Abstract
-
Background
According to the occupational accident status analysis in 2020, of 1,180 occupational deaths, 463 were caused by cardiovascular disease (CVD). Workers should be assessed for CVD risk at regular intervals to prevent work-related CVD in accordance with the rules on occupational safety and health standards. However, no previous study has addressed risk and mortality. Therefore, this longitudinal study was conducted to evaluate the relationship between 10-year cardiovascular risk of the general health checkup and mortality.
-
Methods
The study included 545,859 participants who visited Kangbuk Samsung Total Healthcare Centers from January 1, 2002, to December 31, 2017. We performed 10-year cardiovascular risk assessment for the participants and the risk was divided into 4 groups (low, moderate, high, and very high). The study used death data from the Korea National Statistical Office for survival status as an outcome variable by December 31, 2019, and the cause of death based on the International Classification of Diseases, 10th Revision (ICD-10) was identified. Statistical analysis was performed using Cox proportional hazards regression analysis, and the sum of the periods from the first visit to the date of death or December 31, 2019, was used as a time scale. We also performed a stratified analysis for age at baseline and sex.
-
Results
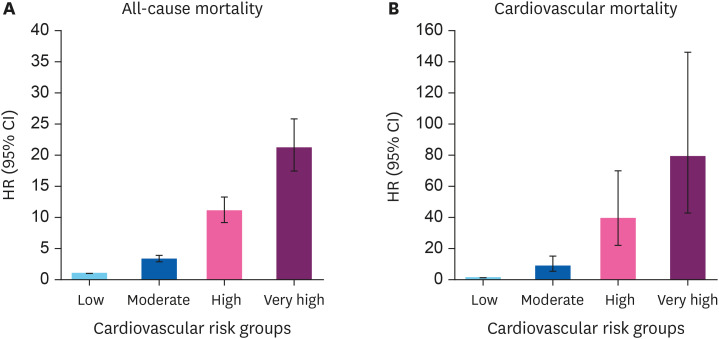
During 5,253,627.9 person-years, 4,738 overall deaths and 654 cardiovascular deaths occurred. When the low-risk group was set as a reference, in the multivariable-adjusted model, the hazard ratios (HRs) (95% confidence interval [CI]) for overall mortality were 3.36 (2.87–3.95) in the moderate-risk group, 11.08 (9.27–13.25) in the high-risk group, and 21.20 (17.42–25.79) in the very-high-risk group, all of which were statistically significant. In cardiovascular deaths, the difference according to the risk classification was more pronounced. The HRs (95% CI) were 8.57 (4.95–14.83), 38.95 (21.77–69.69), and 78.81 (42.62–145.71) in each group. As a result of a subgroup analysis by age and sex, the HRs of all-cause mortality and cardiovascular mortality tended to be higher in the high-risk group.
-
Conclusions
This large-scale longitudinal study confirmed that the risk of death increases with the 10-year cardiovascular risk of general health checkup.
-
Keywords: 10-year cardiovascular risk; Cardiovascular disease; Cardiovascular mortality; Mortality; Longitudinal study; Kangbuk Samsung Cohort Study
BACKGROUND
According to the death data of the National Statistical Office, of 304,948 people who died in 2020, 62,196 died of circulatory system diseases, including ischemic heart disease and cerebrovascular disease.
1 Moreover, according to the occupational accident status analysis in 2020 by the Korea Occupational Safety and Health Agency (KOSHA), of 1,180 occupational deaths in 2020, 463 were caused by cardiovascular disease (CVD), accounting for a high proportion.
2 Workers should be assessed for CVD risk and should undergo follow-up at regular intervals to prevent work-related CVD in accordance with the rules on occupational safety and health standards.
3 The Industrial Safety and Health Act mandates that all Korean workers be classified for the risk of cerebrovascular disease at least every 2 years.
Several studies have evaluated the prediction of the incidence of CVD according to cardiovascular risk assessment models.
4,5,6 However, no previous studies have calculated the mortality and hazard ratio (HR) according to cardiovascular risk using death data produced by the government. There are various CVD prediction models abroad, but they are not used in Korea because of their disadvantages. The Framingham risk score, which was developed based on the Framingham Heart Study in the United States, has been reported to overestimate the risk of CVD in the Asian population.
7,8 The American College of Cardiology/American Heart Association CVD prediction model is developed based on large-scale cohort data in which other cohorts are integrated into the Framingham cohort. This model overestimates the risk of CVD in Korean men, underestimates the risk in Korean women, and overestimates the overall risk.
9 Furthermore, since this model is an evaluation model targeting individuals aged ≥ 40 years, it is difficult to apply it to workers aged < 40 years.
10
We studied the differences in mortality according to cardiovascular risk using cohort data with large samples. In this study, the 10-year cardiovascular risk of the general health checkup was used. We referred to the KOSHA GUIDE (H-200-2018), but the integrated risk classification criteria including angiography and hypertensive retinopathy were not applied, because the purpose of this study was to determine the significant difference in the risk of cardiovascular death, even if only general health examination items, such as blood pressure and blood glucose levels, which can be obtained relatively easily, are used. Using data from the Kangbuk Samsung Cohort Study, which is a cohort of health examination data accumulated since 2002, this study conducted the 10-year cardiovascular risk classification and analyzed the difference in mortality according to the risk using the death data of the National Statistical Office.
METHODS
Study population
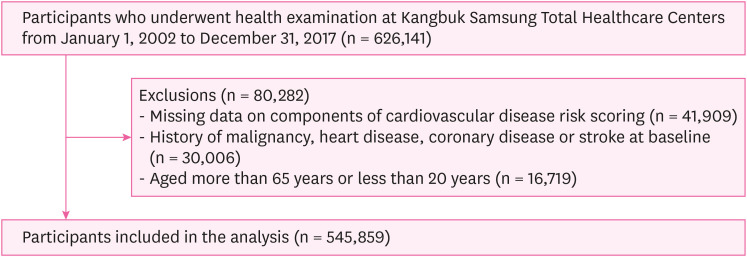
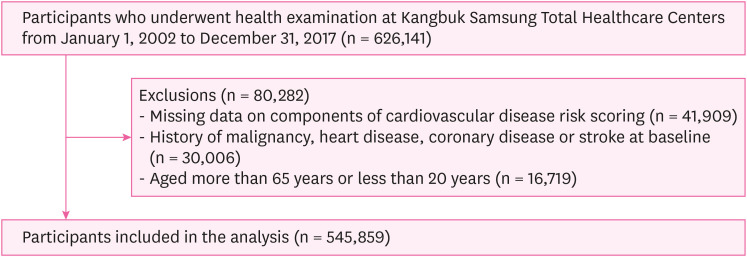
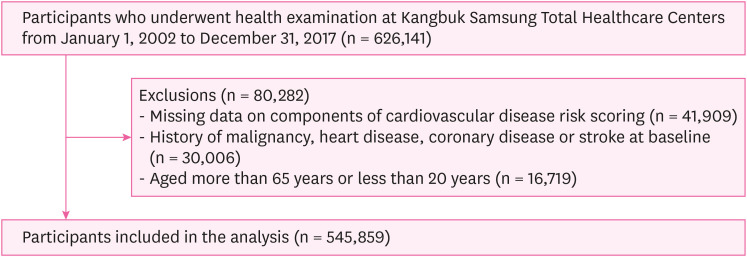
The study used cohort data of individuals who underwent medical examination at Kangbuk Samsung Total Healthcare Centers in Seoul and Suwon. The study participants consisted of individuals who visited Kangbuk Samsung Total Healthcare Centers from January 1, 2002, to December 31, 2017, and whose survival status was confirmed by December 31, 2019. A total of 80,282 subjects who met the following criteria were excluded (
Fig. 1): missing data on components of CVD risk scoring (n = 41,909); history of malignancy, heart disease, coronary disease, or stroke at baseline (n = 30,006); and age > 65 years or < 20 years (n = 16,719). A total of 545,859 participants were included in this study.
Fig. 1Flowchart of study participants.
CVD risk
We calculated the 10-year cardiovascular risk of the participants using the following 11 risk factors: body mass index (BMI), waist circumference, smoking status, blood pressure, medication for hypertension, physical activity, fasting blood glucose, medication for diabetes, serum total cholesterol, glomerular filtration rate (GFR), and dipstick proteinuria. For BMI and waist circumference, those with higher risk were selected, and those with higher GFR and proteinuria were selected. Nine independent odds ratios were determined. To calculate the composite relative risk, which is the sum of the abovementioned nine risk factors, the values obtained by subtracting 1 from the value of each risk factor were added. The adjusted composite relative risk was calculated by dividing this composite relative risk by the average composite relative risk of individuals whose age and sex were the same as the participant. The average composite relative risk according to age and sex was set as the reference value. Finally, the 10-year cardiovascular risk was calculated by multiplying the adjusted composite relative risk by the average 10-year cardiovascular risk of individuals whose age and sex were the same as the participant. Participants were classified by 10-year cardiovascular risk cutoff values as follows: < 1% (low risk), > 1% and < 5% including 1% (moderate risk), > 5% and < 10% including 5% (high risk), and ≥ 10% (very high risk) referring to KOSHA GUIDE (H-200-2018).
3
Examinations for CVD risk scoring were conducted at Kangbuk Samsung Total Healthcare Center. Data on family history, physical activity, alcohol intake, smoking habits, education level and medical history were collected using a standardized, self-administered questionnaire. Alcohol consumption was categorized into none, ≤ 10 g/day, and > 10 g/day. The weekly frequency of moderate- or vigorous-intensity physical activity was also assessed. Education level was categorized into less than college graduate and college graduate or more.
Height and weight were measured by trained nurses with the participants wearing a lightweight hospital gown and no shoes. BMI was calculated as weight in kilograms divided by height in meters squared. Blood pressure was measured by trained nurses while subjects were in a sitting position with the arm supported at heart level. Blood specimens were sampled from the antecubital vein after at least a 10-hour fast. Serum levels of fasting glucose, total cholesterol, triglycerides (TGs), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C) and high sensitivity C-reactive protein (hs-CRP) are measured.
Mortality ascertainment
We used death data of Korea National Statistical Office with survival status as an outcome variable by December 31, 2019. In addition to survival status, the cause of death based on the International Classification of Diseases, 10th Revision (ICD-10) was identified. The death code “I” was classified as cardiovascular death.
Statistical analysis
Based on the first visit, the baseline characteristics were shown using descriptive summary statistics, including mean (standard deviation), median (interquartile range), or number (percentage), according to the risk categories. Statistical analysis was performed using Cox proportional hazards regression analysis, and the sum of the periods from the first visit to the date of death or December 31, 2019 was used as a time scale. Initially, model 1 was adjusted for the health examination center and year of examination at baseline. Model 2 was further adjusted for alcohol consumption, education level, and hs-CRP levels well known CVD factor at baseline.
11 Since the traditional risk factors for CVD, such as blood pressure and glucose level, have already been included in the risk grouping criteria, we cannot adjust for such variables in the statistical analysis. Instead, we performed a stratified analysis for age at baseline and sex. Age was categorized into < 40, 40 to < 50, 50 to < 60, and ≥ 60 years. This study used Stata version 17.0 (StataCorp LP, College Station, TX, USA) for statistical analysis. Statistical significance was defined as a 2-sided
p-value < 0.05.
The Institutional Review Board of Kangbuk Samsung Hospital approved this study (IRB No. 2021-10-050) and waived the requirement for informed consent. This was due to the use of anonymized data that were routinely collected as part of a health checkup program.
RESULTS
The mean age of the study participants at baseline was 37.9 years (standard deviation, 9.2), and men accounted for 54.1%. Of 545,859 participants, 306,424 were assigned to the low-risk group, 199,198 to the moderate-risk group, 32,031 to the high-risk group, and 8,206 to the very-high-risk group. Between 4 groups, there were significant differences in age, sex, smoking status, drinking status, regular exercise, education level, marital status, medication for hypertension, medication for diabetes and medication for dyslipidemia, BMI, obesity, systolic blood pressure (SBP), diastolic blood pressure (DBP), and blood glucose, total cholesterol, LDL-C, HDL-C, TG, and hs-CRP levels. Cardiovascular risk was positively associated with age, medication for hypertension, medication for diabetes, medication for dyslipidemia, BMI, obesity, SBP, DBP, blood glucose, TG, and hs-CRP levels. However cardiovascular risk was inversely associated with education level and HDL-C level (
Table 1).
Table 1 Baseline characteristics according to cardiovascular risk
|
Characteristics |
Overall |
Cardiovascular risk |
p-value for trend |
|
Low |
Moderate |
High |
Very high |
|
Number |
545,859 |
306,424 |
199,198 |
32,031 |
8,206 |
|
|
Age (yr) |
37.9 ± 9.2 |
32.1 ± 4.2 |
42.9 ± 6.5 |
56.5 ± 5.0 |
61.6 ± 2.8 |
< 0.001 |
|
< 40 |
358,818 (65.7) |
288,144 (80.3) |
70,674 (19.7) |
- |
- |
|
40–50 |
116,512 (21.3) |
18,280 (15.7) |
95,096 (81.6) |
3,128 (2.7) |
8 (0.0) |
|
50–60 |
52,182 (9.6) |
- |
31,470 (60.3) |
19,004 (36.4) |
1,708 (3.3) |
|
≥ 60 |
18,347 (3.4) |
- |
1,958 (10.7) |
9,899 (54.0) |
6,490 (35.4) |
|
Men (%) |
54.1 |
39.3 |
72.5 |
72.6 |
82.1 |
< 0.001 |
|
Current smoker (%) |
23.7 |
14.3 |
36.7 |
29.8 |
32.4 |
< 0.001 |
|
Alcohol consumption (%) |
|
|
|
|
|
|
|
≥ 10 g/day |
35.3 |
27.5 |
45.8 |
43.0 |
44.5 |
< 0.001 |
|
Regular exercise (%) |
|
|
|
|
|
|
|
≥ 3 times/week |
14.1 |
12.7 |
15.0 |
20.1 |
19.4 |
< 0.001 |
|
High education level (%) |
|
|
|
|
|
|
|
≥ college graduate |
60.2 |
66.8 |
55.7 |
34.7 |
27.6 |
< 0.001 |
|
Married (%) |
56.0 |
59.2 |
64.2 |
67.0 |
70.4 |
< 0.001 |
|
Medication for hypertension (%) |
4.4 |
0.3 |
5.7 |
26.1 |
43.0 |
< 0.001 |
|
Medication for diabetes (%) |
1.4 |
0.1 |
1.4 |
8.4 |
23.8 |
< 0.001 |
|
Medication for dyslipidemia (%) |
1.4 |
0.2 |
2.1 |
7.3 |
8.5 |
< 0.001 |
|
BMI (kg/m2) |
23.3 ± 3.3 |
22.4 ± 3.2 |
24.5 ± 3.1 |
24.9 ± 2.9 |
25.3 ± 2.9 |
< 0.001 |
|
Obesity (%) |
|
|
|
|
|
|
|
≥ 25 kg/m2
|
29.3 |
18.8 |
41.3 |
48.0 |
53.8 |
< 0.001 |
|
SBP (mmHg) |
111.6 ± 13.9 |
107.1 ± 11.7 |
115.8 ± 13.4 |
123.1 ± 15.4 |
132.1 ± 17.6 |
< 0.001 |
|
DBP (mmHg) |
71.8 ± 10.2 |
68.1 ± 8.5 |
75.6 ± 9.9 |
79.9 ± 10.5 |
83.2 ± 10.9 |
< 0.001 |
|
Glucose level (mg/dL) |
94.2 ± 15.7 |
90.7 ± 9.1 |
96.7 ± 17.4 |
105.9 ± 27.4 |
117.2 ± 35.0 |
< 0.001 |
|
Total cholesterol level (mg/dL) |
193.5 ± 34.7 |
184.7 ± 31.1 |
204.3 ± 35.1 |
207.9 ± 38.2 |
206.1 ± 30.7 |
< 0.001 |
|
LDL-C level (mg/dL) |
116.4 ± 31.4 |
108.8 ± 28.5 |
126.0 ± 31.8 |
128.9 ± 34.1 |
125.6 ± 35.1 |
< 0.001 |
|
HDL-C level (mg/dL) |
57.8 ± 14.5 |
60.7 ± 14.8 |
54.2 ± 13.2 |
53.5 ± 13.1 |
52.2 ± 13.2 |
< 0.001 |
|
TG level (mg/dL) |
94 (66–141) |
79 (59–112) |
119 (83–174) |
127 (90–183) |
137 (98–196) |
< 0.001 |
|
hs-CRP level (mg/dL) |
0.04 (0.02–0.09) |
0.04 (0.02–0.08) |
0.05 (0.03–0.11) |
0.07 (0.04–0.13) |
0.08 (0.04–0.17) |
< 0.001 |
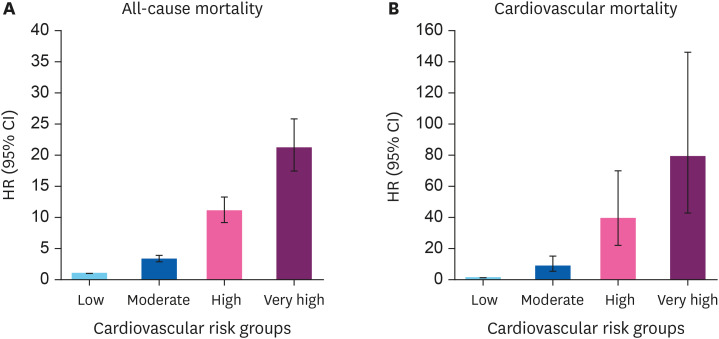
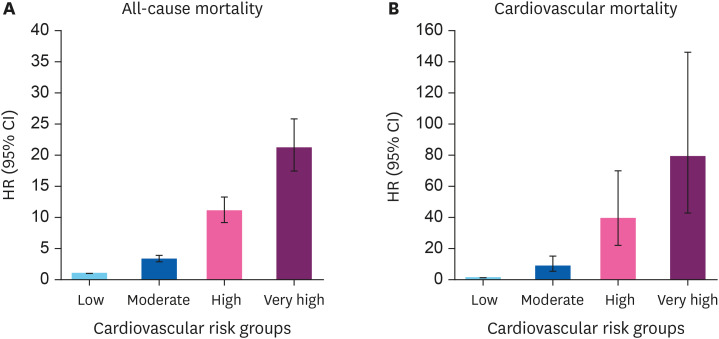
The median follow-up period was 9.07 years and 4,738 overall deaths and 654 cardiovascular deaths occurred in 5,253,627.9 person-years. The 10-year cardiovascular risk is positively associated with all-cause and cardiovascular mortality. The difference in mortality according to the classification of cardiovascular risk was very high. When the low-risk group was set as a reference, in model 1, which was adjusted for the examination center and year of screening examination, the HRs (95% confidence interval [CI]) for overall mortality were 2.93 (2.70–3.18) in the moderate-risk group, 11.88 (10.86–13.00) in the high-risk group, and 26.38 (23.85–29.18) in the very-high-risk group, all of which were statistically significant. In model 2, which was further adjusted for alcohol consumption, education level, marital status, and hs-CRP level, the HRs (95% CI) were 3.36 (2.87–3.95), 11.08 (9.27–13.25), and 21.20 (17.42–25.79) in each group. In cardiovascular deaths, the difference according to risk classification was more pronounced. In model 1, the HRs (95% CI) for cardiovascular mortality were 5.61 (4.24–7.42) in the moderate-risk group, 28.37 (21.22–37.94) in the high-risk group, and 67.68 (49.77–92.04) in the very-high-risk group. In model 2, the HRs (95% CI) were 8.57 (4.95–14.83), 38.95 (21.77–69.69), and 78.81 (42.62–145.71) in each group (
Table 2,
Fig. 2).
Table 2 HRs (95% CIs) for all-cause and cardiovascular mortality according to cardiovascular risk
|
Cardiovascular risk |
PY |
Incident cases |
Incidence density (per 104 PY) (95% CI) |
Multivariable-adjusted HR (95% CI)a
|
|
Model 1b
|
Model 2c
|
|
All-cause mortality |
|
|
|
|
|
|
Low |
2,775,844.8 |
859 |
3.09 (2.89–3.31) |
1.00 (reference) |
1.00 (reference) |
|
Moderate |
2,082,571.4 |
2,000 |
9.60 (9.19–10.03) |
2.93 (2.70–3.18) |
3.36 (2.87–3.95) |
|
High |
311,606.7 |
1,161 |
37.26 (35.18–39.46) |
11.88 (1.86–13.00) |
11.08 (9.27–13.25) |
|
Very high |
83,604.9 |
718 |
85.88 (79.82–92.40) |
26.38 (23.85–29.18) |
21.20 (17.42–25.79) |
|
Cardiovascular mortality |
|
|
|
|
|
|
Low |
2,775,844.8 |
62 |
0.22 (0.17–0.29) |
1.00 (reference) |
1.00 (reference) |
|
Moderate |
2,082,571.4 |
270 |
1.30 (1.15–1.46) |
5.61 (4.24–7.42) |
8.57 (4.95–14.83) |
|
High |
311,606.7 |
193 |
6.19 (5.38–7.13) |
28.37 (21.22–37.94) |
38.95 (21.77–69.69) |
|
Very high |
83,604.9 |
129 |
15.43 (12.98–18.36) |
67.68 (49.77–92.04) |
78.81 (42.62–145.71) |
Fig. 2
HRs (95% CIs) for all-cause and cardiovascular mortality according to health risk appraisal. (A) All-cause mortality. (B) Cardiovascular mortality.
HR: hazard ratio; CI: confidence interval.
Subgroup analyses were conducted based on age and sex. In the group aged < 40 years, there were no subjects classified in the high- and very high-risk groups, and no subjects in the low-risk group were in their 50s and 60s. In all age groups, the HRs of all-cause mortality and cardiovascular mortality tended to be higher in the high-risk group. This association was most clearly observed in the 40s group; however, it was not statistically significant in the 60s group. Moreover, as a result of the subgroup analysis by sex, the HRs of mortality according to the increase in risk group were clearly observed for both men and women (
Table 3).
Table 3 Subgroup analysis for all-cause and cardiovascular mortality by age and sex
|
Variables |
Low |
Moderate |
High |
Very high |
|
All-cause mortality |
|
|
|
|
|
Age |
|
|
|
|
|
|
< 40 |
1.00 (reference) |
2.21 (1.73–2.81) |
- |
- |
|
|
40–50 |
1.00 (reference) |
2.19 (1.42–3.37) |
4.51 (2.62–7.74) |
27.79 (3.71–208.26) |
|
|
50–60 |
- |
1.00 (reference) |
2.02 (1.66–2.47) |
3.13 (2.25–4.35) |
|
|
≥ 60 |
- |
1.00 (reference) |
1.34 (0.79–2.28) |
1.93 (1.13–3.29) |
|
Sex |
|
|
|
|
|
|
Male |
1.00 (reference) |
3.80 (2.97–4.85) |
13.07 (10.02–17.03) |
26.02 (19.70–34.38) |
|
|
Female |
1.00 (reference) |
3.12 (2.46–3.97) |
8.63 (6.44–11.57) |
11.51 (7.64–17.34) |
|
Cardiovascular mortality |
|
|
|
|
|
Age |
|
|
|
|
|
|
< 40 |
1.00 (reference) |
7.09 (3.39–14.79) |
- |
- |
|
|
40–50 |
1.00 (reference) |
4.87 (1.17–20.28) |
17.11 (3.40–86.12) |
-a
|
|
|
50–60 |
- |
1.00 (reference) |
4.70 (2.68–8.24) |
4.05 (1.47–11.15) |
|
|
≥ 60 |
- |
1.00 (reference) |
2.29 (0.31–17.25) |
5.46 (0.74–40.28) |
|
Sex |
|
|
|
|
|
|
Male |
1.00 (reference) |
9.66 (4.30–21.69) |
44.72 (19.05–104.95) |
91.37 (37.85–220.57) |
|
|
Female |
1.00 (reference) |
5.99 (2.64–13.56) |
24.24 (10.05–58.44) |
51.67 (18.86–141.58) |
DISCUSSION
In this large cohort study, we found that the higher the 10-year cardiovascular risk of the general health checkup, the higher the actual overall mortality and CVD mortality. The association between 10-year cardiovascular risk and death remained statistically significant even after confounding variables were adjusted and stratified analysis for age and sex was performed. It is meaningful that the results of our study, which linked the death data of national statistics, materialized the degree of risk that was abstract. The results showed that cardiovascular risk was associated not only with cardiovascular mortality but also with all-cause mortality. This can be interpreted that risk factors used to calculate cardiovascular risk, such as medical history of diabetes and hypertension, are related to all-cause mortality referring to other studies.
12,13
There are previous studies on cardiovascular mortality. According to a study, cardiovascular mortality decreased from the 1980s to the 2010s in Korea, and the trend was analyzed by dividing CVD into ischemic heart disease and cerebrovascular disease.
14 Another study compared which of hypertension, diabetes and dyslipidemia contributed more to mortality from stroke, coronary heart disease, and pulmonary heart disease in China.
15 Another study pointed out that predicting overall cardiovascular risk using cardiovascular mortality in accordance with the prevention guidelines of the European Society of Cardiology may underestimate the actual risk. Therefore, it is suggested that the risk of developing CVD and cardiovascular death should be predicted differently.
16
Among the existing Korean studies on the risk of CVD, there was no study that analyzed the actual mortality according to the risk. Previous studies have focused not on the relationship between CVD risk and mortality, but on evaluating prediction of CVD incidence according to risk assessment or comparing different cardiovascular risk assessment models.
4,5,6 A recent study introduced the characteristics and usage status of the models that are actually widely used among various domestic and foreign CVD prediction models.
4 A past study developed an estimation model for ischemic heart disease risk in Koreans using prospective research data followed for 10 years and evaluated its validity.
5 In addition, a study was to apply an estimation model for ischemic heart disease risk in Koreans of the previous reference to one manufacturing worker and compare it with other risk assessment methods.
6
This study had several limitations. First, it is a limitation of the general health examination itself. There is insufficient information on various variables related to mortality. For example, information on underlying disease and current medications is limited, and the number of examination items is small. However, from the point of view of generalization of research conclusions, which is the purpose of all studies, we think that the study of mortality comparison using general health examinations is meaningful enough. Therefore, we believe that this study is a good attempt to directly show the overall risk of death and death from CVDs using the variables of ordinary health examinations of the general population and workers. Second, in this study, participants were not classified into cardiovascular risk according to the integrated risk classification criteria of KOSHA GUIDE (H-200-2018). We used the 10-year cardiovascular risk of the general health checkup that can be applied to all workers using data from the Korean workers’ health examination. As described above, we had no choice but to use this evaluation method because it can be applied to as many workers and people as possible when the risk of death can be predicted using the results of general examinations. In the future, study using other risk classification methods including the integrated risk classification of KOSHA GUIDE (H-200-2018) is needed. Lastly, since variables such as hypertension and diabetes were already included in 10-year cardiovascular risk calculation as risk factors, the use of adjusted variables in the analysis stage of our study was limited. However, the conclusions of our study could be more clearly demonstrated through a stratified analysis using age and sex variables, which are important for CVD and mortality.
To the best of our knowledge, this is the first mortality study of 10-year cardiovascular risk from routine health checkup linked to a large cohort study. Through this study, we found that the risk classification of the general health examination was actually associated with a very large increase in the risk of mortality. And it is the fact that common diseases such as hypertension and diabetes, which are subjects of general health examination, are very helpful in predicting mortality.
CONCLUSION
This study confirmed that the risk of death increases according to the 10-year cardiovascular risk of the general health checkup and the level of risk was very high. This tendency was observed even when several confounding variables were adjusted and stratified according to age and sex. Since there have been no previous studies on death according to cardiovascular risk, this study can be expected to have an effect that can alert workers by directly showing the risk of death using general health examination variables.
Abbreviations
glomerular filtration rate
high-density lipoprotein cholesterol
high sensitivity C-reactive protein
International Classification of Diseases, 10th Revision
Korea Occupational Safety and Health Agency
low-density lipoprotein cholesterol
NOTES
-
Competing interests: The authors declare that they have no competing interests.
-
Author contributions:
Conceptualization: Lee W.
Investigation: Jeong Y, Lee W, Lee Y, Mun E, Kim D.
Methodology: Jeong Y, Lee W, Lee Y, Seo E, Lee J.
Supervision: Jeong J.
Writing - original draft: Jeong Y.
Writing - review & editing: Lee W.
REFERENCES
REFERENCES
- 1. Korea National Statistical Office. Annual report on the cause of death statistics in 2020. Updated 2021]. Accessed September 28, 2021].
http://www.kostat.go.kr/portal/korea/kor_nw/1/6/2/index.board
.
- 2. Korea Occupational Safety and Health Agency. Occupational accidents and diseases statistics. Accessed December 31, 2021].
https://kosha.or.kr/kosha/data/industrialAccidentStatus.do
.
- 3. Korea Occupational Safety and Health Agency. Risk assessment for the prevention of cardio-cerebrovascular disease at workplace (KOSHA Code H-200-2018). Updated 2018]. Accessed December 14, 2018].
https://www.kosha.or.kr/kosha/data/guidanceH.do
.
- 4. Yun JM, Yoo TG, Oh SW, Cho BL, Kim E, Hwang I. Prediction of cardiovascular disease in Korean population: based on health risk appraisal of national health screening program. J Korean Med Assoc 2017;60(9):746–752.ArticlePDF
- 5. Jee SH, Song JW, Cho HK, Kim SY, Jang YS, Kim JH. Development of the individualized health risk appraisal model of ischemic heart disease risk in Korea. J Korean Soc Lipidol Atheroscler 2004;14(2):153–168.
- 6. Yi KJ, Heo HT, Kim DW, Kim IA, Kim SY, Rho JR, et al. A comparison of KOSHA’s cardiovascular disease risk assessment and the predicted 10-year risk of cardiovascular disease developed by Jee for a male workers at a wallpaper and floor covering manufacturer. Korean J Occup Environ Med 2009;21(2):174–183.ArticlePDF
- 7. D’Agostino RB Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation 2008;117(6):743–753. 18212285.ArticlePubMed
- 8. Ahn KA, Yun JE, Cho ER, Nam CM, Jang Y, Jee SH. Framingham equation model overestimates risk of ischemic heart disease in Korean men and women. Korean J Epidemiol 2006;28(2):162–170.
- 9. Jung KJ, Jang Y, Oh DJ, Oh BH, Lee SH, Park SW, et al. The ACC/AHA 2013 pooled cohort equations compared to a Korean Risk Prediction Model for atherosclerotic cardiovascular disease. Atherosclerosis 2015;242(1):367–375. 26255683.ArticlePubMed
- 10. Goff DC Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014;129(25):Suppl 2. S49–S73. 24222018.PubMed
- 11. Li Y, Zhong X, Cheng G, Zhao C, Zhang L, Hong Y, et al. Hs-CRP and all-cause, cardiovascular, and cancer mortality risk: a meta-analysis. Atherosclerosis 2017;259:75–82. 28327451.ArticlePubMed
- 12. Salehidoost R, Mansouri A, Amini M, Aminorroaya Yamini S, Aminorroaya A. Diabetes and all-cause mortality, a 18-year follow-up study. Sci Rep 2020;10(1):3183. 32081921.ArticlePubMedPMCPDF
- 13. Li C, Chen Y, Zheng Q, Wu W, Chen Z, Song L, et al. Relationship between systolic blood pressure and all-cause mortality: a prospective study in a cohort of Chinese adults. BMC Public Health 2018;18(1):107. 29304766.ArticlePubMedPMCPDF
- 14. Kim HC. Epidemiology of cardiovascular disease and its risk factors in Korea. Glob Health Med 2021;3(3):134–141. 34250288.ArticlePubMedPMC
- 15. Rehman S, Rehman E, Mumtaz A, Jianglin Z. Cardiovascular disease mortality and potential risk factor in china: a multi-dimensional assessment by a grey relational approach. Int J Public Health 2022;67:1604599. 35574277.ArticlePubMedPMC
- 16. Jørstad HT, Colkesen EB, Boekholdt SM, Tijssen JG, Wareham NJ, Khaw KT, et al. Estimated 10-year cardiovascular mortality seriously underestimates overall cardiovascular risk. Heart 2016;102(1):63–68. 26261158.ArticlePubMed
 , Yesung Lee
, Yesung Lee , Eunchan Mun
, Eunchan Mun , Eunhye Seo
, Eunhye Seo , Daehoon Kim
, Daehoon Kim , Jaehong Lee
, Jaehong Lee , Jinsook Jeong
, Jinsook Jeong , Woncheol Lee
, Woncheol Lee


 KSOEM
KSOEM

 Cite
Cite

