Abstract
-
Background
Formaldehyde was classified as a Group I Carcinogen by the International Agency for Research on Cancer (IARC) in 2006. While the IARC has stated that there is a lack of evidence that formaldehyde causes brain cancer, three meta-analyses have consistently reported a significantly higher risk of brain cancer in workers exposed to high levels of formaldehyde. Therefore, we report a case of a worker who was diagnosed with glioblastoma after being exposed to high concentrations of formaldehyde while working with formaldehyde resin in the paper industry.
-
Case presentation
A 40-year-old male patient joined an impregnated paper manufacturer and performed impregnation work using formaldehyde resin for 10 years and 2 months. In 2017, the patient experienced a severe headache and visited the hospital for brain magnetic resonance imaging, which revealed a mass. In the same year, the patient underwent a craniotomy for brain tumor resection and was diagnosed with glioblastoma of the temporal lobe. In 2019, a craniotomy was performed owing to the recurrence of the brain tumor, but he died in 2020. An exposure assessment of the work environment determined that the patient was exposed to formaldehyde above the exposure threshold of 0.3 ppm continuously for more than 10 years and that he had high respiratory and dermal exposure through performing work without wearing a respirator or protective gloves.
-
Conclusions
This case report represents the first instance where the epidemiological investigation and evaluation committee of the Occupational Safety and Health Research Institute in Korea recognized the scientific evidence of work-related brain tumors due to long-term exposure to high concentrations of formaldehyde during impregnated paperwork. This case highlights the importance of proper workplace management, informing workers that prolonged exposure to formaldehyde in impregnation work can cause brain tumors and minimizing exposure in similar processes.
-
Keywords: Brain neoplasms; Glioblastoma; Formaldehyde; Occupational exposure; Case reports
BACKGROUND
Brain tumors encompass neoplasms occurring within the brain parenchyma or ventricles, as well as meningiomas arising in the meninges and pituitary tumors originating in the pituitary gland. The incidence of brain tumors is higher in developed countries, with rates in Western Europe, North America, and Australia estimated at 6–11 cases per 100,000 men and 4–11 cases per 100,000 women.
1 Gliomas, the most common tumors of the brain parenchyma, originate from glial cells. They are histologically graded from 1 to 4, with glioblastoma representing the most malignant form (grade 4). Glioblastoma accounts for 12%–15% of all primary brain tumors and 50%–60% of all gliomas, characterized by rapid progression and a low 5-year survival rate.
2 According to the Centers for Disease Control and Prevention (CDC), the incidence of brain and nervous system cancer in the United States from 2015 to 2019 was 6 to 7 per 100,000 annually, with a mortality rate of 4 to 5 per 100,000.
3 The age-standardized incidence rate for brain tumors is 4.5 per 100,000. Statistical analysis reveals that glioblastoma incidence peaks at age 75, with overall brain and nervous system cancer incidence decreasing, whereas glioblastoma cases are on the rise.
4 In Korea, the 2019 National Cancer Registry reported 1,981 diagnoses of brain and central nervous system cancer, with an age-standardized incidence rate of 2.9 per 100,000.
5 The International Agency for Research on Cancer (IARC) identifies X and gamma radiation as established carcinogens with sufficient evidence for brain tumors, with radiofrequency electromagnetic fields classified as having limited evidence of carcinogenicity.
6
Since formaldehyde is used in various industries worldwide and its carcinogenicity has been confirmed, numerous epidemiological investigations and studies have focused on its effects.
7 An animal study in 1987 reported the occurrence of nasopharyngeal cancer due to formaldehyde exposure.
8 Subsequent studies have investigated the link between formaldehyde and the development of nasopharyngeal cancer and leukemia, reporting associations between them.
9,10 These studies concluded that formaldehyde is carcinogenic for both nasopharyngeal cancer and leukemia. In 2006, it was classified as a Group I Carcinogen by the IARC.
11 Historically, there have been reports of an increased risk of developing brain tumors among anatomists and preservative processors working with formaldehyde.
12,13 Based on these observations, additional studies were conducted to explore the relationship between formaldehyde exposure and the occurrence of brain tumors. However, later studies on formaldehyde exposure and cancer risk indicated that professional workers, such as pathologists, had a high statistical hazard ratio, but this was not observed in industrial workers.
14 Another study found no association between formaldehyde exposure and brain tumors in professionals, including preservative treatment providers.
15 Similarly, a further study reported no link between formaldehyde exposure and brain tumors among professional workers like embalmers.
15 These reports have led the IARC to conclude that the results of epidemiological studies on the association between formaldehyde exposure and brain tumors are inconsistent.
11 However, three meta-analyses reported in 1990, 2008, and 2021 have consistently reported a significantly higher risk of brain cancer in workers exposed to high levels of formaldehyde, such as professional workers.
14,16,17
We report a case where a worker in the paper industry, specifically in the impregnated paper manufacturing sector using formaldehyde resin, was diagnosed with glioblastoma following long-term exposure to high concentrations of formaldehyde. This is the first instance where a brain tumor, attributed to prolonged formaldehyde exposure, has been officially recognized as work-related by the epidemiological investigation and evaluation committee of the Occupational Safety and Health Research Institute (OSHRI) in Korea.
CASE PRESENTATION
Patient information
A 40-year-old male patient visited the emergency room of a local hospital due to a severe headache on September 15, 2017. He was transferred to the emergency room of the university hospital after a brain computed tomography (CT) scan performed at the local hospital revealed a parietal lobe mass. Brain magnetic resonance imaging (MRI), taken on September 17, 2017, showed a 2.7 cm-sized mass in the right temporal lobe, and a craniotomy and tumor resection was performed on September 26, 2017. After the craniotomy, the tumor was diagnosed as glioblastoma of the temporal lobe. The brain tumor recurred in January 2019, and a craniotomy was performed to resect it on February 14, 2019. Despite treatment, he died on February 4, 2020.
No specific findings were observed in his general health checkups from 2009 to 2017. He had a 10-pack-year history of smoking, drank one bottle at a time once or twice a week, and had no relevant family medical history of brain tumors. The worker complained of skin disease and received medical treatment multiple times during his employment, which was confirmed in the worker’s medical records collected in 2017 and statement from the bereaved family.
Occupational history
He worked for 1.5 months at a semiconductor packaging and manufacturing plant from August 8 to September 24, 1995. After that, he joined an impregnated paper manufacturer and worked there for 10 years and 2 months, from February 2, 2004, to March 2015, excluding periods of leave. He moved to a different role in cutting and loading products at the same company for one year and one month until January 2017, and he took an occupational break after leaving the company on January 27, 2017. He joined a different company in the same industry and was engaged in the impregnation process from July 3, 2017, until he was diagnosed with a brain tumor.
Exposure assessment
The worker was involved in the impregnation process, where, according to the Material Safety Data Sheets (MSDS) provided by the workplace, urea-formaldehyde resin and melamine-formaldehyde resin were used for the production of Low-Pressure Melamine impregnated paper at the first workplace. Toluene-4-sulphonate was polymerized as a curing agent and applied to decorative paper (
Supplementary Table 1). In the second workplace, phenol-formaldehyde resin was used to manufacture high-pressure laminate.
The work schedule at the first workplace involved a 2-team, 2-shift system, operating 6 days a week with alternating day and night shifts on a weekly basis. Working hours ranged from 8 to 20 hours a day (12 hours), specifically from 20:00 to 08:00 the next morning (12 hours), with lunch and dinner breaks lasting approximately 10 to 30 minutes each. In the second workplace, the schedule was a day shift, with working hours from 8:00 to 17:00, extending to 19:00 for overtime, and included a 1-hour lunch break.
The worker stated that he worked without protective equipment, and even during the on-site investigation of the 2 workplaces where the impregnation process took place, no respirators or protective gloves were observed to prevent formaldehyde exposure. In addition, equipment malfunctions during work caused him to perform unusual tasks as well as frequent cleaning.
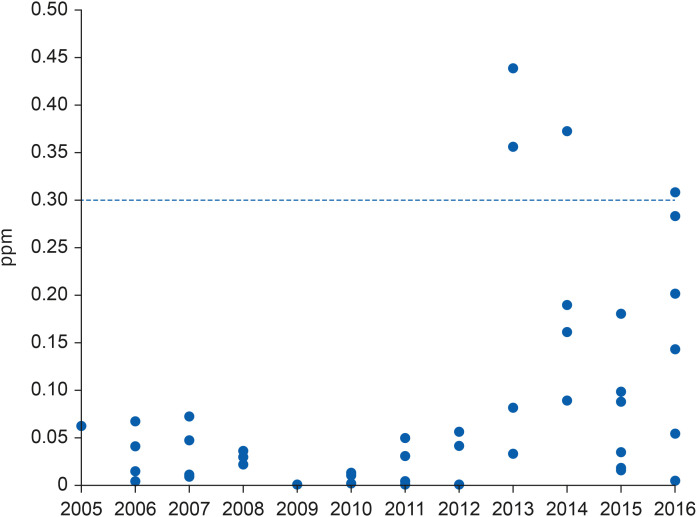
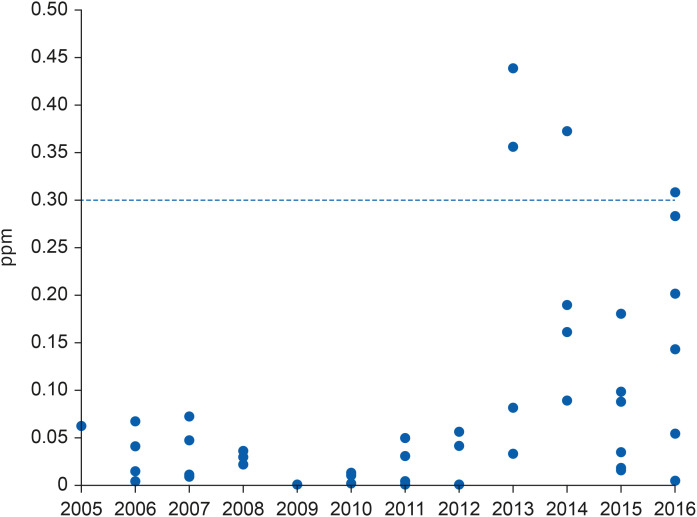
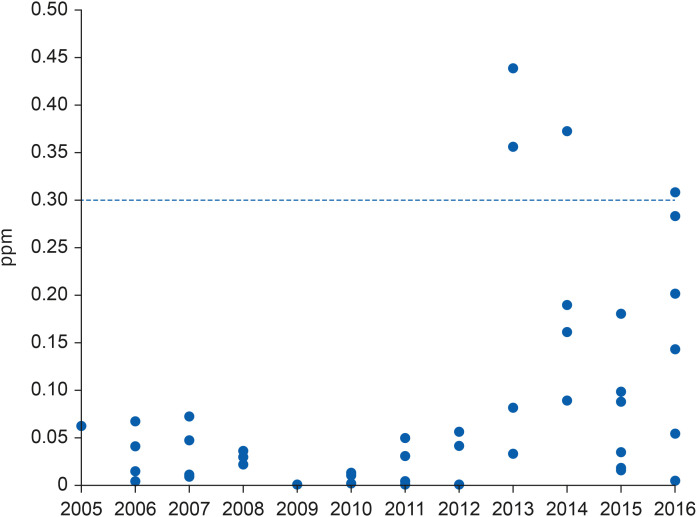
As a result of reviewing the work environment measurement results from 2005 to 2016 at the first workplace (
Table 1,
Fig. 1), it was found that workers were exposed to formaldehyde, formic acid, ammonia, and sodium hydroxide during the impregnation process. Notably, the average exposure level of formaldehyde was 0.072 ppm, which is 24% of the exposure standard (0.3 ppm). The highest measured value was 0.44 ppm, with 4 out of 60 measurements exceeding the exposure standard. In a parametric statistical analysis based on a lognormal distribution with 20 data points since 2013, the 95% upper limit of the measured formaldehyde value was 0.697 ppm, which is more than twice the exposure standard. Furthermore, the probability of the measured value exceeding the exposure standard was 17.3%.
Table 1Measurements of the first impregnated paper plant’s work environment
|
Years |
Workplace |
Harmful factors |
Measurement results (TWA) |
Exposure limit |
Unit |
Hazard ratio |
|
No. |
Average |
Range |
|
2005–2016 |
Impregnation |
Formaldehyde |
60 |
0.072 |
0.001–0.44 |
0.3 |
ppm |
0.24 |
|
Formic acid |
38 |
0.256 |
ND–1.156 |
5 |
ppm |
0.05 |
|
Ammonia |
26 |
0.071 |
ND–0.538 |
25 |
ppm |
0.003 |
|
Sodium hydroxide |
62 |
0.094 |
ND–0.743 |
2 |
mg/m3
|
0.05 |
|
Ethylene glycol |
16 |
- |
ND |
100 |
ppm |
- |
|
2-Butoxyethanol |
12 |
- |
ND |
20 |
ppm |
- |
|
Methanol |
0 |
- |
ND |
200 |
ppm |
|
Fig. 1Work-environment measurements of formaldehyde by year at the first workplace.
The second workplace did not conduct work environment measurements in 2017 when the worker was employed, so we reviewed the nearest work environment measurement results from the first half of 2018 (
Table 2). In the impregnation process, formaldehyde and methanol were detected, while phenol was not. The average concentration of formaldehyde was 0.056 ppm, which is 19% of the exposure limit, and the average concentration of methanol was 74.8 ppm, which is 37% of the exposure limit. Since the worker was setting up the line at the second workplace, it is generally expected that the exposure concentration of hazardous substances during such atypical work may be higher than during standardized daily operations.
Table 2Measurements of the second impregnated paper plant’s work environment
|
Years |
Workplace |
Harmful factors |
Measurement results (TWA) |
Exposure limit |
Unit |
Hazard ratio |
|
No. |
Average |
Range |
|
First half of 2018 |
Impregnation |
Formaldehyde |
2 |
0.056 |
0.06–0.05 |
0.3 |
ppm |
0.19 |
|
Phenol |
2 |
- |
ND |
5 |
ppm |
- |
|
Methanol |
2 |
74.8 |
57.2–92.4 |
200 |
ppm |
0.37 |
Formaldehyde exposure levels of workers at the first workplace were assessed through sampling and analysis, even though the workplace had moved to a different location than when the worker was employed there. Individual samples were collected and analyzed from 2 cutting/packing workers at the rear end of the impregnation line, where the worker mainly worked. The results were 0.284 and 0.247 ppm, respectively, with these high values constituting 95% of the exposure standard. The results of sampling and analysis for 2 local samples were 0.203 ppm at a distance of 1 m from the feed roll at the front of Impregnation Line Unit 2 and 0.341 ppm at a distance of 1 m from the packing roll (
Table 3).
Table 3Formaldehyde exposure assessment results for the first impregnated paper plant
|
Number |
Measurement location |
Personal/Area |
Measurement results |
Exposure limit |
Unit |
Hazard ratio |
|
1 |
Worker 1, Packing Unit 5 |
Personal |
0.284 |
0.3 |
ppm |
0.95 |
|
2 |
Worker 2, Packing Unit 5 |
Personal |
0.247 |
0.82 |
|
3 |
1 meter from the feed roll of impregnation unit 2 |
Area |
0.203 |
0.68 |
|
4 |
1-meter side of the Unit 2 packing roll |
Area |
0.341 |
1.14 |
Ethics statement
The OSHRI Institutional Review Board (IRB) approved the study protocol (IRB No. OSHRI-202206-HR-015). Written informed consent was obtained from the patient for publication of this case report and any accompanying data.
DISCUSSION AND CONCLUSION
We report the first case in which the epidemiological investigation and evaluation committee of the OSHRI recognized scientific evidence of occupational brain tumors caused by long-term exposure to high concentrations of formaldehyde during impregnated paperwork. The reasons for the relationship between brain tumor development and formaldehyde exposure are summarized as follows.
In this case, first, the age at which glioblastoma occurred in the workers was far from the typical age of predisposition.
4 Second, based on the results of work environment measurements and the literature on formaldehyde exposure evaluation conducted in the past, we estimated that the worker was continuously exposed to a high concentration of formaldehyde equivalent to that of professional workers during the manufacturing process of impregnated paper.
18,19 Third, the fact that the worker did not wear appropriate protective equipment while working and complained of skin diseases in medical records suggests both respiration and skin exposure. Therefore, despite the IARC’s current opinion that the association between formaldehyde and brain tumors is inconsistent,
11 the Committee recognized that based on the results of a recent meta-analysis,
14,16,17 the possibility of an increased risk of brain tumors due to continuous exposure to high concentrations of formaldehyde could not be excluded.
Combined with the report that epidemiological studies on the association between formaldehyde exposure and brain tumors in the IARC monograph
11 are inconsistent, formaldehyde was excluded from discussion in a study based on cohort studies showing an increase in the risk of central nervous system tumors in the paper industry.
20
However, a 2021 meta-analysis using 12 epidemiological studies on formaldehyde exposure and brain tumors and focusing on the group exposed to high concentrations of formaldehyde reports an increased risk of brain tumors in individuals exposed to high concentrations of formaldehyde (meta-relative risk [meta-RR]: 1.71; 95% confidence interval [CI]: 1.07–2.73).
16 In this study, subjects were divided into professional and industrial workers, with anatomists, pathologists, embalmers, and undertakers classified as professionals. There was a statistically significant increase in the risk of brain tumors due to formaldehyde exposure among professional workers (meta-RR: 2.42; 95% CI: 1.41–4.17) but not among industrial workers (meta-RR: 1.32; 95% CI: 0.72–2.44). These results suggest differences in exposure levels and patterns between industrial and professional workers, as initially found in studies on the incidence of leukemia and exposure to formaldehyde.
21 For example, embalmers and anatomists are more likely to be exposed to higher concentrations of formaldehyde than workers in industries involved in apparel. Past literature suggests that embalmers are exposed to levels of formaldehyde ranging from 1.32 to 2.86 ppm,
22 while anatomists and pathologists are exposed to levels between 0.7 and 3.7 ppm.
23 Professionals are also more likely to absorb formaldehyde through their skin during embalming or specimen preparation.
24 This absorption means that they may be exposed to formaldehyde through routes other than inhalation. On the other hand, the lower risk found for industrial workers is likely because these groups are exposed to much lower concentrations of formaldehyde compared to professional workers. For example, garment workers are typically exposed to levels between 0.09 and 0.20 ppm.
25 It can also be difficult to compare cohorts of workers from different industries, as industrial workers have a wider range of actual exposure levels due to their diverse occupations. Additionally, similar results to those reported in two meta-analyses are consistently reported (
Table 4).
14,16,17
Table 4 Comparison of meta-analysis results for brain tumors
|
Groups |
A result reported in 199017
|
A result reported in 200814
|
A result reported in 202116
|
|
No. |
Meta-RR (95% CI) |
No. |
Meta-RR (95% CI) |
No. |
Meta-RR (95% CI) |
|
Professional workers |
9 |
1.5 (1.2–2.0) |
7 |
1.56 (1.24–1.96) |
5 |
2.42 (1.41–4.17) |
|
Industrial workers |
3 |
0.9 (0.7–1.1) |
4 |
0.92 (0.75–1.13) |
7 |
1.32 (0.72–2.44) |
|
Whole workers |
12 |
1.29 (0.95–1.76) |
11 |
1.26 (1.01–1.59) |
12 |
1.71 (1.07–2.73) |
A previous study reports that formaldehyde induces brain tumors through the dysregulation of gene expression and post-translational abnormalities.
16 Specifically, the inflammation of olfactory neurons, along with oxidative stress and lipid peroxidation, may lead to the proliferation of mutant cells that contribute to brain tumor development.
16 Elevated levels of lipid peroxidation, which are indicative of oxidative stress, have been observed in brain tissues.
26 Additionally, brain tumor patients often exhibit diminished olfactory function, a condition known as anosmia,
27 which is also a consequence of formaldehyde exposure.
28 The olfactory epithelium of mammals continuously regenerates olfactory receptor neurons throughout an individual’s life; this process is facilitated and supported by olfactory envelope cells.
29 These olfactory envelope cells can also target glioblastoma stem-like cells selectively, increasing the risk of brain tumors.
30
The sample measurement results at the first workplace corroborate the work environment measurement results from the previous workplace, indicating that workers were exposed to formaldehyde exceeding the exposure limit for a prolonged period. Although there is a limitation that these measurements were taken at the new factory rather than where the worker was employed, interviews with fellow workers revealed no significant differences in the work environment. Therefore, considering past work environment measurement results and current exposure evaluation results, when converted to an 8-hour time-weighted average concentration for 12-hour workdays, 6 days a week, the concentration increases by more than 50%. The failure to wear appropriate protective equipment while working, abnormal work and frequent cleaning due to equipment malfunctions, and these factors suggest that workers were continuously exposed to formaldehyde levels exceeding the current exposure standard (0.3 ppm) set by the Ministry of Employment and Labor over the 10 years and 2 months of working in the impregnation process. Furthermore, the American Conference of Governmental Industrial Hygienists sets the formaldehyde exposure limit at 0.1 ppm time-weighted average, with a short-term exposure limit of 0.3 ppm. This indicates that workers were continuously exposed to formaldehyde at levels more than three times the recommended standard. Additionally, considering the measurement results from local samples, it is estimated that workers were continuously exposed to formaldehyde during their work, albeit at lower levels than in the impregnation work involving cutting and loading products. Moreover, there has been a report
18 indicating that the process of polymerizing and coating melamine-formaldehyde resin and urea-formaldehyde resin with toluene-4-sulfonate, a curing agent, for impregnating patterned paper at the first workplace leads to high concentrations of formaldehyde exposure, supporting the evidence of long-term exposure exceeding exposure limits.
Considering that the worker was also exposed to a significant level of formaldehyde for 2.5 months before the diagnosis of a brain tumor at the second workplace, and given that he performed the production line setup, it cannot be excluded that he was exposed to a level of formaldehyde exceeding the exposure standard set by the Ministry of Employment and Labor during atypical work. Additionally, given that workers have continuously complained about skin diseases and medical records confirm these complaints, they were likely exposed to harmful substances such as formaldehyde through skin contact during their work.
The worker in this case was involved in the process of coating paper with formaldehyde-based resin using calendering machines at the workplace (
Supplementary Fig. 1). In 2004, the IARC’s international epidemiological study on chemical solvent occupational exposure in the pulp and paper industry reported high exposure to formaldehyde in the process of calendering and using machinery, particularly among paper industry workers producing coating products with formaldehyde-based urea, phenol, and melamine resins.
19 This indicates that the level and probability of formaldehyde exposure were higher for workers in this case than for workers in other industries.
A limitation of this case report is that we did not review studies that had reported an association between individual types of brain tumors (i.e., glioblastoma) and formaldehyde exposure; instead, we only reviewed reports of associations between overall brain-tumor development and formaldehyde exposure. Since we only found previous studies that evaluated formaldehyde with regard to brain tumors as a whole, but not for individual types of brain tumors. We estimated that this is likely because brain tumors have one of the lowest incidences among all diseases.
In conclusion, this case demonstrates that industrial workers manufacturing impregnated paper with formaldehyde resin can be exposed to formaldehyde at levels comparable to those experienced by professional workers. Furthermore, it highlights the potential health effects of long-term exposure to high concentrations of formaldehyde, such as brain tumors, in addition to lympho-hematopoietic cancer. It also underscores the importance of proper work environment management to prevent exposure to high concentrations of formaldehyde. Moreover, it is necessary to investigate the risk of brain tumors, including glioblastoma, in industrial workers who are involved in the coating process using formaldehyde resin.
Acknowledgements
The present study utilized workers’ data that were formally obtained from the Occupational Safety and Health Research Institute, and the Korean Occupational Safety and Health Agency and did not include identifiable personal information.
Abbreviations
Chemical Abstract Service
Centers for Disease Control and Prevention
International Agency for Research on Cancer
magnetic resonance imaging
Material Safety Data Sheet
Occupational Safety and Health Institute
NOTES
-
Competing interests: The authors declare that they have no competing interests.
-
Authors contributions:
Conceptualization: Ye S, Kwon J, Lee Y.
Data curation: Lee Y, Jang M.
Investigation: Ye S, Kwon J, Lee Y.
Writing - original draft: Lee Y.
Writing - review & editing: Ye S, Kwon J, Ma S, Jun KY, Yoon M, Lee Y.
SUPPLEMENTARY MATERIALS
Supplementary Table 1
Components of chemicals (MSDS data of the first workplace)
aoem-36-e17-s001.xls
REFERENCES
REFERENCES
- 1. Ferlay J, Bray F, Pisani P, Parkin DM. GLOBOCAN 2000: Cancer Incidence, Mortality and Prevalence Worldwide, Version 1.0. Lyon, France: IARC Press; 2001.
- 2. Tykocki T, Eltayeb M. Ten-year survival in glioblastoma. A systematic review. J Clin Neurosci 2018;54:7–13. 29801989.ArticlePubMed
- 3. U.S. Cancer Statistics Working Group. U.S. Cancer Statistics Data Visualizations Tool, based on 2021 submission data (1999-2019): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute. Updated June 2022]. Accessed April 25, 2022].
www.cdc.gov/cancer/dataviz
.
- 4. Li K, Lu D, Guo Y, Wang C, Liu X, Liu Y, et al. Trends and patterns of incidence of diffuse glioma in adults in the United States, 1973-2014. Cancer Med 2018;7(10):5281–5290. 30175510.ArticlePubMedPMCPDF
- 5. Korea Central Cancer Registry. Annual Report of Cancer Statistics in Korea in 2019. Goyang, Korea: National Cancer Center; 2021.
- 6. International Agency for Research on Cancer (IARC). World Health Organization. List of Classifications by Cancer Sites with Sufficient or Limited Evidence in Humans, IARC Monographs Volumes 1–132. Lyon, France: IARC; 2022.
- 7. Swenberg JA, Moeller BC, Lu K, Rager JE, Fry RC, Starr TB. Formaldehyde carcinogenicity research: 30 years and counting for mode of action, epidemiology, and cancer risk assessment. Toxicol Pathol 2013;41(2):181–189. 23160431.ArticlePubMedPMCPDF
- 8. Roush GC, Walrath J, Stayner LT, Kaplan SA, Flannery JT, Blair A. Nasopharyngeal cancer, sinonasal cancer, and occupations related to formaldehyde: a case-control study. J Natl Cancer Inst 1987;79(6):1221–1224. 3480373.PubMed
- 9. Bachand AM, Mundt KA, Mundt DJ, Montgomery RR. Epidemiological studies of formaldehyde exposure and risk of leukemia and nasopharyngeal cancer: a meta-analysis. Crit Rev Toxicol 2010;40(2):85–100. 20085478.ArticlePubMed
- 10. Kwon SC, Kim I, Song J, Park J. Does formaldehyde have a causal association with nasopharyngeal cancer and leukaemia? Ann Occup Environ Med 2018;30(1):5. 29423228.ArticlePubMedPMCPDF
- 11. International Agency for Research on Cancer (IARC). World Health Organization. Formaldehyde. Chemical Agents and Related Occupations. IARC Monographs on the Evaluation of Carcinogenic Risks to Human, Volume 100F. Lyon, France: IARC; 2012, 401–436.
- 12. Walrath J, Fraumeni JF Jr. Cancer and other causes of death among embalmers. Cancer Res 1984;44(10):4638–4641. 6467219.PubMed
- 13. Stroup NE, Blair A, Erikson GE. Brain cancer and other causes of death in anatomists. J Natl Cancer Inst 1986;77(6):1217–1224. 3467114.PubMed
- 14. Bosetti C, McLaughlin JK, Tarone RE, Pira E, La Vecchia C. Formaldehyde and cancer risk: a quantitative review of cohort studies through 2006. Ann Oncol 2008;19(1):29–43. 17897961.ArticlePubMed
- 15. Lacourt A, Cardis E, Pintos J, Richardson L, Kincl L, Benke G, et al. INTEROCC case-control study: lack of association between glioma tumors and occupational exposure to selected combustion products, dusts and other chemical agents. BMC Public Health 2013;13(1):340. 23587105.ArticlePubMedPMCPDF
- 16. Rana I, Rieswijk L, Steinmaus C, Zhang L. Formaldehyde and brain disorders: a meta-analysis and bioinformatics approach. Neurotox Res 2021;39(3):924–948. 33400181.ArticlePubMedPMCPDF
- 17. Blair A, Saracci R, Stewart PA, Hayes RB, Shy C. Epidemiologic evidence on the relationship between formaldehyde exposure and cancer. Scand J Work Environ Health 1990;16(6):381–393. 2284588.ArticlePubMed
- 18. Ratnasingam J, Natthondan V, Ioras F, McNulty T. Dust, noise and chemical solvents exposure of workers in the wooden furniture industry in South East Asia. J Appl Sci (Faisalabad) 2010;10(14):1413–1420.Article
- 19. Korhonen K, Liukkonen T, Ahrens W, Astrakianakis G, Boffetta P, Burdorf A, et al. Occupational exposure to chemical agents in the paper industry. Int Arch Occup Environ Health 2004;77(7):451–460. 15368059.ArticlePubMedPDF
- 20. Andersson E, Nilsson R, Torén K. Gliomas among men employed in the Swedish pulp and paper industry. Scand J Work Environ Health 2002;28(5):333–340. 12432987.ArticlePubMed
- 21. Jiang X, Zhang R, Wang Y, Lu P, Gu X. Study on the tumor mortality of a retrospective cohort of formaldehyde exposed workers in chemical industry. Chin J Ind Hyg Occup Dis 1990;8(5):261–264.
- 22. Hiipakka DW, Dyrdahl KS, Garcia Cardenas M. Successful reduction of morticians’ exposure to formaldehyde during embalming procedures. AIHAJ 2001;62(6):689–696. 11767933.ArticlePubMed
- 23. Dias-Teixeira M, Domingues V, Dias-Teixeira A, Teles T, Delerue-Matos C. Risk of exposure to formaldehyde in pathological anatomy laboratories. Advances in Safety Management and Human Factors. Cham, Switzerland: Springer; 2016, 379–385.
- 24. Boeniger MF, Stewart P. Biological Markers for Formaldehyde Exposure in Mortician Students, Report II: Extent of Exposure, Final Report. Report number IWSB 125.27. Washington, D.C., USA: National Institute for Occupational Safety and Health; 1992.
- 25. Pinkerton LE, Hein MJ, Stayner LT. Mortality among a cohort of garment workers exposed to formaldehyde: an update. Occup Environ Med 2004;61(3):193–200. 14985513.ArticlePubMedPMC
- 26. Popov B, Gadjeva V, Valkanov P, Popova S, Tolekova A. Lipid peroxidation, superoxide dismutase and catalase activities in brain tumor tissues. Arch Physiol Biochem 2003;111(5):455–459. 16026034.ArticlePubMed
- 27. Daniels C, Gottwald B, Pause BM, Sojka B, Mehdorn HM, Ferstl R. Olfactory event-related potentials in patients with brain tumors. Clin Neurophysiol 2001;112(8):1523–1530. 11459693.ArticlePubMed
- 28. Hisamitsu M, Okamoto Y, Chazono H, Yonekura S, Sakurai D, Horiguchi S, et al. The influence of environmental exposure to formaldehyde in nasal mucosa of medical students during cadaver dissection. Allergol Int 2011;60(3):373–379. 21593581.ArticlePubMed
- 29. Schwob JE. Neural regeneration and the peripheral olfactory system. Anat Rec 2002;269(1):33–49. 11891623.ArticlePubMed
- 30. Carvalho LA, Teng J, Fleming RL, Tabet EI, Zinter M, de Melo Reis RA, et al. Olfactory ensheathing cells: a Trojan horse for glioma gene therapy. J Natl Cancer Inst 2019;111(3):283–291. 30257000.ArticlePubMedPMC
 , Jiwoon Kwon2,3
, Jiwoon Kwon2,3 , Miyeon Jang1
, Miyeon Jang1 , Seongwon Ma1,4
, Seongwon Ma1,4 , Kyo Yeon Jun2
, Kyo Yeon Jun2 , Minjoo Yoon2
, Minjoo Yoon2 , Shinhee Ye2
, Shinhee Ye2





 KSOEM
KSOEM

 Cite
Cite

