Abstract
-
Background
Occupational skin diseases are common in industrial settings; however, few studies have examined workers involved in the production of lithium-ion battery cathode-active materials. This study aimed to investigate the patterns and factors associated with skin diseases in these workers.
-
Methods
Overall, 37 workers with a history of skin disease were recruited from two cathode-active material manufacturing companies. Onsite investigations, semi-structured interviews, and workplace observations were conducted. Information on skin symptoms, affected areas, symptom frequency, and aggravating factors was collected.
-
Results
The most commonly reported symptoms were pruritus (27.5%), erythema (20.3%), and chemical burns (15.9%). The most commonly affected areas were the hands and forearms (67.6%), whereas 27.0% of workers reported symptoms in unexposed areas, such as the thighs. The symptoms tended to worsen on workdays and improved during holidays. Less-experienced workers reported more frequent symptoms.
-
Conclusions
Skin diseases during cathode material production appear to be primarily caused by irritants and allergic contact dermatitis, as well as chemical burns caused by exposure to metal dust, such as lithium, nickel, and cobalt. An urgent need exists for appropriate personal protective equipment, improved work environments, and targeted education for new workers.
-
Keywords: Occupational dermatitis; Skin diseases; Nickel; Cobalt; Lithium hydroxide
BACKGROUND
Occupational skin diseases are common in industrial settings, accounting for 30%–45% of all occupational diseases, with contact dermatitis comprising the majority.
1 Contact dermatitis is broadly classified into irritant and allergic types, with irritant contact dermatitis accounting for approximately 80% of occupational cases.
2 However, according to Korean industrial accident statistics, skin diseases account for less than 1% of all recognized occupational diseases. This underreporting is likely attributable to low awareness among workers, employers, and health examination agencies, challenges in diagnosis, limited recognition of occupational causes, and the transient nature of many skin conditions.
3 In 2023, among 2,668,878 workers who underwent special health examinations, only 8,552 (0.32%) were classified under “other diseases,” a category that includes skin diseases, infectious diseases, malignant neoplasms, and musculoskeletal disorders.
4 This indicates that the actual proportion of workers diagnosed with skin diseases was likely even lower.
Chemical agents such as organic compounds, acids, alkalis, and metals can induce various skin conditions, including allergic dermatitis, irritant dermatitis, and chemical burns.
5 Nickel and cobalt are representative metal allergens causing allergic contact dermatitis, and simultaneous sensitization and co-exposure are associated with higher incidence rates.
6,7
Although lithium is widely used in the battery industry and in psychiatric treatment, lithium hydroxide (LiOH)—commonly utilized in the production of cathode-active materials—can cause severe skin burns and eye damage, is toxic upon skin contact, and may lead to serious eye injury.
8 Nevertheless, dermatologic effects from occupational dermal exposure to lithium compounds have rarely been reported.
In the lithium-ion battery industry, especially in cathode-active material production, workers are exposed to metallic raw materials, including lithium, nickel, cobalt, and manganese.
9 Among these, the risk of exposure to Ni, Co, and Li is highest during cathode material production. Although these metals pose significant health risks, research on the prevalence of occupational skin diseases among exposed workers remains limited.
Therefore, this study aimed to investigate the frequency and risk factors of occupational skin diseases among workers involved in the production of lithium-ion battery cathode-active materials, focusing on those who had experienced skin symptoms and voluntarily participated. These findings provide preliminary data that may support the development of strategies to protect worker health and improve the work environment in this industry.
METHODS
Participant selection
In 2023, workers with a history of skin diseases were recruited from two lithium-ion battery cathode-active material manufacturing companies. During the study period, 514 workers and 162 workers were employed at the respective sites. Of these, 31 workers from the first company and six from the second company had experienced skin diseases within the past year or were currently experiencing skin symptoms, and voluntarily consented to participate in the study, resulting in a total of 37 participants. The exact number of workers in each process, as well as the number of workers who experienced skin diseases but declined to participate, could not be determined.
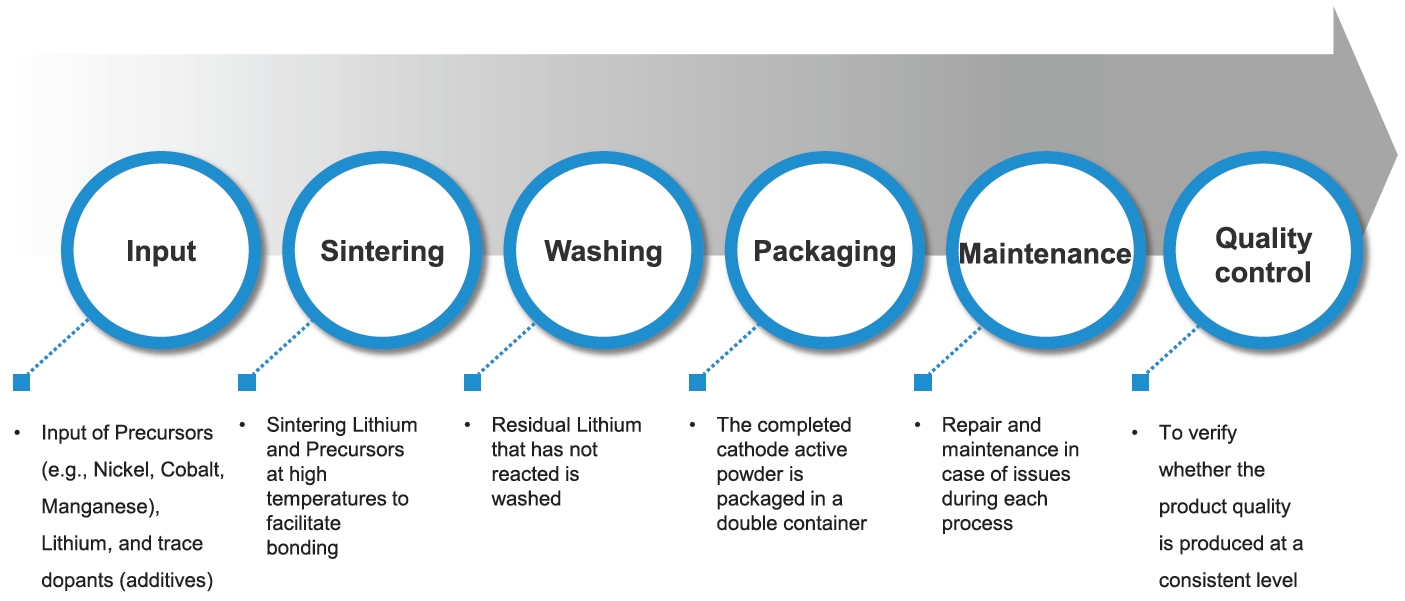
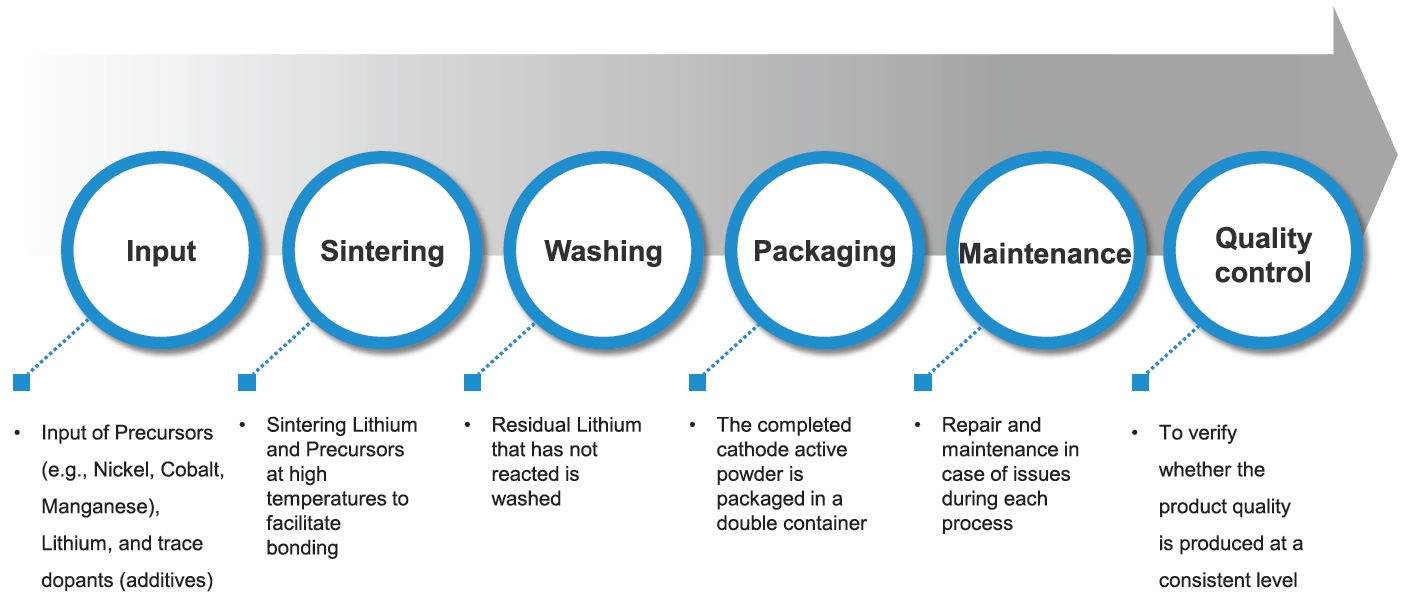
The participants were employed in the input, sintering, washing, packaging, maintenance, and quality control processes. Most of the participants worked in the sintering process (18 workers, 48.6%), followed by input (six workers, 16.2%), maintenance (five workers, 13.5%), washing (two workers, 5.4%), and quality control (two workers, 5.4%).
Process assessment
The research team conducted onsite visits to observe the work environment and tasks. Job characteristics and potentially hazardous exposures relevant to each participant were identified through direct observations.
In-depth interviews
An occupational and environmental medicine specialist conducted semi-structured interviews to explore occupational characteristics and skin symptoms. Interviews focused on exposure sources, symptom onset and patterns, personal protective equipment (PPE) use, and symptom response.
Ethics statement
This study was approved by the Institutional Review Board of the Occupational Safety and Health Research Institute (OSHRI-202303-HR-001). All participants received a detailed explanation of the study’s purpose, procedures, data handling, and academic use of photographs. Written informed consent was obtained from each participant.
RESULTS
General characteristics
The mean age of participants was 29.0 years (
Table 1). Of the 37 participants, 36 were male and one was female. The average duration of current employment was 10.7 months. Employment duration was distributed as follows: two workers (5.4%) were employed for ≤3 months, 15 workers (40.5%) for 3–6 months, 12 workers (32.4%) for 6 months to 1 year, four workers (10.8%) for 1–2 years, and four workers (10.8%) for 2–3 years. None of the workers had more than 3 years of employment.
Most of the workers were in their twenties and had less than 1 year of work experience, which is attributable to the fact that the majority were hired after the company began full-scale production in 2021.
Process overview
Both participating companies are located in Korea, and were established in 2019. Since 2021, they have been producing cathode-active materials used as raw materials for secondary batteries. At the time of the survey, the annual production of cathode-active materials was approximately 90,000 tons. Cathode-active materials are produced by mixing lithium with precursors such as nickel and cobalt, followed by sintering, washing, and packaging (
Fig. 1). Precursors are categorized as coarse (10–20 μm) or fine (<5 μm) particles. Lithium is used in the form of LiOH or lithium carbonate powder. Sintering was conducted near the kilns at 700–900°C. Most processes are operated by automated systems; however, certain tasks within the production line, such as raw material input, product packaging, and maintenance, are occasionally performed manually by workers.
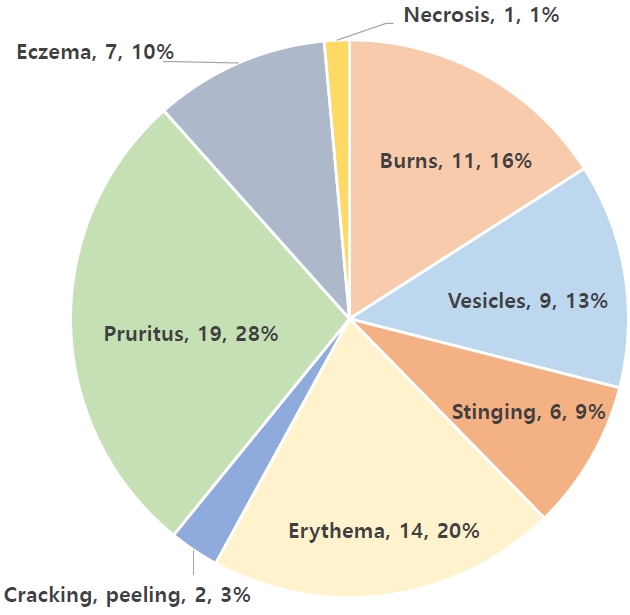
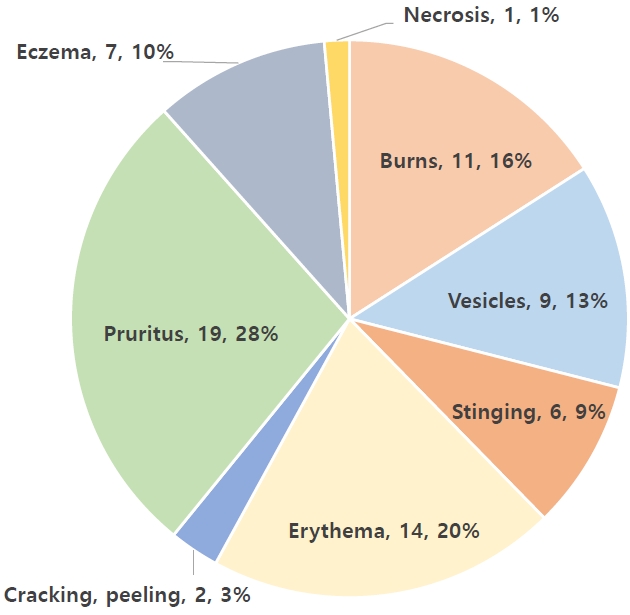
All 37 workers reported skin symptoms. The most common symptoms were pruritus (19 workers, 27.5%), erythema (14 workers, 20.3%), and chemical burns (11 workers, 15.9%). A few patients reported a single symptom, whereas others reported recurrent or multiple concurrent symptoms (
Fig. 2). Eighteen workers (48.6%) experienced symptoms more than twice annually (
Table 2). The symptom duration was <3 weeks in 21 workers (56.8%).
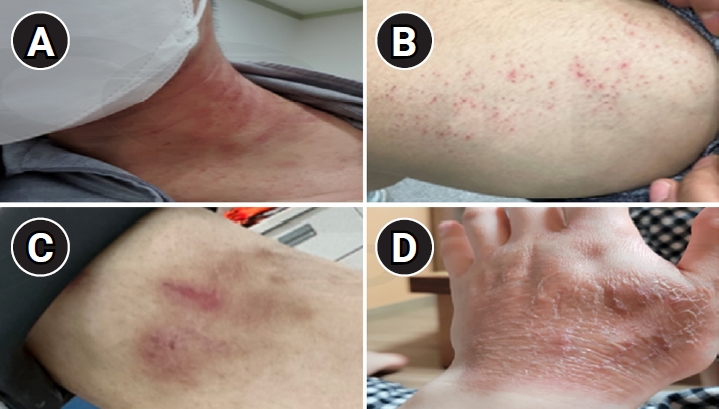
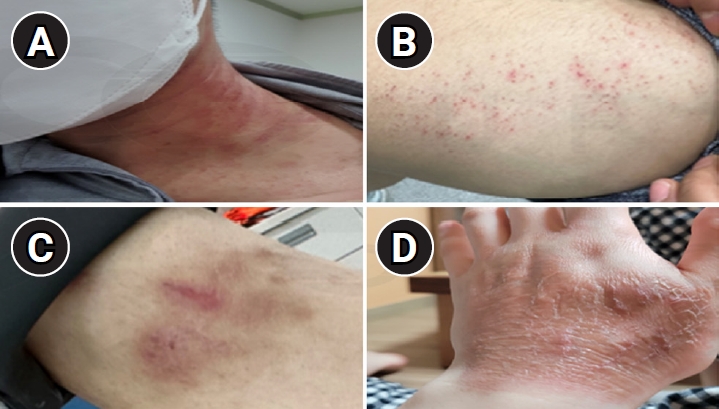
The most commonly affected sites were the forearms and hands (25 workers, 67.6%), followed by the neck and face (12 workers, 32.4%), chest/back/shoulders/axilla/groin (four workers, 10.8%), whole body (one worker, 2.7%), and feet/toes (one worker, 2.7%) (multiple responses allowed). Although symptoms were predominantly observed in exposed areas, 10 workers (27.0%) reported symptoms in non-exposed areas, such as the thighs (
Fig. 3). At the time of investigation, 16 workers (43.2%) presented with active symptoms. Twenty-six workers (70.3%) reported worsening symptoms on workdays and improvement during holidays.
Symptom distribution and patterns varied by process (
Table 3). Input workers reported pruritus and erythema in exposed areas. Sintering workers experienced symptoms in both exposed and non-exposed areas. Washing workers reported stinging and pruritus at non-exposed sites. Packaging workers had localized symptoms on the neck and face. Maintenance workers frequently reported vesicles and pruritus on the forearms and hands. Quality control workers reported erythema and pruritus on the forearms and hands.
PPE—including positive-pressure respirators, dust-proof clothing, antistatic gloves, and rubber gloves—was provided to all departments except the quality control department. In the sintering process, where workers are exposed to high temperatures, additional heat-resistant gloves and particulate respirators were supplied. All study participants reported experiencing occupational skin diseases. Due to the small sample size, a quantitative analysis of the association between PPE uses and skin diseases was not possible; however, workers reported skin symptoms regardless of PPE use.
According to in-depth interviews, workers in lithium manufacturing processes were repeatedly exposed to lithium dust through various pathways. Primary exposure routes included the process of inserting hands into flexible intermediate bulk container (bulk bag) to load raw materials, the phenomenon of dust infiltration between work clothes and gloves, and situations where large amounts of dust were generated due to hopper malfunctions causing materials to spill onto the floor. Additionally, workers reported dust exposure during product spillage into shoes, manual scooping operations, packaging machine and filter cleaning, equipment inspections, vacuum cleaning, dust container emptying, and when removing protective equipment. Skin symptoms manifested in diverse forms such as itching, erythema, burns, and vesicles, with symptoms tending to worsen in hot environments or during manual tasks. In particular, symptoms began after switching to a lithium hydroxide process, and immediate irritation occurred when powder contacted sweaty areas. Symptoms were especially severe on the neck, face, and back of hands. When wearing thin work clothes, workers reported that dust penetrated clothing and caused symptoms on the thighs. A total of 15 workers underwent dermatological examinations, among whom one was diagnosed with cobalt sensitization through patch testing, while the remaining 14 were diagnosed with burns, skin necrosis, contact dermatitis, and other conditions. Symptoms improved during rest and worsened during work. Some workers were unaware that black powder indicated lithium exposure. Regarding the use of protective equipment, dust-proof clothing was often not worn due to heat and sweating, although longer gloves were found to reduce wrist symptoms. Symptoms appeared at the edges of half-masks, and switching to full-face or positive-pressure masks alleviated symptoms; however, frequent equipment failures caused inconvenience on-site. There were also issues such as insufficient glove supply. Coping methods mainly consisted of personal measures, such as wrapping a towel around the neck or washing affected areas. Some workers expressed the need for systematic burn management guidelines provided by the company. Key opinions from the in-depth interviews are summarized in
Table 4.
DISCUSSION
This study examined the frequency and risk factors of occupational skin diseases among workers involved in the production of lithium-ion battery cathode-active materials, focusing on those who had experienced skin symptoms and voluntarily participated. Among the 37 participants, 18 (48.6%) reported experiencing skin symptoms more than twice annually. The most common symptoms were pruritus, erythema, and chemical burns, predominantly affecting the forearms, hands, neck, and face. Additionally, 27.0% of participants reported symptoms in non-exposed areas. The symptoms tended to worsen during workdays and subside on holidays.
It should be noted that, due to the study design targeting only symptomatic and voluntarily participating workers, these findings do not represent the prevalence of occupational skin diseases among all workers in this industry.
Symptom frequency varied according to employment duration. Approximately 73% of the workers had <1 year of experience (mean, 10.7 months), their annual incidence rate appeared higher than that of workers with >2 years of experience; however, the small number of experienced workers and the lack of statistical testing limit the strength of this observation. Notably, experienced workers reported reduced symptom frequency through preventive measures such as moisture-wicking undergarments, protective creams, and skin washing during breaks. This finding suggests that work experience and coping strategies may play a preventive role, whereas the higher incidence among new employees could be attributed to their unfamiliarity with chemical exposure management.
Chemical burns were commonly observed in the input, sintering, and maintenance processes, all of which are associated with high dust exposure. Strongly alkaline LiOH dust can mix with sweat, leading to irritation or chemical burns. Visual inspection and worker reports confirmed significant dust generation during the handling of powdered raw materials in these processes. LiOH, a key component in these processes, reacts with moisture to cause chemical burns. Its strong alkalinity induces saponification of skin lipids, thereby destroying the skin’s physical barrier.
10 This suggests that LiOH present in raw materials can react with sweat on workers’ skin, leading to chemical burns.
A recent case study described erythema multiforme following lithium contact in a battery factory worker, with recurrence after re-exposure and histopathologic findings suggestive of immune-mediated skin injury. The U.S. National Institute for Occupational Safety and Health classifies lithium compounds as skin irritants and recommends strict exposure limits, skin protection, and washing facilities to prevent adverse effects.
11 These findings imply that lithium may trigger cutaneous immune responses independent of systemic exposure. In light of the growing use of lithium in industry, its potential role in occupational skin disease should be carefully considered. Preventive strategies and surveillance are warranted in exposed worker populations.
In the studied workplaces, lithium, nickel, and cobalt were used simultaneously. Without quantitative assessment of each hazardous agent, it is impossible to distinguish the specific contributions of each substance to the observed health effects. The complex dermatological symptoms observed among workers are not merely the result of overlapping exposures, but may be explained by the three-stage cascade mechanism described by Patel and Nixon (2022).
12 According to this mechanism, alkaline LiOH first damages the skin’s protective barrier, which then allows nickel and cobalt ions to penetrate the compromised skin. These metal ions can subsequently trigger an excessive immune response. As a result, symptoms of chemical burns—such as stinging and vesicles—and allergic reactions—such as pruritus and erythema—may occur simultaneously at the same site.
The skin diseases observed in this study, arising in a work environment with combined exposure to LiOH, cobalt, nickel, and perspiration, showed distinct pathological mechanisms and clinical presentations compared to those reported in single-metal (cobalt or nickel) exposure industries. In other metal-related occupations (e.g., smelting, metal processing), allergic contact dermatitis due to cobalt and nickel is most frequently reported, often beginning as irritant contact dermatitis but progressing to allergic contact dermatitis after chronic, repeated exposure.
13 In such cases, lesions are confined to exposed areas such as the hands, arms, and face, and typically occur during prolonged work without appropriate protective equipment. The pathological mechanism involves contact of metal ions with the skin surface, recognition and metal–protein complex formation by Langerhans cells, activation of T cells (Th1, Th17), secretion of inflammatory cytokines, and the subsequent development of localized dermatitis.
In contrast, in the workplaces studied here, LiOH-induced skin barrier disruption facilitated the penetration of nickel and cobalt ions, triggering metal-induced allergic immune responses that co-occurred with chemical burn symptoms at the same site. Moreover, penetration of metal dust through work clothing fibers, high ambient temperatures, and perspiration contributed to symptom exacerbation and the occurrence of lesions in atypical, non-exposed areas such as the thighs. This comparison underscores the complexity and distinctiveness of skin diseases arising from the combined exposure environment of the lithium-ion battery industry, highlighting the need for industry-specific prevention and management strategies.
Although LiOH-induced damage can potentially be quantified using skin pH monitoring, and nickel/cobalt exposure can be assessed by analyzing metal ion concentrations in sweat, the lack of standardized exposure assessment methods makes it difficult to distinguish between chemical burns and allergic reactions as the underlying cause of symptoms. To address these limitations, it is essential to establish a multi-exposure matrix that integrates quantitative chemical exposure levels, biological responses (such as inflammatory biomarkers), and environmental factors (including temperature and humidity). Future research should adopt comprehensive frameworks to systematically interpret complex occupational dermatoses in such settings.
Although patch testing was not performed as part of this study, one worker reported having undergone patch testing at a medical institution and was found to be sensitized to cobalt. This suggests that some of the skin diseases observed among workers in this study may be attributable to allergic contact dermatitis. These findings are consistent with the literature on metal-induced irritant and allergic contact dermatitis.
7,14,15
The strength of this study lies in the detailed characterization of skin disease patterns and risk factors in actual industrial settings. Interview findings highlighted limitations of PPE (e.g., heat stress, insufficient glove length, and mask type) as well as inadequate management of work clothing and workplace environments.
However, the limitations include the small sample size, cross-sectional design, reliance on subjective complaints, and limited clinical assessment. Furthermore, the recruitment method relying on voluntary participation of symptomatic workers may introduce selection bias and limits generalizability to all cathode material workers. Another major limitation of this study is the absence of quantitative environmental monitoring data for airborne metal dusts. Exposure assessment relied primarily on worker reports and observational data, which may introduce information bias. Future studies should incorporate objective exposure measurements to strengthen causal inference.
CONCLUSIONS
Skin symptoms among lithium-ion battery cathode material workers were primarily attributed to burns and irritant or allergic contact dermatitis associated with exposure to metal dusts such as LiOH, nickel, and cobalt. Suboptimal use of PPE and insufficient environmental management may have contributed to symptom occurrence, as indicated by worker reports; however, direct causal relationships could not be established due to the lack of a control group and statistical analysis. Despite these limitations, this study provides detailed insights into the patterns and risk factors of occupational skin diseases in a real-world industrial setting, specifically among workers with self-reported symptoms who voluntarily participated.
Urgent actions include providing process-specific PPE, improving the work environment, enabling early diagnosis, and enhancing worker education. Improvements to reporting systems, standardized training programs, onsite practical education for new workers, and mentorship by experienced employees are recommended. These findings offer preliminary data that may support the prevention, early diagnosis, and effective health management of occupational skin diseases in similar industrial settings.
Abbreviations
personal protective equipment
NOTES
-
Funding
This study was supported by a grant from the Occupational Safety and Health Research Institute (2023-OSHRI-738), funded by the Korea Occupational Safety and Health Agency.
-
Competing interests
The authors declare that they have no competing interest.
-
Author contributions
Conceptualization and methodology: Won YL. Data curation: Lee HY, Koh DH, Won YL, Choi J. Formal analysis: Lee HY. Investigation: Koh DH, Lee HY. Writing - original draft: Lee HY. Writing - review & editing: Choi J, Koh DH, Won YL.
Fig. 1.Manufacturing process of cathode-active materials.
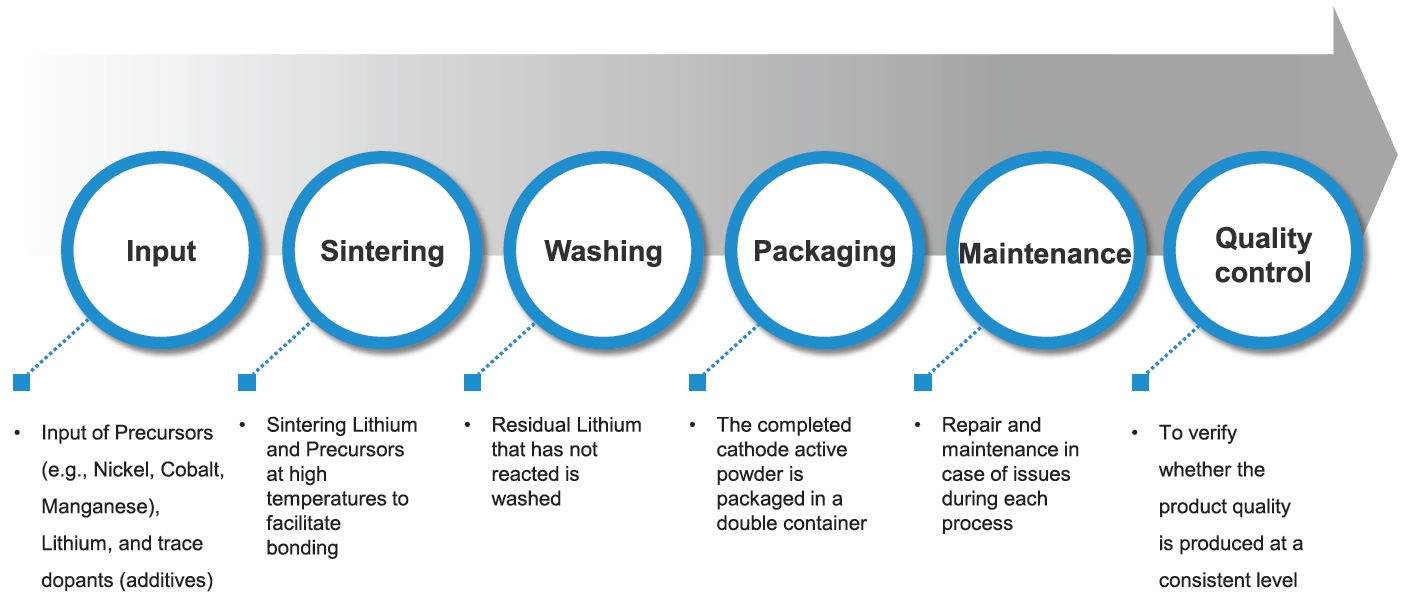
Fig. 2.Prevalent skin symptoms among affected workers. Symptoms were presented as number (%).
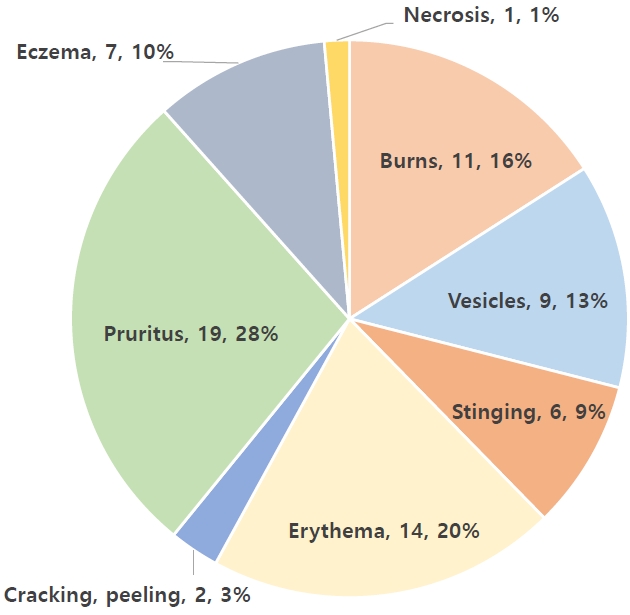
Fig. 3.Examples of skin lesions among cathode-active material manufacturing workers. (A) Neck. (B) Thigh. (C) Wrist. (D) Dorsum of the hand.
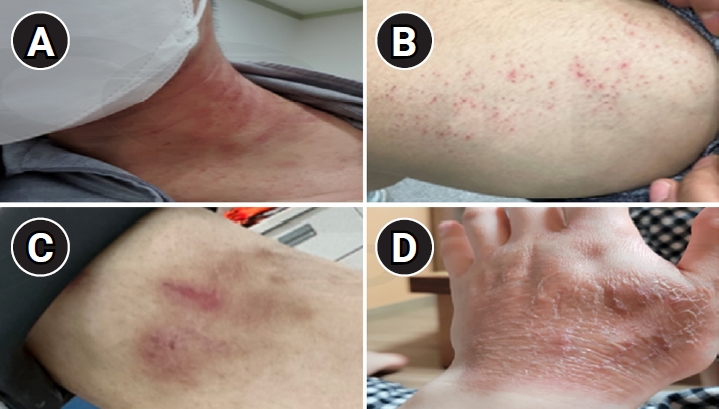
Table 1.General characteristics of study participants
|
Characteristic |
No. (%) (n = 37) |
|
Age (years) |
|
|
20–29 |
31 (83.8) |
|
30–39 |
5 (13.5) |
|
40–49 |
1 (2.7) |
|
Sex |
|
|
Male |
36 (97.3) |
|
Female |
1 (2.7) |
|
Duration of current working |
|
|
<3 months |
2 (5.4) |
|
3–6 months |
15 (40.5) |
|
6 months–1 year |
12 (32.4) |
|
1–2 years |
4 (10.8) |
|
2–3 years |
4 (10.8) |
|
>3 years |
0 (0) |
Table 2.Frequency and sites of skin symptoms
|
Characteristics |
No. (%) (n = 37) |
|
Frequency of symptom occurrence |
|
|
Two or more times per year |
18 (48.6) |
|
Less than two times per year |
14 (37.8) |
|
Unknown |
5 (13.5) |
|
Duration of symptoms |
|
|
More than 3 weeks |
16 (43.2) |
|
Less than 3 weeks |
21 (56.8) |
|
Site of symptom occurrence (multiple responses allowed) |
|
|
Whole body |
1 (2.7) |
|
Neck, face |
12 (32.4) |
|
Forearms, hands |
25 (67.6) |
|
Chest, back, shoulders, axilla, groin |
4 (10.8) |
|
Thighs |
10 (27.0) |
|
Feet, toes |
1 (2.7) |
|
Current presence of symptoms |
|
|
Yes |
16 (43.2) |
|
No |
21 (56.8) |
|
Worsening during work, improvement during holidays |
|
|
Yes |
26 (70.3) |
|
No |
6 (16.2) |
|
Unknown |
5 (13.5) |
Table 3.Sites and patterns of skin symptom occurrence by process (multiple responses allowed)
|
Process |
No. of workers per process |
Site of symptom occurrence
|
Symptom patterns
|
|
Whole body |
Neck, face |
Forearms, hands |
Chest, back |
Thighs |
Feet, toes |
Burns |
Necrosis |
Vesicles |
Stinging |
Erythema |
Cracking, peeling |
Pruritus |
Eczema |
|
Inputa
|
6 |
- |
3 |
6 |
- |
1 |
- |
1 |
- |
- |
- |
3 |
- |
4 |
- |
|
Sinteringb
|
18 |
- |
5 |
11 |
1 |
5 |
1 |
9 |
1 |
4 |
4 |
4 |
- |
5 |
7 |
|
Washinga
|
2 |
- |
- |
- |
1 |
2 |
- |
- |
- |
- |
1 |
- |
- |
2 |
- |
|
Packaginga
|
4 |
- |
4 |
2 |
1 |
1 |
- |
- |
- |
2 |
- |
3 |
1 |
2 |
- |
|
Maintenancea
|
5 |
1 |
1 |
4 |
1 |
1 |
- |
1 |
- |
3 |
1 |
2 |
1 |
4 |
- |
|
Quality controlc
|
2 |
- |
- |
2 |
- |
- |
- |
- |
- |
- |
- |
2 |
- |
2 |
- |
Table 4.In-depth interview results from cathode material workers with occupational skin disease
|
Category |
Topic |
Content |
|
Exposure routes |
Main contact paths |
Direct contact inside flexible intermediate bulk container (bulk bag) |
|
Dust infiltration between work clothes and gloves |
|
Dust generated during hopper malfunctions |
|
Other exposure situations |
Product spillage into shoes |
|
Dust exposure during manual tasks (scooping, cleaning, equipment inspection) |
|
Dust resuspension when removing protective equipment |
|
Symptoms |
Symptom types |
Itching |
|
Erythema |
|
Burns |
|
Vesicles |
|
Aggravating factors |
Hot environments |
|
Physical fatigue and manual work |
|
Main affected areas |
Exposed sites: neck, face, back of hands |
|
Non-exposed sites: symptoms on thighs and other areas due to dust penetration through work clothes |
|
Diagnosis |
Dermatologist diagnoses including burns, contact dermatitis, necrosis |
|
Symptom pattern |
Worsening during work |
|
Improvement during rest |
|
Protective equipment |
Usage status |
Frequent non-use of dust-proof clothing due to heat and sweating |
|
Insufficient glove supply |
|
Effectiveness and issues |
Full-face or positive-pressure masks effective but frequently malfunction |
|
Longer gloves help reduce wrist symptoms |
|
Coping methods |
Personal actions |
Wrapping towels around the neck |
|
Washing affected areas immediately when irritation occurs |
|
Company measures |
No official company guidelines for burn management |
REFERENCES
- 1. Srinivas CR, Sethy M. Occupational dermatoses. Indian Dermatol Online J 2023;14(1):21–31.ArticlePubMedPMC
- 2. Sasseville D. Occupational contact dermatitis. Allergy Asthma Clin Immunol 2008;4(2):59–65.ArticlePubMedPMCPDF
- 3. Ahn YS, Kim MG. Occupational skin diseases in Korea. J Korean Med Sci 2010;25(Suppl):S46–52.ArticlePubMedPMC
- 4. Ministry of Employment and Labor. Special Health Examination Results. Sejong, Korea: Ministry of Employment and Labor; 2024.
- 5. Won JU. Health effects of chemicals used in hospitals among healthcare workers. J Korean Med Assoc 2010;53(6):474–82.Article
- 6. Duarte I, Amorim JR, Perazzio EF, Schmitz Junior R. Metal contact dermatitis: prevalence of sensitization to nickel, cobalt and chromium. An Bras Dermatol 2005;80(2):137–42.
- 7. Karagounis TK, Cohen DE. Occupational hand dermatitis. Curr Allergy Asthma Rep 2023;23(4):201–12.ArticlePubMedPMCPDF
- 8. European Chemicals Agency. Substance information: lithium hydroxide. https://echa.europa.eu/substance-information/-/substanceinfo/100.013.804. Updated 2023. Accessed June 26, 2025
- 9. Perttula P, Rodriguez Llopis I, Saamanen A, Barruetabena L, Garcia L, Kannisto H, et al. Lithium-Ion Battery’s Life Cycle: Safety Risks and Risk Management at Workplaces. Helsinki, Finland: Finnish Institute of Occupational Health; 2023.
- 10. Milner SM. Alkali burns of the skin. Eplasty 2023;23:QA12.PubMedPMC
- 11. National Institute for Occupational Safety and Health (NIOSH). NIOSH Pocket Guide to Chemical Hazards Lithium hydride. Updated 2019. https://www.cdc.gov/niosh/npg/npgd0371.html. Accessed June 27, 2025
- 12. Patel K, Nixon R. Irritant contact dermatitis: a review. Curr Dermatol Rep 2022;11(2):41–51.ArticlePubMedPMCPDF
- 13. Kim D, Kim AR, Kim H, Lee S, Seo B, Suh HS, et al. Nickel dust-induced occupational contact dermatitis by welding and grinding work in shipyard workers: a report of nine cases. Ann Occup Environ Med 2022;34:e7.ArticlePubMedPMCPDF
- 14. Chamani S, Mobasheri L, Rostami Z, Zare I, Naghizadeh A, Mostafavi E. Heavy metals in contact dermatitis: a review. J Trace Elem Med Biol 2023;79:127240.ArticlePubMed
- 15. Pacheco KA. Occupational dermatitis: How to identify the exposures, make the diagnosis, and treat the disease. Ann Allergy Asthma Immunol 2018;120(6):583–91.ArticlePubMed
 , Dong-Hee Koh2
, Dong-Hee Koh2 , Junhyeok Choi1
, Junhyeok Choi1 , Yong Lim Won1,*
, Yong Lim Won1,*

 KSOEM
KSOEM

 Cite
Cite

