Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 35; 2023 > Article
- Original Article Risk of insomnia symptoms according to Work-Family Conflict by workers’ characteristics
-
Kwanghyun Seo1
 , Seungjun Ryu1
, Seungjun Ryu1 , Saebomi Jeong1
, Saebomi Jeong1 , Hee-Tae Kang1
, Hee-Tae Kang1 , Sung-Kyung Kim1
, Sung-Kyung Kim1 , Sang-Baek Koh2
, Sang-Baek Koh2 , Kyoung Sook Jeong1
, Kyoung Sook Jeong1 , Sung-Soo Oh1
, Sung-Soo Oh1
-
Annals of Occupational and Environmental Medicine 2023;35:e36.
DOI: https://doi.org/10.35371/aoem.2023.35.e36
Published online: August 23, 2023
1Department of Occupational and Environmental Medicine, Wonju Severance Christian Hospital, Wonju College of Medicine, Yonsei University, Wonju, Korea.
2Department of Preventive Medicine and Genomic Cohort Institute, Wonju College of Medicine, Yonsei University, Wonju, Korea.
- Correspondence: Kyoung Sook Jeong. Department of Occupational and Environmental Medicine, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, 20 Ilsan-ro, Wonju 26426, Korea. jeongks@yonsei.ac.kr
- Correspondence: Sung-Soo Oh. Department of Occupational and Environmental Medicine, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, 20 Ilsan-ro, Wonju 26426, Korea. oss0609@yonsei.ac.kr
Copyright © 2023 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background Work-Family Conflict means that the demands of work and family roles cannot be met simultaneously, so one cannot concentrate on one’s work or family role. This conflict can negatively affect mental health and cause insomnia symptoms.
-
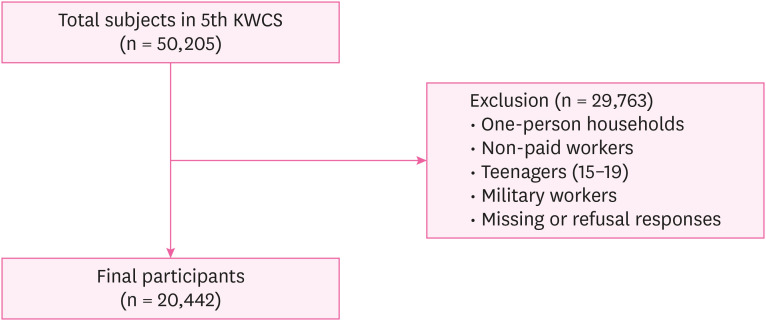
Methods This study was conducted on 20,442 subjects. Insomnia symptoms were assessed using the Minimal Insomnia Symptom Scale, and other variables were assessed using the questionnaire method. Logistic regression analyses were performed to evaluate the effect of Work-Family Conflict on insomnia symptoms, and subgroup logistic regression analyses were also performed.
-
Results The number of people with insomnia symptoms was 4,322 (15.1%). Compared with Low Work-Family Conflict, the odds ratios (ORs) for the risk of insomnia symptoms were 1.84 (95% confidence interval: 1.56–2.16) in High work-to-family conflict, 1.16 (1.02–1.32) in High family-to-work conflict, and 3.19 (2.87–3.55) in High Work-Family Conflict. The ORs were higher for men than women in High WFC but higher for women than men in High Work-Family Conflict.
-
Conclusions The risk of insomnia symptoms was highest in High Work-Family Conflict.
BACKGROUND
METHODS
Classification of participants according to Work-Family Conflict.
Four classifications of Work-Family Conflict
| Variables | WFC | ||
|---|---|---|---|
| Low | High | ||
| FWC | |||
| Low | Low Work-Family Conflict (n = 6,602) | High WFC (n = 2,004) | |
| High | High FWC (n = 6,663) | High Work-Family Conflict (n = 13,307) | |
RESULTS
Characteristics of study subjects according to insomnia symptoms
Distribution of Work-Family Conflict by general characteristics
Odds ratios of insomnia symptoms according to Work-Family Conflict
Adjusted odds ratios of insomnia symptoms according to Work-Family Conflict in subgroups
DISCUSSION
CONCLUSIONS
Acknowledgements
Abbreviations
CI
FWC
KRW
KWCS
MISS
OR
OSHRI
SD
Sx
WFC
-
Competing interests: The authors declare that they have no competing interests.
-
Authors contributions:
Conceptualization: Seo K.
Data curation: Seo K, Ryu S, Jeong S.
Formal analysis: Seo K.
Investigation: Ryu S, Jeong S, Jeong KS, Oh SS.
Methodology: Seo K, Oh SS.
Software: Seo K.
Supervision: Kang HT, Kim SK, Koh SB, Jeong KS, Oh SS.
Validation: Jeong KS, Oh SS.
Visualization: Seo K.
Writing - original draft: Seo K.
Writing - review & editing: Jeong KS, Oh SS.
NOTES
- 1. Owens JF, Matthews KA. Sleep disturbance in healthy middle-aged women. Maturitas 1998;30(1):41–50. 9819782.ArticlePubMed
- 2. HIRA Healthcare Bigdata Hub. Disease statistics of national interest. Updated 2022]. Accessed November 7, 2022]. http://opendata.hira.or.kr/op/opc/olapMfrnIntrsIlnsInfo.do .
- 3. Kripke DF, Simons RN, Garfinkel L, Hammond EC. Short and long sleep and sleeping pills. Is increased mortality associated? Arch Gen Psychiatry 1979;36(1):103–116. 760693.ArticlePubMed
- 4. Grandner MA, Jackson NJ, Pak VM, Gehrman PR. Sleep disturbance is associated with cardiovascular and metabolic disorders. J Sleep Res 2012;21(4):427–433. 22151079.ArticlePubMed
- 5. Pearson NJ, Johnson LL, Nahin RL. Insomnia, trouble sleeping, and complementary and alternative medicine: analysis of the 2002 national health interview survey data. Arch Intern Med 2006;166(16):1775–1782. 16983058.ArticlePubMed
- 6. Roth T, Jaeger S, Jin R, Kalsekar A, Stang PE, Kessler RC. Sleep problems, comorbid mental disorders, and role functioning in the national comorbidity survey replication. Biol Psychiatry 2006;60(12):1364–1371. 16952333.ArticlePubMedPMC
- 7. Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry 2012;73(9):e1160–e1167. 23059158.ArticlePubMed
- 8. Greenhaus JH, Beutell NJ. Sources of conflict between work and family roles. Acad Manage Rev 1985;10(1):76–88.Article
- 9. Sato S, Liu Y, Ikeda A, Filomeno R, Suzuki Y, Maruyama K, et al. Work-family conflict and insomnia symptoms among women working in aged care services in Japan. Sleep Med 2021;82:155–158. 33930791.ArticlePubMed
- 10. Voydanoff P. Work role characteristics, family structure demands, and work/family conflict. J Marriage Fam 1988;50(3):749–761.Article
- 11. Borgmann LS, Rattay P, Lampert T. Health-related consequences of work-family conflict from a European perspective: results of a scoping review. Front Public Health 2019;7:189. 31338358.ArticlePubMedPMC
- 12. Thorpy MJ. Classification of sleep disorders. Neurotherapeutics 2012;9(4):687–701. 22976557.ArticlePubMedPMCPDF
- 13. Frone MR. Work-family conflict and employee psychiatric disorders: the National Comorbidity Survey. J Appl Psychol 2000;85(6):888–895. 11155895.ArticlePubMed
- 14. Sohn YM, Park CY. Influence of work-family related values on work-family conflict and facilitation: focused on married working woman. J Korea Contents Assoc 2015;15(7):203–215.Article
- 15. Yavas U, Babakus E, Karatepe OM. Attitudinal and behavioral consequences of work-family conflict and family-work conflict: does gender matter? Int J Serv Ind Manage 2008;19(1):7–31.
- 16. Son MG. The changes of father’s participation in the domestic activities of everyday life: focusing on statistics from time use survey in 1999 and 2014. J Korean Soc Trend Perspect 2016;6.
- 17. Choi Y, Park J. The Korean Working Conditions Survey (KWCS): a review on the utilization of the survey database. J Korean Soc Occup Environ Hyg 2019;29(4):431–441.
- 18. Eshak ES. Work-to-family conflict rather than family-to-work conflict is more strongly associated with sleep disorders in Upper Egypt. Ind Health 2019;57(3):351–358. 30101898.ArticlePubMed
- 19. Broman JE, Smedje H, Mallon L, Hetta J. The Minimal Insomnia Symptom Scale (MISS): a brief measure of sleeping difficulties. Ups J Med Sci 2008;113(2):131–142. 18509808.PubMed
- 20. Hellström A, Hagell P, Fagerström C, Willman A. Measurement properties of the Minimal Insomnia Symptom Scale (MISS) in an elderly population in Sweden. BMC Geriatr 2010;10(1):84. 21054878.PubMedPMC
- 21. Yang B, Wang Y, Cui F, Huang T, Sheng P, Shi T, et al. Association between insomnia and job stress: a meta-analysis. Sleep Breath 2018;22(4):1221–1231. 29959635.ArticlePubMedPDF
- 22. Buxton OM, Lee S, Beverly C, Berkman LF, Moen P, Kelly EL, et al. Work-family conflict and employee sleep: evidence from IT workers in the Work, Family and Health Study. Sleep 2016;39(10):1871–1882. 27568810.ArticlePubMedPMC
- 23. Fujimura Y, Sekine M, Tatsuse T. Sex differences in factors contributing to family-to-work and work-to-family conflict in Japanese civil servants. J Occup Health 2014;56(6):485–497. 25374422.ArticlePubMedPDF
- 24. Ministry of Gender Equality and Family (KR). 2021 Gender equality report. Updated 2022]. Accessed November 14, 2022]. http://www.mogef.go.kr/mp/pcd/mp_pcd_s001d.do?mid=plc500&bbtSn=704919 .
- 25. Yoon SY, Kim HJ. A Study on the subjective cognition and conflict degree of work-family balance and family strength of a dual career men. J Korean Fam Resour Manage Assoc 2013;17(2):19–35.
- 26. Sawang S, Newton CJ. Defining work stress in young people. J Employ Couns 2018;55(2):72–83.ArticlePDF
- 27. Choung SI, Lee KY. A study on the interaction between work-family of married employees. J Korean Fam Resour Manage Assoc 2007;11(1):83–107.
- 28. Park SH. Emotional labor job characteristics and policy implications using KNOW. Korean Longit Stud Elder Employ 2015;(10):2–13.
- 29. Kang D, Yang JW, Choi WJ, Ham S, Kang SK, Lee W. Anxiety, depression and sleep disturbance among customer-facing workers. J Korean Med Sci 2019;34(48):e313. 31833267.ArticlePubMedPMCPDF
- 30. Yanchus NJ, Eby LT, Lance CE, Drollinger S. The impact of emotional labor on work–family outcomes. J Vocat Behav 2010;76(1):105–117.Article
- 31. Wöhrmann AM, Müller G, Ewert K. Shift work and work-family conflict: a systematic review. Sozialpolitik Ch 2020;3:1–6.
- 32. Lee S, Kwon Y. The mediating effect of work-family conflict on the relationship between family-friendly workplace culture and paternal involvement. Fam Cult 2009;21(1):1–28.Article
- 33. Adkins CL, Premeaux SF. Spending time: the impact of hours worked on work–family conflict. J Vocat Behav 2012;80(2):380–389.Article
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Longitudinal trajectories and risk factors of insomnia symptoms among Chinese bus drivers
Jingbo Zhao, Huatao Yang, Qiling Fan, Zijie Ma, Yang Yang, Zicong Guan, Guoxi He
Frontiers in Public Health.2026;[Epub] CrossRef - Benefits and Drawbacks of 12-hour Shifts in Steel Manufacturing: a Comprehensive Qualitative Investigation of Workers, Managers, and Family Perspectives
Alireza Choobineh, Mahnaz Shakerian, Majid Faraji, Hossein Modaresifar, Javad Kiani, Mehdi Hatami, Reza Tahmasebi
Occupational Health Science.2025; 9(4): 1075. CrossRef - Female workers with long working hours are more likely to have depressive symptoms when having family-to-work conflict
Garin Lee, Ji-Hwan Kim, Seung-Sup Kim
International Archives of Occupational and Environmental Health.2024; 97(2): 199. CrossRef - Association between long working hours and engagement in preventive healthcare services in Korean workers: Findings from the Korean National Health and Nutrition Examination Survey
Seong-Uk Baek, Yu-Min Lee, Jin-Ha Yoon
Preventive Medicine.2024; 180: 107849. CrossRef - Difficulty Falling Asleep, Nocturnal Awakening, Sleep Dissatisfaction, and Irritability in the General Population
Tetsuya Akaishi
The Tohoku Journal of Experimental Medicine.2024; 263(4): 261. CrossRef - Association between single-person household wage workers in South Korea and insomnia symptoms: the 6th Korean Working Conditions Survey (KWCS)
Yoon Ho Lee, Yong-Jin Lee, Eun-Chul Jang, Young-Sun Min, Soon-Chan Kwon
Ann Occup Environ Med.2024; 36: e25. CrossRef
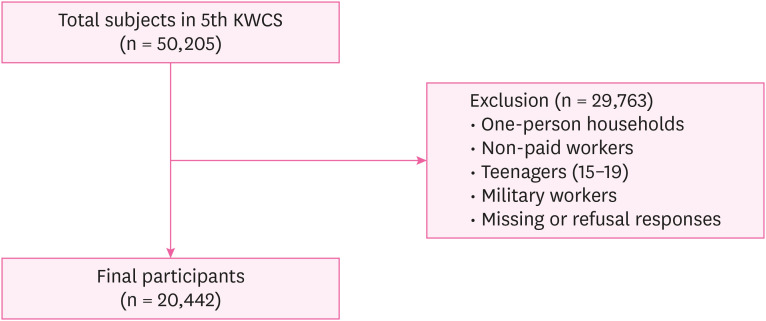
Fig. 1
| Variables | WFC | ||
|---|---|---|---|
| Low | High | ||
| FWC | |||
| Low | Low Work-Family Conflict (n = 6,602) | High WFC (n = 2,004) | |
| High | High FWC (n = 6,663) | High Work-Family Conflict (n = 13,307) | |
| Variables | Total (n = 28,576)a | Insomnia Sx | |||
|---|---|---|---|---|---|
| Yes (n = 4,322)a | No (n = 24,254)a | ||||
| Sex | < 0.001 | ||||
| Male | 16,302 (57.0) | 2,336 (14.3) | 13,966 (85.7) | ||
| Female | 12,274 (43.0) | 1,986 (16.2) | 10,288 (83.8) | ||
| Age (years) | < 0.001 | ||||
| 20–29 | 4,631 (16.2) | 633 (13.7) | 3,998 (86.3) | ||
| 30–39 | 7,388 (25.9) | 981 (13.3) | 6,407 (86.7) | ||
| 40–49 | 7,743 (27.1) | 1,136 (14.7) | 6,607 (85.3) | ||
| 50–59 | 5,879 (20.6) | 1,008 (17.1) | 4,871 (82.9) | ||
| ≥ 60 | 2,936 (10.3) | 564 (19.2) | 2,372 (80.8) | ||
| Mean ± SD | 43.2 ± 12.4 | 44.8 ± 12.9 | 42.9 ± 12.3 | < 0.001 | |
| Education level | < 0.001 | ||||
| High school or below | 10,943 (38.3) | 1,825 (16.7) | 9,118 (83.3) | ||
| University or above | 17,633 (61.7) | 2,496 (14.2) | 15,137 (85.8) | ||
| Monthly income (10,000 Korean won) | 0.003 | ||||
| < 100 | 1,896 (6.6) | 304 (16.0) | 1,592 (84.0) | ||
| 100–199 | 6,987 (24.5) | 1,142 (16.3) | 5,845 (83.7) | ||
| 200–299 | 8,176 (28.6) | 1,188 (14.5) | 6,988 (85.5) | ||
| 300 | 11,517 (40.3) | 1,687 (14.6) | 9,830 (85.4) | ||
| Depressive symptom | < 0.001 | ||||
| No | 27,985 (97.9) | 4,122 (14.7) | 23,863 (85.3) | ||
| Yes | 590 (2.1) | 199 (33.7) | 391 (66.3) | ||
| Anxiety symptom | < 0.001 | ||||
| No | 27,759 (97.1) | 4,062 (14.6) | 23,697 (85.4) | ||
| Yes | 817 (2.9) | 260 (31.8) | 557 (68.2) | ||
| Workplace scale (persons) | < 0.001 | ||||
| 1–49 | 20,744 (72.6) | 3,304 (15.9) | 17,440 (84.1) | ||
| 50–249 | 5,026 (17.6) | 676 (13.5) | 4,350 (86.5) | ||
| ≥ 250 | 2,806 (9.8) | 342 (12.2) | 2,464 (87.8) | ||
| Weekly working time (hours) | < 0.001 | ||||
| ≤ 40 | 17,065 (59.7) | 2,330 (13.7) | 14,735 (86.3) | ||
| 41–52 | 7,871 (27.5) | 1,245 (15.8) | 6,626 (84.2) | ||
| ≥ 53 | 3,640 (12.7) | 746 (20.5) | 2,894 (79.5) | ||
| Occupational type | < 0.001 | ||||
| Blue-collar | 8,889 (31.1) | 1,408 (15.8) | 7,481 (84.2) | ||
| Service and sales | 5,523 (19.3) | 943 (17.1) | 4,580 (82.9) | ||
| White-collar | 14,163 (49.6) | 1,970 (13.9) | 12,193 (86.1) | ||
| Shift work | < 0.001 | ||||
| No | 25,306 (88.6) | 3,676 (14.5) | 21,630 (85.5) | ||
| Yes | 3,270 (11.4) | 646 (19.8) | 2,624 (80.2) | ||
| Work intensity | < 0.001 | ||||
| Low | 13,359 (46.7) | 1,369 (10.2) | 11,990 (89.8) | ||
| High | 15,217 (53.3) | 2,953 (19.4) | 12,264 (80.6) | ||
| Job autonomy | 0.017 | ||||
| High | 14,187 (49.6) | 2,073 (14.6) | 12,114 (85.4) | ||
| Low | 14,389 (50.4) | 2,249 (15.6) | 12,140 (84.4) | ||
| Job stress | < 0.001 | ||||
| Low | 19,786 (69.2) | 2,505 (12.7) | 17,281 (87.3) | ||
| High | 8,790 (30.8) | 1,817 (20.7) | 6,973 (79.3) | ||
| Emotional labor | < 0.001 | ||||
| No | 16,784 (58.7) | 2,265 (13.5) | 14,519 (86.5) | ||
| Yes | 11,793 (41.3) | 2,057 (17.4) | 9,736 (82.6) | ||
| Work-Family Conflict | < 0.001 | ||||
| Low Work-Family Conflict | 6,602 (23.1) | 478 (7.2) | 6,124 (92.8) | ||
| High WFC | 2,004 (7.0) | 275 (13.7) | 1,729 (86.3) | ||
| High FWC | 6,663 (23.3) | 564 (8.5) | 6,099 (91.5) | ||
| High Work-Family Conflict | 13,307 (46.6) | 3,004 (22.6) | 10,303 (77.4) | ||
| Subgroup | Work-Family Conflict | |||||
|---|---|---|---|---|---|---|
| Low Work-Family Conflict (n = 6,602)a | High WFC (n = 2,004)a | High FWC (n = 6,663)a | High Work-Family Conflict (n = 13,307)a | |||
| Sex | < 0.001 | |||||
| Male | 3,654 (22.4) | 1,274 (7.8) | 3,830 (23.5) | 7,544 (46.3) | ||
| Female | 2,948 (24.0) | 730 (5.9) | 2,833 (23.1) | 5,763 (47.0) | ||
| Age (years) | < 0.001 | |||||
| 20–29 | 1,213 (26.2) | 312 (6.7) | 1,158 (25.0) | 1,947 (42.1) | ||
| 30–39 | 1,504 (20.4) | 541 (7.3) | 1,768 (23.9) | 3,575 (48.4) | ||
| 40–49 | 1,749 (22.6) | 597 (7.7) | 1,646 (21.3) | 3,751 (48.4) | ||
| 50–59 | 1,274 (21.7) | 389 (6.6) | 1,338 (22.8) | 2,878 (49.0) | ||
| ≥ 60 | 863 (29.4) | 164 (5.6) | 753 (25.6) | 1,156 (39.4) | ||
| Education level | < 0.001 | |||||
| High school or below | 2,686 (24.5) | 702 (6.4) | 2,497 (22.8) | 5,058 (46.2) | ||
| University or above | 3,917 (22.2) | 1,302 (7.4) | 4,166 (23.6) | 8,249 (46.8) | ||
| Weekly working time (hours) | < 0.001 | |||||
| ≤ 40 | 4,449 (26.1) | 972 (5.7) | 4,534 (26.6) | 7,110 (41.7) | ||
| 41–52 | 1,666 (21.2) | 611 (7.8) | 1,570 (19.9) | 4,024 (51.1) | ||
| ≥ 53 | 488 (13.4) | 421 (11.6) | 558 (15.3) | 2,173 (59.7) | ||
| Occupational type | < 0.001 | |||||
| Blue-collar | 2,121 (23.9) | 656 (7.4) | 2,016 (22.7) | 4,097 (46.1) | ||
| Service and sales | 1,213 (22.0) | 321 (5.8) | 1,297 (23.5) | 2,692 (48.7) | ||
| White-collar | 3,268 (23.1) | 1,027 (7.3) | 3,349 (23.6) | 6,519 (46.0) | ||
| Shift work | < 0.001 | |||||
| No | 5,907 (23.3) | 1,715 (6.8) | 6,028 (23.8) | 11,656 (46.1) | ||
| Yes | 695 (21.3) | 289 (8.8) | 635 (19.4) | 1,651 (50.5) | ||
| Work-Family Conflict | Insomnia Sx | |||
|---|---|---|---|---|
| Crude | Model 1a | Model 2b | Model 3c | |
| Low Work-Family Conflict | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) | 1 (Ref.) |
| High WFC | 2.04 (1.74–2.39) | 2.14 (1.82–2.50) | 2.21 (1.88–2.59) | 1.84 (1.56–2.16) |
| High FWC | 1.18 (1.04–1.34) | 1.20 (1.06–1.37) | 1.22 (1.07–1.38) | 1.16 (1.02–1.32) |
| High Work-Family Conflict | 3.73 (3.37–4.13) | 3.85 (3.48–4.27) | 3.97 (3.58–4.40) | 3.19 (2.87–3.55) |
| Subgroup | Work-Family Conflicta | ||||
|---|---|---|---|---|---|
| Low Work-Family Conflict | High WFC | High FWC | High Work-Family Conflict | ||
| Sex | |||||
| Male | 1 (Ref.) | 1.98 (1.61–2.43) | 1.19 (1.00–1.42) | 2.91 (2.52–3.37) | |
| Female | 1 (Ref.) | 1.60 (1.23–2.09) | 1.13 (0.93–1.36) | 3.62 (3.10–4.23) | |
| Age (years) | |||||
| 20–29 | 1 (Ref.) | 2.46 (1.61–3.77) | 1.36 (0.97–1.90) | 4.64 (3.50–6.15) | |
| 30–39 | 1 (Ref.) | 1.80 (1.26–2.56) | 1.38 (1.04–1.83) | 3.35 (2.64–4.26) | |
| 40–49 | 1 (Ref.) | 1.94 (1.41–2.67) | 1.28 (0.98–1.69) | 3.43 (2.75–4.28) | |
| 50–59 | 1 (Ref.) | 1.23 (0.85–1.78) | 1.02 (0.78–1.33) | 2.60 (2.10–3.23) | |
| ≥ 60 | 1 (Ref.) | 3.37 (2.20–5.16) | 0.88 (0.64–1.21) | 3.15 (2.41–4.11) | |
| Education level | |||||
| High school or below | 1 (Ref.) | 1.63 (1.26–2.10) | 1.13 (0.94–1.37) | 2.77 (2.37–3.24) | |
| University or above | 1 (Ref.) | 2.02 (1.64–2.50) | 1.18 (0.99–1.41) | 3.28 (3.10–4.14) | |
| Weekly working time (hours) | |||||
| ≤ 40 | 1 (Ref.) | 1.35 (1.05–1.74) | 1.09 (0.93–1.28) | 3.82 (3.34–4.37) | |
| 41–52 | 1 (Ref.) | 1.76 (1.29–2.41) | 1.37 (1.06–1.78) | 3.14 (2.54–3.87) | |
| ≥ 53 | 1 (Ref.) | 2.22 (1.54–3.19) | 1.10 (0.76–1.61) | 1.79 (1.32–2.42) | |
| Occupational type | |||||
| Blue-collar | 1 (Ref.) | 1.56 (1.18–2.07) | 1.05 (0.85–1.30) | 2.62 (2.20–3.13) | |
| Service and sales | 1 (Ref.) | 2.57 (1.78–3.72) | 1.26 (0.94–1.67) | 3.57 (2.81–4.55) | |
| White-collar | 1 (Ref.) | 1.83 (1.44–2.34) | 1.22 (1.00–1.48) | 3.58 (3.04–4.20) | |
| Shift work | |||||
| No | 1 (Ref.) | 1.76 (1.47–2.10) | 1.15 (1.00–1.32) | 3.29 (2.93–3.69) | |
| Yes | 1 (Ref.) | 2.11 (1.43–3.11) | 1.20 (0.85–1.70) | 2.62 (1.97–3.49) | |
Number of workers was weighted.
WFC: work-to-family conflict; FWC: family-to-work conflict.
Unit: person (%).
Sx: symptoms; WFC: work-to-family conflict; FWC: family-to-work conflict; SD: standard deviation.
aWeighted numbers of workers.
bχ2 test for binomial variables and t-test for numeric variables.
Unit: person (%).
WFC: work-to-family conflict; FWC: family-to-work conflict.
aWeighted numbers of workers.
bχ2 test for binomial variables and t-test for numeric variables.
Data are shown as odds ratio and 95% confidence intervals.
Sx: symptoms; WFC: work-to-family conflict; FWC: family-to-work conflict.
aModel 1: adjusted for sex, age, and education level.
bModel 2: adjusted for all variables in Model 1 and monthly income.
cModel 3: adjusted for all variables in Model 2, workplace scale, weekly working time, occupational type, shift work, work intensity, job autonomy, job stress, emotional labor, depressive symptom, and anxiety symptom.
Data are shown as adjusted odds ratio and 95% confidence intervals.
WFC: work-to-family conflict; FWC: family-to-work conflict.
aAdjusted for sex, age, education level, monthly income, workplace scale, weekly working time, occupational type, shift work, work intensity, job autonomy, job stress, emotional labor, depressive symptom, and anxiety symptom.
 KSOEM
KSOEM

 Cite
Cite

