Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 36; 2024 > Article
- Original Article The impact of long working hours on daily sodium intake
-
Kyungho Ju1,2
 , Yangwoo Kim2,3
, Yangwoo Kim2,3 , Seung Hee Woo1,2
, Seung Hee Woo1,2 , Juhyeong Kim1,2
, Juhyeong Kim1,2 , Inah Kim1,2
, Inah Kim1,2 , Jaechul Song1,2
, Jaechul Song1,2 , Soo-Jin Lee1,2
, Soo-Jin Lee1,2 , Jeehee Min1,2
, Jeehee Min1,2
-
Annals of Occupational and Environmental Medicine 2024;36:e9.
DOI: https://doi.org/10.35371/aoem.2024.36.e9
Published online: April 1, 2024
1Department of Occupational and Environmental Medicine, Hanyang University Hospital, Seoul, Korea.
2Department of Occupational and Environmental Medicine, Hanyang University College of Medicine, Seoul, Korea.
3Department of Occupational and Environmental Medicine, Hanyang University Guri Hospital, Guri, Korea.
- Correspondence: Jeehee Min. Department of Occupational and Environmental Medicine, Hanyang University Hospital, 222-1 Wangsimni-ro, Seongdong-gu, Seoul 04763, Korea. jhmin.oem@gmail.com
Copyright © 2024 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background Long working hours are associated with an increased risk of cardiovascular disease, yet the underlying mechanism(s) remain unclear. The study examines how occupational factors like working hours, shift work, and employment status correlate with dietary choices and sodium intake, impacting hypertension risk.
-
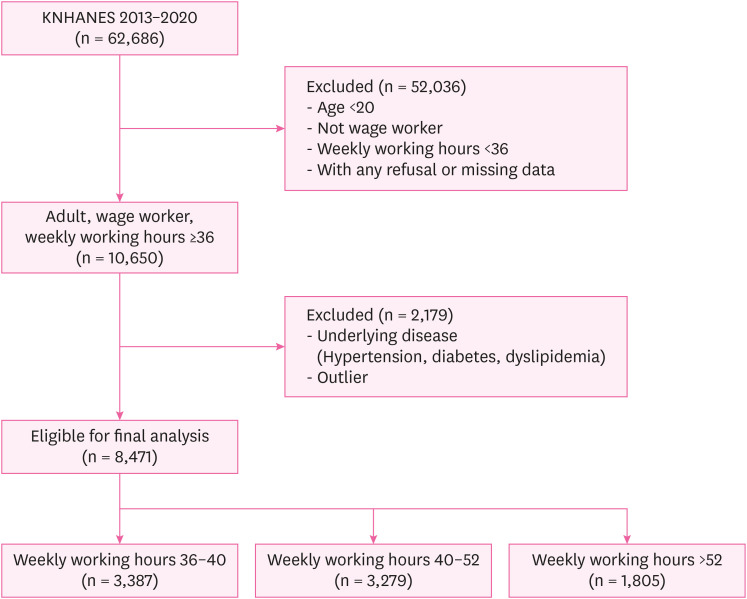
Methods This study used data from the Korea National Health and Nutrition Examination Survey conducted between 2013 and 2020. The dataset included 8,471 respondents, all of whom were wage workers aged 20 or older and reported working at least 36 hours per week. Individuals who have been previously diagnosed with or are currently diagnosed with hypertension, diabetes, or dyslipidemia were excluded. The average daily sodium intake was assessed via a 24-hour dietary recall method. Average weekly working hours were categorized into 3 groups: 36–40 hours, 41–52 hours, and over 52 hours. Multiple logistic regression models were used.
-
Results Study findings revealed that 83.7% of participants exceeded the recommended daily sodium intake of 2 g set by the World Health Organization. After adjusting for confounding factors, a positive correlation was observed between average working hours and daily sodium intake. Among males, statistical significance was found in the group with average weekly working hours of 41–52 hours (prevalence ratio [PR]: 1.17; 95% confidence interval [CI]: 1.05–1.30) and the group exceeding 52 hours (PR: 1.22; 95% CI: 1.09–1.38) when comparing the fourth quartile of daily sodium intake to the combined quartiles of Q1, Q2, and Q3. Among females, no significance was noted.
-
Conclusions Long working hours were associated with increased sodium intake, primarily among male workers. This connection is likely attributed to having less time for home-cooked meals, resulting in higher fast food consumption and dining out. A workplace intervention promoting healthy eating and reducing stress is essential to lower sodium consumption and mitigate hypertension risk.
BACKGROUND
METHODS
RESULTS
Demographic characteristics of the study participants
Sodium intake and blood pressure according to working hours per week
Adjusted prevalence ratios of daily sodium intake quartiles associated with weekly working hours
Adjusted prevalence ratios of Q1 + Q2 + Q3 and Q4 of daily sodium intake
DISCUSSION
CONCLUSIONS
Acknowledgements
Abbreviations
BMI
CI
KNHANES
OECD
PR
SD
WHO
-
Competing interests: The authors declare that they have no competing interests.
-
Authors contributions:
Conceptualization: Ju K, Min J.
Data curation: Ju K, Kim J.
Formal analysis: Ju K, Woo SH, Kim J.
Investigation: Min J.
Methodology: Kim Y, Kim I.
Software: Woo SH.
Validation: Kim Y.
Visualization: Song J, Lee SJ.
Writing - original draft: Ju K.
Writing - review & editing: Ju K, Min J, Kim I, Song J, Lee SJ.
NOTES
- 1. Organization for Economic Cooperation and Development (OECD). Average Annual Hours Actually Worked per Worker. Paris, France: OECD; 2021.
- 2. National Assembly Budget Office (KR). Economic Trends. Seoul, Korea: National Assembly Budget Office; 2023.
- 3. World Health Organization (WHO). Long Working Hours Increasing Deaths From Heart Disease and Stroke: WHO, ILO. Geneva, Switzerland: WHO; 2021.
- 4. Li J, Pega F, Ujita Y, Brisson C, Clays E, Descatha A, et al. The effect of exposure to long working hours on ischaemic heart disease: a systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ Int 2020;142:105739. 32505014.ArticlePubMedPMC
- 5. Descatha A, Sembajwe G, Pega F, Ujita Y, Baer M, Boccuni F, et al. The effect of exposure to long working hours on stroke: a systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ Int 2020;142:105746. 32505015.ArticlePubMed
- 6. Trudel X, Brisson C, Gilbert-Ouimet M, Vézina M, Talbot D, Milot A. Long working hours and the prevalence of masked and sustained hypertension. Hypertension 2020;75(2):532–538. 31852264.ArticlePubMed
- 7. Seo E, Lee Y, Mun E, Kim DH, Jeong Y, Lee J, et al. The effect of long working hours on developing type 2 diabetes in adults with prediabetes: the Kangbuk Samsung Cohort Study. Ann Occup Environ Med 2022;34(1):e4. 35425614.ArticlePubMedPMCPDF
- 8. Kivimäki M, Nyberg ST, Batty GD, Kawachi I, Jokela M, Alfredsson L, et al. Long working hours as a risk factor for atrial fibrillation: a multi-cohort study. Eur Heart J 2017;38(34):2621–2628. 28911189.PubMedPMC
- 9. Charles LE, Fekedulegn D, Landsbergis P, Burchfiel CM, Baron S, Kaufman JD, et al. Associations of work hours, job strain, and occupation with endothelial function: the Multi-Ethnic Study of Atherosclerosis (MESA). J Occup Environ Med 2014;56(11):1153–1160. 25376409.PubMedPMC
- 10. Virtanen M, Kivimäki M. Long working hours and risk of cardiovascular disease. Curr Cardiol Rep 2018;20(11):123. 30276493.ArticlePubMedPMCPDF
- 11. Park S, Kook H, Seok H, Lee JH, Lim D, Cho DH, et al. The negative impact of long working hours on mental health in young Korean workers. PLoS One 2020;15(8):e0236931. 32750080.ArticlePubMedPMC
- 12. Leung SL, Barber JA, Burger A, Barnes RD. Factors associated with healthy and unhealthy workplace eating behaviours in individuals with overweight/obesity with and without binge eating disorder. Obes Sci Pract 2018;4(2):109–118. 29670748.ArticlePubMedPMCPDF
- 13. Bauer KW, Hearst MO, Escoto K, Berge JM, Neumark-Sztainer D. Parental employment and work-family stress: associations with family food environments. Soc Sci Med 2012;75(3):496–504. 22591825.ArticlePubMedPMC
- 14. Souza RV, Sarmento RA, de Almeida JC, Canuto R. The effect of shift work on eating habits: a systematic review. Scand J Work Environ Health 2019;45(1):7–21. 30088659.ArticlePubMed
- 15. Bucher Della Torre S, Wild P, Dorribo V, Danuser B, Amati F. Energy, nutrient and food intakes of male shift workers vary according to the schedule type but not the number of nights worked. Nutrients 2020;12(4):919. 32230756.PubMedPMC
- 16. Wardle J, Steptoe A, Oliver G, Lipsey Z. Stress, dietary restraint and food intake. J Psychosom Res 2000;48(2):195–202. 10719137.ArticlePubMed
- 17. Min J, Lee DW, Kang MY, Myong JP, Kim HR, Lee J. Working for long hours is associated with dietary fiber insufficiency. Front Nutr 2022;9:786569. 35252290.ArticlePubMedPMC
- 18. Lee W, Jung J, Ahn J, Kim HR. Rate of inappropriate energy and micronutrient intake among the Korean working population. Public Health Nutr 2020;23(18):3356–3367. 32183914.ArticlePubMedPMC
- 19. Kivimäki M, Jokela M, Nyberg ST, Singh-Manoux A, Fransson EI, Alfredsson L, et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet 2015;386(10005):1739–1746. 26298822.ArticlePubMed
- 20. Soek H, Won JU, Lee TI, Kim YK, Lee W, Lee JH, et al. A dose-response relationship between long working hours and unmet need for access to hospital facilities. Scand J Work Environ Health 2016;42(2):135–143. 26862879.ArticlePubMed
- 21. Filippou CD, Tsioufis CP, Thomopoulos CG, Mihas CC, Dimitriadis KS, Sotiropoulou LI, et al. Dietary approaches to stop hypertension (DASH) diet and blood pressure reduction in adults with and without hypertension: a systematic review and meta-analysis of randomized controlled trials. Adv Nutr 2020;11(5):1150–1160. 32330233.ArticlePubMedPMCPDF
- 22. Lee DW, Lee J, Kim HR, Jun KY, Kang MY. Long work hours and decreased glomerular filtration rate in the Korean working population. Occup Environ Med 2020;77(10):699–705. 32576647.ArticlePubMed
- 23. Strazzullo P, Leclercq C. Sodium. Adv Nutr 2014;5(2):188–190. 24618759.ArticlePubMedPMC
- 24. Alderman MH, Cohen H, Madhavan S. Dietary sodium intake and mortality: the National Health and Nutrition Examination Survey (NHANES I). Lancet 1998;351(9105):781–785. 9519949.ArticlePubMed
- 25. Ruiz AMP, Lima MG, Medina LPB, Pinto RL, Barros MBA, Filho AAB. Can meals outside homes impact sodium intake? Curr Dev Nutr 2020;4(6):nzaa091. 32582874.ArticlePubMedPMCPDF
- 26. Coutinho LM, Scazufca M, Menezes PR. Methods for estimating prevalence ratios in cross-sectional studies. Rev Saude Publica 2008;42(6):992–998. 19009156.PubMed
- 27. Monsivais P, Aggarwal A, Drewnowski A. Time spent on home food preparation and indicators of healthy eating. Am J Prev Med 2014;47(6):796–802. 25245799.ArticlePubMedPMC
- 28. Nagler EM, Viswanath K, Ebbeling CB, Stoddard AM, Sorensen G. Correlates of fruit and vegetable consumption among construction laborers and motor freight workers. Cancer Causes Control 2013;24(4):637–647. 22729935.ArticlePubMedPMCPDF
- 29. Barrington WE, Ceballos RM, Bishop SK, McGregor BA, Beresford SA. Perceived stress, behavior, and body mass index among adults participating in a worksite obesity prevention program, Seattle, 2005-2007. Prev Chronic Dis 2012;9:E152. 23036611.ArticlePubMedPMC
- 30. Järvelä-Reijonen E, Karhunen L, Sairanen E, Rantala S, Laitinen J, Puttonen S, et al. High perceived stress is associated with unfavorable eating behavior in overweight and obese Finns of working age. Appetite 2016;103:249–258. 27108837.ArticlePubMed
- 31. Cho C, Nam Y, Yoo HJ. Evaluation of nutritional quality of convenience store meal boxes according to store company and meal price. Korean J Community Nutr 2022;27(2):105–120.ArticlePDF
- 32. Wong K, Chan AH, Ngan SC. The effect of long working hours and overtime on occupational health: a meta-analysis of evidence from 1998 to 2018. Int J Environ Res Public Health 2019;16(12):2102. 31200573.ArticlePubMedPMC
- 33. Iwasaki K, Sasaki T, Oka T, Hisanaga N. Effect of working hours on biological functions related to cardiovascular system among salesmen in a machinery manufacturing company. Ind Health 1998;36(4):361–367. 9810150.ArticlePubMed
- 34. Nakanishi N, Yoshida H, Nagano K, Kawashimo H, Nakamura K, Tatara K. Long working hours and risk for hypertension in Japanese male white collar workers. J Epidemiol Community Health 2001;55(5):316–322. 11297649.ArticlePubMedPMC
- 35. Pimenta AM, Beunza JJ, Bes-Rastrollo M, Alonso A, López CN, Velásquez-Meléndez G, et al. Work hours and incidence of hypertension among Spanish university graduates: the Seguimiento Universidad de Navarra prospective cohort. J Hypertens 2009;27(1):34–40. 19050449.ArticlePubMed
- 36. Kang MY, Park H, Seo JC, Kim D, Lim YH, Lim S, et al. Long working hours and cardiovascular disease: a meta-analysis of epidemiologic studies. J Occup Environ Med 2012;54(5):532–537. 22576460.PubMed
- 37. Kivimäki M, Leino-Arjas P, Kaila-Kangas L, Luukkonen R, Vahtera J, Elovainio M, et al. Is incomplete recovery from work a risk marker of cardiovascular death? Prospective evidence from industrial employees. Psychosom Med 2006;68(3):402–407. 16738071.ArticlePubMed
- 38. van Diest R, Appels A. Vital exhaustion and perception of sleep. J Psychosom Res 1992;36(5):449–458. 1619584.ArticlePubMed
- 39. Chen JD, Cheng TJ, Lin YC, Hsiao ST. Job categories and acute ischemic heart disease: a hospital-based, case-control study in Taiwan. Am J Ind Med 2007;50(6):409–414. 17450543.ArticlePubMed
- 40. Rosenman RH, Friedman M, Straus R, Wurm M, Kositchek R, Hahn W, et al. A predictive study of coronary heart disease. JAMA 1964;189(1):15–22. 14149016.ArticlePubMed
- 41. Karasek RA. Job demands, job decision latitude, and mental strain: implications for job redesign. Adm Sci Q 1979;24(2):285–308.Article
- 42. Kwon MJ. Occupational health inequalities by issues on gender and social class in labor market: absenteeism and presenteeism across 26 OECD countries. Front Public Health 2020;8:84. 32269984.ArticlePubMedPMC
- 43. Shim JS, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health 2014;36:e2014009. 25078382.ArticlePubMedPMC
- 44. Black AE. Critical evaluation of energy intake using the Goldberg cut-off for energy intake:basal metabolic rate. A practical guide to its calculation, use and limitations. Int J Obes 2000;24(9):1119–1130.ArticlePDF
- 45. de Mestral C, Mayén AL, Petrovic D, Marques-Vidal P, Bochud M, Stringhini S. Socioeconomic determinants of sodium intake in adult populations of high-income countries: a systematic review and meta-analysis. Am J Public Health 2017;107(4):e1–e12.Article
- 46. Kye S, Kwon SO, Lee SY, Lee J, Kim BH, Suh HJ, et al. Under-reporting of energy intake from 24-hour dietary recalls in the Korean National Health and Nutrition Examination Survey. Osong Public Health Res Perspect 2014;5(2):85–91. 24955317.ArticlePubMedPMC
- 47. Straßburg A, Eisinger-Watzl M, Krems C, Roth A, Hoffmann I. Comparison of food consumption and nutrient intake assessed with three dietary assessment methods: results of the German National Nutrition Survey II. Eur J Nutr 2019;58(1):193–210. 29189903.ArticlePubMedPDF
- 48. Trends in sodium intake, 2010-2020. Public Health Wkly Rep 2022;15(48):2914–2915.Article
- 49. World Health Organization (WHO). WHO Global Report on Sodium Intake Reduction. Geneva, Switzerland: WHO; 2023.
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Association of long working hours with visceral adiposity index, anthropometric indices, and weight management behaviors: a study of Korean workers
Seong-Uk Baek, Jin-Ha Yoon
Family Practice.2025;[Epub] CrossRef - Gender discrimination in the workplace and the onset of problematic alcohol use among female wage workers: A longitudinal study in Korea
Seong-Uk Baek, Jin-Ha Yoon, Jong-Uk Won
Social Science & Medicine.2025; 379: 118183. CrossRef - Association between long working hours and poor cardiovascular health assessed by the American Heart Association’s “Life’s essential 8”: findings from a nationally representative sample of Korean workers (2014–2021)
Seong-Uk Baek, Jin-Ha Yoon
Postgraduate Medical Journal.2025; 101(1200): 980. CrossRef - Association Between Food Insecurity and Poor Cardiovascular Health Assessed by the Life’s Essential 8 Metric: A Population-Based Study of Korean Adults
Seong-Uk Baek, Jin-Ha Yoon
Nutrients.2025; 17(13): 2148. CrossRef - OECD Ülkelerinde Kadın Sağlığı Araştırmalarının: Eğilimlerini Analiz Etmek, Boşlukları ve Gelecek Yönelimlerini Belirlemek
Merve Tekinarslan
KutBilim Sosyal Bilimler ve Sanat Dergisi.2025; 5(1): 19. CrossRef - Sex Differences in the Association Between the Korean Healthy Eating Index and Liver Enzymes Among Korean Adults
Seong-Uk Baek, Jin-Ha Yoon
Nutrients.2025; 17(14): 2372. CrossRef - The physical activity paradox in the development of metabolic syndrome: Based on the Korea National Health and nutrition examination survey
Hyung Doo Kim, Tae-Won Jang
Preventive Medicine Reports.2025; 57: 103203. CrossRef - Shift work and dietary behaviors among Korean workers
Chung Ho Kim, Wanhyung Lee
Journal of Occupational Health.2025;[Epub] CrossRef - Flexible screen-printed graphene oxide-based biosensor for sweat sodium detection
L. Marini, P. Chithra Lekha, Roop L. Mahajan, T. Devasena
Current Applied Physics.2025; 80: 145. CrossRef - Association Between Exposure to Age Discrimination and Nutritional Risk: Findings from a Nationwide Sample of Older Adults in South Korea
Seong-Uk Baek, Jin-Ha Yoon
Nutrients.2025; 17(23): 3643. CrossRef - Associations of long working hours with the use of combustible cigarettes, electronic cigarettes, and heated tobacco products among young adults: a population-based study of South Korea
Seong-Uk Baek, Jin-Ha Yoon
Postgraduate Medical Journal.2025;[Epub] CrossRef - Temporary Employment Is Associated with Poor Dietary Quality in Middle-Aged Workers in Korea: A Nationwide Study Based on the Korean Healthy Eating Index, 2013–2021
Seong-Uk Baek, Myeong-Hun Lim, Yu-Min Lee, Jong-Uk Won, Jin-Ha Yoon
Nutrients.2024; 16(10): 1482. CrossRef
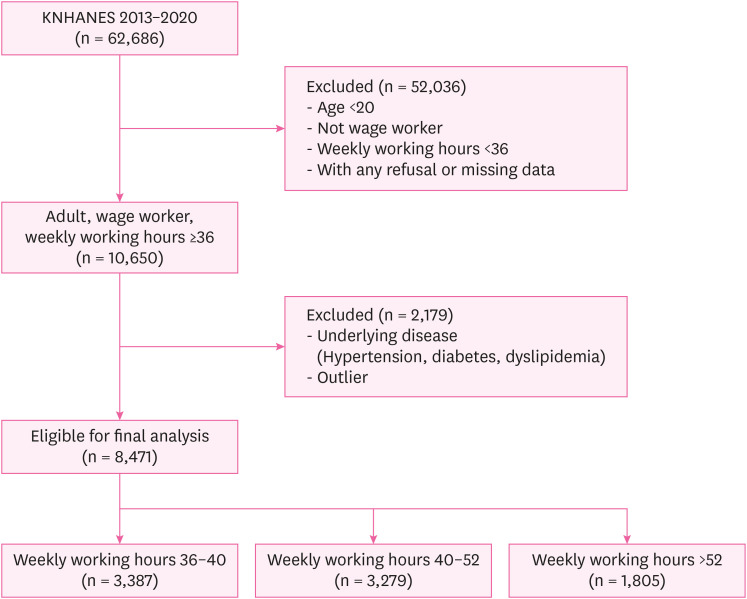
Fig. 1
| Characteristics | Total | Weekly working hours (hours) | ||||
|---|---|---|---|---|---|---|
| 36–40 | 40–52 | > 52 | ||||
| Total | 8,471 (100.0) | 3,387 (40.0) | 3,279 (38.7) | 1,805 (21.3) | ||
| Sex | < 0.001 | |||||
| Male | 4,681 (55.3) | 1,574 (46.5) | 1,864 (56.8) | 1,243 (68.9) | ||
| Female | 3,790 (44.7) | 1,813 (53.5) | 1,415 (43.2) | 562 (31.1) | ||
| Age (years) | < 0.001 | |||||
| 20–29 | 1,370 (16.2) | 575 (17.0) | 563 (17.2) | 232 (12.9) | ||
| 30–39 | 2,608 (30.8) | 997 (29.7) | 1,081 (33.0) | 530 (29.4) | ||
| 40–49 | 2,499 (29.5) | 1,057 (31.2) | 919 (28.0) | 523 (29.0) | ||
| 50–59 | 1,472 (17.4) | 571 (16.9) | 552 (16.8) | 349 (19.3) | ||
| 60 and older | 522 (6.2) | 187 (5.5) | 164 (5.0) | 171 (9.5) | ||
| Household income | < 0.001 | |||||
| Low | 293 (3.5) | 99 (2.9) | 107 (3.3) | 87 (4.8) | ||
| Mid-low | 1,734 (20.5) | 609 (18.0) | 661 (20.2) | 464 (25.7) | ||
| Mid-high | 2,861 (33.8) | 1,065 (31.4) | 1,154 (35.2) | 642 (35.6) | ||
| High | 3,583 (42.3) | 1,614 (47.7) | 1,357 (41.4) | 612 (33.9) | ||
| Education | < 0.001 | |||||
| Elementary | 342 (4.0) | 85 (2.9) | 107 (3.3) | 87 (4.8) | ||
| Middle school | 430 (5.1) | 119 (3.5) | 152 (4.6) | 159 (8.8) | ||
| High school | 2,681 (31.6) | 971 (28.7) | 1,006 (30.7) | 704 (39.0) | ||
| University | 5,018 (59.2) | 2,212 (65.3) | 1,992 (60.8) | 814 (45.1) | ||
| Body mass index | < 0.001 | |||||
| Normal | 5,813 (68.6) | 2,414 (71.3) | 2,245 (68.5) | 1,154 (63.9) | ||
| Overweight or obese | 2,658 (31.4) | 973 (28.7) | 1,034 (31.5) | 651 (36.1) | ||
| Drinking | < 0.001 | |||||
| Non-drinker | 6,944 (82.0) | 2,836 (83.7) | 2,698 (82.3) | 1,410 (78.1) | ||
| Drinker | 1,527 (18.0) | 551 (16.3) | 581 (17.7) | 395 (21.9) | ||
| Smoking | < 0.001 | |||||
| Non-smoker | 4,515 (53.3) | 2,043 (60.3) | 1,722 (52.5) | 750 (41.6) | ||
| Ex-smoker | 1,887 (22.3) | 711 (21.0) | 747 (22.8) | 429 (23.8) | ||
| Current smoker | 2,069 (24.4) | 633 (18.7) | 810 (24.7) | 626 (34.7) | ||
| Occupation group | < 0.001 | |||||
| Manual worker | 2,419 (28.6) | 725 (21.4) | 921 (28.1) | 773 (42.8) | ||
| Non-manual worker | 6,052 (71.4) | 2,662 (78.6) | 2,358 (71.9) | 1,032 (57.2) | ||
| Employment status | < 0.001 | |||||
| Full-time job | 7,319 (86.4) | 3,023 (89.3) | 2,830 (86.3) | 1,466 (81.2) | ||
| Temporary job | 910 (10.7) | 298 (8.8) | 367 (11.2) | 245 (13.6) | ||
| Day labor | 242 (2.9) | 66 (1.9) | 82 (2.5) | 94 (5.2) | ||
| Shiftwork | < 0.001 | |||||
| Day work | 7,334 (86.6) | 3,049 (90.0) | 2,847 (86.8) | 1,466 (79.7) | ||
| Shiftwork | 1,137 (13.4) | 338 (10.0) | 432 (13.2) | 367 (20.3) | ||
| Dining out | < 0.001 | |||||
| Less than once a week | 686 (8.1) | 235 (6.9) | 227 (6.9) | 224 (12.4) | ||
| 1–6 times a week | 3,881 (45.8) | 1,691 (49.9) | 1,495 (45.6) | 695 (38.5) | ||
| More than once a day | 3,904 (46.1) | 1,461 (43.1) | 1,557 (47.5) | 886 (49.1) | ||
| Characteristics | Total | Weekly working hours (hours) | Mean ± SD (mg) | |||
|---|---|---|---|---|---|---|
| 36–40 | 40–52 | > 52 | ||||
| Sodium (mg) | 3,946.8 ± 2,288.2 | 3,740.7 ± 2,086.5 | 4,042.0 ± 2,438.3 | 4,160.6 ± 2,338.2 | ||
| Excessive sodium intake | ||||||
| Less than 2 g | 1,383 (16.3) | 589 (17.4) | 521 (15.9) | 273 (15.1) | 1,431.2 ± 407.6 | |
| More than 2 g | 7,088 (83.7) | 2,798 (82.6) | 2,758 (84.1) | 1,532 (84.9) | 4,437.7 ± 2,179.3 | |
| Sodium intake quartilea | ||||||
| Q1 | 2,118 (25.0) | 909 (26.8) | 796 (24.3) | 413 (22.9) | 1,699.1 ± 498.0 | |
| Q2 | 2,118 (25.0) | 888 (26.2) | 801 (24.4) | 429 (23.8) | 2,957.8 ± 325.8 | |
| Q3 | 2,117 (25.0) | 875 (25.8) | 818 (24.9) | 424 (23.5) | 4,187.1 ± 416.1 | |
| Q4 | 2,118 (25.0) | 715 (21.1) | 864 (26.3) | 539 (29.9) | 6,943.4 ± 2,312.2 | |
| Blood pressure (mmHg) | ||||||
| Systolic | 113.8 ± 13.7 | 113.0 ± 13.9 | 113.6 ± 13.5 | 115.5 ± 13.6 | ||
| Diastolic | 76.1 ± 9.9 | 75.6 ± 9.9 | 76.0 ± 9.9 | 77.1 ± 9.8 | ||
| Characteristics | Weekly working hours (hours) | ||||
|---|---|---|---|---|---|
| 36–40 | 40–52 | > 52 | |||
| Totala | |||||
| Q1 vs. Q2 + Q3 + Q4 | 1 | 1.02 (1.00–1.05) | 1.03 (0.99–1.06) | 0.00 | |
| Q1 + Q2 vs. Q3 + Q4 | 1 | 1.06 (1.01–1.12)b | 1.08 (1.01–1.14)b | 0.00 | |
| Q1 + Q2 + Q3 vs. Q4 | 1 | 1.18 (1.08–1.30)b | 1.28 (1.15–1.43)b | 0.00 | |
| Malea | |||||
| Q1 vs. Q2 + Q3 + Q4 | 1 | 1.02 (0.99–1.05) | 1.01 (0.98–1.05) | 0.91 | |
| Q1 + Q2 vs. Q3 + Q4 | 1 | 1.07 (1.00–1.12) | 1.07 (1.00–1.14)b | 0.28 | |
| Q1 + Q2 + Q3 vs. Q4 | 1 | 1.17 (1.05–1.30)b | 1.22 (1.09–1.38)b | 0.00 | |
| Femalea | |||||
| Q1 vs. Q2 + Q3 + Q4 | 1 | 1.00 (0.97–1.06) | 1.00 (0.92–1.09) | 0.24 | |
| Q1 + Q2 vs. Q3 + Q4 | 1 | 0.98 (0.88–1.09) | 0.89 (0.76–1.05) | 0.45 | |
| Q1 + Q2 + Q3 Vs. Q4 | 1 | 1.03 (0.85–1.26) | 1.12 (0.85–1.47) | 0.06 | |
| Characteristics | Totala | Malea | Femalea | |
|---|---|---|---|---|
| Age (years) | ||||
| 20–29 | 1.00 | 1.00 | 1.00 | |
| 30–39 | 1.16 (1.02–1.31)b | 1.03 (0.90–1.19) | 1.21 (0.94–1.55) | |
| 40–49 | 1.05 (0.92–1.19) | 0.96 (0.83–1.12) | 0.90 (0.69–1.19) | |
| 50–59 | 1.11 (0.96–1.29) | 0.99 (0.83–1.17) | 1.06 (0.75–1.51) | |
| 60 and older | 0.82 (0.67–1.08) | 0.76 (0.59–0.97) | 0.73 (0.39–1.39) | |
| Drinker | ||||
| Non-drinker | 1.00 | 1.00 | 1.00 | |
| Drinker | 1.19 (1.09–1.31)b | 1.15 (1.05–1.26)b | 1.03 (0.73–1.47) | |
| Smoker | ||||
| Non-smoker | 1.00 | 1.00 | 1.00 | |
| Ex-smoker | 1.45 (1.31–1.61)b | 1.09 (0.97–1.23) | 0.82 (0.55–1.22) | |
| Current-smoker | 1.44 (1.30–1.59)b | 1.07 (0.95–1.20) | 0.95 (0.65–1.38) | |
| Household income | ||||
| Low | 1.00 | 1.00 | 1.00 | |
| Mid-low | 1.08 (0.84–1.40) | 1.02 (0.77–1.36) | 1.36 (0.72–2.47) | |
| Mid-high | 1.15 (0.89–1.48) | 1.07 (0.82–1.41) | 1.61 (0.90–2.89) | |
| High | 1.13 (0.88–1.46) | 1.01 (0.77–1.33) | 1.90 (1.07–3.40)b | |
| Education | ||||
| Elementary | 1.00 | 1.00 | 1.00 | |
| Middle school | 0.96 (0.71–1.31) | 1.11 (0.78–1.57) | 0.48 (0.24–0.97) | |
| High school | 1.08 (0.84–1.40) | 1.06 (0.78–1.44) | 0.85 (0.50–1.44) | |
| University | 1.12 (0.85–1.46) | 1.07 (0.78–1.47) | 0.67 (0.38–1.19) | |
| Job | ||||
| Non-manual worker | 1.00 | 1.00 | 1.00 | |
| Manual worker | 1.14 (1.03–1.26)b | 1.04 (0.93–1.15) | 1.03 (0.78–1.37) | |
| Shiftwork | ||||
| Day work | 1.00 | 1.00 | 1.00 | |
| Shiftwork | 0.94 (0.80–1.02) | 0.87 (0.77–1.00) | 1.04 (0.78–1.38) | |
| Employment status | ||||
| Full-time job | 1.00 | 1.00 | 1.00 | |
| Temporary job | 0.87 (0.75–1.02) | 0.87 (0.72–1.04) | 1.16 (0.90–1.49) | |
| Day labor | 1.02 (0.80–1.29) | 1.00 (0.78–1.29) | 1.12 (0.57–2.19) | |
| Frequency of dining out | ||||
| Less than once a week | 1.00 | 1.00 | 1.00 | |
| 1–6 times a week | 1.37 (1.10–1.70)b | 1.25 (0.96–1.63) | 1.39 (0.96–2.02) | |
| More than once a day | 1.67 (1.34–2.08)b | 1.46 (1.12–1.90)b | 1.60 (1.09–2.35)b | |
| Weekly working hours (hours) | ||||
| 36–40 | 1.00 | 1.00 | 1.00 | |
| 40–52 | 1.18 (1.08–1.30)b | 1.17 (1.05–1.30)b | 1.03 (0.85–1.26) | |
| > 52 | 1.28 (1.15–1.43)b | 1.22 (1.09–1.38)b | 1.12 (0.85–1.47) | |
SD: standard deviation.
aQ1: 153.1–2,389.3 mg, Q2: 2,390.0–3,519.0 mg, Q3: 3,520.0–4,961.0 mg, Q4: 4,962.0–28,112.0 mg.
Values are presented as prevalence ratio (95% confidence interval).
aAdjusted for age, drinking, smoking, household income, education, job, employment, shiftwork, and frequency of dining out.
b
Values are presented as prevalence ratio (95% confidence interval).
aAdjusted for age, drinking, smoking, household income, education, job, employment, shift work, and frequency of dining out.
b
 KSOEM
KSOEM

 Cite
Cite

