Abstract
-
Background
Shift work is associated with a higher risk of cardiovascular diseases. Here, we sought to assess the relationship between shift work and plasma homocysteine levels. Determining the correlations between shift work and homocysteine levels may provide a better understanding of the mechanisms underlying cardiovascular diseases.
-
Methods
This study was performed using data from routine health examinations of steel workers in 2017. In total, 431 male workers (70 daytime workers and 361 shift workers) employed on a rolling departure schedule were recruited. Plasma homocysteine levels > 15 μmol/L were considered elevated. The χ2, analysis of variance, and multiple logistic regression analyses were used to examine the association between shift work and plasma homocysteine levels.
-
Results
In comparison to daytime workers, the odds ratio (OR) of hyperhomocysteinemia in individuals with < 10 years of shift work was 1.14 (95% confidence interval [CI]: 0.64–2.03), compared to 2.01 (95% CI: 1.14–3.54) for workers with ≥ 10 years of experience. After adjusting for confounding variables, the adjusted OR for shift workers with < 10 years of experience was 0.95 (95% CI: 0.50–1.80), compared to 2.00 (95% CI: 1.07–3.74) for workers with ≥ 10 years of experience.
-
Conclusions
The risk of hyperhomocysteinemia was significantly higher in shift workers compared to those working normal daytime hours, particularly among long-term shift workers.
-
Keywords: Shift work; Homocysteine; Hyperhomocysteinemia; Cardiovascular disease
BACKGROUND
According to the International Labor Office, shift work is defined as “a method of organization of working time in which workers succeed one another at the workplace so that the establishment can operate longer than the hours of work of individual workers” [
1]. More generally, the term is used to encompasses any shift that occurs outside regular daytime hours, with night work regarded as taking place from 22:00 to 06:00 [
2].
Health problems associated with shift work include sleep disorders, mental health issues (such as depression), gastrointestinal complications, and injury, with the most severe symptoms typically being associated with night shifts. In recent years, cerebral cardiovascular disease and cancer have been added to the wide range of negative health outcomes attributed to shift work [
3].
Numerous studies have examined the relationship between cardiovascular diseases and shift work. In a meta-analysis by Bøggild et al. [
4] which reviewed 17 studies (9 cohort studies, 4 case-report studies, and 4 cross-sectional studies) performed prior to 1999, shift workers had a 40% increased risk of cardiovascular disease relative to controls. More recently, Torquati et al. [
5] reviewed 21 studies involving 173,010 unique participants, and found that the risk of any cardiovascular disease event was 17% higher among shift workers compared to daytime workers. Furthermore, the risk of coronary heart disease-related morbidity was 26% higher than that seen in daytime workers.
Shift work-related pathology is typically attributed to circadian stress, in which disruption of the normal circadian rhythms can lead to the dysregulation of normal physiological, behavioral, and psychosocial pathways. Over long periods, these disruptions can lead to a host of chronic diseases, such as atherosclerosis and metabolic syndrome, and may increase the risk of cardiovascular diseases [
4].
Emerging research examining the processes underlying atherosclerosis and inflammatory biomarkers has provided direct evidence of a link between atherosclerosis and shift work [
6]. One such risk factor for cardiovascular disease is plasma homocysteine levels. Homocysteine is a non-proteinogenic amino acid produced during metabolism of the essential amino acid methionine. In addition, homocysteine can be re-synthesized into methionine by a re-methylation process, in which vitamin B
12 acts as a cofactor [
7]. Increased levels of plasma homocysteine are important in cardiovascular disease, increasing the risk associated with factors such as smoking, hypertension, and hyperlipidemia [
8]. Homocysteine levels are also associated with oxidative stress and endothelial dysfunction [
9]; however, the exact role of homocysteine in disease pathogenesis is still controversial. Despite this, the association between hyperhomocysteinemia and cardiovascular disease is strongly supported by epidemiological studies, which have consistently identified hyperhomocysteinemia as an independent risk factor for cardiovascular diseases [
10].
While homocysteine is understood to cause cardiovascular disease, little is known regarding the relationships among plasma homocysteine levels, shift work and cardiovascular disease. Here, we used data from workers' health examinations conducted by a steel company to investigate the association between shift work and cardiovascular disease.
METHODS
Study subjects
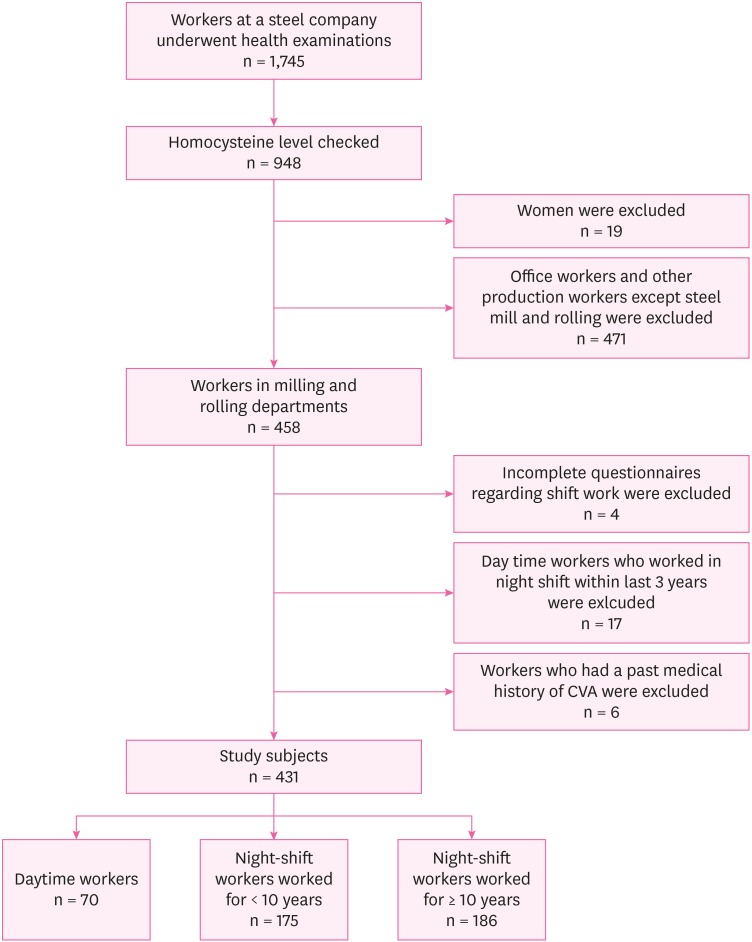
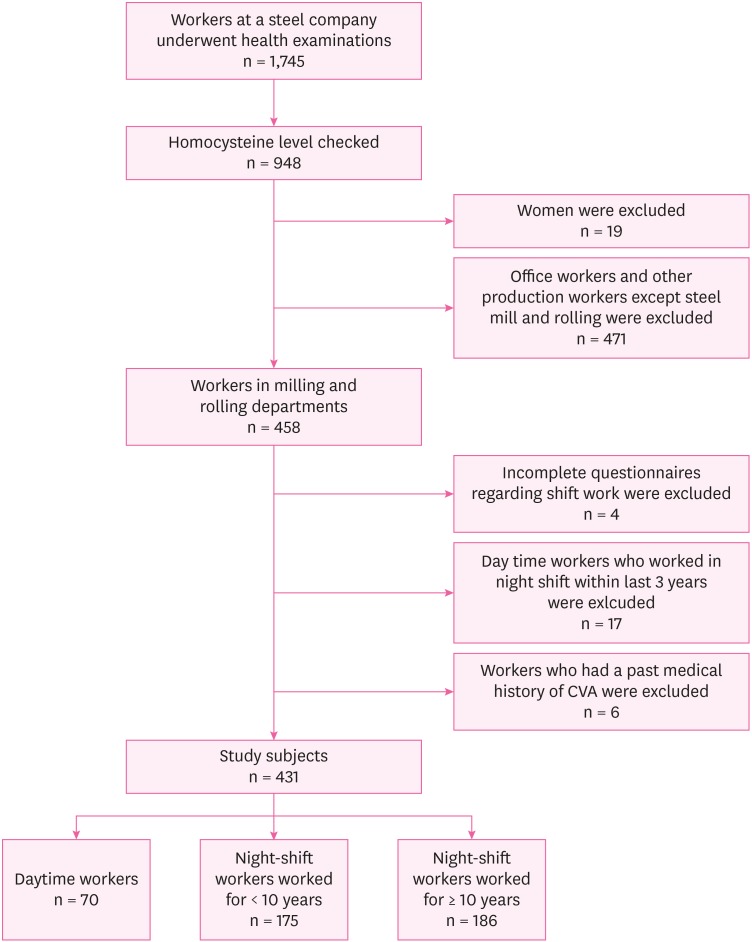
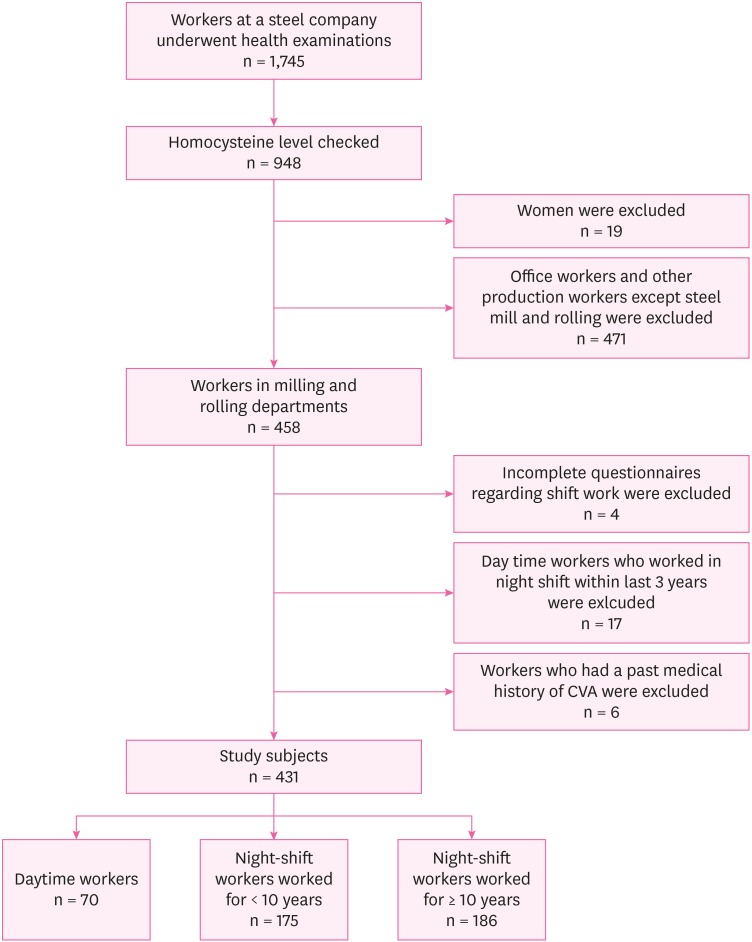
A total of 1,745 workers at a steel company in Incheon, Korea underwent routine workers' health examinations in 2017; 948 workers underwent additional blood tests assessing a variety of factors, including homocysteine levels. These 948 workers were selected as the initial subjects in the analysis of the association between plasma homocysteine levels and shift work. Nineteen female workers were excluded from the cohort, as the number of women was too small to enable any meaningful analyses. A large difference was evident between the numbers of daytime and shift workers. To reduce the effect of these differences, inclusion of daytime workers was limited to those working in the milling and rolling departments (n = 471). A further four workers were excluded due to incomplete questionnaires regarding shift work. To reduce the confounding effects of previous shift work, daytime workers who had engaged in shift work within the previous 3 years were also excluded. We also excluded six workers who had a past medical history of a cerebrovascular accident (CVA), which has been related to elevated homocysteine levels [
11,
12]. After all exclusions were applied, in total 431 workers, including 70 daytime and 361 shift workers, were selected for further analysis. Shift workers were further classified into two groups according to the duration of shift work: short term (those with < 10 years shift work), and long-term (those with ≥ 10 years shift work) (
Fig. 1).
Fig. 1
Flow chart of the study subjects.
CVA: cerebrovascular accident.
Questionnaire
During the health-screening process, subjects were asked to complete a self-reported questionnaire. Data on age, working hours, working department, history of past illness, family history, history of smoking and drinking, physical activity, and symptoms related to the target organs were collected. In addition, shift workers were asked to provide additional details regarding their shift work, including its duration, type, work interval, number of days of continuous night work, workload relative to daytime work, weekly average working hours, and rest time during night work.
Physical examinations and blood tests
All subjects underwent simultaneous health examinations and additional blood tests. Measurements of height, weight, systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting blood glucose, renal function and a lipid profile were obtained for all subjects. In addition, homocysteine levels and glycated hemoglobin (HbA1c) levels were measured by additional blood tests independent of the routine health examinations. Hyperhomocysteinemia was defined as plasma homocysteine levels > 15 µmol/L, as recommended by the American Heart Association (AHA) [
13].
Descriptive statistical analyses were used to compare demographic and baseline health characteristics between groups. Analysis of variance and χ2 tests were used to assess differences in demographic and medical characteristics between daytime and shift workers. A multiple logistic regression model was used to adjust for variables known to affect cardiovascular disease, including age; smoking, drinking and exercise status; a family history of CVA; and body mass index (BMI). The odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to assess the effect of shift work on hyperhomocysteinemia. All statistical analyses were performed in R software (ver. 3.4.1; R Development Core Team, Vienna, Austria).
Ethics statement
This study was conducted after obtaining approval from the Institutional Review Board (IRB) of Gachon University's Gil Medical Center (IRB No. GAIRB2018-251).
RESULTS
General characteristics of research subjects
Long-term shift workers (≥ 10 years) were the oldest group, with an average age of 49.4 years, compared to the overall average of 41.3 years. Significant differences were evident between groups, with workers aged 30–39 years representing 47.1% and 67.4% of the daytime and short-term (< 10 years) shift workers, respectively. Meanwhile, 55.9% of long-term shift workers were > 50 years of age. Group differences were also observed in smoking status, with the rate of current smoking being highest among long-term shift workers. Analysis of medical history data revealed significant differences between the groups in terms of hypertension and diabetes mellitus (DM). The prevalence of hypertension and DM were highest among long-term shift workers. A family history of CVA was significantly higher in long-term shift workers. Long-term shift workers were more likely to report heavy drinking, although the differences were not statistically significant. Short-term shift workers were less likely to exercise than the other groups, and the differences were statistically significant (
Table 1).
Table 1General characteristics of the subjects
|
Characteristics |
All subjects (n = 431) |
Daytime workers (n = 70) |
Shift workers |
p-value |
|
< 10 years (n = 175) |
≥ 10 years (n = 186) |
|
Mean age (years) |
41.3 ± 10.9 |
41.9 ± 10.5 |
32.5 ± 5.3 |
49.4 ± 8.3 |
< 0.001 |
|
Age (years) |
|
|
|
|
< 0.001 |
|
20–29 |
52 (12.1) |
6 (8.6) |
46 (26.3) |
0 (0.0) |
|
30–39 |
183 (42.5) |
33 (47.1) |
118 (67.4) |
32 (17.2) |
|
40–49 |
64 (14.8) |
7 (10.0) |
7 (4.0) |
50 (26.9) |
|
50–59 |
102 (23.7) |
21 (30.0) |
3 (1.7) |
78 (41.9) |
|
60–69 |
30 (7.0) |
3 (4.3) |
1 (0.6) |
26 (14.0) |
|
Smokinga
|
|
|
|
|
< 0.001 |
|
Never |
116 (27.0) |
21 (30.0) |
63 (36.0) |
32 (17.3) |
|
Past smoker |
130 (30.2) |
28 (40.0) |
37 (21.1) |
65 (35.1) |
|
Current smoker |
184 (42.8) |
21 (30.0) |
75 (42.9) |
88 (47.6) |
|
Heavy drinking |
|
|
|
|
0.108 |
|
No |
296 (68.7) |
54 (77.1) |
123 (70.3) |
119 (64.0) |
|
Yes |
135 (31.3) |
16 (22.9) |
52 (29.7) |
67 (36.0) |
|
Regular exercise |
|
|
|
|
0.043 |
|
No |
243 (56.4) |
34 (48.6) |
111 (63.4) |
98 (52.7) |
|
Yes |
188 (43.6) |
36 (51.4) |
64 (36.6) |
88 (47.3) |
|
Hypertension |
|
|
|
|
< 0.001 |
|
No |
385 (89.3) |
62 (88.6) |
174 (99.4) |
149 (80.1) |
|
Yes |
46 (10.7) |
8 (11.4) |
1 (0.6) |
37 (19.9) |
|
DM |
|
|
|
|
< 0.001 |
|
No |
410 (95.1) |
67 (95.7) |
174 (99.4) |
169 (90.9) |
|
Yes |
21 (4.9) |
3 (4.3) |
1 (0.6) |
17 (9.1) |
|
Family history of CVA |
|
|
|
|
< 0.001 |
|
No |
388 (90.0) |
65 (92.9) |
167 (95.4) |
156 (83.9) |
|
Yes |
43 (10.0) |
5 (7.1) |
8 (4.6) |
30 (16.1) |
Results of physical examinations and biochemistry blood tests according to work type
Clinical analysis of daytime and shift workers found that a BMI > 25 kg/m
2 was significantly higher among long-term shift workers. Both SBP and DBP were significantly higher in long-term shift workers compared to daytime workers. Plasma homocysteine levels were also elevated in this group, with a homocysteine level > 15 μmol/L being significantly more prevalent among long-term shift workers. In fasting glucose tests, mean HbA1c and triglyceride (TG) levels, as well as the rate of clinically meaningful findings, were significantly higher in long-term shift workers. Other measurements, including mean BMI, waist circumference, low-density lipoprotein-cholesterol, high-density lipoprotein-cholesterol, total cholesterol, and creatinine levels did not differ significantly between groups (
Table 2).
Table 2Results of physical examinations and biochemistry blood tests according to work type
|
Characteristics |
All subjects (n = 431) |
Daytime workers (n = 70) |
Shift workers |
p-value |
|
< 10 years (n = 173) |
≥ 10 years (n = 186) |
|
BMI (kg/m2) |
|
|
|
|
|
|
Mean |
25.3 ± 3.3 |
24.9 ± 2.7 |
25.1 ± 3.8 |
25.6 ± 3.0 |
0.158 |
|
< 25 |
215 (49.9) |
39 (55.7) |
94 (53.7) |
82 (44.1) |
0.048 |
|
25–30 |
179 (41.5) |
30 (42.9) |
63 (36.0) |
86 (46.2) |
|
|
≥ 30 |
37 (8.6) |
1 (1.4) |
18 (10.3) |
18 (9.7) |
|
|
WC (cm) |
|
|
|
|
|
|
Mean |
85.0 ± 8.4 |
83.6 ± 6.3 |
84.7 ± 9.8 |
85.7 ± 7.7 |
0.200 |
|
< 90 |
330 (76.6) |
61 (87.1) |
127 (72.6) |
142 (76.3) |
0.052 |
|
≥ 90 |
101 (23.4) |
9 (12.9) |
48 (27.4) |
44 (23.7) |
|
|
SBP (mmHg) |
|
|
|
|
|
|
Mean |
122.4 ± 11.6 |
120.3 ± 11.1 |
120.5 ± 11.2 |
125.0 ± 11.7 |
< 0.001 |
|
< 140 |
416 (96.5) |
68 (97.1) |
169 (96.6) |
179 (96.2) |
0.939 |
|
≥ 140 |
15 (3.5) |
2 (2.9) |
6 (3.4) |
7 (3.8) |
|
|
DBP (mmHg) |
|
|
|
|
|
|
Mean |
78.2 ± 8.5 |
76.2 ± 8.6 |
75.7 ± 8.8 |
81.3 ± 7.1 |
< 0.001 |
|
< 90 |
413 (95.8) |
67 (95.7) |
169 (96.6) |
177 (95.2) |
0.798 |
|
≥ 90 |
18 (4.2) |
3 (4.3) |
6 (3.4) |
9 (4.8) |
|
|
Homocysteine (µmol/L) |
|
|
|
|
|
|
Mean |
15.6 ± 5.2 |
15.4 ± 5.8 |
15.5 ± 5.3 |
15.8 ± 4.8 |
0.802 |
|
< 15 |
240 (55.7) |
45 (64.3) |
107 (61.1) |
88 (47.3) |
0.009 |
|
≥ 15 |
191 (44.3) |
25 (35.7) |
68 (38.9) |
98 (52.7) |
|
|
Glucose (fast) (mg/dL) |
|
|
|
|
|
|
Mean |
93.7 ± 20.3 |
90.3 ± 10.8 |
89.5 ± 21.1 |
98.8 ± 21.2 |
< 0.001 |
|
< 126 |
410 (95.1) |
70 (100.0) |
172 (98.3) |
168 (90.3) |
< 0.001 |
|
≥ 126 |
21 (4.9) |
0 (0.0) |
3 (1.7) |
18 (9.7) |
|
|
HbA1c (%) |
|
|
|
|
|
|
Mean |
5.7 ± 0.8 |
5.5 ± 0.4 |
5.5 ± 0.7 |
5.9 ± 1.0 |
< 0.001 |
|
< 6.5 |
391 (90.7) |
67 (95.7) |
169 (96.6) |
155 (83.3) |
< 0.001 |
|
≥ 6.5 |
40 (9.3) |
3 (4.3) |
6 (3.4) |
31 (16.7) |
|
|
LDL-C (mg/dL) |
|
|
|
|
|
|
Mean |
110.9 ± 31.1 |
113.2 ± 29.2 |
112.1 ± 29.7 |
108.9 ± 33.1 |
0.489 |
|
< 150 |
381 (88.4) |
61 (87.1) |
154 (88.0) |
166 (89.2) |
0.876 |
|
≥ 150 |
50 (11.6) |
9 (12.9) |
21 (12.0) |
20 (10.8) |
|
|
TG (mg/dL) |
|
|
|
|
|
|
Mean |
174.9 ± 156.2 |
148.7 ± 116.1 |
155.6 ± 150.8 |
202.8 ± 170.0 |
0.005 |
|
< 200 |
315 (73.1) |
61 (87.1) |
136 (77.7) |
118 (63.4) |
< 0.001 |
|
≥ 200 |
116 (26.9) |
9 (12.9) |
39 (22.3) |
68 (36.6) |
|
|
HDL-C (mg/dL) |
|
|
|
|
|
|
Mean |
51.9 ± 12.9 |
52.2 ± 14.3 |
53.5 ± 12.9 |
50.2 ± 12.2 |
0.051 |
|
< 40 |
361 (83.8) |
57 (81.4) |
155 (88.6) |
149 (80.1) |
0.079 |
|
≥ 40 |
70 (16.2) |
13 (18.6) |
20 (11.4) |
37 (19.9) |
|
|
Total cholesterol (mg/dL) |
|
|
|
|
|
|
Mean |
195.7 ± 35.8 |
192.8 ± 34.6 |
195.0 ± 35.0 |
197.3 ± 37.1 |
0.634 |
|
< 220 |
324 (75.2) |
57 (81.4) |
126 (72.0) |
141 (75.8) |
0.294 |
|
≥ 220 |
107 (24.8) |
13 (18.6) |
49 (28.0) |
45 (24.2) |
|
|
Creatinine (mg/dL) |
|
|
|
|
|
|
Mean |
0.88 ± 0.12 |
0.85 ± 0.10 |
0.88 ± 0.11 |
0.88 ± 0.12 |
0.110 |
|
< 1.2 |
423 (98.1) |
70 (100.0) |
171 (97.7) |
182 (97.8) |
0.643 |
|
≥ 1.2 |
8 (1.9) |
0 (0.0) |
4 (2.3) |
4 (2.2) |
|
Comparison of homocysteine levels by age
Age is the most important risk factor for cardiovascular disease. In this study, the subjects were grouped according to shift period, with a significant difference in age seen between groups. Even though we were able to correct for age using a multivariate regression model, to assess the effects of this variable on homocysteine levels better, we compared homocysteine levels by age independent of shift status. Homocysteine levels, as well as the prevalence of hyperhomocysteinemia, did not differ significantly among age groups (
Table 3). These results indicate that the high proportion of homocysteinemia in long-term shift workers was not simply an effect of age differences among groups.
Table 3Comparison of plasma homocysteine levels according to age group
|
Homocysteine |
Age (years) |
p-value |
|
20–29 |
30–39 |
40–49 |
50–59 |
60–69 |
|
Mean |
16.1 ± 5.4 |
15.5 ± 5.8 |
15.6 ± 4.1 |
15.8 ± 5.1 |
14.4 ± 3.1 |
0.651 |
|
< 15 |
28 (53.8) |
111 (60.7) |
32 (50.0) |
52 (51.0) |
17 (56.7) |
0.453 |
|
≥ 15 |
24 (46.2) |
72 (39.3) |
32 (50.0) |
50 (49.0) |
13 (43.3) |
|
Multiple logistic regression models of hyperhomocysteinemia according to work type
We calculated ORs and 95% CIs using multiple logistic regression analyses, to adjust for other potential confounding variables within our dataset. In comparison to daytime workers, the OR for hyperhomocysteinemia was 1.14 (95% CI: 0.64–2.03) in short-term shift workers, compared to 2.01 (95% CI: 1.14–3.54) in long-term shift workers. In model 2, after adjusting for age, the ORs for hyperhomocysteinemia in short- and long-term shift workers were 1.04 (95% CI: 0.56–1.93) and 2.17 (95% CI: 1.18–4.00), respectively. In model 3, after adjusting for age and for smoking, drinking, and regular exercise status, the OR for hyperhomocysteinemia was 1.00 (95% CI: 0.53–1.88) in short-term shift workers, compared to 2.02 (95% CI: 1.09–3.75) in long-term shift workers. In model 4, after adjusting for age; and for smoking, drinking, and regular exercise status; a family history of CVA; and BMI, the OR for hyperhomocysteinemia in short-term shift workers was 0.95 (95% CI: 0.50–1.80), compared to 2.00 (95% CI: 1.07–3.74) for long-term shift workers (
Table 4).
Table 4Multiple logistic regression model of hyperhomocysteinemia according to work type
|
Characteristics |
Model 1 |
Model 2 |
Model 3 |
Model 4 |
|
OR |
95% CI |
OR |
95% CI |
OR |
95% CI |
OR |
95% CI |
|
Type of work |
|
|
|
|
|
|
|
|
|
Daytime workers |
1.00 |
- |
1.00 |
- |
1.00 |
- |
1.00 |
- |
|
Short-term (< 10 years) shift work |
1.14 |
0.64–2.03 |
1.04 |
0.56–1.93 |
1.00 |
0.53–1.88 |
0.95 |
0.50–1.80 |
|
Long-term (≥ 10 years) shift work |
2.01 |
1.14–3.54 |
2.17 |
1.18–4.00 |
2.02 |
1.09–3.75 |
2.00 |
1.07–3.74 |
|
Age (years) |
|
|
|
|
|
|
|
|
|
20–29 |
|
|
1.00 |
- |
1.00 |
- |
1.00 |
- |
|
30–39 |
|
|
0.66 |
0.35–1.25 |
0.64 |
0.33–1.23 |
0.55 |
0.28–1.09 |
|
40–49 |
|
|
0.65 |
0.27–1.57 |
0.58 |
0.23–1.42 |
0.46 |
0.18–1.16 |
|
50–59 |
|
|
0.64 |
0.28–1.47 |
0.62 |
0.26–1.45 |
0.55 |
0.23–1.32 |
|
60–69 |
|
|
0.47 |
0.16–1.34 |
0.46 |
0.16–1.33 |
0.41 |
0.14–1.21 |
|
Smoking |
|
|
|
|
|
|
|
|
|
Never |
|
|
|
|
1.00 |
- |
1.00 |
- |
|
Past smoker |
|
|
|
|
1.14 |
0.66–1.96 |
1.16 |
0.67–2.00 |
|
Current smoker |
|
|
|
|
1.65 |
0.99–2.75 |
1.74 |
1.04–2.92 |
|
Heavy drinking |
|
|
|
|
|
|
|
|
|
No |
|
|
|
|
1.00 |
- |
1.00 |
- |
|
Yes |
|
|
|
|
1.05 |
0.68–1.61 |
0.99 |
0.64–1.54 |
|
Regular exercise |
|
|
|
|
|
|
|
|
|
No |
|
|
|
|
1.00 |
- |
1.00 |
- |
|
Yes |
|
|
|
|
1.14 |
0.76–1.72 |
1.19 |
0.78–1.81 |
|
Family history of CVA |
|
|
|
|
|
|
|
|
|
No |
|
|
|
|
|
|
1.00 |
- |
|
Yes |
|
|
|
|
|
|
0.72 |
0.36–1.44 |
|
BMI (kg/m2) |
|
|
|
|
|
|
|
|
|
< 25 |
|
|
|
|
|
|
1.00 |
- |
|
25–30 |
|
|
|
|
|
|
1.71 |
1.12–2.61 |
|
≥ 30 |
|
|
|
|
|
|
2.01 |
0.96–4.21 |
DISCUSSION
The major finding of this study was that the risk of hyperhomocysteinemia was significantly higher for long-term shift workers compared to their day-time counterparts. Numerous independent risk factors for cardiovascular disease, such as smoking, SBP, and TG, were also significantly more prevalent in shift workers compared to daytime workers. Other covariates, including mean age, hypertension, DM, family history of CVA, smoking, SBP, DBP, TG, fasting glucose level, and HbA1C were all significantly higher in long-term shift workers compared with daytime workers. Importantly, the increase in hyperhomocysteinemia among long-term shift workers compared to daytime workers remained statistically significant even after adjusting for these cofactors. Hyperhomocysteinemia increases the risk of cardiovascular disease. In other words, this study confirmed that long-term shift work increases the risk of cardiovascular disease. These results are consistent with the conclusion of Bøggild et al. [
4] who found that the pathological mechanism underlying the association between hyperhomocysteinemia and cardiovascular disease was changes in the natural circadian rhythms brought about by irregular sleep. Furthermore, with the appearance of hyperglycemia, other conditions, such as dyslipidemia and abdominal obesity, may occur due to changes in normal lipid and carbohydrate metabolism. In addition, greater consumption of coffee, cigarettes, alcohol, hypnotic drugs, and a sedentary lifestyle may arise as a result of altered social and family support, as perceived by these workers due to their irregular work hours.
Although shift work and homocysteine levels are both independent risk factors for cardiovascular disease, few studies have directly examined homocysteine levels among shift workers. In 2003, a study examined homocysteine levels in a cohort of bus drivers consisting of 30 male shift workers and 22 control daytime workers in Brazil. Shift working bus drivers had significantly higher plasma homocysteine levels compared to the control group (18.57 vs. 9.43 μmol) [
14]. A similar study of workers at the Israel Electric Company in 2007 assessed 129 shift workers and 173 daytime workers for serum factors, including homocysteine. The mean level of homocysteine in shift workers who complained about sleep disturbances and were over 40 years of age was 19.54 mmol/L, with one-third of workers exhibiting plasma homocysteine concentrations > 15 mmol/L, indicative of hyperhomocysteinemia [
15]. In this study, there was no difference in mean homocysteine concentrations between the shift work or age groups, although the risk of hyperhomocysteinemia was significantly higher in long-term shift workers compared to their daytime counterparts.
Homocysteine is an independent risk factor for cardiovascular disease, similar to other factors, such as blood lipids, diabetes, and hypertension. In 1969, after McCully [
16] published results describing the autopsy of a child with hyperhomocysteinemia and hyperhomocysteinuria as a result of systemic atherosclerosis, numerous studies examining the toxicity of homocysteine in the vascular system have been carried out. Hyperhomocysteinemia has been shown to affect arterial wall remodeling, which could lead to vascular damage. Furthermore, elevated homocysteine levels may enhance oxidative stress and inflammation of vascular endothelial cells, reducing the production and bioavailability of nitric oxide, a strong vasodilator produced by the endothelium. Alternatively, the enhanced arterial stiffness seen in hyperhomocysteinemia may be attributed to the effects of homocysteine atherogenesis, via the production of small particles of low-density lipoprotein [
17]. These effects, along with other factors, constitute strong evidence that oxidation is a major factor underlying the effects of increased homocysteine on atherosclerosis [
18]. Given this litany of deleterious effects on vascular function, homocysteine is now considered an independent risk factor for cardiovascular disease. This was well supported by a systematic review and meta-analysis, which found that an increase in the homocysteine level of 5 μmol/L was associated with an almost 20% increase in disease morbidity, independent of other risk factors for coronary heart disease [
19]. Significant associations between homocysteine and clinical outcomes are usually observed for homocysteine levels greater than 15 μmol/L [
20]; however, there is evidence of a continuous dose-dependent effect, with no apparent threshold concentration for most conditions [
21]. In this study, hyperhomocysteinemia was defined as a homocysteine level above 15 μmol/L [
13], as suggested by the AHA guidelines.
Several factors related to homocysteine levels have been documented. Age, male sex, smoking, coffee consumption, high blood pressure, unfavorable lipid profile, high creatinine level, and methyltetrahydrofolate reductase (MTHFR) gene expression are all factors associated with increased homocysteine levels, while physical activity, moderate alcohol consumption, and a good folate or vitamin B
12 status have been associated with lower homocysteine levels [
22]. Given these risk factors for increased homocysteine levels, there are a number of possible explanations for the increased prevalence of hyperhomocysteinemia in long-term shift workers.
Shift work is stressful and associated with continuous desynchronization and readjustment of circadian rhythms by the hypothalamus [
23]. A previous study demonstrated a 24-hour oscillation in plasma homocysteine concentrations, with a nocturnal peak and a daytime nadir [
24]. Although the exact times were not recorded, most health checks and blood sampling were conducted between 08:00 and 11:00. Interruption of the sleep/wake cycle can alter the overall increase in homocysteine concentrations or move the nocturnal peak to morning hours [
15]. Also, exposure to light at any time suppresses pineal melatonin production in humans [
25]. Of note, increased plasma concentrations of homocysteine and decreased melatonin levels have been reported in rats after pinealectomy, while exogenous melatonin treatment restored basal concentrations [
26]. Thus, a shift work-related decrease in melatonin secretion may also contribute to increased plasma homocysteine concentrations.
In considering the relationship between shift work and clinical outcomes, it is important to determine whether shift work itself is merely a trigger for other lifestyle-related health effects related to coronary heart disease. Risk factors of deleterious socio-temporal patterns and behaviors, including smoking, diet, alcohol, and exercise levels, are all significantly more common among shift workers [
21,
27], and may themselves lead to cardiovascular disease [
4]. As smoking and coffee consumption increase homocysteine, they have a greater impact on the rise of homocysteine levels in shift workers [
28,
29]. In this study, coffee consumption, heavy drinking, and regular exercise levels did not differ significantly between shift workers and controls, although the proportion of current smokers was significantly higher in the former group. It is therefore possible that some lifestyle habits associated with shift work may contribute to changes in homocysteine levels.
While homocysteine production is important, degradation of this compound is equally important for determining baseline plasma concentrations. Under normal conditions, homocysteine is metabolized by two major pathways. When methionine is excessive, homocysteine is directed to the transsulfuration pathway, where it is irreversibly conjugated to cysteine by cystathionine B-synthase with vitamin B
6 as a cofactor. Alternatively, homocysteine can also be remethylated in a methionine-conserving pathway. This process requires methionine synthase, vitamin B
12 as a cofactor, and methyltetrahydrofolate as a co-substrate. The methionine-conserving pathway requires folic acid and MTHFR [
27]. Deficiencies in any of the above enzymes, folic acid, or the cofactors may lead to some degree of hyperhomocysteinemia [
30]. As shift workers generally have shorter meal times and are more likely to eat out, they are also more likely to choose convenient foods rich in carbohydrates and lipids. Furthermore, unlike a diet rich in vegetables and fruit, the foods they consume do not contain adequate amounts of B vitamins and folic acids, which can result in increased homocysteine levels.
In general, serum homocysteine levels > 15 μmol/L are considered clinically abnormal; this threshold was therefore chosen as the baseline for determining hyperhomocysteinemia in this study [
13,
20]. The percentage of workers in this study with hyperhomocysteinemia was 44%, reaching as high as 52.9% in the long-term shift work group. Data from the Framingham study showed that the prevalence of hyperhomocysteinemia was 29.3% for the entire cohort [
31]. In another study examining 103 healthy college students in South Korea, hyperhomocysteinemia was observed in 44% of all students, including 54% of males [
32]. While the concentrations of homocysteine observed in this study did seem to be a little higher than expected, these levels were not significantly different from previous studies. One explanation for this apparent discrepancy may be that homocysteine levels are typically higher in men than in women [
21,
33]. Since this study examined only male workers, the rate of hyperhomocysteinemia is likely not reflective of the population as a whole.
In general, the factors affecting cardiovascular diseases are highly correlated with age. Furthermore, workers who have performed shift work for long periods are invariably older than their less-experienced coworkers. For this reason, increased homocysteine levels might be thought of as an effect of age rather than of shift work. However, on analyzing the rates of hyperhomocysteinemia and homocysteine concentrations by age, we found no significant difference among groups. Therefore, we were able to control for the effects of age effectively, enabling us to conclude that the prevalence of hyperhomocysteinemia was significantly higher among long-term shift workers.
This study enrolled subjects from representative departments of a large corporation (i.e., only mill and rolling departments) to increase the homogeneity of the study group. Since the type of work can vary depending on individual and company circumstances, it is necessary to minimize any effects not associated with shift schedule. By adjusting our inclusion criteria, we were able to increase the comparability among groups. Also, the shift history of shift workers over the previous 3 years was confirmed independent of study questionnaires. Daytime workers who had performed shift work in the previous 3 years were excluded from the daytime worker group, allowing us to minimize the effects of previous shift work.
Despite these strengths, this study had some limitations that should be considered when evaluating the results. First, we did not adequately control for some potentially relevant factors associated with hyperhomocysteinemia, particularly workers' diets, which are associated with hyperhomocysteinemia. Hyperhomocysteinemia levels are also related to vitamin B
12, methyltetrahydrofolate and folic acid deficiency [
30]. In this study, information on nutritional deficiency could not be confirmed; however, it was considered unlikely that the workers would exhibit any nutritional deficiencies associated with hyperhomocysteinemia, as all study participants were employees of a large corporation and were not expected to have a low socioeconomic status. Further studies need to consider factors that play important roles in homocysteine metabolism, along with diet information on vitamin B
12, folic acid intake, and the genetics of methyltetrahydrofolate metabolism. While daytime workers with a history of shift work were excluded, we were unable to completely exclude the possibility of previous shift work among current daytime workers. Worker screening included confirmation of work history, as well as determining whether the individual had undergone a medical health examination for night work in the previous 3 years. However, we were unable to confirm whether workers had engaged in shift work previously based on company records. Finally, this study was limited by the cross-sectional nature of its design, as it was based on observational data obtained from health checkups conducted by a single company. Although an association between shift work and hyperhomocysteinemia was confirmed, it remains difficult to draw any definitive conclusion regarding causality.
CONCLUSIONS
This study investigated the relationship between shift work and plasma homocysteine levels, and found that homocysteine levels were higher in shift workers than in their daytime counterparts, particularly those with a long history of shift work. This suggests that long-term shift work may increase the risk of cardiovascular disease. More active prevention and disease-management strategies may therefore be necessary to reduce the risk of cardiovascular disease in shift workers.
Abbreviations
American Heart Association
methyltetrahydrofolate reductase
low-density lipoprotein-cholesterol
high-density lipoprotein-cholesterol
NOTES
-
Competing interests: The authors declare that they have no competing interests.
-
Availability of data and materials: The datasets analyzed during the current study are not publicly available because they included the personal information of the examinees but are available from the corresponding author on reasonable request.
-
Authors contributions:
Conceptualization: Kang D, Kwak K, Kang SK.
Formal analysis: Kang D, Kwak K.
Investigation: Kang D, Choi WJ, Lee SH, Lee JH.
Supervision: Kwak K.
Writing - original draft: Kang D, Kwak K, Kang SK.
Writing - review & editing: Choi WJ, Lee SH, Lee JH, Kang SK.
REFERENCES
REFERENCES
- 1. International Labor Office. C171 - Night work convention. Geneva: International Labor Office; 1990.
- 2. Dinavahi R, Falkner B. Relationship of homocysteine with cardiovascular disease and blood pressure. J Clin Hypertens (Greenwich) 2004;6(9):494–498. 15365276.ArticlePubMedPMCPDF
- 3. Harrington JM. Health effects of shift work and extended hours of work. Occup Environ Med 2001;58(1):68–72.ArticlePMC
- 4. Bøggild H, Knutsson A. Shift work, risk factors and cardiovascular disease. Scand J Work Environ Health 1999;25(2):85–99. 10360463.ArticlePubMed
- 5. Torquati L, Mielke GI, Brown WJ, Kolbe-Alexander T. Shift work and the risk of cardiovascular disease. A systematic review and meta-analysis including dose-response relationship. Scand J Work Environ Health 2018;44(3):229–238. 29247501.ArticlePubMed
- 6. Puttonen S, Kivimäki M, Elovainio M, Pulkki-Råback L, Hintsanen M, Vahtera J, et al. Shift work in young adults and carotid artery intima-media thickness: the Cardiovascular Risk in Young Finns study. Atherosclerosis 2009;205(2):608–613. 19215924.ArticlePubMed
- 7. Selhub J. Homocysteine metabolism. Annu Rev Nutr 1999;19:217–246. 10448523.ArticlePubMed
- 8. Veerkamp MJ, de Graaf J, den Heijer M, Blom HJ, Stalenhoef AF. Plasma homocysteine in subjects with familial combined hyperlipidemia. Atherosclerosis 2003;166(1):111–117. 12482557.ArticlePubMed
- 9. McDowell IF, Lang D. Homocysteine and endothelial dysfunction: a link with cardiovascular disease. J Nutr 2000;130(2S):Suppl. 369S–372S. 10721909.ArticlePubMed
- 10. van der Griend R, Biesma DH, Banga JD. Hyperhomocysteinaemia as a cardiovascular risk factor: an update. Neth J Med 2000;56(3):119–130. 10759023.ArticlePubMed
- 11. Datta S, Pal SK, Mazumdar H, Bhandari B, Bhattacherjee S, Pandit S. Homocysteine and cerebrovascular accidents. J Indian Med Assoc 2009;107(6):345–346. 19886370.PubMed
- 12. Taylor LM Jr. Elevated plasma homocysteine as risk factor for peripheral arterial disease--what is the evidence? Semin Vasc Surg 2003;16(3):215–222. 12975761.ArticlePubMed
- 13. Maron BA, Loscalzo J. The treatment of hyperhomocysteinemia. Annu Rev Med 2009;60:39–54. 18729731.ArticlePubMedPMC
- 14. Martins PJ, D'Almeida V, Vergani N, Perez AB, Tufik S. Increased plasma homocysteine levels in shift working bus drivers. Occup Environ Med 2003;60(9):662–666. 12937187.ArticlePubMedPMC
- 15. Lavie L, Lavie P. Elevated plasma homocysteine in older shift-workers: a potential risk factor for cardiovascular morbidity. Chronobiol Int 2007;24(1):115–128. 17364583.ArticlePubMed
- 16. McCully KS. Vascular pathology of homocysteinemia: implications for the pathogenesis of arteriosclerosis. Am J Pathol 1969;56(1):111–128. 5792556.PubMedPMC
- 17. Zhang S, Bai YY, Luo LM, Xiao WK, Wu HM, Ye P. Association between serum homocysteine and arterial stiffness in elderly: a community-based study. J Geriatr Cardiol 2014;11(1):32–38. 24748879.PubMedPMC
- 18. Shenoy V, Mehendale V, Prabhu K, Shetty R, Rao P. Correlation of serum homocysteine levels with the severity of coronary artery disease. Indian J Clin Biochem 2014;29(3):339–344. 24966483.ArticlePubMedPMCPDF
- 19. Humphrey LL, Fu R, Rogers K, Freeman M, Helfand M. Homocysteine level and coronary heart disease incidence: a systematic review and meta-analysis. Mayo Clin Proc 2008;83(11):1203–1212. 18990318.ArticlePubMed
- 20. Guo H, Chi J, Xing Y, Wang P. Influence of folic acid on plasma homocysteine levels & arterial endothelial function in patients with unstable angina. Indian J Med Res 2009;129(3):279–284. 19491420.PubMed
- 21. Refsum H, Nurk E, Smith AD, Ueland PM, Gjesdal CG, Bjelland I, et al. The Hordaland Homocysteine Study: a community-based study of homocysteine, its determinants, and associations with disease. J Nutr 2006;136(6):Suppl. 1731S–1740S. 16702348.ArticlePubMed
- 22. Härmä MI, Ilmarinen JE. Towards the 24-hour society--new approaches for aging shift workers? Scand J Work Environ Health 1999;25(6):610–615. 10884161.ArticlePubMed
- 23. Haus E, Smolensky M. Biological clocks and shift work: circadian dysregulation and potential long-term effects. Cancer Causes Control 2006;17(4):489–500. 16596302.ArticlePubMedPDF
- 24. Bremner WF, Holmes EW, Kanabrocki EL, Hermida RC, Ayala D, Garbincius J, et al. Circadian rhythm of serum total homocysteine in men. Am J Cardiol 2000;86(10):1153–1156. A9–1110. 11074221.ArticlePubMed
- 25. Zeitzer JM, Dijk DJ, Kronauer R, Brown E, Czeisler C. Sensitivity of the human circadian pacemaker to nocturnal light: melatonin phase resetting and suppression. J Physiol 2000;526 Pt 3:695–702. 10922269.ArticlePubMedPMCPDF
- 26. Baydas G, Gursu MF, Cikim G, Canatan H. Homocysteine levels are increased due to lack of melatonin in pinealectomized rats: is there a link between melatonin and homocysteine? J Pineal Res 2002;32(1):63–64. 11841603.ArticlePubMedPDF
- 27. Finkelstein JD. The metabolism of homocysteine: pathways and regulation. Eur J Pediatr 1998;157(Suppl 2):S40–S44. 9587024.ArticlePubMedPDF
- 28. Verhoef P, Pasman WJ, Van Vliet T, Urgert R, Katan MB. Contribution of caffeine to the homocysteine-raising effect of coffee: a randomized controlled trial in humans. Am J Clin Nutr 2002;76(6):1244–1248. 12450889.ArticlePubMed
- 29. Haj Mouhamed D, Ezzaher A, Neffati F, Douki W, Najjar MF. Effect of cigarette smoking on plasma homocysteine concentrations. Clin Chem Lab Med 2011;49(3):479–483. 21143017.ArticlePubMed
- 30. Ford ES, Smith SJ, Stroup DF, Steinberg KK, Mueller PW, Thacker SB. Homocyst(e)ine and cardiovascular disease: a systematic review of the evidence with special emphasis on case-control studies and nested case-control studies. Int J Epidemiol 2002;31(1):59–70. 11914295.ArticlePubMed
- 31. Selhub J. The many facets of hyperhomocysteinemia: studies from the Framingham cohorts. J Nutr 2006;136(6):Suppl. 1726S–1730S. 16702347.ArticlePubMed
- 32. Kim JS, Park EJ, Min HS, Kang MH. Relationships of plasma homocysteine concentration and oxidative stress markers in Korean collage students. Korean J Nutr 2010;43(5):443–452.Article
- 33. Nygård O, Vollset SE, Refsum H, Stensvold I, Tverdal A, Nordrehaug JE, et al. Total plasma homocysteine and cardiovascular risk profile. The Hordaland Homocysteine Study. JAMA 1995;274(19):1526–1533. 7474221.ArticlePubMed
 , Seong-Kyu Kang2, Won-Jun Choi2, Sang Ha Lee1
, Seong-Kyu Kang2, Won-Jun Choi2, Sang Ha Lee1 , Jun-Hyung Lee1
, Jun-Hyung Lee1 , Kyeongmin Kwak3,4
, Kyeongmin Kwak3,4

 KSOEM
KSOEM

 Cite
Cite

