Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 29; 2017 > Article
- Research Article Factors affecting heat-related diseases in outdoor workers exposed to extreme heat
-
Jungsun Park1, Yangho Kim2,3
 , Inbo Oh2
, Inbo Oh2 -
Annals of Occupational and Environmental Medicine 2017;29:30.
DOI: https://doi.org/10.1186/s40557-017-0183-y
Published online: June 29, 2017
1Department of Occupational Health, Catholic University of Daegu, Gyeongsan, South Korea
2Environmental Health Center, University of Ulsan College of Medicine, Ulsan, South Korea
3Department of Occupational and Environmental Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, 877 Bangeojinsunhwando-ro, Dong-gu, Ulsan, 44033 South Korea
© The Author(s). 2017
Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Abstract
-
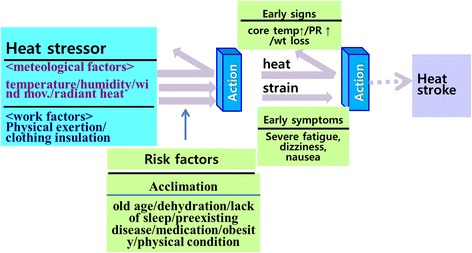
Background The objectives of the present study are to: (i) evaluate the effect of environmental and metabolic heat on heat-related illnesses in outdoor workers; and (ii) evaluate the effect of personal factors, including heat acclimation, on the risk of heat-related illnesses in outdoor workers.
-
Methods We identified 47 cases of illnesses from exposure to environmental heat in outdoor workers in Korea from 2010 to 2014, based on review of workers’ compensation data. We also obtained the information on location, time, and work environment of each heat-related illness.
-
Results Our major results are that 29 cases (61.7%) occurred during a heat wave. Forty five cases (95.7%) occurred when the maximum estimated WBGT (WBGTmax) was equal to or greater than the case specific threshold value which was determined by acclimatization and metabolic rate. Twenty two cases (46.8%) were not acclimated to the heat. Thirty-seven cases (78.7%) occurred after tropical night (temperature above 25 °C), during which many people may find it hard to sleep.
-
Conclusion Personal risk factors such as heat acclimation as well as environmental factors and high metabolic rate during work are the major determinants of heat-related illnesses.
Background
Methods
Results
Discussion
Conclusion
Acknowledgements
Abbreviations
ACGIH
ASOS
AWS
NIOSH
OSHA
RAL
REL
REM
RH
SWS
Ta
TLV
Tw
WBGT
- 1. Nichols AW. Heat-related illness in sports and exercise. Curr Rev Musculoskelet Med 2014;7:355–365. 10.1007/s12178-014-9240-0. 25240413.ArticlePubMedPMCPDF
- 2. Lucas RA, Epstein Y, Kjellstrom T. Excessive occupational heat exposure: a significant ergonomic challenge and health risk for current and future workers. Extrem Physiol Med 2014;3:14. 10.1186/2046-7648-3-14. 25057350.ArticlePubMedPMCPDF
- 3. Garzon-Villalba XP, Mbah A, Wu Y, Hiles M, Moore H, Schwartz SW, et al. Exertional heat illness and acute injury related to ambient wet bulb globe temperature. Am J Ind Med 2016;59:1169–1176. 10.1002/ajim.22650. 27779310.ArticlePubMed
- 4. Minard D, Copman L. In: Hardy JD, editor. Elevation of body temperature in disease. Temperature: its measurement and control in science and industry. 1963, New York: Reenhold Co..
- 5. Leithead CS, Lind AR. Heat stress and heat disorders. 1964, London: Cassell.
- 6. Minard D. In: National Institute for Occupational Safety and Health, United States Public Health Service, Division of Occupational Health, editor. Physiology of heat stress. The occupational environment: its evaluation & control. 1973, 3rd. Washington, DC: U.S. Government Printing Office.
- 7. Lind AR. In: DHK L, Falk HL, Murphy SD, American Physiological Society, editors. Human tolerance to hot climates. Handbook of physiology: a critical, comprehensive presentation of physiological knowledge and concepts. 1977, American Physiological Society: Bethesda.ArticlePDF
- 8. Dinman BD, Horvath SM. Heat disorders in industry: a reevaluation of diagnostic criteria. J Occup Med 1984;26:489–495. 6747736.PubMed
- 9. Springer K. If you can’t stand the heat. Ohio Monitor 1985;58:4–9.
- 10. CDC. Heat-related deaths among crop workers-United States, 1992–2006. 2008, 649–653.
- 11. Ramsey JD, Burford CL, Beshir MY, Jensen RC. Effects of workplace thermal conditions on safe work behavior. J Saf Res 1983;14:105–114. 10.1016/0022-4375(83)90021-X.Article
- 12. Fogleman M, Fakhrzadeh L, Bernard TE. The relationship between outdoor thermal conditions and acute injury in an aluminum smelter. Int J Ind Ergon 2005;35:47–55. 10.1016/j.ergon.2004.08.003.Article
- 13. Schulte PA, Bhattacharya A, Butler CR, Chun HK, Jacklitsch B, Jacobs T, et al. Advancing the framework for considering the effects of climate change on worker safety and health. J Occup Environ Hyg 2016;13:847–846. 10.1080/15459624.2016.1179388. 27115294.ArticlePubMedPMC
- 14. Schulte PA, Chun H. Climate change and occupational safety and health: establishing a preliminary framework. J Occup Environ Hyg 2009;6:542–554. 10.1080/15459620903066008. 19551548.ArticlePubMed
- 15. Henschel A, Burton LL, Margolies L, Smith JE. An analysis of the heat deaths in St. Louis during July, 1966. Am J Public Health Nations Health 1969;59:2232–2242. 10.2105/AJPH.59.12.2232. 5389506.ArticlePubMedPMC
- 16. Ellis FP. Mortality from heat illness and heat-aggravated illness in the United States. Environ Res 1972;5:1–58. 10.1016/0013-9351(72)90019-9. 4555874.ArticlePubMed
- 17.
- 18. NIOSH. Criteria for a recommended standard. Occupational exposure to heath and hot environments. 2016, Cincinnati: DHHS (NIOSH).
- 19. ISO. Estimation of the heat stress on working man, based on the WBGT-index. 1989.
- 20. Kenny GP, Yardley J, Brown C, Sigal RJ, Jay O. Heat stress in older individuals and patients with common chronic diseases. CMAJ 2010;182:1053–1060. 10.1503/cmaj.081050. 19703915.ArticlePubMedPMC
- 21. Taylor NAS, Kondo N, Kenny WL. In: Taylor NAS, Groeller H, editors. The physiology of acute heat exposure, with implications for human performance in the heat. Physiological bases of human performance during work and exercise. 2008, 1st. Edinburgh: Elsevier.
- 22. Wright HE, Larose J, McLellan TM, Hardcastle SG, Boulay P, Kenny GP. Moderate-intensity intermittent work in the heat results in similar low-level dehydration in young and older males. J Occup Environ Hyg 2014;11:144–153. 10.1080/15459624.2013.817676. 24521064.ArticlePubMed
- 23. Epstein Y, Albukrek D, Kalmovitc B, Moran DS, Shapiro Y. Heat intolerance induced by antidepressants [case report]. Ann N Y Acad Sci 1997;813:553–558. 10.1111/j.1749-6632.1997.tb51746.x. 9100934.PubMed
- 24. Moran DS, Erlich T, Epstein Y. The heat tolerance test: an efficient screening tool for evaluating susceptibility to heat [case report]. J Sport Rehabil 2007;16:215–221. 10.1123/jsr.16.3.215. 17923727.ArticlePubMed
- 25. DOD. Technical bulletin: heat stress control and heat casualty management. 2003, Washington, DC: Departments of the U.S. Army, Navy, and Air Force.
- 26. Khagali M, Hayes JSR. Heatstroke and temperature regulation. 1983, Sydney: Academic Press.
- 27. Redmond CK, Emes JJ, Mazumdar S, Magee PC, Kamon E. Mortality of steelworkers employed in hot jobs. J Environ Pathol Toxicol 1979;2:75–96. 512565.PubMed
- 28. Dukes-Dobos FN. Hazards of heat exposure: a review. Scand J Work Environ Health 1981;7:73–83. 10.5271/sjweh.2560. 7031869.ArticlePubMed
- 29. McArdle WD, Katch FI, Katch VI. Exercise at medium and high altitude. 1996, 4. Williams & Wilkins: Baltimore.
- 30. Williams WJ, Schneider SM, Stuart CA, Gretebeck RJ, Lane HW, Whitson PA. Effect of dietary sodium and fluid/electrolyte regulation in humans during bed rest. Aviat Space Environ Med 2003;74:37–46. 12546297.PubMed
- 31. Kim SH, Jo SN, Myung HN, Jang JY. The effect of pre-existing medical conditions on heat stroke during hot weather in South Korea. Environ Res 2014;133:246–252. 10.1016/j.envres.2014.06.003. 24981822.ArticlePubMed
- 32. Cho WY. Exercise induced heat stroke and acute renal failure. Korean J Med 2002;62:365–368.
- 33. Lee S-H, Yoo T-H, Kim B-H, K-g K. Exertional heat stroke: clinical characteristics and courses of 15 patients. Korean J Med 2012;62:379–389.
- 34. Choi WJ, Jae Wook Lee JW, Lee SW. Exertional heat stroke in a young man with multi-organ dysfunction and fulminant pneumonia. Korean J Emerg Med 2009;20:458–462.
- 35. Park SW, Cho YL, Oh DH, Choe JY, Jun HR. A case of heat stroke in an aluminium utensil plant. Korean J Occup Environ Med 1999;11:293–303.ArticlePDF
- 36. Na W, Jang JY, Lee KE, Kim H, Jun B, Kwon J-W, et al. The effects of temperature on heat-related illness according to the characteristics of patients during the summer of 2012 in the Republic of Korea. J Prev Med Public Health 2013;46:19–27. 10.3961/jpmph.2013.46.1.19. 23407385.ArticlePubMedPMC
- 37. Kim H, Ha JS, Park J. High temperature, heat index, and mortality in 6 major cities in South Korea. Arch Environ Occup Health 2006;61:265–270. 10.3200/AEOH.61.6.265-270. 17967749.ArticlePubMed
- 38. Lee WK, Lee HA, Park H. Modifying effect of heat waves on the relationship between temperature and mortality. J Korean Med Sci 2016;31:702–708. 10.3346/jkms.2016.31.5.702. 27134490.ArticlePubMedPMCPDF
- 39. Lee S, Kim H, Yi SM. The relationships between temperature changes and mortality in Seoul, Korea. J Environ Health Sci 2010;36:20–26.Article
- 40. Chung JY, Honda Y, Hong YC, Pan XC, Guo YL, Kim H. Ambient temperature and mortality: an international study in four capital cities of East Asia. Sci Total Environ 2009;408:390–396. 10.1016/j.scitotenv.2009.09.009. 19853280.ArticlePubMed
- 41. Korea Occupational Safety and Health Agency. Statistics on workers’ compensation. 2015.
- 42. Korea Meteorological Administration Forum on Heat Wave. Still killer, current status and measures. 2015.
- 43. Lee E, Park J, Kim H, Park M. Report on the development of Meterological information in Daily Living Life. Korea Meteorological Administration. 2016.
- 44. Buguet A. Sleep under extreme environments: effects of heat and cold exposure, altitude, hyperbaric pressure and microgravity in space. J Neurol Sci 2007;262:145–152. 10.1016/j.jns.2007.06.040. 17706676.ArticlePubMed
- 45. Haskell EH, Palca JW, Walker JM, Berger RJ, Heller HC. The effects of high and low ambient temperatures on human sleep stages. Electroencephalogr Clin Neurophysiol 1981;51:494–501. 10.1016/0013-4694(81)90226-1. 6165549.ArticlePubMed
- 46. Okamoto-Mizuno K, Mizuno K. Effects of thermal environment on sleep and circadian rhythm. J Physiol Anthropol 2012;31:14. 10.1186/1880-6805-31-14. 22738673.ArticlePubMedPMCPDF
- 47. http://www.osha.gov/dts/osta/otm/otm_iii/otm_iii_4.html.
- 48. Havenith G. Heat balance when wearing protective clothing. Ann Occup Hyg 1999;43:289–296. 10.1016/S0003-4878(99)00051-4. 10481628.ArticlePubMed
- 49. Bernard TE, Barrow CA. Empirical approach to outdoor WBGT from meteorological data and performance of two different instrument designs. Ind Health 2013;51:79–85. 10.2486/indhealth.2012-0160. 23385431.ArticlePubMed
- 50. ISO. Ergonomics of the thermal environment: estimation of thermal insulation and water vapour resistance of a clothing ensemble. 2007, Geneva: ISO.
- 51. Goldman RF. Clothing, its physiological effects, adequacy in extreme thermal environments, and possibility of future improvements. Arch Sci Physiol (Paris) 1973;27:137–147. 4807365.PubMed
- 52. McCullough EA, Arpin EJ, Jones B, Konz SA, Rohles FH. Heat transfer characteristics of clothing worn in hot industrial environments. ASHRAE, Journal of the American Society of Heating Refrigerating and Air-Conditioning Engineers 1982;88:1077–1094.
- 53. Vogt JJ, Candas V, Libert JP. Graphical determination of heat tolerance limits. Ergonomics 1982;25:285–294. 10.1080/00140138208924955. 7128562.ArticlePubMed
- 54. Armstrong LE, Casa DJ, Millard-Stafford M, Moran DS, Pyne SW, Roberts WO. American College of Sports Medicine position stand: exertional heat illness during training and competition. Med Sci Sports Exerc 2007;39:556–572. 10.1249/MSS.0b013e31802fa199. 17473783.PubMed
- 55. d'Ambrosio Alfano FR, Malchaire J, Palella BI, Riccio G. WBGT index revisited after 60 years of use. Ann Occup Hyg 2014;58:955–970. 25062982.PubMed
- 56. Arbury S, Jacklitsch B, Farquah O, Hodgson M, Lamson G, Martin H, et al. Heat illness and death among workers: United States, 2012–2013. MMWR Morb Mortal Wkly Rep 2014;63:661–665. 25102413.PubMedPMC
- 57. Navy Environmental Health Center. Prevention and treatment of heat and cold stress injuries. 2007, Navy Environmental Health Center, Bureau of Medicine and Surgery: Portsmouth.
- 58. Pandolf KB, Burse RL, Goldman RF. Role of physical fitness in heat acclimatization, decay and reinduction. Ergonomics 1977;20:399–408. 10.1080/00140137708931642. 908323.ArticlePubMed
- 59. Yeargin SW, Casa DJ, Armstrong LE, Watson G, Judelson DA, Psathas E, et al. Heat acclimatization and hydration status of American football players during initial summer workouts. J Strength Cond Res 2006;20:463–470. 16937956.ArticlePubMed
- 60. NIOSH. Criteria for a recommended standard: occupational exposure to hot environments. 1972, Cincinnati: U.S. Department of Health, Education, and Welfare, Health Services and Mental Health Administration, National Institute for Occupational Safety and Health, DHEW (NIOSH) Publication No. HSM 72–10269.
- 61. NIOSH. Criteria for a recommended standard: occupational exposure to hot environments: revised criteria. 1986, Cincinnati: U.S. Department of Health and Human Services, Centers for Disease Control, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 86–113.
- 62. AIHA. In: 2nd, editor. The occupational environment: its evaluation, control, and management. 2003, Fairfax: AIHA Press.
- 63. Gabriel KMA, Endlicher WR. Urban and rural mortality rates during heat waves in Berlin and Brandenburg, Germany. Environ Pollut 2011;159:2044–2050. 10.1016/j.envpol.2011.01.016. 21295389.ArticlePubMed
- 64. ISO. Ergonomics: evaluation of thermal strain by physiological measurements. 2004, Geneva: ISO.
REFERENCES
Figure & Data
REFERENCES
Citations

- An Umbrella Review of Systematic Reviews and Meta-Analyses on Occupational Heat Exposure, Health Risks, and Productivity Losses Globally
Aditya Nath, Subhashis Sahu, Jason Kai Wei Lee
Current Environmental Health Reports.2026;[Epub] CrossRef - Occupational heat stress and adaptation among outdoor workers: a narrative review of global evidence and policy responses
Nisha Bhati, Ankit Sheth
International Journal of Biometeorology.2026;[Epub] CrossRef - Impacts of heat on sleep quality among heat-exposed workers: a systematic review
Maarthi Raja, Vidhya Venugopal, D. C. Mathangi, Suvarna Jyothi Kantipudi, K. Mahesh Kumar, Somnath Panda, Latha Perumal Kamalakkannan
Annals of Occupational and Environmental Medicine.2026; 38: e3. CrossRef - Heat strain in road construction workers during the summer in New Mexico: a preliminary study
Jonathan W Specht, Serena Garcia, David H Wegman, Jason Glaser, Zachary J Schlader, Fabiano T Amorim
Annals of Work Exposures and Health.2025; 69(2): 225. CrossRef - Heat stress in landfill environments: Evaluating worker exposure and occupational risks
Azham Umar Abidin, Anisful Lailil Munawaroh, Aulia Rosinta, Arvi Tri Sulistiyani
Case Studies in Chemical and Environmental Engineering.2025; 11: 101097. CrossRef - Heat impacts on health and productivity: the case of two ready-made garment factories in tropical Bangladesh
Farzana Yeasmin, Aaron J. E. Bach, Jean P. Palutikof, Fahim Tonmoy, Fahmida Tofail, Mahbubur Rahman, Shannon Rutherford
Environmental and Occupational Health Practice.2025; 7(1): n/a. CrossRef - Association between climate change and impacts of heat stress among mining employees: a systematic review and meta-analysis
Mahdi Jafari Nodoushan, Ali Jafari, Mostafa Jafari Zaveh, Nafiseh Nasirzadeh, Farideh Golbabaei
Journal of Public Health.2025;[Epub] CrossRef - Development of the equivalent air temperature index (EATI) among male workers under hot and dry and hot and humid climatic conditions
Saeid Yazdanirad, Milad Abbasi, Tahere Eskandari
BMC Public Health.2025;[Epub] CrossRef - Heat stress and strain in commercial construction workers in the summer: A pilot study
Jonathan W. Specht, Serena A. Garcia, Erica Tourula, M. Jo Hite, Charlie Walker, Hillary A. Yoder, David H. Wegman, Jason Glaser, Zachary J. Schlader, Fabiano T. Amorim
Journal of Occupational and Environmental Hygiene.2025; 22(10): 807. CrossRef - Climate Change and Occupational Risks in Outdoor Workers: A Systematic Review of the Health Effects of Extreme Temperatures
Maria Francesca Rossi, Raimondo Leone, Umberto Moscato
Atmosphere.2025; 16(7): 839. CrossRef - Heat stress risk assessment of farmers working in a hot environment: What about in Zambia?
Anayawa Nyambe, Edwell S Mwaanga, Allan Mayaba Mwiinde, Charles Michelo
The Journal of Climate Change and Health.2025; 24: 100457. CrossRef - “Heat is a danger to my health even though I said I am used to it”: Qualitative insights of workplace heat among community health workers and health promoters in Kenya
Teresia Wamuyu Maina, Chelsea Williams, Thomas Jaenisch, Till Bärnighausen, Astrid Berner-Rodoreda, Kate Bärnighausen, Sari Kovats
PLOS Climate.2025; 4(12): e0000748. CrossRef - Climate change and heat stress resilient outdoor workers: findings from systematic literature review
Peymaneh Habibi, Jaleh Razmjouei, Amirhossein Moradi, Farank Mahdavi, Saeed Fallah-Aliabadi, Ahad Heydari
BMC Public Health.2024;[Epub] CrossRef - Augmented human thermal discomfort in urban centers of the Arabian Peninsula
Safi Ullah, Abdullah Aldossary, Waheed Ullah, Sami G. Al-Ghamdi
Scientific Reports.2024;[Epub] CrossRef - Heat exposure and coping strategies for food delivery riders under urban heat extremes
Lanfei Jiang, Junqi Wang, Raúl Castaño-Rosa, Chen Zhong, Shi-jie Cao
Energy and Buildings.2024; 322: 114693. CrossRef - Coping with extreme heat: current exposure and implications for the future
Charles A Weitz
Evolution, Medicine, and Public Health.2024; 12(1): 156. CrossRef - Occupational heat stress and its health impacts- an overview of research status and need for further research in Southeast Asia with special emphasis on mitigation strategies in North East India
Benzamin Hanse, S. M. Alam, S. Krishnan, Manasi Bhattacharjee, A. Sinha, L. Sundareswaran, Jyotirmay Kalita
International Journal of Biometeorology.2024; 68(12): 2477. CrossRef - Protecting vulnerable populations in extreme heat – a growing and pervasive health challenge
Zachary J. Schlader, Erica Tourula, Maxime Jeanovitch Lignier
eBioMedicine.2024; 109: 105448. CrossRef - Impact of climate change on occupational health and safety: A review of methodological approaches
Guilherme Neto Ferrari, Gislaine Camila Lapasini Leal, Rodrigo Clemente Thom de Souza, Edwin Vladimir Cardoza Galdamez
Work.2023; 74(2): 485. CrossRef - The Effect of Evaporative Cooling Vests on the Physiological and Perceptual Strain Indices of Construction Workers
Habibollah Dehghan, Mohammad Reza Mirzabe
International Journal of Environmental Health Engineering.2023;[Epub] CrossRef - Investigation into the thermal comfort and physiological adaptability of outdoor physical training in college students
Tianwei Tang, Xiaoqing Zhou, Yuchun Zhang, Xiwen Feng, Weiwei Liu, Zhaosong Fang, Zhimin Zheng
Science of The Total Environment.2022; 839: 155979. CrossRef - Characteristics of human thermal stress in South Asia during 1981–2019
Safi Ullah, Qinglong You, Guojie Wang, Waheed Ullah, D A Sachindra, Yechao Yan, Asher Samuel Bhatti, Adnan Abbas, Mushtaq Ahmad Jan
Environmental Research Letters.2022; 17(10): 104018. CrossRef - Health impact assessment of Delhi’s outdoor workers exposed to air pollution and extreme weather events: an integrated epidemiology approach
Vaishnavi Barthwal, Suresh Jain, Ayushi Babuta, Chubamenla Jamir, Arun Kumar Sharma, Anant Mohan
Environmental Science and Pollution Research.2022; 29(29): 44746. CrossRef - Assessing the outdoor thermal comfort conditions of exercising people in the semi-arid region of India
Pardeep Kumar, Amit Sharma
Sustainable Cities and Society.2022; 76: 103366. CrossRef - Determination of Waste Management Workers’ Physical and Psychological Load: A Cross-Sectional Study Using Biometric Data
Itsuki Kageyama, Nobuki Hashiguchi, Jianfei Cao, Makoto Niwa, Yeongjoo Lim, Masanori Tsutsumi, Jiakan Yu, Shintaro Sengoku, Soichiro Okamoto, Seiji Hashimoto, Kota Kodama
International Journal of Environmental Research and Public Health.2022; 19(23): 15964. CrossRef - Construct validity and invariance assessment of the social impacts of occupational heat stress scale (SIOHSS) among Ghanaian mining workers
Victor Fannam Nunfam, Ebenezer Afrifa-Yamoah, Kwadwo Adusei-Asante, Eddie John Van Etten, Kwasi Frimpong, Isaac Adjei Mensah, Jacques Oosthuizen
Science of The Total Environment.2021; 771: 144911. CrossRef - Heat Safety in the Workplace: Modified Delphi Consensus to Establish Strategies and Resources to Protect the US Workers
Margaret C. Morrissey, Douglas J. Casa, Gabrielle J. Brewer, William M. Adams, Yuri Hosokawa, Courteney L. Benjamin, Andrew J. Grundstein, David Hostler, Brendon P. McDermott, Meredith L. McQuerry, Rebecca L. Stearns, Erica M. Filep, David W. DeGroot, Jul
GeoHealth.2021;[Epub] CrossRef - Analysis of Mortality Change Rate from Temperature in Summer by Age, Occupation, Household Type, and Chronic Diseases in 229 Korean Municipalities from 2007–2016
Jongchul Park, Yeora Chae, Seo Hyung Choi
International Journal of Environmental Research and Public Health.2019; 16(9): 1561. CrossRef - Perceptions of climate change and occupational heat stress risks and adaptation strategies of mining workers in Ghana
Victor Fannam Nunfam, Jacques Oosthuizen, Kwadwo Adusei-Asante, Eddie John Van Etten, Kwasi Frimpong
Science of The Total Environment.2019; 657: 365. CrossRef - Implementing sensor technology applications for workplace health promotion: a needs assessment among workers with physically demanding work
Sander Mathijn Spook, Wendy Koolhaas, Ute Bültmann, Sandra Brouwer
BMC Public Health.2019;[Epub] CrossRef
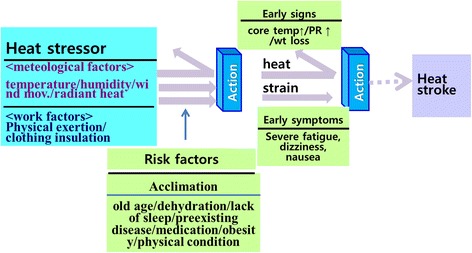
Fig. 1
| No. | Heavy exertion | Unaccli-matized | Age | Tropical night | Heat wave | WBGT |
|---|---|---|---|---|---|---|
| 1 | o | x | 41 | x | o | 31.75 |
| 2 | o | x | 55 | x | o | 32.59 |
| 3 | o | x | 66 | x | o | 30.24 |
| 4 | o | x | 29 | o | o | 30.62 |
| 5 | o | x | 54 | o | o | 29.9 |
| 6 | o | x | 44 | o | o | 31.76 |
| 7 | o | x | 49 | o | o | 30.98 |
| 8 | o | x | 63 | o | o | 31.29 |
| 9 | o | x | 50 | o | o | 30.76 |
| 10 | o | x | 29 | o | o | 32.29 |
| 11 | o | x | 53 | o | o | 29.0 |
| 12 | o | x | 44 | o | o | 29.97 |
| 13 | o | x | 46 | o | o | 29.14 |
| 14 | o | x | 62 | o | o | 31.89 |
| 15 | o | o | 45 | o | o | 25.71 |
| 16 | o | o | 35 | o | o | 30.37 |
| 17 | o | o | 54 | o | o | 30.28 |
| 18 | o | o | 44 | o | o | 31.27 |
| 19 | o | o | 56 | o | o | 29.88 |
| 20 | o | o | 44 | o | o | 30.77 |
| 21 | o | o | 56 | o | o | 29.03 |
| 22 | o | o | 52 | o | o | 30.48 |
| 23 | o | o | 45 | o | o | 29.31 |
| 24 | o | o | 39 | o | o | 30.78 |
| 25 | o | o | 39 | o | x | 25.98 |
| 26 | o | o | 42 | o | x | 29.29 |
| 27 | o | o | 54 | o | x | 31.66 |
| 28 | o | o | 51 | o | x | 30.09 |
| 29 | o | o | 49 | o | x | 30.76 |
| 30 | o | o | 47 | o | x | 28.85 |
| 31 | o | o | 64 | o | x | 29.09 |
| 32 | o | o | 62 | o | x | 27.46 |
| 33 | o | o | 51 | o | x | 32.72 |
| 34 | o | o | 66 | o | x | 29.57 |
| 35 | o | x | 47 | o | x | 30.59 |
| 36 | o | x | 50 | x | x | 29.73 |
| 37 | o | x | 60 | x | x | 30.11 |
| 38 | o | x | 54 | x | x | 30.39 |
| 39 | o | x | 49 | x | x | 24.37 |
| 40 | o | x | 60 | x | x | 23.43 |
| 41 | o | x | 59 | x | x | 25.87 |
| 42 | x | x | 67 | o | o | 32.59 |
| 43 | x | x | 56 | o | o | 30.67 |
| 44 | x | x | 77 | o | o | 30.53 |
| 45 | x | o | 37 | o | o | 29.29 |
| 46 | x | o | 51 | x | x | 30.72 |
| 47 | x | x | 71 | o | o | 32.45 |
 KSOEM
KSOEM

 Cite
Cite

