Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 26; 2014 > Article
- Research Article Co morbidities of Myofascial Neck Pain among Information Technology Professionals
- Mathankumar Mohandoss1, Deepak Sharan2, Rameshkumar Ranganathan1, Jeena Jose1
-
Annals of Occupational and Environmental Medicine 2014;26:21.
DOI: https://doi.org/10.1186/s40557-014-0021-4
Published online: September 3, 2014
1Department of Physiotherapy, RECOUP Neuromusculoskeletal Rehabilitation Centre, # 312, 10th Block, Further Extension of Anjanapura Layout, Bangalore 560062, Karnataka, India
2Department of Orthopedic Surgery and Rehabilitation, RECOUP Neuromusculoskeletal Rehabilitation Centre, # 312, 10th Block, Further Extension of Anjanapura Layout, Bangalore 560062, Karnataka, India
Copyright © 2014 Mohandoss et al.; licensee BioMed Central
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Abstract
-
Objectives The objective of this study was to identify the musculoskeletal co-morbidities of neck pain of myofascial origin among IT professionals.
-
Methods A retrospective report analysis of 5357 IT professionals from various IT companies in India was conducted. Demographic details, type and intensity of the musculoskeletal problems, employee feedbacks on status of musculoskeletal health and physician’s diagnosis were analysed. Descriptive statistics were used to describe the age, gender, body area affected and nature of work. Chi square test was used to find the association between musculoskeletal co-morbidities and myofascial neck pain (MNP).
-
Results The study participants were predominantly males (71%). 41% of the population used laptops, 35% desktops and 24% both. Neck pain was the commonest reported symptom, followed by low back, shoulder and arm pain respectively. Statistical analysis also revealed that low back pain and shoulder pain, had a significant association with neck pain. Further analysis revealed that there was a significant association between the presence of MNP and thoracic outlet syndrome (p < 0.001) and fibromyalgia syndrome (p < 0.001). Other than the listed co-morbidities, eye strain was also found to be associated with MNP.
-
Conclusions Low back pain and shoulder pain was found to be co morbid symptoms noted among IT professionals with MNP. Thoracic outlet syndrome and fibromyalgia were found to be the most commonly associated disorders with MNP among IT professionals.
Introduction
Materials and Methods
Results
Discussion
Competing interests
Authors’ contributions
Acknowledgements
- Sharan D, Parijat P, Sasidharan AP, Ranganathan R, Mohandoss M, Jose J: Workstyle risk factors for work related musculoskeletal symptoms among computer professionals in India. J Occup Rehabil 2011;21(4):520–525. 10.1007/s10926-011-9294-4. 21328059.ArticlePubMedPDF
- Sharan D, Ajeesh PS, Rameshkumar R, Jose J: Risk factors, clinical features and outcome of treatment of work related musculoskeletal disorders in on-site clinics among IT companies in India. Work 2012;41(Suppl 1):5702–5704. 22317658.ArticlePubMed
- Picavet HS, Schouten JS: Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC (3)-study. Pain 2003;102:167–178. 10.1016/s0304-3959(02)00372-x. 12620608.ArticlePubMed
- Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, Van-den BGAM: Causes and consequences of co-morbidity: a review. J Clin Epidemiol 2001;54(7):661–674. 10.1016/S0895-4356(00)00363-2. 11438406.PubMed
- TRS 919. 2003, World Health Organization, Geneva, Switzerland.
- Croft PR, Lewis M, Papageorgiou AC, Thomas E, Jayson MI, Macfarlane GJ, Silman AJ: Risk factors for neck pain: a longitudinal study in the general population. Pain 2001;93(3):317–325. 10.1016/S0304-3959(01)00334-7. 11514090.ArticlePubMed
- Carroll LJ, Hogg-Johnson S, Côté P, van der Velde G, Holm LW, Carragee EJ, Hurwitz EL, Peloso PM, Cassidy JD, Guzman J, Nordin M, Haldeman S: Course and prognostic factors for neck pain in workers: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;33(Suppl 4):S93–S100. 10.1097/BRS.0b013e31816445d4. 18204406.ArticlePubMed
- McLean SM, May S, Moffett J, Sharp DM, Gardiner E: Prognostic factors for progressive non-specific neck pain: a systematic review.Phys Ther Rev 2007, 12(3):220..
- Walton DM, Carroll LJ, Kasch H, Sterling M, Verhagen AP, Macdermid JC, Gross A, Santaguida PL, Carlesso L: An overview of systematic reviews on prognostic factors in neck pain: results from the international collabration on neck pain. Open Orthop J 2013;7:494–505. 10.2174/1874325001307010494. 24115971.PubMedPMC
- Simons DG: Diagnostic criteria of myofascial pain due to trigger points. J Musculoskelet Pain 1999;7(1/2):111–120. 10.1300/J094v07n01_11.
- Alexopoulos EC, Stathi IC, Charizani F: Prevalence of musculoskeletal disorders in dentists.BMC Musculoskelet Disord 2004, 5:16..
- Alexopoulos EC, Tanagra D, Konstantinou E, Burdorf A: Musculoskeletal disorders in shipyard industry: prevalence, healthcare use, and absenteeism.BMC Musculoskelet Disord 2006, 7:88..
- IJzelenberg W, Burdorf A: Impact of musculoskeletal co-morbidity of neck and upper extremities on healthcare utilization and sickness absence for low back pain. Occup Environ Med 2004;61:806–810. 10.1136/oem.2003.011635. 15377765.ArticlePubMedPMC
- Haukka E, Arjas PL, Solovieva S, Ranta R, Viikari-Juntura E, Riihimäki H: Co-occurrence of musculoskeletal pain among female kitchen workers. Int Arch Occup Environ Health 2006;80(2):141–148. 10.1007/s00420-006-0113-8. 16688464.ArticlePubMedPDF
- Hill J, Lewis M, Papageorgiou AC: Predicting persistent neck pain: A 1-year follow-up of a population cohort. Spine 2004;29:1648–1654. 10.1097/01.BRS.0000132307.06321.3C. 15284511.ArticlePubMed
- Hoving JL, De Vet HCW, Twisk JWR: Prognostic factors for neck pain in general practice. Pain 2004;110:639–645. 10.1016/j.pain.2004.05.002. 15288404.ArticlePubMed
- Jordan SE, Ahn SS, Gelabert HA: Differentiation of thoracic outlet syndrome from treatment-resistant cervical brachial pain syndromes: development and utilization of a questionnaire, clinical examination and ultrasound evaluation. Pain Physician 2007;10(3):441–452. 17525778.ArticlePubMed
- Cakit BD, Taskin S, Nacir B, Unlu I, Genc H, Erdem HR: Co-morbidity of fibromyalgia and cervical myofascial pain syndrome. Clin Rheumatol 2010;29(4):405–411. 10.1007/s10067-009-1342-5. 20066449.ArticlePubMedPDF
- Scott KM, Korff MV, Alonso J, Angermeyer MC, Bromet E, Fayyad J, de Girolamo G, Demyttenaere K, Gasquet I, Gureje O, Haro JM, He Y, Kessler RC, Levinson D, Mora MEM, Browne MO, Ormel J, Villa JP, Watanabe M, Williams D: Mental-Physical Co-morbidity and its relationship with disability: results from the world mental health surveys. Psychol Med 2009;39(1):33–43. 10.1017/S0033291708003188. 18366819.ArticlePubMedPMC
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Effects of repeated cervical active range of motion with overpressure on fascial displacement of the upper trapezius muscle among individuals with and without myofascial pain syndrome: A case-control study
Valentin C. Dones, Chrizelle Joy Del Rosario, Andrea Janelle Co, Sean Jerimiah Agbayani, Patricia Denise Cabrera, Edrin Isabel Dellosa, Daniel Rey Ibo, Ivy Sophia Pagente, Angelika Camille Sua, Clarence Pryce Joshua Almazan, Marie Arallu Capistrano, Kimbe
Journal of Bodywork and Movement Therapies.2025; 42: 955. CrossRef - Common pain sites, prevalence and predictors of work-related musculoskeletal pain among Indian information technology professionals: a systematic review and meta-analysis
Janmejaya Samal, Hari Singh
Discover Public Health.2025;[Epub] CrossRef - Mapping Research on Ageism, Personal and Social Well-Being in IT Professionals: A Literature Review and Bibliometric Analysis
Rinku Mahindru, Hersheen Kaur, Renu Gupta
Acta Universitatis Bohemiae Meridionalis.2023; 26(2): 18. CrossRef
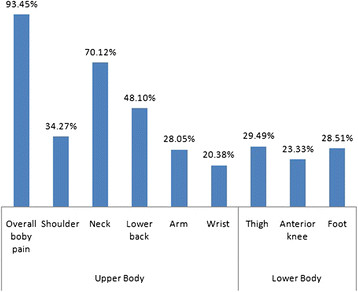
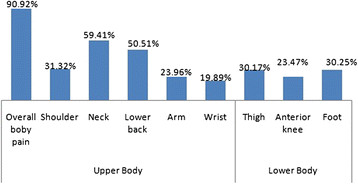
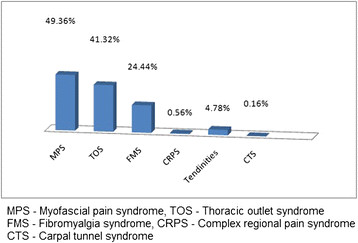
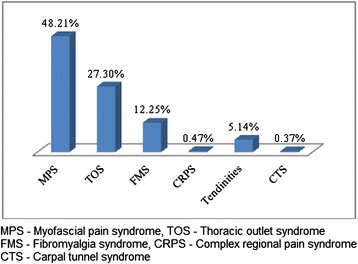
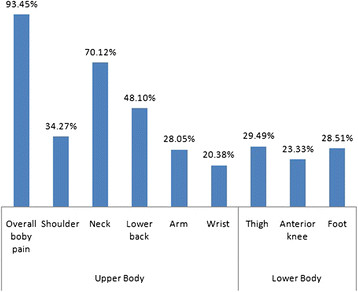
Figure 1
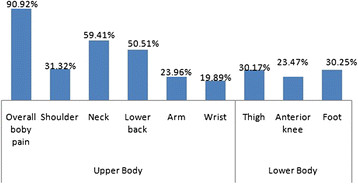
Figure 2
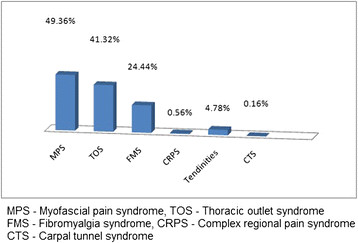
Figure 3
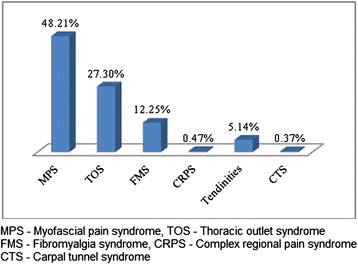
Figure 4
| Variables | n | % |
|---|---|---|
| Gender | ||
| Male | 3831 | 71.5 |
| Female | 1526 | 28.5 |
| Age group | ||
| <25 Years | 569 | 10.6 |
| 25 to 35 | 3822 | 71.3 |
| 36 to 45 | 840 | 15.7 |
| 46 to 55 | 117 | 2.2 |
| >56 years | 9 | 0.2 |
| Hours of computer work/day | ||
| < 8 hours | 489 | 9 |
| 8 to 12 hours | 4371 | 81.6 |
| >12 hours | 497 | 9.4 |
| Job category | ||
| Managerial | 1500 | 28 |
| Software Engineer | 1446 | 27 |
| Application Engineer | 1179 | 22 |
| Analyst | 804 | 15 |
| Human Resource | 161 | 3 |
| Others | 267 | 5 |
| Type of computer used | ||
| Desktop | 1872 | 35 |
| Laptop | 2187 | 41 |
| Both | 1298 | 24 |
| Variable | Co-morbid symptom | Co-morbid disorder | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Low back pain | Shoulder pain | Forearm & wrist pain | TOS ф | FMS Ὼ | ||||||
| n (%) | p-value* | n (%) | p-value* | n (%) | p-value* | n (%) | p-value* | n (%) | p-value* | |
| Gender | ||||||||||
| Male (n = 2276) | 1064 (47) | 0.75 | 921 (41) | 0.47 | 553 (24) | 0.34 | 913 (40) | 0.005# | 378 (17) | 1.7E-05# |
| Female (n = 1070) | 494 (46) | 447 (42) | 244 (23) | 484 (45) | 244 (23) | |||||
| Age group | ||||||||||
| <25 years (n = 362) | 184 (51) | 0.004# | 156 (43) | 0.6 | 65 (17) | 0.005# | 104 (28) | 0.00# | 50 (13) | 0.014 |
| 25 to 35 (n = 2398) | 1126 (47) | 975 (41) | 564 (24) | 1013 (42) | 440 (18) | |||||
| 36 to 45 (n = 526) | 218 (41) | 204 (38) | 145 (27) | 236 (44) | 119 (22) | |||||
| 46 to 55 (n = 55) | 16 (29) | 24 (44) | 16 (29) | 28 (51) | 7 (13) | |||||
| >56 years (n = 5) | 2 (40) | 1(20) | 3 (60) | 3 (60) | 1 (20) | |||||
| Computer work/day | ||||||||||
| < 8 hours (n = 310) | 61(20) | 0.00# | 134 (43) | 0.00# | 29 (9.4) | 0.00# | 52 (17) | 0.00# | 18 (6) | 0.00# |
| 8 to 12 hours (n = 2726) | 1262 (46) | 1105 (41) | 658 (24) | 1206 (43) | 533 (19) | |||||
| >12 hours (n = 310) | 204 (66) | 186 (60) | 73 (25) | 90 (29) | 31(10) | |||||
| Computer used | ||||||||||
| Desktop (n = 1170) | 677(58) | 0.00# | 625 (53) | 0.00# | 255 (22) | 0.1 | 353(30) | 0.00# | 107 (10) | 0.00# |
| Laptop (n = 1396) | 629 (45) | 589 (42) | 342 (25) | 596 (43) | 282 (20) | |||||
| Both (n = 780) | 252 (32) | 154 (20) | 200 (26) | 448 (57) | 233 (30) | |||||
ф- Thoracic outlet syndrome.
Ὼ- Fibromyalgia syndrome.
*- Calculated using the Chi square test.
#- Variables with significant association.
 KSOEM
KSOEM

 Cite
Cite

