Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 28; 2016 > Article
- Research Article Long working hours and overweight and obesity in working adults
- Byung-Mi Kim1, Bo-Eun Lee2, Hye-Sook Park3, Young-Ju Kim4, Young-Ju Suh5,6, Jeong-youn Kim7, Ji-Young Shin3, Eun-Hee Ha3
-
Annals of Occupational and Environmental Medicine 2016;28(1):36.
DOI: https://doi.org/10.1186/s40557-016-0110-7
Published online: August 22, 2016
1National cancer control Institute, National Cancer Center, Goyang, South Korea 
2Environmental Health Research Division, Environmental Health Research Department, National Institute of Environmental Research, Ministry of Environment, Incheon, South Korea 
3Department of Preventive Medicine, School of Medicine, Ewha Womans University, Seoul, South Korea 
4Department of Obstetrics and Gynecology, School of Medicine, Ewha Womans University, Seoul, South Korea 
5Department of Biostatistics, Inha University Hospital and Center for Advanced Medical Education by BK21 project, College of Medicine, Inha University, Shinheung-dong 3ga, Chung-gu, Incheon, Korea 
6Chronic Diseases Research Division, Korea Center for Disease Control and Prevention, Seoul, South Korea 
7Worker Health Protection Division, Occupational safety and health Bureau, Ministry of labor Government Complex III, Seoul, South Korea 
© Ha. 2016
Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Abstract
-
Background Previous studies have identified a link between gender and the various risk factors associated with obesity. We examined obesity risk factors in working adults to identify the effects of differences in body mass index (BMI) and percentage body fat (PBF) between women and men.
-
Methods A total of 1,120 adults agreed to participate in the study. Data from 711 participants, including 411 women and 300 men, were analyzed. Multiple logistic regression analysis was used to estimate the effects of risk factors on obesity and being overweight. In addition, the least-squares (LS) means of both BMI and PBF were estimated by analysis of covariance (ANCOVA) in a generalized linear model.
-
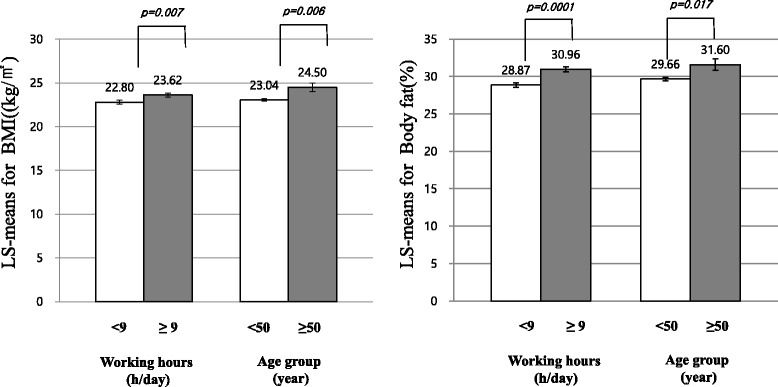
Results Increases in BMI and PBF were significantly related to an age > 50 years and long working hours in women after compensating for confounding factors. Using the PBF criterion, the odds ratio (OR) of being overweight or obese in women > 50 years of age who worked for > 9 h a day was 3.9 (95% confidence interval [CI], 1.05–11.00). For BMI, women who were > 50 years of age and worked for > 9 h a day were 3.82 times (95% CI, 1.31–11.14) more likely to be overweight or obese than those who were < 50 years of age and worked for < 9 h a day.
-
Conclusion Obesity in working adults was associated with > 50 years of age and long working hours in women. Further studies are needed to investigate the underlying mechanisms of this relationship and its potential implications for the prevention and management of excess weight and obesity.
Background
Methods
Results
Discussion
Conclusions
Acknowledgements
Abbreviations
ANCOVA
BIA
BMI
IRB
LS means
MONICA
PBF
WHO
- 1. Keeffe EB, Adesman PW, Stenzel P, Palmer RM. Steatosis and cirrhosis in an obese diabetic. Dig Dis Sci 1987;32(4):441–445. 10.1007/BF01296300. 3829884.ArticlePubMedPDF
- 2.
- 3. Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev 2007;29:6–28. 10.1093/epirev/mxm007. 17510091.ArticlePubMed
- 4.
- 5.
- 6. Kim HJ, Kim Y, Cho Y, Jun B, Oh KW. Trends in the prevalence of major cardiovascular disease risk factors among Korean adults: results from the Korea National Health and Nutrition Examination Survey, 1998–2012. Int J Cardiol 2014;174(1):64–72. 10.1016/j.ijcard.2014.03.163. 24742812.ArticlePubMed
- 7. Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA 2002;288(14):1723–1727. 10.1001/jama.288.14.1723. 12365955.ArticlePubMed
- 8. Martinez JA, Kearney JM, Kafatos A, Paquet S, Martínez-Gonzélez MA. Variables independently associated with self-reported obesity in the European Union. Public Health Nutr 1999;2(1a):125–133. 10.1017/S1368980099000178. 10933632.ArticlePubMed
- 9.
- 10.
- 11. ..
- 12. Lallukka T, Sarlio-Lahteenkorva S, Kaila-Kangas L, Pitkaniemi J, Luukkonen R, Leino-Arjas P. Working conditions and weight gain: a 28-year follow-up study of industrial employees. Eur J Epidemiol 2008;23(4):303–310. 10.1007/s10654-008-9233-7. 18322807.ArticlePubMedPDF
- 13.
- 14. Ostry AS, Radi S, Louie AM, LaMontagne AD. Psychosocial and other working conditions in relation to body mass index in a representative sample of Australian workers. BMC Public Health 2006;6:53. 10.1186/1471-2458-6-53. 16512915.ArticlePubMedPMCPDF
- 15. Kong M-H. Economic Development and Women’s Status in Korea. Contemp South Korean Soc 2013;26:41.
- 16. Gynaecol ANZJO. 1. WHO: Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000;894:1–253.
- 17. Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960–1994. Int J Obes Relat Metab Disord 1998;22(1):39–47. 10.1038/sj.ijo.0800541. 9481598.ArticlePubMedPDF
- 18. Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. Jama 2001;286(10):1195–1200. 10.1001/jama.286.10.1195. 11559264.ArticlePubMed
- 19. Kuskowska-Wolk A, Rössner S. Body mass distribution of a representative adult population in Sweden. Diabetes Res Clin Pract 1990;10:S37–S41. 10.1016/0168-8227(90)90138-J. 2286149.ArticlePubMed
- 20. Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA 2004;291(23):2847–2850. 10.1001/jama.291.23.2847. 15199035.ArticlePubMed
- 21. Haarbo J, Marslew U, Gotfredsen A, Christiansen C. Postmenopausal hormone replacement therapy prevents central distribution of body fat after menopause. Metabolism 1991;40(12):1323–1326. 10.1016/0026-0495(91)90037-W. 1961129.ArticlePubMed
- 22. Godsland I, Wynn V, Crook D, Miller N. Sex, plasma lipoproteins, and atherosclerosis: prevailing assumptions and outstanding questions. Am Heart J 1987;114(6):1467–1503. 10.1016/0002-8703(87)90552-7. 3318361.ArticlePubMed
- 23. Iwao S, Iwao N, Muller DC, Elahi D, Shimokata H, Andres R. Effect of aging on the relationship between multiple risk factors and waist circumference. J Am Geriatr Soc 2000;48(7):788–794. 10.1111/j.1532-5415.2000.tb04754.x. 10894318.ArticlePubMed
- 24. Trémollieres FA, Pouilles J-M, Ribot CA. Relative influence of age and menopause on total and regional body composition changes in postmenopausal women. Am J Obstet Gynecol 1996;175(6):1594–1600. 10.1016/S0002-9378(96)70111-4. 8987946.ArticlePubMed
- 25. Boynton A, Neuhouser ML, Sorensen B, McTiernan A, Ulrich CM. Predictors of diet quality among overweight and obese postmenopausal women. J Am Diet Assoc 2008;108(1):125–130. 10.1016/j.jada.2007.10.037. 18155998.ArticlePubMed
- 26. Mayes J, Watson G. Direct effects of sex steroid hormones on adipose tissues and obesity. Obes Rev 2004;5(4):197–216. 10.1111/j.1467-789X.2004.00152.x. 15458395.ArticlePubMed
- 27.
- 28. Jang T-W, Kim H-R, Lee H-E, Myong J-P, Koo J-W. Long work hours and obesity in Korean adult workers. J Occup Health 2013;55(5):359–366. 10.1539/joh.13-0043-OA. 23892643.ArticlePubMedPDF
- 29. Porter JS, Bean MK, Gerke CK, Stern M. Psychosocial factors and perspectives on weight gain and barriers to weight loss among adolescents enrolled in obesity treatment. J Clin Psychol Med Settings 2010;17(2):98–102. 10.1007/s10880-010-9186-3. 20119710.ArticlePubMedPDF
- 30. Chrousos G. The role of stress and the hypothalamic-pituitary-adrenal axis in the pathogenesis of the metabolic syndrome: neuro-endocrine and target tissue-related causes. Int J Obes Relat Metab Disord 2000;24:S50–55. 10.1038/sj.ijo.0801278. 10997609.ArticlePubMedPDF
- 31. Chaput JP, Després JP, Bouchard C, Tremblay A. Short sleep duration is associated with reduced leptin levels and increased adiposity: results from the Quebec family study. Obesity 2007;15(1):253–261. 10.1038/oby.2007.512. 17228054.ArticlePubMed
- 32. Forbes S, Bui S, Robinson BR, Hochgeschwender U, Brennan MB. Integrated control of appetite and fat metabolism by the leptin-proopiomelanocortin pathway. Proc Natl Acad Sci 2001;98(7):4233–4237. 10.1073/pnas.071054298. 11259669.ArticlePubMedPMC
- 33. Flier JS, Elmquist JK. A good night’s sleep: future antidote to the obesity epidemic? Ann Intern Med 2004;141(11):885–886. 10.7326/0003-4819-141-11-200412070-00014. 15583232.ArticlePubMed
- 34.
- 35. Maruyama S, Morimoto K. Effects of long workhours on life-style, stress and quality of life among intermediate Japanese managers. Scand J Work Environ Health 1996;22:353–359. 10.5271/sjweh.153. 8923608.ArticlePubMed
- 36. Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer 2004;4(8):579–591. 10.1038/nrc1408. 15286738.ArticlePubMedPDF
- 37. James PT, Leach R, Kalamara E, Shayeghi M. The worldwide obesity epidemic. Obes Res 2001;9(S11):228S–233S. 10.1038/oby.2001.123. 11707546.ArticlePubMed
- 38. Kang S-J, Song Y, Kim D-Y, Kim S-H, Park J-H. Validation of Bioelectrical Impedance Analyzer for Measuring Percentage of Body Fat. Fort Worth, Texas: 2008 AAHPERD National Convention and Exposition: 2008. 2008.
REFERENCES
Figure & Data
REFERENCES
Citations

- The association between working hours and working type with non-alcoholic fatty liver disease: results from the NHANES 1999-2014
Ruli Wang, Ningxi Wu, Huan Qu, Xiaowei Zheng, Haoyang Zhang, Lihong Zhu, Xiaolei Wang, Xiaodie Yao, Le Zhang
Frontiers in Endocrinology.2025;[Epub] CrossRef - Association of long working hours with visceral adiposity index, anthropometric indices, and weight management behaviors: a study of Korean workers
Seong-Uk Baek, Jin-Ha Yoon
Family Practice.2025;[Epub] CrossRef - Obesity and cardiovascular risk factors among internists in Indonesia
Sally Aman Nasution, Lugyanti Sukrisman, Eka Ginanjar, Evy Yunihastuti, Simon Salim, Rudy Hidayat, Muhadi Muhadi, Siprianus Ugroseno Yudho Bintoro, Asri Ludin Tambunan, Hery Djagat Purnomo, Andi Makbul Aman, Mohammad Robikhul Ikhsan, Ahmad Mekah, Angkasa
Frontiers in Endocrinology.2025;[Epub] CrossRef - Relationship between consumption of high fat, sugar or sodium (HFSS) food and obesity and non-communicable diseases
Sasinee Thapsuwan, Sirinya Phulkerd, Aphichat Chamratrithirong, Rossarin Soottipong Gray, Nongnuch Jindarattanaporn, Nutnicha Loyfah, Natjera Thongcharoenchupong, Umaporn Pattaravanich
BMJ Nutrition, Prevention & Health.2024; 7(1): 78. CrossRef - Night shift-induced circadian disruption: links to initiation of non-alcoholic fatty liver disease/non-alcoholic steatohepatitis and risk of hepatic cancer
Anjali Singh, Baby Anjum, Qulsoom Naz, Sana Raza, Rohit A. Sinha, Mohammad Kaleem Ahmad, Abbas Ali Mehdi, Narsingh Verma
Hepatoma Research.2024;[Epub] CrossRef - Fenugreek (Trigonella foenum-graecum L.) Modulates Energy Metabolism
and Anti-inflammatory Response in Obesity via Combinatorial Analysis
Fong Fong Liew, Theysshana Visuvanathan, Shalini Vellasamy
The Natural Products Journal.2023;[Epub] CrossRef - The association between long working hours and obstructive sleep apnea assessed by STOP-BANG score: a cross-sectional study
Dong-Wook Lee, Jongin Lee
International Archives of Occupational and Environmental Health.2023; 96(2): 191. CrossRef - The social determinants of health influencing obesity for the aged in the Pakpoon community context: A qualitative study
Pornchanuch Chumpunuch, Urai Jaraeprapal
International Journal of Nursing Sciences.2022; 9(2): 211. CrossRef - You Can’t Avoid Shift Work? Then Focus on Body Fat Rather than Weight
Eun Kyung Lee
Endocrinology and Metabolism.2022; 37(5): 756. CrossRef - Maternal working hours and smoking and drinking in adolescent children: based on the Korean National Health and Nutrition Examination Survey VI and VII
Tae-Hwi Park, Yong-Duk Ahn, Jeong-Bae Rhie
Annals of Occupational and Environmental Medicine.2021;[Epub] CrossRef - Long working hours are associated with a higher risk of non-alcoholic fatty liver disease: A large population-based Korean cohort study
Yesung Lee, Eunchan Mun, Soyoung Park, Woncheol Lee, Jee-Fu Huang
PLOS ONE.2021; 16(7): e0255118. CrossRef - Long Working Hours and Risk of Nonalcoholic Fatty Liver Disease: Korea National Health and Nutrition Examination Survey VII
Eyun Song, Jung A. Kim, Eun Roh, Ji Hee Yu, Nam Hoon Kim, Hye Jin Yoo, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi
Frontiers in Endocrinology.2021;[Epub] CrossRef - The causes of obesity: an in-depth review
Tahir Omer
Advances in Obesity, Weight Management & Control.2020; 10(4): 90. CrossRef - Association between Occupational Characteristics and Overweight and Obesity among Working Korean Women: The 2010–2015 Korea National Health and Nutrition Examination Survey
Mi-Jung Eum, Hye-Sun Jung
International Journal of Environmental Research and Public Health.2020; 17(5): 1585. CrossRef - Factors Associated with the Nutritional Status among Male Workers of Iron and Steel Industries in Bara District, Nepal
Raj Kumar Sangroula, Hari Prasad Subedi, Kalpana Tiwari
Journal of Nutrition and Metabolism.2020; 2020: 1. CrossRef - Obesity Fact Sheet in Korea, 2019: Prevalence of Obesity and Abdominal Obesity from 2009 to 2018 and Social Factors
Ga Eun Nam, Yang-Hyun Kim, Kyungdo Han, Jin-Hyung Jung, Eun-Jung Rhee, Seong-Su Lee, Dae Jung Kim, Kwan-Woo Lee, Won-Young Lee
Journal of Obesity & Metabolic Syndrome.2020; 29(2): 124. CrossRef - Gender differences and occupational factors for the risk of obesity in the Italian working population
C. Di Tecco, L. Fontana, G. Adamo, M. Petyx, S. Iavicoli
BMC Public Health.2020;[Epub] CrossRef - Long working hours, anthropometry, lung function, blood pressure and blood-based biomarkers: cross-sectional findings from the CONSTANCES study
Marianna Virtanen, Linda Magnusson Hansson, Marcel Goldberg, Marie Zins, Sari Stenholm, Jussi Vahtera, Hugo Westerlund, Mika Kivimäki
Journal of Epidemiology and Community Health.2019; 73(2): 130. CrossRef - Physical fitness, musculoskeletal disorders and body mass index in transport drivers from Barranquilla, Colombia
Martha Mendinueta-Martínez, Yaneth Herazo-Beltrán, José Vidarte-Claros, Estela Crissien-Quiroz, Roberto Rebolledo-Cobos
Revista de la Facultad de Medicina.2019; 67(4): 407. CrossRef - Auswirkungen verkürzter Ruhezeiten auf Gesundheit und Work-Life-Balance bei Vollzeitbeschäftigten: Ergebnisse der BAuA-Arbeitszeitbefragung 2017
Nils Backhaus, Corinna Brauner, Anita Tisch
Zeitschrift für Arbeitswissenschaft.2019; 73(4): 394. CrossRef - Lung morbidity of traffic wardens exposed to chronic vehicular pollution in Lahore, Pakistan
International Journal of Biosciences (IJB).2019; : 294. CrossRef - Evaluation for Fatigue and Accident Risk of Korean Commercial Bus Drivers
Hogil Kim, Tae-Won Jang, Hyoung-Ryoul Kim, Seyoung Lee
The Tohoku Journal of Experimental Medicine.2018; 246(3): 191. CrossRef
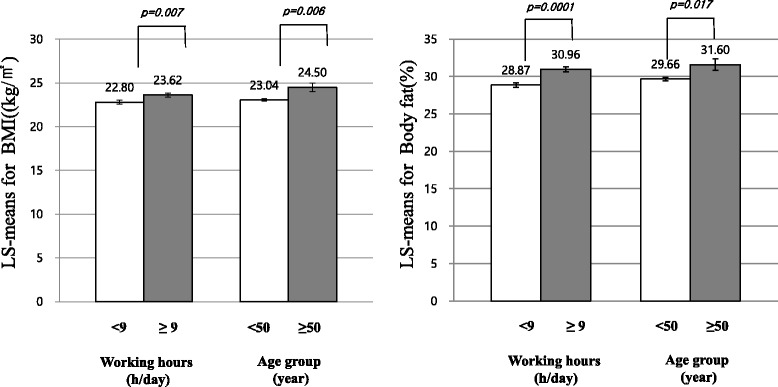
Fig. 1
| Variable | N (%), Mean ± SD | |
|---|---|---|
| Women(N = 411) | Men(N = 300) | |
| General characteristics | ||
| Age group | ||
| 40–49 | 220(53.5) | 141(47) |
| 50–59 | 123(37.5) | 111(37) |
| ≥ 60 | 57(17.4) | 48(16) |
| Marital status | ||
| Unmarried | 10(2.5) | 8(2.7) |
| Married | 367(91.5) | 277(93.9) |
| Divorced/Widow/Widower | 24(6.0) | 10(3.4) |
| Educational level | ||
| Low | 200(48.7) | 129(43) |
| Middle | 191(46.5) | 136(45.3) |
| High | 20(4.9) | 35(11.7) |
| Household income (US$/Month) | ||
| < 2,000 | 21(5.8) | 18(6.3) |
| 2,000–3,000 | 18(5) | 17(6.0) |
| ≥ 3,000 | 321(89.2) | 249(87.7) |
| Smoking | ||
| Non-smoker | 396(96.3) | 86(28.7) |
| Smoker | 15(3.7) | 214(71.3) |
| Alcohol consumption | ||
| Non-drinking | 284(69.1) | 54(18) |
| Drinking | 127(30.9) | 246(82) |
| Anthropometric characteristics | ||
| BMI(kg/m2)* | 23.2 ± 2.9 | 24.5 ± 2.7 |
| Prevalence of overweight(%)+ | 102(24.8 %) | 85(28.3 %) |
| Prevalence of obesity(%)+ | 97 (23.6 %) | 134(44.7 %) |
| PBF(%)* | 27.3 ± 5.3 | 23.9 ± 4.5 |
| Prevalence of overweight(%)+ | 156 (38.0 %) | 115 (38.3 %) |
| Prevalence of obesity(%)+ | 48 (11.7 %) | 136(45.3 %) |
| Lean body mass(kg)* | 36.9 ± 3.5 | 48.9 ± 4.5 |
| BMI (kg/m2) | PBF (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Women | Men | Women | Men | |||||
| Variable | Controls* | Cases+ | Controls* | Cases+ | Controls* | Cases+ | Controls* | Cases+ |
| (N = 207) | (N = 204) | (N = 81) | (N = 219) | (N = 207) | (N = 204) | (N = 49) | (N = 251) | |
| Age group | ||||||||
| 40–49 | 126 (59.4) | 94 (47.2) | 34 (42) | 107 (42) | 132 (63.8) | 88 (43.1) | 25 (51) | 116 (46.2) |
| 50–59 | 69 (32.6) | 79 (39.7) | 31 (38.3) | 80 (38.3) | 67 (32.4) | 81 (39.7) | 17 (34.7) | 94 (37.5) |
| ≥ 60 | 17 (8) | 26 (13.1) | 16 (19.8) | 32 (19.8) | 8 (3.9) | 35 (17.2) | 7 (14.3) | 41 (16.3) |
| p = 0.01 | p = 0.21 | p < 0.0001 | p = 0.55 | |||||
| Marital status | ||||||||
| Unmarried | 5 (2.4) | 5 (2.6) | 3 (3.8) | 5 (2.3) | 5 (2.5) | 5 (2.5) | 1 (2) | 7 (2.9) |
| Married | 191 (92.3) | 176 (90.7) | 74 (92.5) | 203 (94.4) | 187 (92.6) | 180 (90.5) | 45 (91.8) | 232 (94.3) |
| Divorced/Widow/Widower | 11 (5.3) | 13 (6.7) | 3 (3.8) | 7 (3.3) | 10 (5) | 14 (7) | 3 (6.1) | 7 (2.9) |
| p = 0.67 | p = 0.79 | p = 0.48 | p = 0.29 | |||||
| Educational level | ||||||||
| Low | 89 (42) | 111 (55.8) | 36 (44.4) | 93 (42.5) | 89 (43) | 111 (54.4) | 23 (46.9) | 106 (42.2) |
| Middle | 110 (51.9) | 81 (40.7) | 40 (49.4) | 96 (43.8) | 104 (50.2) | 87 (42.7) | 22 (44.9) | 114 (45.4) |
| High | 13 (6.1) | 7 (3.5) | 5 (6.2) | 30 (13.7) | 14 (6.8) | 6 (2.9) | 4 (8.2) | 31 (12.4) |
| p = 0.005 | p = 0.28 | p = 0.01 | p = 0.40 | |||||
| Income (US$/Month) | ||||||||
| < 2,000 | 12 (6.6) | 9 (5.1) | 4 (5) | 14 (6.9) | 11 (6.1) | 10 (5.6) | 2 (4.1) | 16 (6.8) |
| 2,000-3,000 | 8 (4.4) | 10 (5.6) | 5 (6.3) | 12 (5.9) | 7 (3.9) | 11 (6.2) | 2 (4.1) | 15 (6.4) |
| ≥ 3,000 | 162 (89) | 159 (89.3) | 71 (88.8) | 178 (87.3) | 163 (90.1) | 158 (88.3) | 45 (91.8) | 204 (86.8) |
| p = 0.73 | p = 0.63 | p = 0.81 | p = 0.35 | |||||
| Smoking | ||||||||
| Non-smoker | 207 (97.6) | 189 (95) | 25 (30.9) | 61 (27.9) | 202 (97.6) | 194 (95.1) | 15 (30.6) | 71 (28.3) |
| Smoker | 5 (2.4) | 10 (5) | 56 (69.1) | 158 (72.2) | 5 (2.4) | 10 (4.9) | 34 (69.4) | 180 (71.7) |
| p = 0.24 | p = 0.71 | p = 0.28 | p = 0.88 | |||||
| Alcohol consumption | ||||||||
| Non-drinking | 151 (71.2) | 133 (66.8) | 14 (17.3) | 40 (18.3) | 146 (70.5) | 138 (67.7) | 10 (20.4) | 44 (17.5) |
| Drinking | 61 (28.8) | 66 (33.2) | 67 (82.7) | 179 (81.7) | 61 (29.5) | 66 (32.4) | 39 (79.6) | 207 (82.5) |
| p = 0.39 | p = 0.98 | p = 0.60 | p = 0.78 | |||||
| Working hours | ||||||||
| < 9 h/day | 193 (93.7) | 169 (86.7) | 47 (58.8) | 146 (67.6) | 189 (93.6) | 173 (86.9) | 29 (60.4) | 164 (66.1) |
| ≥ 9 h/day | 13 (6.3) | 26 (13.3) | 33 (41.3) | 70 (32.4) | 13 (6.4) | 26 (13.1) | 19 (39.6) | 84 (33.9) |
| p = 0.03 | p = 0.20 | p = 0.04 | p = 0.55 | |||||
| Occupational sitting time | ||||||||
| < 4 h/day | 152 (71.7) | 132 (66.3) | 28 (34.6) | 74 (33.8) | 149 (72) | 135 (66.2) | 14 (28.6) | 88 (35.1) |
| ≥ 4 h/day | 60 (28.3) | 67 (33.7) | 53 (65.4) | 145 (66.2) | 58 (28) | 69 (33.8) | 35 (71.4) | 163 (64.9) |
| p = 0.28 | p = 1.00 | p = 0.24 | p = 0.48 | |||||
| Regular exercise | ||||||||
| No | 89 (42.4) | 73 (36.9) | 34 (42.5) | 84 (38.7) | 79 (38.5) | 83 (40.9) | 19 (38.8) | 99 (39.9) |
| Yes | 121 (57.6) | 125 (63.1) | 46 (57.5) | 133 (61.3) | 126 (61.5) | 120 (59.1) | 30 (61.2) | 149 (60.1) |
| p = 0.30 | p = 0.65 | p = 0.70 | p = 1.00 | |||||
| Sleeping hours | ||||||||
| > 9 h/day | 135 (65.5) | 146 (75.7) | 59 (72.8) | 157 (72) | 132 (65.4) | 149 (75.6) | 35 (71.4) | 181 (72.4) |
| ≤ 9 h/day | 71 (34.5) | 47 (24.4) | 22 (27.2) | 61 (28) | 70 (34.7) | 48 (24.4) | 14 (28.6) | 69 (27.6) |
| p = 0.04 | p = 1.00 | p = 0.03 | p = 1.00 | |||||
| BMI (kg/m2) | PBF (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Women | Men | Women | Men | |||||
| Variable | Crude OR | Adjusted OR* | Crude OR | Adjusted OR* | Crude OR | Adjusted OR* | Crude OR | Adjusted OR* |
| (95 % CI) | (95 % CI) | (95 % CI) | (95 % CI) | (95 % CI) | (95 % CI) | (95 % CI) | (95 % CI) | |
| Socio-demographic factors | ||||||||
| Age group | ||||||||
| 40–49 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 50–59 | 1.54 | 1.47 | 0.82 | 0.66 | 1.81 | 1.96 | 1.19 | 1.41 |
| (1.01–2.33) | (0.89–2.42) | (0.47–1.45) | (0.34–1.28) | (1.19–2.76) | (1.18–3.24) | (0.61–2.34) | (0.66–3.02) | |
| 60+ | 2.05 | 2.49 | 0.64 | 0.48 | 6.56 | 7.37 | 1.26 | 1.65 |
| (1.05–4.00) | (1.16–5.33) | (0.31–1.30) | (0.21–1.11) | (2.91–14.81) | (3.06–17.76) | (0.51–3.14) | (0.57–4.76) | |
| Marital status | ||||||||
| Unmarried | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Married | 0.92 | 0.74 | 1.65 | 1.65 | 0.96 | 1.41 | 0.74 | 0.94 |
| (0.26–3.24) | (0.17–3.18) | (0.38–7.06) | (0.35–7.71) | (0.27–3.38) | (0.30–6.65) | (0.09–6.13) | (0.11–8.35) | |
| Divorced, Widow/Widower | 1.18 | 0.51 | 1.4 | 0.83 | 1.4 | 0.75 | 0.33 | 0.14 |
| (0.27–5.18) | (0.09–2.89) | (0.20–10.03) | (0.09–7.49) | (0.32–6.16) | (0.12–4.7) | (0.03–4.04) | (0.01–2.09) | |
| Educational level | ||||||||
| Low | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Middle | 0.59 | 0.72 | 0.93 | 0.87 | 0.67 | 0.87 | 1.12 | 1.29 |
| (0.40–0.88) | (0.45–1.16) | (0.55–1.58) | (0.48–1.59) | (0.45–1.00) | (0.54–1.41) | (0.59–2.14) | (0.64–2.61) | |
| High | 0.43 | 0.20 | 2.32 | 2.60 | 0.34 | 0.21 | 1.68 | 1.80 |
| (0.17–1.13) | (0.05–0.78) | (0.84–6.45) | (0.81–8.36) | (0.13–0.93) | (0.05–0.85) | (0.54–5.23) | (0.54–6.02) | |
| Income (US$/Month) | ||||||||
| < 2,000 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 2,000–3,000 | 1.67 | 1.72 | 0.69 | 0.42 | 1.73 | 1.63 | 0.94 | 0.99 |
| (0.47–5.93) | (0.41–7.31) | (0.15–3.15) | (0.08–2.33) | (0.48–6.2) | (0.37–7.20) | (0.12–7.52) | (0.11–9.07) | |
| ≥ 3,000 | 1.31 | 1.29 | 0.72 | 0.40 | 1.07 | 0.82 | 0.57 | 0.41 |
| (0.54–3.19) | (0.48–3.48) | (0.23–2.25) | (0.10–1.57) | (0.44–2.58) | (0.30–2.24) | (0.13–2.55) | (0.08–2.03) | |
| Lifestyle factors | ||||||||
| Smoking | ||||||||
| Non-smoker | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Smoker | 2.19 | 1.87 | 1.16 | 1.47 | 2.08 | 1.86 | 1.12 | 1.25 |
| (0.74–6.52) | (0.55–6.39) | (0.66–2.02) | (0.77–2.81) | (0.70–6.20) | (0.54–6.43) | (0.57–2.18) | (0.58–2.67) | |
| Alcohol consumption | ||||||||
| Non-drinking | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Drinking | 1.23 | 1.39 | 0.94 | 0.91 | 1.15 | 1.44 | 1.21 | 1.70 |
| (0.81–1.87) | (0.85–2.25) | (0.48–1.83) | (0.43–1.96) | (0.75–1.74) | (0.88–2.37) | (0.56–2.60) | (0.73–3.93) | |
| Working hours | ||||||||
| < 9 h/day | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| ≥ 9 h/day | 2.28 | 2.42 | 0.68 | 0.46 | 2.19 | 2.50 | 0.78 | 0.63 |
| (1.14–4.59) | (1.05–5.57) | (0.40–1.16) | (0.24–0.87) | (1.09–4.39) | (1.07–5.79) | (0.41–1.48) | (0.30–1.32) | |
| Occupational sitting time | ||||||||
| < 4 h/day | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| ≥ 4 h/day | 1.29 | 0.96 | 1.04 | 1.16 | 1.26 | 0.98 | 0.85 | 0.91 |
| (0.85–1.96) | (0.53–1.76) | (0.61–1.77) | (0.63–2.12) | (0.78–2.06) | (0.53–1.83) | (0.46–1.57) | (0.45–1.85) | |
| Regular exercise | ||||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 1.26 | 1.04 | 1.17 | 1.31 | 0.91 | 0.81 | 0.95 | 0.89 |
| (0.85–1.88) | (0.65–1.66) | (0.70–1.97) | (0.74–2.33) | (0.61–1.35) | (0.5–1.32) | (0.51–1.79) | (0.46–1.74) | |
| Sleeping hours | ||||||||
| > 9 h/day | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| ≤ 9 h/day | 0.61 | 0.66 | 1.04 | 1.05 | 0.61 | 0.65 | 0.95 | 0.79 |
| (0.40–0.95) | (0.40–1.09) | (0.59–1.85) | (0.56–1.99) | (0.39–0.94) | (0.39–1.10) | (0.48–1.88) | (0.39–1.63) | |
| Category | N (%) | Odds ratios (95 % Confidence Intervals) | |||
|---|---|---|---|---|---|
| BMI | PBF | ||||
| Crude | Adjusted* | Crude | Adjusted* | ||
| Group1 (Age < 50 and working hours < 9) | 263 (37.73) | 1 | 1 | 1 | 1 |
| Group2 (Age ≥ 50 and working hours < 9) | 292 (41.89) | 1.69(1.11–2.56) | 1.68(1.04–2.73) | 2.66(1.67–3.91) | 2.87(1.75–4.69) |
| Group3 (Age < 50 and working hours ≥ 9) | 87 (12.48) | 2.39(0.94–6.03) | 2.34(0.77–7.11) | 2.60(1.32–8.90) | 2.73(1.19–12.06) |
| Group4 (Age ≥ 50 and working hours ≥ 9) | 55 (7.89) | 3.82(1.31–11.14) | 3.56(1.03–12.37) | 3.43(1.23–9.54) | 3.90(1.05–11.00) |
*Values are Mean ± SD
+Abbreviations. BMI: Body mass index (Cut-off limits of overweight: 23 ≤ BMI (kg/m2) < 25, Cut-off limits of obesity: BMI (kg/m2) ≥25), PBF: Percent body fat (Cut-off limits of overweight: 20 = <PBF (%) < 25 in men and 30 ≤ PBF (%) < 35 in women, Cut-off limits of obesity: men’s PBF (%) ≥ 25; women’s PBF (%) ≥ 35)
aDifferences between sexes: *
*Controls. BMI: Body mass index (Cut-off limits of overweight: BMI (kg/m2) <25, PBF: Percent body fat (Cut-off limits of overweight: men’s BF (%) < 20; women’s BF (%) < 30)
+Cases. BMI: Body mass index (Cut-off limits of overweight: BMI (kg/m2) ≥25, PBF: Percent body fat (Cut-off limits of overweight: men’s BF (%) ≥ 20; women’s BF (%) ≥ 3
Working hours, occupational sitting time and Sleeping time were dichotomized at the median
*Adjusted for confounding factors except for the targeted variable itself. The confounding factors involve age, educational level, smoking, alcohol consumption, working hours, daily occupational sitting time, and sleeping hours (h/day)
*Adjusted for confounding factors except for the targeted variable itself. The confounding factors involve age, educational level, smoking, alcohol consumption, working hours, daily occupational sitting time, and sleeping hours (h/day). Working hours and age group were dichotomized at the median
 KSOEM
KSOEM

 Cite
Cite

