Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 28; 2016 > Article
- Research Article Gender differences in Reasons for Sickness Presenteeism - a study among GPs in a Swedish health care organization
- Marie Gustafsson Sendén1, Karin Schenck-Gustafsson2, Ann Fridner1
-
Annals of Occupational and Environmental Medicine 2016;28:50.
DOI: https://doi.org/10.1186/s40557-016-0136-x
Published online: September 20, 2016
1Department of psychology, Stockholm University, 106 91 Stockholm, Sweden 
2Karolinska Institute, Stockholm, Sweden 
© The Author(s). 2016
Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Figure & Data
REFERENCES
Citations

- The relationship between career calling and presenteeism: the role of workaholism and self-compassion
Zhaobiao Zong, Feifei Sun, Haichao Sun, Shaoqing Su, Baojian Wei
Australian Journal of Psychology.2025;[Epub] CrossRef - Gender disparities in job flexibility, job security, psychological distress, work absenteeism, and work presenteeism among U.S. adults
Monica L. Wang, Marie-Rachelle Narcisse, Kate Rodriguez, Pearl A. McElfish
SSM - Population Health.2025; 29: 101761. CrossRef - Influence of the pandemic on the mental health of professional workers
Jelena Atanackovic, Henrietta Akuamoah-Boateng, Jungwee Park, Melissa Corrente, Ivy Lynn Bourgeault
BMC Psychology.2025;[Epub] CrossRef - Reasons behind sickness presenteeism: insights from four national surveys in Latvia
Svetlana Lakiša, Inese Gobina, Ivars Vanadziņš, Linda Matisāne
Frontiers in Public Health.2025;[Epub] CrossRef - Predictive modeling of presenteeism among radiographers: a secondary analysis of comprehensive data using Bayesian neural network
Ullas U. Nayak, Shivanath Shanbhag, Nitika C. Panakkal, Vennila J., Sidhiprada Mohapatra
International Journal of Occupational Safety and Ergonomics.2025; : 1. CrossRef - The Status of Presenteeism Among Clinical Nurses in China: A Systematic Review and Meta-Analysis
Xiang Zeng, Kun Wang, Ya Le Guo, Zhao lan Wang, Jun Wen Li
Evaluation & the Health Professions.2025;[Epub] CrossRef - Presenteeism and Its Associated Factors Among Teachers
Hend Serya, Abdel-Hady El-Gilany
La Medicina del Lavoro.2025; 116(2): 16010. CrossRef - The relationship between job burnout and presenteeism among Chinese primary public health physicians: a moderated mediation model
Xinru Kong, Miaomiao Zhao, Ruyu Li, Zhouxiang Li, Danfeng Chang, Xinyi Zhou, Qiang Ma, Yuexia Gao
BMC Medical Education.2025;[Epub] CrossRef - Prevalence of Sickness Presenteeism and Contributing Factors Among Formal Sector Workers in Indonesia: A Cross-Sectional Study
Jessica SIDHARTA, Nuri Purwito ADI, Marsen ISBAYUPUTRA, Dewi S. SOEMARKO, HERQUTANTO
Journal of UOEH.2025; 47(2): 45. CrossRef - Effect of Exposure to Physical Environmental Risk Factors of Korean Wage Workers on Presenteeism using the 6th Korean Working Conditions Survey (KWCS): Focusing on Gender Differences
Yoon Ho Lee, Jeong-Beom Lee, Mid-Eum Moon, Myoung-Je Song, Jong-Sun Kim, Hwa-Young Lee, Eun Chul Jang, Soon-Chan Kwon, Young-Sun Min, In-Ho Lee
Journal of The Korean Society of Living Environmental System.2025; 32(3): 359. CrossRef - Association between Presenteeism, Associated Factors, and Outcomes among Intern Physicians in Public Hospitals during the COVID-19 Pandemic: A Cross-Sectional Study
Vithawat Surawattanasakul, Wuttipat Kiratipaisarl, Penprapa Siviroj
Medicina.2024; 60(6): 962. CrossRef - Remote Workers’ Reasons for Changed Levels of Absenteeism, Presenteeism and Working Outside Agreed Hours During the COVID-19 Pandemic
Luke Anthony Fiorini
Sage Open.2024;[Epub] CrossRef - UMA TEORIA DO PRESENTEÍSMO PARA ALÉM DA DOENÇA E UMA FERRAMENTA PARA SUA MENSURAÇÃO
Salim Yılmaz, Selma Söyük
Revista de Administração de Empresas.2024;[Epub] CrossRef - Differences in how women and men in a Swedish population-based sample think about sick leave: A cross-sectional vignette study
Gunnel Hensing, Sara Blom, Ida Björkman, Monica Bertilsson, Johan Martinsson, Lena Wängnerud, Jesper Löve
Work.2024; 77(3): 827. CrossRef - A THEORY OF PRESENTEEISM BEYOND BEING SICK AND A MEASUREMENT TOOL
Salim Yılmaz, Selma Söyük
Revista de Administração de Empresas.2024;[Epub] CrossRef - LİTERATÜRDE TARTIŞMALI BİR KAVRAM: PRESENTEEISM
Salim Yılmaz, Selma Söyük
Sağlık Akademisi Kastamonu.2024; 9(1): 196. CrossRef - Transcultural nursing: a qualitative analysis of nursing students’ experiences in a multicultural context in North-Eastern Namibia
Vistolina Nuuyoma, Sitembile Muvumwaeni, Leonard Chihururu
BMC Nursing.2024;[Epub] CrossRef - Costs of Presenteeism and Absenteeism Associated With Psychological Distress Among Male and Female Older Workers
Mahée Gilbert-Ouimet, Hélène Sultan-Taïeb, Karine Aubé, Léonie Matteau, Xavier Trudel, Chantal Brisson, Jason Robert Guertin
Journal of Occupational & Environmental Medicine.2024; 66(10): e467. CrossRef - Work-Related Factors Influencing Presenteeism in Croatia during COVID-19: A Logistic Regression Approach
Markus Dulhofer
Naše gospodarstvo/Our economy.2024; 70(4): 23. CrossRef - Presenteeism and home-based Telework across the Visegrad countries during the COVID-19 Pandemic: A Multivariate Analysis Approach
Markus Dulhofer
Gazdaság és Társadalom.2024; 17(3): 97. CrossRef - Reduced Immune Fitness and Job Performance: Absenteeism, Presenteeism, and Associated Costs for the Dutch Economy
Annabel S. M. Sips, Noortje R. Severeijns, Aletta D. Kraneveld, Johan Garssen, Joris C. Verster
International Journal of Environmental Research and Public Health.2023; 20(3): 1761. CrossRef - Employee Affiliation and Presenteeism in Health-care Settings
Jasmina Starc, Tanja Regina Fabjan
Open Access Macedonian Journal of Medical Sciences.2023; 11(E): 338. CrossRef - Presenteeism and noise perception at work: a cross-sectional study using association analysis
Renata da Silva Cardoso Rocha Tavares, Luiz Felipe Silva, Jorge Muniz Júnior
Sao Paulo Medical Journal.2023; 141(1): 36. CrossRef - Gender differences at the workplace: Sickness absence and productivity loss at work and their association with health and work-related factors
Bosiljka Đikanović, Tessa Kouwenhoven-Pasmooij, Roderik Kraaijenhagen, Van Roeters, Alex Burdorf, Vladimir Vasilev, Suzan Robroek
Srpski medicinski casopis Lekarske komore.2023; 4(1): 11. CrossRef - Gender analysis of Spanish National Questionnaire on behaviours and attitudes of doctors towards their own illness (CAMAPE)
I. Sebastián-Sánchez, A. Gállego-Royo, B. Marco-Gómez, C. Pérez-Álvarez, O. Urbano Gonzalo, M.T. Delgado-Marroquín, R. Altisent-Trota, M.P. Astier-Peña
Journal of Healthcare Quality Research.2023; 38(3): 165. CrossRef - Women deserve better: A discussion on COVID‐19 and the gendered organization in the new economy
Simisola Johnson
Gender, Work & Organization.2022; 29(2): 639. CrossRef - Sickness Presenteeism among Employees Having Workplace Conflicts—Results from Pooled Analyses in Latvia
Svetlana Lakiša, Linda Matisāne, Inese Gobiņa, Hans Orru, Ivars Vanadziņš
International Journal of Environmental Research and Public Health.2022; 19(17): 10525. CrossRef - Primary Care Physicians’ Personal and Professional Attributes Associated With Forgoing Own Care and Presenteeism: A Cross Sectional Study
Christine Cohidon, Liv Mahler, Barbara Broers, Thierry Favrod-Coune, Amir Moussa, Paul Sebo
International Journal of Public Health.2022;[Epub] CrossRef - Cluster Headache and the Comprehension Paradox
Heiko Pohl, Andreas R. Gantenbein, Peter S. Sandor, Jean Schoenen, Colette Andrée
SN Comprehensive Clinical Medicine.2022;[Epub] CrossRef - In Sickness and in Health: The Role of Housework Engagement in Work Productivity despite Presenteeism
Catarina Correia Leal, Aristides I. Ferreira
The Spanish Journal of Psychology.2021;[Epub] CrossRef - The Compensatory Protective Effects of Social Support at Work in Presenteeism During the Coronavirus Disease Pandemic
Jia Wun Chen, Luo Lu, Cary L. Cooper
Frontiers in Psychology.2021;[Epub] CrossRef - Activities and Perceived Risk of Transmission and Spread of SARS-CoV-2 among Specialists and Residents in a Third Level University Hospital in Spain
Jesús Aranaz-Andrés, Amaranta McGee-Laso, Juan Galán, Rafael Cantón, José Mira
International Journal of Environmental Research and Public Health.2021; 18(6): 2838. CrossRef - Association of Laryngeal Botulinum Neurotoxin Injection With Work Productivity for Patients With Spasmodic Dysphonia
Tanya K. Meyer, Charles Spiekerman, Rachel Kaye, Andrew Blitzer, Rouya S. Kamizi, Lan Jiang, Edward M. Weaver
JAMA Otolaryngology–Head & Neck Surgery.2021; 147(9): 804. CrossRef - The association between direct supervisor's behavior and employee presenteeism in Korean wage workers: findings from the fifth Korean Working Condition Survey
Sung Hee Lee, Joo Hyun Sung, Dae Hwan Kim, Chang Sun Sim
Annals of Occupational and Environmental Medicine.2021;[Epub] CrossRef - Reasons for presenteeism in different occupational branches in Sweden: a population based cross-sectional study
Staffan Marklund, Klas Gustafsson, Gunnar Bergström, Constanze Leineweber
International Archives of Occupational and Environmental Health.2021; 94(6): 1385. CrossRef - The association between doctors’ presenteeism and job burnout: a cross-sectional survey study in China
Pei Pei, Guohua Lin, Gaojie Li, Yifan Zhu, Xiaoyu Xi
BMC Health Services Research.2020;[Epub] CrossRef - Factors Related to Presenteeism among South Korean Workers Exposed to Workplace Psychological Adverse Social Behavior
Jee-Seon Yi, Hyeoneui Kim
International Journal of Environmental Research and Public Health.2020; 17(10): 3472. CrossRef - Presenteeism among health care workers: literature review
Paulo Henrique Poti Homrich, Fabio Fernandes Dantas-Filho, Laura Luna Martins, Emilian Rejane Marcon
Revista Brasileira de Medicina do Trabalho.2020; 18(1): 97. CrossRef - Association between employment status and sickness presenteeism among Korean employees: a cross-sectional study
Jeong Woo Park, Seong Sik Cho, JongWoo Lee, Jonghyun Hwang, Jung Il Kim, Byoung Gwon Kim, Young Seoub Hong
Annals of Occupational and Environmental Medicine.2020;[Epub] CrossRef - Gender differences in the longitudinal association between obesity, and disability with workplace absenteeism in the Australian working population
Syed Afroz Keramat, Khorshed Alam, Jeff Gow, Stuart J. H. Biddle, Fakir M Amirul Islam
PLOS ONE.2020; 15(5): e0233512. CrossRef - Home-Based Telework and Presenteeism Across Europe
Corinna Steidelmüller, Sophie-Charlotte Meyer, Grit Müller
Journal of Occupational & Environmental Medicine.2020; 62(12): 998. CrossRef - Body mass index and risk of sick leave: A systematic review and meta‐analysis
Sohrab Amiri, Sepideh Behnezhad
Clinical Obesity.2019;[Epub] CrossRef - Presenteeism: Symptom of an ailing practice model for Canadian physicians?
Kevin B Laupland, Louis Valiquette
Journal of the Association of Medical Microbiology and Infectious Disease Canada.2019; 4(3): 136. CrossRef - Attitudes about sickness presenteeism in medical training: is there a hidden curriculum?
Lauris C. Kaldjian, Laura A. Shinkunas, Heather Schacht Reisinger, Marc A. Polacco, Eli N. Perencevich
Antimicrobial Resistance & Infection Control.2019;[Epub] CrossRef - Presenteeism as a predictor of disability pension: A prospective study among nursing professionals and care assistants in Sweden
Klas Gustafsson, Gunnar Bergström, Staffan Marklund, Emmanuel Aboagye, Constanze Leineweber
Journal of Occupational Health.2019; 61(6): 453. CrossRef - A Comparison of Job Stress Models
Burkhard Schmidt, Michael Schneider, Philipp Seeger, Annelies van Vianen, Adrian Loerbroks, Raphael M. Herr
Journal of Occupational & Environmental Medicine.2019; 61(7): 535. CrossRef - Presenteeism: A review and research directions
Daniela Lohaus, Wolfgang Habermann
Human Resource Management Review.2019; 29(1): 43. CrossRef - Sickness presenteeism: Are we sure about what we are studying? A research based on a literature review and an empirical illustration
Albert Navarro, Sergio Salas‐Nicás, Clara Llorens, Salvador Moncada, Emilia Molinero‐Ruíz, David Moriña
American Journal of Industrial Medicine.2019; 62(7): 580. CrossRef - Sickness presenteeism at work: prevalence, costs and management
Gail Kinman
British Medical Bulletin.2019; 129(1): 69. CrossRef - Near misses and presenteeism among paramedics
T Ishimaru, T Kubo, K Honno, Y Toyokuni, Y Fujino
Occupational Medicine.2019;[Epub] CrossRef - Presenteeism exposures and outcomes amongst hospital doctors and nurses: a systematic review
Juliana Nga Man Lui, Ellie Bostwick Andres, Janice Mary Johnston
BMC Health Services Research.2018;[Epub] CrossRef - Prevalence, associated factors and reasons for sickness presenteeism: a cross-sectional nationally representative study of salaried workers in Spain, 2016
Albert Navarro, Sergio Salas-Nicás, Salvador Moncada, Clara Llorens, Emilia Molinero-Ruiz
BMJ Open.2018; 8(7): e021212. CrossRef - Associations Between Supportive Leadership Behavior and the Costs of Absenteeism and Presenteeism
Johannes Albert Schmid, Marc Nicolas Jarczok, Diana Sonntag, Raphael Manfred Herr, Joachim Ernst Fischer, Burkhard Schmidt
Journal of Occupational & Environmental Medicine.2017; 59(2): 141. CrossRef
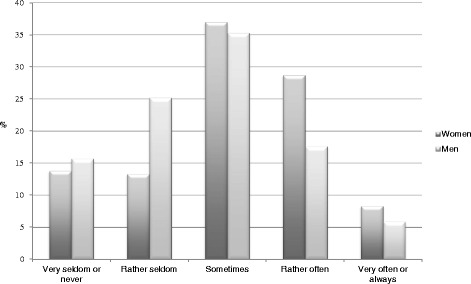
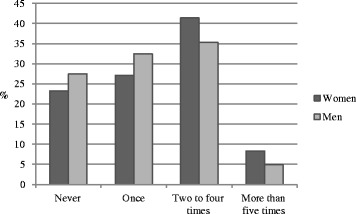
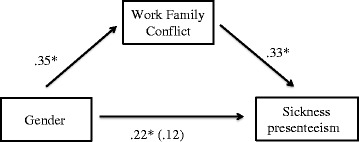
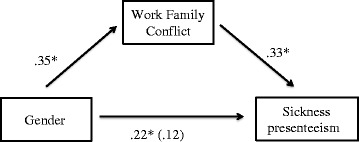
Fig. 1
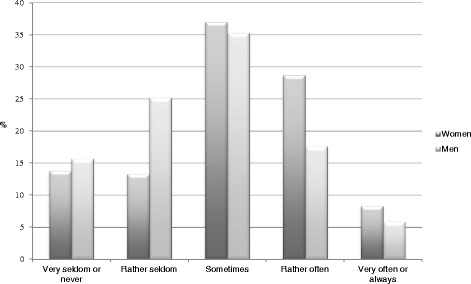
Fig. 2
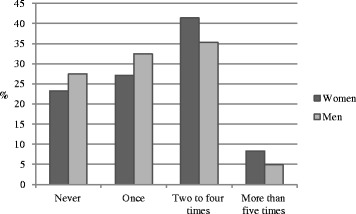
Fig. 3
| Women | Men | All | p-value | |||
|---|---|---|---|---|---|---|
| % | % | % | ||||
| Age | .260 | |||||
| <=44 | 44.2 | 34.3 | 40.5 | |||
| 45-54 | 26 | 29.4 | 27.2 | |||
| > = 55 | 29.8 | 36.3 | 32.2 | |||
| Position | .400 | |||||
| Residents | 30.9 | 23.5 | 28.2 | |||
| Specialist | 61.9 | 57.5 | 64.0 | |||
| Chief physicians | 7.2 | 8.8 | 7.8 | |||
| Marital status | .483 | |||||
| Married/or cohabiting | 82.3 | 84.3 | 83.0 | |||
| In a relation, not cohabitinga | 3.9 | 5.9 | 4.6 | |||
| Single* | 13.8 | 9.8 | 12.4 | |||
| M | SD | M | SD | M | ||
| Number kids | 1.97 | 1.05 | 1.83 | 1.22 | 1.92 | .313 |
| Working Time | 39.85 | 10.43 | 41.27 | 8.12 | 40.36 | .238 |
| Work-family conflict | 3.10 | 1.08 | 2.75 | 1.06 | 2.97 | .008 |
| General Health | 3.76 | 0.87 | 3.63 | 0.97 | 3.71 | .256 |
| Women (n = 158) | Men (n = 85) | |||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | p | ŋ p 2 | |
| Work piles up | 4.30 | 0.95 | 3.91 | 1.09 | 0.004 | 0.039 |
| Concern for colleagues | 3.76 | 0.99 | 3.52 | 1.11 | 0.082 | 0.012 |
| Concern for patients | 3.67 | 1.07 | 3.32 | 1.16 | 0.018 | 0.023 |
| Can handle it | 3.11 | 0.89 | 3.39 | 0.89 | 0.019 | 0.029 |
| Money loss | 2.18 | 1.20 | 2.64 | 1.25 | 0.006 | 0.030 |
*Gender differences were tested by chi-square analyses on frequencies and
aIn Sweden it is common that romantic partners do not live together. Therefor, this marital status was included in the questionnaire
 KSOEM
KSOEM

 Cite
Cite

