29.7) |
1,100 (67.9) |
520 (32.1) |
975 (73.3) |
355 (26.7) |
|
Pterygium |
|
|
< 0.001
|
|
|
0.004
|
|
|
< 0.001
|
|
No |
8,658 (78.9) |
2,320 (21.1) |
4,462 (75.4) |
1,458 (24.6) |
4,196 (83.0) |
862 (17.0) |
|
Yes |
540 (67.8) |
257 (32.2) |
299 (69.2) |
133 (30.8) |
241 (66.0) |
124 (34.0) |
|
AMD |
|
|
< 0.001
|
|
|
< 0.001
|
|
|
< 0.001
|
|
No |
8,900 (78.8) |
2,390 (21.2) |
4,589 (75.6) |
1,478 (24.4) |
4,311 (82.5) |
912 (17.5) |
|
Yes |
298 (61.4) |
187 (38.6) |
172 (60.4) |
113 (39.6) |
126 (63.0) |
74 (37.0) |
The χ2 test showed statistically significant differences in general characteristics (age and sex), socioeconomic status (household income, education level, occupation), chronic diseases (hypertension and diabetes mellitus), and eye disorders (cataract, pterygium, AMD) between the groups based on sunlight exposure. Meanwhile, health behavioral status also showed differences for each variable. There was no significant relationship between alcohol consumption and sunlight exposure time in the total study group and in men. Smoking status showed no statistically significant differences with sunlight exposure time in groups stratified by sex. While physical activity showed statistically significant differences based on sunlight exposure time, obesity in men showed no differences.
Eye disorders
Table 2 presents the association between hours of sun exposure and the prevalence of eye disorders. Odds ratios (ORs) and confidence intervals (CIs) were calculated using multiple regression analysis. ORs were adjusted for age, sex, household income, education level, occupational classification, alcohol consumption, current smoking status, physical activity, obesity, hypertension, and diabetes mellitus. Meanwhile, each stratified analysis was not adjusted for sex. The group with < 5 hours of sunlight exposure was considered the reference group. There was no significant relationship between sunlight exposure and cataracts. The OR for cataract was 0.88 (95% CI: 0.77–1.00) for all participants, and it was 0.89 (95% CI: 0.75–1.05) and 0.87 (95% CI: 0.70–1.07) for the male and female participants, respectively. The OR for pterygium was 1.10 (95% CI: 0.93–1.30) for all participants, and it was 0.88 (95% CI: 0.70–1.10) and 1.47 (95% CI: 1.15–1.89) for the male and female participants, respectively. The OR for AMD was 1.42 (95% CI: 1.16–1.73) for all participants, while it was 1.33 (95% CI: 1.03–1.73) and 1.58 (95% CI: 1.15–2.16) for the male and female participants, respectively.
Table 2Multiple logistic regression analysis of eye disorders in male and female participants
|
Sunlight exposure level |
Total |
Male |
Female |
|
No. of participants |
OR (95% CI) |
No. of participants |
OR (95% CI) |
No. of participants |
OR (95% CI) |
|
Cataract |
No
|
Yes
|
|
No
|
Yes
|
|
No
|
Yes
|
|
|
Lowa
|
7,123 |
2,075 |
1.00 (Reference) |
3,661 |
1,100 |
1.00 (Reference) |
3,462 |
975 |
1.00 (Reference) |
|
Highb
|
1,702 |
875 |
0.88 (0.77–1.00) |
1,071 |
520 |
0.89 (0.75–1.05) |
631 |
355 |
0.87 (0.70–1.07) |
|
Pterygium |
No
|
Yes
|
|
No
|
Yes
|
|
No
|
Yes
|
|
|
Low |
8,658 |
540 |
1.00 (Reference) |
4,462 |
299 |
1.00 (Reference) |
4,196 |
241 |
1.00 (Reference) |
|
High |
2,320 |
257 |
1.10 (0.93–1.30) |
1,458 |
133 |
0.88 (0.70–1.10) |
862 |
124 |
1.47 (1.15–1.89)
|
|
AMD |
No
|
Yes
|
|
No
|
Yes
|
|
No
|
Yes
|
|
|
Low |
8,900 |
298 |
1.00 (Reference) |
4,589 |
172 |
1.00 (Reference) |
4,311 |
126 |
1.00 (Reference) |
|
High |
2,390 |
187 |
1.42 (1.16–1.73)
|
1,478 |
113 |
1.33 (1.03–1.73)
|
912 |
74 |
1.58 (1.15–2.16)
|
Dose-dependent relationship between sunlight exposure and eye disorders
Subgroup analysis was performed using the 5th KNHANES (2010–2012) data, which included 6,338 participants (3,437 men and 2,901 women;
Fig. 1), based on the sunlight exposure time. The group with < 2 hours of exposure was considered the reference group. In the subgroup analysis, no significant relationship was observed between exposure to sunlight and cataracts. In contrast, a dose-dependent relationship was observed between the hours of sunlight exposure and pterygium, especially in the female participants. Compared with the reference group, the OR for pterygium for all participants was 1.07 (95% CI: 0.80–1.43) for 2–5 hours and 1.62 (95% CI: 1.25–2.08) for > 5 hours of sunlight exposure (
p for trend < 0.001). The OR for pterygium in the female participants was 1.28 (95% CI: 0.83–1.97) for 2–5 hours and 2.00 (95% CI: 1.39–2.88) for > 5 hours of sunlight exposure (
p < 0.001). The subgroup analysis showed no relationship between sunlight exposure and AMD (
Table 3).
Table 3Multiple logistic regression analysis of eye disorder according to hours of sunlight exposure (KNHANES 2010–2012)
|
Sun exposure level |
Total |
Male |
Female |
|
No. of participants |
OR (95% CI) |
p for trend |
No. of participants |
OR (95% CI) |
p for trend |
No. of participants |
OR (95% CI) |
p for trend |
|
Cataract |
No
|
Yes
|
|
0.189 |
No
|
Yes
|
|
0.117 |
No
|
Yes
|
|
0.974 |
|
Sunlight exposure < 2 hr |
3,025 |
736 |
1.00 (Reference) |
1,454 |
392 |
1.00 (Reference) |
1,571 |
344 |
1.00 (Reference) |
|
2 hr ≤ sunlight exposure < 5 hr |
1,102 |
338 |
0.85 (0.70–1.03) |
677 |
202 |
0.78 (0.61–1.01) |
425 |
136 |
0.97 (0.72–1.31) |
|
Sunlight exposure ≥ 5 hr |
600 |
537 |
1.01 (0.83–1.23) |
394 |
318 |
1.01 (0.78–1.30) |
206 |
219 |
1.01 (0.74–1.37) |
|
Pterygium |
No
|
Yes
|
|
< 0.001
|
No
|
Yes
|
|
0.159 |
No
|
Yes
|
|
< 0.001
|
|
Sunlight exposure < 2 hr |
3,601 |
160 |
1.00 (Reference) |
1,765 |
81 |
1.00 (Reference) |
1,836 |
79 |
1.00 (Reference) |
|
2 hr ≤ Sunlight exposure < 5 hr |
1,360 |
80 |
1.07 (0.80–1.43) |
836 |
43 |
0.90 (0.61–1.34) |
524 |
37 |
1.28 (0.83–1.97) |
|
Sunlight exposure ≥ 5 hr |
960 |
177 |
1.62 (1.25–2.08)
|
622 |
90 |
1.30 (0.91–1.86) |
338 |
87 |
2.00 (1.39–2.88)
|
|
AMD |
No
|
Yes
|
|
0.311 |
No
|
Yes
|
|
0.333 |
No
|
Yes
|
|
0.693 |
|
Sunlight exposure < 2 hr |
3,644 |
117 |
1.00 (Reference) |
1,785 |
61 |
1.00 (Reference) |
1,859 |
56 |
1.00 (Reference) |
|
2 hr ≤ Sunlight exposure < 5 hr |
1,366 |
74 |
1.27 (0.93–1.74) |
831 |
48 |
1.36 (0.91–2.05) |
535 |
26 |
1.25 (0.75–2.08) |
|
Sunlight exposure ≥ 5 hr |
1,024 |
113 |
1.17 (0.87–1.58) |
647 |
65 |
1.17 (0.78–1.76) |
377 |
48 |
1.12 (0.71–1.77) |
DISCUSSION
This study analyzed the relationship between outdoor sunlight exposure and the prevalence of eye disorders in the economically active population using data of the KNHANES, a large-scale epidemiological study. The χ2 test revealed that participants with higher sunlight exposure in the economically active population were relatively older and had lower income, education, and high-intensity physical activity. This group included mostly green- and blue-collar workers with a higher prevalence of hypertension, diabetes mellitus, cataract, pterygium, and AMD. However, exposure to sunlight showed no consistent relationship with drinking, smoking, and obesity in this group.
Multiple logistic regression analyses revealed that exposure to sunlight had no significant relationship with the prevalence of cataracts, while it had a significant relationship with pterygium in female participants and with AMD in all participants. Similarly, multiple logistic regression analyses of subgroups based on sunlight exposure levels showed that cataracts and AMD were not significantly associated with sunlight exposure levels. In contrast, the prevalence of pterygium was high in the subgroup with > 5 hours of sunlight exposure in all participants and in female participants.
Sunlight is electromagnetic radiation mainly composed of UV, visible, and IR radiation.
21 Although visible light does not significantly affect the human body and eyes, acute exposure to shorter wavelengths (< 450 nm) of visible light can cause solar retinopathy.
22 IR is known to induce cataracts through a mechanism that increase body temperature and accelerates the aging process,
52 although this requires exposure for several decades or more.
The thermal effect of IR is also important; however, the most important aspect in terms of the pathophysiology of eye disorders is the photochemical damage caused by UV radiation. UV-B and UV-A are mostly absorbed by the cornea and lens, while 1%–2% of UV-A reaches the retina. The cornea mostly absorbs UV-C. Although anatomical structures such as the orbit bones and the avoidance reaction to light effectively protect the eyes from UV, the absorbed UV causes DNA photo-damage owing to the action of reactive oxygen species.
32 Notably, UV-B is known to be the wavelength most associated with cataracts.
53,54
In this study, no significant relationship was found between sunlight exposure and cataract prevalence. Although we did not distinguish between the different electromagnetic radiations of sunlight, it is safe to assume that participants with high levels of sunlight exposure would have high levels of UV exposure as well. Cataracts are still the leading cause of blindness and low vision, and the World Health Organization (WHO) estimates that the incidence of age-related cataracts will continue to increase.
55 In 2006, the WHO estimated that the disability-adjusted life year for cataracts owing to UV exposure was 529,242.
56 Therefore, the economically active population, the target group of this study, may have been affected by the health worker effect.
UV-B is also a major risk factor for pterygium.
57 In a study of approximately 5,000 nursing home residents aged 40 and older in the Australian state of Victoria, the OR for pterygium in men to women was approximately 2.02 (95% CI: 1.35–3.03).
58 Similarly, in a study of 2,000 Chinese people aged 40–79 on an island in Singapore, the OR for pterygium in men to women was 4.2 (95% CI: 2.5–6.9).
59 A recent systematic review and meta-analysis, including 68 studies with 415,911 participants from 24 countries, showed that the OR for pterygium in men to women was 1.30 (95% CI: 1.14–1.45).
13 The European Agency for Safety and Health at Work defines outdoor workers as those exposed to sunlight for more than 75% of their working hours, and it is estimated that 90% of the 15 million outdoor workers are men.
60 In addition, a dose-dependent relationship has been reported between sunlight exposure and pterygium. In a questionnaire-based case-control study in Western Australia, the OR for the group with the highest sunlight exposure was 4.38 (95% CI: 1.88–10.93). Furthermore, the OR for not wearing sunglasses or other protective equipment was 6.77 (95% CI: 2.60–19.68).
16 Personal protective equipment for eye (especially sunglasses) effectively reduces ocular UV-B exposure.
61 Therefore, in general, sunglasses are recommended as protective equipment to prevent eye disorders.
19 According to a Canadian cohort study, the percentage of outdoor workers wearing sunglasses was 74% during work and 78% during leisure activities.
62 On the other hand, so far, it is difficult to find a study on the rate of wearing eye protective equipment for the prevention of eye disorders among outdoor workers in Korea. Specifically, DNA mutations caused by UV-induced oxidative stress can lead to changes in tumor suppressor genes, apoptosis-related proteins, cell adhesion molecules, proliferation-related proteins, heat shock proteins, tight junction proteins, extracellular matrix proteins, interleukin, and growth factors. These cellular changes have also been associated with pterygium formation.
63 Of these, gender-specific oxidative stress pathways may be considered in further studies.
Previous studies such as the Beaver Dam Eye study
9,17 have reported a relationship between sunlight exposure and AMD. In addition, a recent study using the European Genetic Database reported that past sunlight exposure is a greater risk factor than current sunlight exposure.
15 In this study, a correlation between sunlight and AMD prevalence was observed, but there was no statistical significance of this relationship in subgroup analysis. This may be because of the relatively small proportion of the subgroup or the exposure lag between sunlight exposure and AMD.
This study had several limitations. First, KNHANES is a cross-sectional study and only showed the relationship between sunlight exposure and eye disorders and not the causality. Second, we did not differentiate between UV, visible light, and IR as components of sunlight. Third, since sunlight exposure, the main variable in the study, was assessed using a questionnaire and was not quantified, it may have been influenced by recall bias.
To the best of our knowledge, this is the first study to analyze the relationship between sunlight exposure and eye disorders by adjusting for related confounding factors in a large-scale economically active population. In general, it is known that there are more male outdoor workers, and the prevalence of pterygium is also high, but the OR of pterygium according to sunlight exposure was higher in the female group. Considering the results of this study, that female outdoor workers may be more vulnerable to pterygium. Further research is needed to clarify the biochemical and immunological pathophysiology of sunlight-related eye disorders.
CONCLUSIONS
This study demonstrates the association between sunlight exposure and the prevalence of eye disorders in an economically active population. Despite the study limitations, we provided some information about the relationship between sunlight exposure and cataracts, pterygium, and AMD in an economically active population. The working population, like the general population, was also at risk of developing eye disorders due to sunlight exposure. It seems necessary to consider the appropriate use of personal protective equipment to block sunlight such as sunglasses or a hat. A dose-dependent relationship between sunlight exposure and pterygium was observed in women, and further studies well designed in consideration of the pathophysiology are needed.
Abbreviations
age-related macular degeneration
International Standard Classification of Occupation
Korea National Health and Nutrition Examination Survey
World Health Organization
NOTES
-
Competing interests: The authors declare that they have no competing interests.
-
Author Contributions:
Conceptualization: Lee J, Lee W.
Data curation: Lee J, Lee Y, Han E.
Formal analysis: Lee J, Kim UJ, Lee Y.
Investigation: Lee J, Ham S, Choi WJ, Kang SK.
Methodology: Lee W.
Project administration: Kang SK.
Software: Lee W.
Supervision: Kang SK.
Validation: Ham S, Choi WJ, Lee W.
Visualization: Lee J.
Writing - original draft: Lee J.
Writing - review & editing: Lee W, Kang SK.
REFERENCES
REFERENCES
- 1. Webb AR. Who, what, where and when-influences on cutaneous vitamin D synthesis. Prog Biophys Mol Biol 2006;92(1):17–25. 16766240.ArticlePubMed
- 2. Smolensky MH, Sackett-Lundeen LL, Portaluppi F. Nocturnal light pollution and underexposure to daytime sunlight: complementary mechanisms of circadian disruption and related diseases. Chronobiol Int 2015;32(8):1029–1048. 26374931.ArticlePubMed
- 3. Jackson LL, Rosenberg HR. Preventing heat-related illness among agricultural workers. J Agromed 2010;15(3):200–215.Article
- 4. Taylor CR, Sober AJ. Sun exposure and skin disease. Annu Rev Med 1996;47(1):181–191. 8712772.ArticlePubMed
- 5. Zee PC, Vitiello MV. Circadian rhythm sleep disorder: irregular sleep wake rhythm. Sleep Med Clin 2009;4(2):213–218. 20160950.ArticlePubMedPMC
- 6. Dumont M, Beaulieu C. Light exposure in the natural environment: relevance to mood and sleep disorders. Sleep Med 2007;8(6):557–565. 17383230.ArticlePubMed
- 7. Taylor HR, West SK, Rosenthal FS, Muñoz B, Newland HS, Abbey H, et al. Effect of ultraviolet radiation on cataract formation. N Engl J Med 1988;319(22):1429–1433. 3185661.ArticlePubMed
- 8. Coroneo M. Ultraviolet radiation and the anterior eye. Eye Contact Lens 2011;37(4):214–224. 21670690.ArticlePubMed
- 9. Cruickshanks KJ, Klein R, Klein BE. Sunlight and age-related macular degeneration. The Beaver Dam Eye Study. Arch Ophthalmol 1993;111(4):514–518. 8470986.ArticlePubMed
- 10. Delic NC, Lyons JG, Di Girolamo N, Halliday GM. Damaging effects of ultraviolet radiation on the cornea. Photochem Photobiol 2017;93(4):920–929. 27935054.ArticlePubMedPDF
- 11. Oddone E, Taino G, Vita S, Schimd M, Frigerio F, Imbriani M. Macular degeneration: peculiar sunlight exposure in an agricultural worker. Med Lav 2019;110(3):241–245. 31268431.ArticlePubMedPMCPDF
- 12. Pastor-Valero M, Fletcher AE, de Stavola BL, Chaqués-Alepúz V. Years of sunlight exposure and cataract: a case-control study in a Mediterranean population. BMC Ophthalmol 2007;7(1):18. 18039367.ArticlePubMedPMCPDF
- 13. Rezvan F, Khabazkhoob M, Hooshmand E, Yekta A, Saatchi M, Hashemi H. Prevalence and risk factors of pterygium: a systematic review and meta-analysis. Surv Ophthalmol 2018;63(5):719–735. 29551597.ArticlePubMed
- 14. Roberts JE. Ultraviolet radiation as a risk factor for cataract and macular degeneration. Eye Contact Lens 2011;37(4):246–249. 21617534.ArticlePubMed
- 15. Schick T, Ersoy L, Lechanteur YT, Saksens NT, Hoyng CB, den Hollander AI, et al. History of sunlight exposure is a risk factor for age-related macular degeneration. Retina 2016;36(4):787–790. 26441265.ArticlePubMed
- 16. Threlfall TJ, English DR. Sun exposure and pterygium of the eye: a dose-response curve. Am J Ophthalmol 1999;128(3):280–287. 10511020.ArticlePubMed
- 17. Tomany SC, Cruickshanks KJ, Klein R, Klein BE, Knudtson MD. Sunlight and the 10-year incidence of age-related maculopathy: the Beaver Dam Eye Study. Arch Ophthalmol 2004;122(5):750–757. 15136324.ArticlePubMed
- 18. West SK, Rosenthal FS, Bressler NM, Bressler SB, Munoz B, Fine SL, et al. Exposure to sunlight and other risk factors for age-related macular degeneration. Arch Ophthalmol 1989;107(6):875–879. 2786410.ArticlePubMed
- 19. Yam JC, Kwok AK. Ultraviolet light and ocular diseases. Int Ophthalmol 2014;34(2):383–400. 23722672.ArticlePubMedPDF
- 20. Zhou H, Zhang H, Yu A, Xie J. Association between sunlight exposure and risk of age-related macular degeneration: a meta-analysis. BMC Ophthalmol 2018;18(1):331. 30572865.ArticlePubMedPMCPDF
- 21. Zamanian A, Hardiman C. Electromagnetic radiation and human health: a review of sources and effects. High Freq Electron 2005;4(3):16–26.
- 22. Yannuzzi LA, Fisher YL, Slakter JS, Krueger A. Solar retinopathy: a photobiologic and geophysical analysis. 1989. Retina 2012;32(Suppl 1):28–43. 22451949.PubMed
- 23. Scott JA. The computation of temperature rises in the human eye induced by infrared radiation. Phys Med Biol 1988;33(2):243–257. 3362967.ArticlePubMed
- 24. Lee J, Lee YH, Choi WJ, Ham S, Kang SK, Yoon JH, et al. Heat exposure and workers' health: a systematic review. Rev Environ Health 2021.ArticlePMC
- 25. Alcott LM. Little Women. New York, NY, USA: Macmillan; 1994.
- 26. Lee J, Lee W, Choi WJ, Kang SK, Ham S. Association between exposure to extreme temperature and injury at the workplace. Int J Environ Res Public Health 2019;16(24):4955.ArticlePubMedPMC
- 27. Lee W, Lee J, Kim UJ, Yoon JH, Choi WJ, Ham S, et al. Working conditions and mental health status related with occupational injury of Korean outdoor workers. J Occup Environ Med 2020;62(7):e334–e339. 32730037.ArticlePubMed
- 28. Wittenborn JS, Zhang X, Feagan CW, Crouse WL, Shrestha S, Kemper AR, et al. The economic burden of vision loss and eye disorders among the United States population younger than 40 years. Ophthalmology 2013;120(9):1728–1735. 23631946.ArticlePubMedPMC
- 29. Chakravarthy U, Wong TY, Fletcher A, Piault E, Evans C, Zlateva G, et al. Clinical risk factors for age-related macular degeneration: a systematic review and meta-analysis. BMC Ophthalmol 2010;10(1):31. 21144031.ArticlePubMedPMCPDF
- 30. Prokofyeva E, Wegener A, Zrenner E. Cataract prevalence and prevention in Europe: a literature review. Acta Ophthalmol 2013;91(5):395–405. 22715900.ArticlePubMed
- 31. Liu T, Liu Y, Xie L, He X, Bai J. Progress in the pathogenesis of pterygium. Curr Eye Res 2013;38(12):1191–1197. 24047084.ArticlePubMed
- 32. Modenese A, Korpinen L, Gobba F. Solar radiation exposure and outdoor work: An underestimated occupational risk. Int J Environ Res Public Health 2018;15(10):2063.ArticlePubMedPMC
- 33. Yasmin R, Ahmad R, Sultana N, Sayed S, Ahmad SA, Zaman F, et al. Eye problems among the workers in re-rolling mill exposed to high temperature. Work 2013;46(1):93–97. 22976158.ArticlePubMed
- 34. Kumah D, Oteng-Amoako A, Apio H. Prevalence of pterygium among kitchen staff in senior high schools in the Kumasi metropolis, Ghana. Ghana J Sci 2011;13(2):83–88.
- 35. Rim TH, Nam J, Kim EK, Kim TI. Risk factors associated with pterygium and its subtypes in Korea: the Korean National Health and Nutrition Examination Survey 2008–2010. Cornea 2013;32(7):962–970. 23442251.PubMed
- 36. Kim K, Yoon S, Kim J, Woo KH, Cho SY, Jo HR. Relationship between shift work and age-related macular degeneration: a cross-sectional analysis of data from the 5th Korea National Health and Nutrition Examination Survey (2010–2012). Ann Occup Environ Med 2021;33(1):e7.ArticlePubMedPMCPDF
- 37. Lim CY, Kim SH, Chuck RS, Lee JK, Park CY. Risk factors for pterygium in Korea: The Korean national health and nutrition examination survey V, 2010–2012. Medicine (Baltimore) 2015;94(32):e1258. 26266358.PubMedPMC
- 38. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea national health and nutrition examination survey (KNHANES). Int J Epidemiol 2014;43(1):69–77. 24585853.ArticlePubMedPMC
- 39. Hussmanns R, Mehran F, Varmā V. Surveys of Economically Active Population, Employment, Unemployment, and Underemployment: an ILO Manual on Concepts and Methods. Geneva, Switzerland: International Labour Office; 1990.
- 40. Zetterberg M. Age-related eye disease and gender. Maturitas 2016;83:19–26. 26508081.ArticlePubMed
- 41. Modenese A, Gobba F. Macular degeneration and occupational risk factors: a systematic review. Int Arch Occup Environ Health 2019;92(1):1–11. 30191305.ArticlePubMedPMCPDF
- 42. Bazeer S, Jansonius N, Snieder H, Hammond C, Vehof J. The relationship between occupation and dry eye. Ocul Surf 2019;17(3):484–490. 30951831.ArticlePubMed
- 43. Leske MC, Chylack LT Jr, Wu SY. The lens opacities case-control study: risk factors for cataract. Arch Ophthalmol 1991;109(2):244–251. 1993036.ArticlePubMed
- 44. Hiratsuka Y, Li G. Alcohol and eye diseases: a review of epidemiologic studies. J Stud Alcohol 2001;62(3):397–402. 11414350.ArticlePubMed
- 45. Ong SR, Crowston JG, Loprinzi PD, Ramulu PY. Physical activity, visual impairment, and eye disease. Eye (Lond) 2018;32(8):1296–1303. 29610523.ArticlePubMedPMCPDF
- 46. Kawashima M, Uchino M, Yokoi N, Uchino Y, Dogru M, Komuro A, et al. The association between dry eye disease and physical activity as well as sedentary behavior: results from the Osaka study. J Ophthalmol 2014;2014:943786. 25485144.ArticlePubMedPMCPDF
- 47. Cheung N, Wong TY. Obesity and eye diseases. Surv Ophthalmol 2007;52(2):180–195. 17355856.ArticlePubMedPMC
- 48. Lee W, Yeom H, Yoon JH, Won JU, Jung PK, Lee JH, et al. Metabolic outcomes of workers according to the International Standard Classification of Occupations in Korea. Am J Ind Med 2016;59(8):685–694. 27345305.ArticlePubMed
- 49. International Standard Classification of Occupations. 2008 (ISCO-08): Structure, Group Definitions and Correspondence Tables. Geneva, Switzerland: International Labour Office; 2012.
- 50. Wong TY, Mitchell P. The eye in hypertension. Lancet 2007;369(9559):425–435. 17276782.ArticlePubMed
- 51. Duh EJ, Sun JK, Stitt AW. Diabetic retinopathy: current understanding, mechanisms, and treatment strategies. JCI Insight 2017;2(14):e93751.ArticlePubMedPMC
- 52. Wolbarsht M. Damage to the lens from infrared. Proceedings Volume 0229, Ocular Effects of Non-Ionizing Radiation. Washington, D.C., USA: International Society for Optics and Photonics; 1980, 121–143.
- 53. Taylor HR. Ocular effects of UV-B exposure. Doc Ophthalmol 1994-1995;88(3-4):285–293.ArticlePDF
- 54. Taylor HR. Epidemiology of age-related cataract. Eye (Lond) 1999;13(3):Pt 3b. 445–448. 10627822.ArticlePubMedPDF
- 55. Tenkate T, Adam B, Al-Rifai RH, Chou BR, Gobba F, Ivanov ID, et al. WHO/ILO work-related burden of disease and injury: Protocol for systematic reviews of occupational exposure to solar ultraviolet radiation and of the effect of occupational exposure to solar ultraviolet radiation on cataract. Environ Int 2019;125:542–553. 30737039.ArticlePubMed
- 56. Lucas R, McMichael I, Smith W, Armstrong BK, Prüss-Üstün A. Solar Ultraviolet Radiation: Global Burden of Disease from Solar Ultraviolet Radiation. Geneva, Switzerland: World Health Organization; 2006.
- 57. Saw SM, Tan D. Pterygium: prevalence, demography and risk factors. Ophthalmic Epidemiol 1999;6(3):219–228. 10487976.ArticlePubMed
- 58. McCarty CA, Fu CL, Taylor HR. Epidemiology of pterygium in Victoria, Australia. Br J Ophthalmol 2000;84(3):289–292. 10684840.ArticlePubMedPMC
- 59. Wong TY, Foster PJ, Johnson GJ, Seah SK, Tan DT. The prevalence and risk factors for pterygium in an adult Chinese population in Singapore: the Tanjong Pagar survey. Am J Ophthalmol 2001;131(2):176–183. 11228292.ArticlePubMed
- 60. European Agency for Safety and Health at Work. New and Emerging Risks in Occupational Safety and Health. Bilbao, Spain: European Agency for Safety and Health at Work; 2009.
- 61. Rosenthal FS, Bakalian AE, Lou CQ, Taylor HR. The effect of sunglasses on ocular exposure to ultraviolet radiation. Am J Public Health 1988;78(1):72–74. 3337309.ArticlePubMedPMC
- 62. Peters CE, Koehoorn MW, Demers PA, Nicol AM, Kalia S. Outdoor workers' use of sun protection at work and leisure. Saf Health Work 2016;7(3):208–212. 27630789.ArticlePubMedPMC
- 63. Wanzeler ACV, Barbosa IAF, Duarte B, Borges D, Barbosa EB, Kamiji D, et al. Mechanisms and biomarker candidates in pterygium development. Arq Bras Oftalmol 2019;82(6):528–536. 31576927.ArticlePubMed
 , Ui-Jin Kim1,2
, Ui-Jin Kim1,2 , Yongho Lee1,2
, Yongho Lee1,2 , Eunseun Han1,2
, Eunseun Han1,2 , Seunghon Ham1,2,3
, Seunghon Ham1,2,3 , Wanhyung Lee1,2,3
, Wanhyung Lee1,2,3 , Won-Jun Choi1,2,3
, Won-Jun Choi1,2,3 , Seong-Kyu Kang1,2,3
, Seong-Kyu Kang1,2,3

 KSOEM
KSOEM

 Cite
Cite

