Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 34; 2022 > Article
- Original Article The effect of long working hours on developing type 2 diabetes in adults with prediabetes: The Kangbuk Samsung Cohort Study
-
Eunhye Seo
 , Yesung Lee
, Yesung Lee , Eunchan Mun
, Eunchan Mun , Dae Hoon Kim
, Dae Hoon Kim , Youshik Jeong
, Youshik Jeong , Jaehong Lee
, Jaehong Lee , Jinsook Jeong
, Jinsook Jeong , Woncheol Lee
, Woncheol Lee
-
Annals of Occupational and Environmental Medicine 2022;34:e4.
DOI: https://doi.org/10.35371/aoem.2022.34.e4
Published online: March 14, 2022
Department of Occupational and Environmental Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- Correspondence: Woncheol Lee. Department of Occupational and Environmental Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, 29 Saemunan-ro, Jongno-gu, Seoul 03181, Korea. doctor.oem@gmail.com
Copyright © 2022 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background Long working hours are known to account for approximately one-third of the total expected work-related diseases, and much interest and research on long working hours have recently been conducted. Additionally, as the prevalence of prediabetes and the high-risk group for diabetes are increasing worldwide, interest in prediabetes is also rising. However, few studies have addressed the development of type 2 diabetes and long working hours in prediabetes. Therefore, the aim of this longitudinal study was to evaluate the relationship between long working hours and the development of diabetes in prediabetes.
-
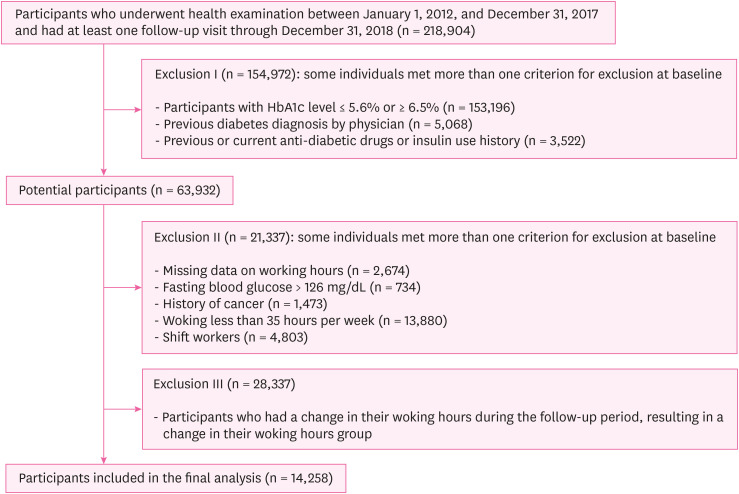
Methods We included 14,258 prediabetes participants with hemoglobinA1c (HbA1c) level of 5.7 to 6.4 in the Kangbuk Samsung Cohort Study. According to a self-reported questionnaire, we evaluated weekly working hours, which were categorized into 35–40, 41–52, and > 52 hours. Development of diabetes was defined as an HbA1c level ≥ 6.5%. Hazard ratios (HRs) and 95% confidence intervals (CIs) for the development of diabetes were estimated using Cox proportional hazards analyses with weekly working 35–40 hours as the reference.
-
Results During a median follow-up of 3.0 years, 776 participants developed diabetes (incidence density, 1.66 per 100 person-years). Multivariable-adjusted HRs of development of diabetes for weekly working > 52 hours compared with working 35–40 hours were 2.00 (95% CI: 1.50–2.67). In subgroup analyses by age (< 40 years old, ≥ 40 years old), sex (men, women), and household income (< 6 million KRW, ≥ 6 million KRW), consistent and significant positive associations were observed in all groups.
-
Conclusions In our large-scale longitudinal study, long working hours increases the risk of developing diabetes in prediabetes patients.
BACKGROUND
METHODS
RESULTS
Characteristics of participants with prediabetes at baseline by weekly working hours
Development of diabetes in prediabetes according to weekly working hours
Hazard ratios (95% CI) for development of diabetes in prediabetes by weekly working hours in clinically relevant subgroups
DISCUSSION
CONCLUSIONS
Abbreviations
BMI
CI
HbA1c
HOMA-IR
HR
hsCRP
-
Funding: This research has been supported by the Korean Society of Occupational and Environmental Medicine (KSOEM) to assist a small research group.
-
Competing interests: The authors declare that they have no competing interests.
-
Author contributions:
NOTES
SUPPLEMENTARY MATERIAL
Supplementary Table 1
- 1. Tabák AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M. Prediabetes: a high-risk state for diabetes development. Lancet 2012;379(9833):2279–2290. 22683128.ArticlePubMedPMC
- 2. Hostalek U. Global epidemiology of prediabetes - present and future perspectives. Clin Diabetes Endocrinol 2019;5(1):5. 31086677.ArticlePubMedPMCPDF
- 3. Echouffo-Tcheugui JB, Narayan KM, Weisman D, Golden SH, Jaar BG. Association between prediabetes and risk of chronic kidney disease: a systematic review and meta-analysis. Diabet Med 2016;33(12):1615–1624. 26997583.ArticlePubMedPDF
- 4. Diabetes Prevention Program Research Group. The prevalence of retinopathy in impaired glucose tolerance and recent-onset diabetes in the Diabetes Prevention Program. Diabet Med 2007;24(2):137–144. 17257275.ArticlePubMedPMC
- 5. Lee CC, Perkins BA, Kayaniyil S, Harris SB, Retnakaran R, Gerstein HC, et al. Peripheral neuropathy and nerve dysfunction in individuals at high risk for type 2 diabetes: the PROMISE cohort. Diabetes Care 2015;38(5):793–800. 25665810.ArticlePubMedPDF
- 6. Huang Y, Cai X, Mai W, Li M, Hu Y. Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ 2016;355:i5953. 27881363.ArticlePubMedPMC
- 7. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346(6):393–403. 11832527.ArticlePubMedPMC
- 8. Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care 1997;20(4):537–544. 9096977.ArticlePubMedPDF
- 9. Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V, et al. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia 2006;49(2):289–297. 16391903.ArticlePubMedPDF
- 10. Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001;344(18):1343–1350. 11333990.ArticlePubMed
- 11. Organisation for Economic Cooperation and Development. Hours worked. Updated 2020]. Accessed November 19, 2021]. https://data.oecd.org/emp/hours-worked.htm .
- 12. Li W, Ruan W, Chen Z, Yi G, Lu Z, Wang D. A meta-analysis of observational studies including dose-response relationship between long working hours and risk of obesity. Rev Endocr Metab Disord 2021;22(4):837–845. 33713311.ArticlePubMedPDF
- 13. Nakanishi N, Yoshida H, Nagano K, Kawashimo H, Nakamura K, Tatara K. Long working hours and risk for hypertension in Japanese male white collar workers. J Epidemiol Community Health 2001;55(5):316–322. 11297649.ArticlePubMedPMC
- 14. Kivimäki M, Jokela M, Nyberg ST, Singh-Manoux A, Fransson EI, Alfredsson L, et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet 2015;386(10005):1739–1746. 26298822.ArticlePubMed
- 15. Lee Y, Mun E, Park S, Lee W. Long working hours are associated with a higher risk of non-alcoholic fatty liver disease: a large population-based Korean cohort study. PLoS One 2021;16(7):e0255118. 34297733.ArticlePubMedPMC
- 16. Nakashima M, Morikawa Y, Sakurai M, Nakamura K, Miura K, Ishizaki M, et al. Association between long working hours and sleep problems in white-collar workers. J Sleep Res 2011;20(1 Pt 1):110–116. 20561174.ArticlePubMed
- 17. Dembe AE, Erickson JB, Delbos RG, Banks SM. The impact of overtime and long work hours on occupational injuries and illnesses: new evidence from the United States. Occup Environ Med 2005;62(9):588–597. 16109814.ArticlePubMedPMC
- 18. Lee HE, Kim I, Kim HR, Kawachi I. Association of long working hours with accidents and suicide mortality in Korea. Scand J Work Environ Health 2020;46(5):480–487. 32096547.ArticlePubMedPMC
- 19. American Diabetes Association. Standards of medical care in diabetes--2013. Diabetes Care 2013;36(Suppl 1):S11–S66. 23264422.ArticlePubMedPMCPDF
- 20. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28(7):412–419. 3899825.ArticlePubMedPDF
- 21. Ratziu V, Bellentani S, Cortez-Pinto H, Day C, Marchesini G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J Hepatol 2010;53(2):372–384. 20494470.ArticlePubMed
- 22. Bellentani S, Saccoccio G, Masutti F, Crocè LS, Brandi G, Sasso F, et al. Prevalence of and risk factors for hepatic steatosis in Northern Italy. Ann Intern Med 2000;132(2):112–117. 10644271.ArticlePubMed
- 23. Okechukwu CA. Long working hours are linked to risky alcohol consumption. BMJ 2015;350:g7800. 25587066.ArticlePubMed
- 24. Kim BG, Pang DD, Park YJ, Lee JI, Kim HR, Myong JP, et al. Heavy smoking rate trends and related factors in Korean occupational groups: analysis of KNHANES 2007-2012 data. BMJ Open 2015;5(11):e008229.ArticlePubMedPMC
- 25. Akter S, Goto A, Mizoue T. Smoking and the risk of type 2 diabetes in Japan: a systematic review and meta-analysis. J Epidemiol 2017;27(12):553–561. 28716381.ArticlePubMedPMC
- 26. Polsky S, Akturk HK. Alcohol consumption, diabetes risk, and cardiovascular disease within diabetes. Curr Diab Rep 2017;17(12):136. 29103170.ArticlePubMedPDF
- 27. Evert AB, Dennison M, Gardner CD, Garvey WT, Lau KH, MacLeod J, et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care 2019;42(5):731–754. 31000505.ArticlePubMedPMCPDF
- 28. Richter J, Herzog N, Janka S, Baumann T, Kistenmacher A, Oltmanns KM. Twice as high diet-induced thermogenesis after breakfast vs dinner on high-calorie as well as low-calorie meals. J Clin Endocrinol Metab 2020;105(3):e211.ArticlePDF
- 29. Mekary RA, Giovannucci E, Willett WC, van Dam RM, Hu FB. Eating patterns and type 2 diabetes risk in men: breakfast omission, eating frequency, and snacking. Am J Clin Nutr 2012;95(5):1182–1189. 22456660.ArticlePubMedPMC
- 30. Sakai R, Hashimoto Y, Ushigome E, Miki A, Okamura T, Matsugasumi M, et al. Late-night-dinner is associated with poor glycemic control in people with type 2 diabetes: the KAMOGAWA-DM cohort study. Endocr J 2018;65(4):395–402. 29375081.ArticlePubMed
- 31. Lee K, Suh C, Kim JE, Park JO. The impact of long working hours on psychosocial stress response among white-collar workers. Ind Health 2017;55(1):46–53. 27498571.ArticlePubMed
- 32. Hackett RA, Steptoe A. Type 2 diabetes mellitus and psychological stress - a modifiable risk factor. Nat Rev Endocrinol 2017;13(9):547–560. 28664919.ArticlePubMedPDF
- 33. Luc K, Schramm-Luc A, Guzik TJ, Mikolajczyk TP. Oxidative stress and inflammatory markers in prediabetes and diabetes. J Physiol Pharmacol 2019;70(6):809–824.
- 34. Korean Diabetes Association. Treatment Guideline for Diabetes. 6th ed. Seoul: Korean Diabetes Association; 2019.
- 35. Jung CH, Son JW, Kang S, Kim WJ, Kim HS, Kim HS, et al. Diabetes fact sheets in Korea, 2020: an appraisal of current status. Diabetes Metab J 2021;45(1):1–10. 33434426.ArticlePubMedPMCPDF
- 36. de Souza Santos R, Härter Griep R, Mendes da Fonseca MJ, Chor D, Santos IS, Melo EC. Combined use of job stress models and the incidence of glycemic alterations (prediabetes and diabetes): results from ELSA-Brasil Study. Int J Environ Res Public Health 2020;17(5):1539.ArticlePubMedPMC
- 37. Lee J, Kim HR, Jang TW, Lee DW, Jeong C, Kang MY. Poor glycemic control in workers with diabetes mellitus in relation to long working hours: a cross-sectional study. Ind Health 2020;58(5):451–459. 32536633.ArticlePubMedPMC
- 38. Kivimaki M, Virtanen M, Kawachi I, Nyberg ST, Alfredsson L, Batty GD, et al. Long working hours, socioeconomic status, and the risk of incident type 2 diabetes: a meta-analysis of published and unpublished data from 222 120 individuals. Lancet Diabetes Endocrinol 2015;3(1):27–34. 25262544.ArticlePubMedPMC
- 39. Kuwahara K, Miyamoto T, Yamamoto S, Honda T, Nakagawa T, Mizoue T, et al. Patterns of changes in overtime working hours over 3\xe2\x80\xafyears and the risk for progression to type 2 diabetes in adults with pre-diabetes. Prev Med 2019;121:18–23. 30742872.PubMed
- 40. Gan Y, Yang C, Tong X, Sun H, Cong Y, Yin X, et al. Shift work and diabetes mellitus: a meta-analysis of observational studies. Occup Environ Med 2015;72(1):72–78. 25030030.ArticlePubMed
- 41. Bannai A, Yoshioka E, Saijo Y, Sasaki S, Kishi R, Tamakoshi A. The risk of developing diabetes in association with long working hours differs by shift work schedules. J Epidemiol 2016;26(9):481–487. 27001115.ArticlePubMedPMC
- 42. Rooney MR, Rawlings AM, Pankow JS, Echouffo Tcheugui JB, Coresh J, Sharrett AR, et al. Risk of progression to diabetes among older adults with prediabetes. JAMA Intern Med 2021;181(4):511–519. 33555311.ArticlePubMedPMC
- 43. Souza CF, Gross JL, Gerchman F, Leitão CB. Prediabetes: diagnosis, evaluation of chronic complications, and treatment. Arq Bras Endocrinol Metabol 2012;56(5):275–284. 22911279.PubMed
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Social determinants of health and type 2 diabetes in Asia
Kyunghun Sung, Seung‐Hwan Lee
Journal of Diabetes Investigation.2025; 16(6): 971. CrossRef - Risk factors for progression to type 2 diabetes in prediabetes: a systematic review and meta-analysis
Shengying Hu, Wenting Ji, Yizhu Zhang, Wendi Zhu, Hongyu Sun, Yumei Sun
BMC Public Health.2025;[Epub] CrossRef - Preventable Cancers Caused by Infection in Korea From 2015 to 2030
Sungji Moon, Jeoungbin Choi, Soseul Sung, Youjin Hong, Kwang-Pil Ko, Jung Eun Lee, Inah Kim, Seungho Ryu, Sun Ha Jee, Guen Hui Kim, Sun Young Yang, Aesun Shin, Sun-Seog Kweon, Jeongseon Kim, Jieun Jang, Sangjun Lee, Kyungsik Kim, Woojin Lim, Yoon-Jung Cho
Journal of Korean Medical Science.2025;[Epub] CrossRef - Low Vision Rehabilitation and Eye Exercises: A Comprehensive Guide to Tertiary Prevention of Diabetic Retinopathy
Tibor Rák, Andrea Kovács-Valasek, Etelka Pöstyéni, Róbert Gábriel, Adrienne Csutak
Life.2025; 15(6): 857. CrossRef - Work stress trends in Germany: stable qualitative work overload but rising quantitative work overload across socio-demographic groups in a repeated cross-sectional study
Johannes Beller, Julia Graßhoff, Batoul Safieddine, Jelena Epping, Siegfried Geyer
BMC Public Health.2025;[Epub] CrossRef - Association between long working hours and diet quality and patterns: A latent profile analysis of a nationally representative sample of Korean workers
Seong-Uk Baek, Jong-Uk Won, Yu-Min Lee, Jin-Ha Yoon
Preventive Medicine.2024; 180: 107890. CrossRef - Working Hours, Shift, and Remote Work by Industry and Occupation in U.S. Full-time Workers
Guang X. Chen
Workplace Health & Safety.2024; 72(9): 392. CrossRef - The impact of long working hours on daily sodium intake
Kyungho Ju, Yangwoo Kim, Seung Hee Woo, Juhyeong Kim, Inah Kim, Jaechul Song, Soo-Jin Lee, Jeehee Min
Annals of Occupational and Environmental Medicine.2024;[Epub] CrossRef - Investigating medication adherence among Taiwanese patient with hypertension, hyperlipidemia, and diabetes: A pilot study using the Chinese version of a Two-Part Medication Nonadherence Scale and the NHI MediCloud system
Ya-Wen Lin, Pei-Chun Chen, Che-Huei Lin, Ming-Hung Lin, Fadwa Alhalaiqa
PLOS ONE.2024; 19(7): e0304442. CrossRef - Relationship between Marriage and Prediabetes among Healthcare Workers: Mediating Effect of Triglycerides
Yong-Hsin Chen, Jia-June Lin, Hsiu-Mei Tang, Ching-Wen Yang, Gwo-Ping Jong, Yi-Sun Yang
Medicina.2024; 60(9): 1418. CrossRef - Association between long working hours and metabolic dysfunction–associated steatotic liver disease: a nationwide population-based study in Korea
S.-U. Baek, J.-U. Won, Y.-M. Lee, J.-H. Yoon
Public Health.2024; 232: 188. CrossRef - Working hours and the onset of suicidal ideation and depressive symptoms: A 10-year nationwide longitudinal study in South Korea (2012–2022)
Seong-Uk Baek, Min-Seok Kim, Myeong-Hun Lim, Taeyeon Kim, Jong-Uk Won, Jin-Ha Yoon
Psychiatry Research.2023; 326: 115344. CrossRef - Association between long working hours and physical inactivity in middle-aged and older adults: a Korean longitudinal study (2006–2020)
Seong-Uk Baek, Won-Tae Lee, Min-Seok Kim, Myeong-Hun Lim, Jin-Ha Yoon, Jong-Uk Won
Journal of Epidemiology and Community Health.2023; 77(6): 355. CrossRef - The Korea Cohort Consortium: The Future of Pooling Cohort Studies
Sangjun Lee, Kwang-Pil Ko, Jung Eun Lee, Inah Kim, Sun Ha Jee, Aesun Shin, Sun-Seog Kweon, Min-Ho Shin, Sangmin Park, Seungho Ryu, Sun Young Yang, Seung Ho Choi, Jeongseon Kim, Sang-Wook Yi, Daehee Kang, Keun-Young Yoo, Sue K. Park
Journal of Preventive Medicine and Public Health.2022; 55(5): 464. CrossRef
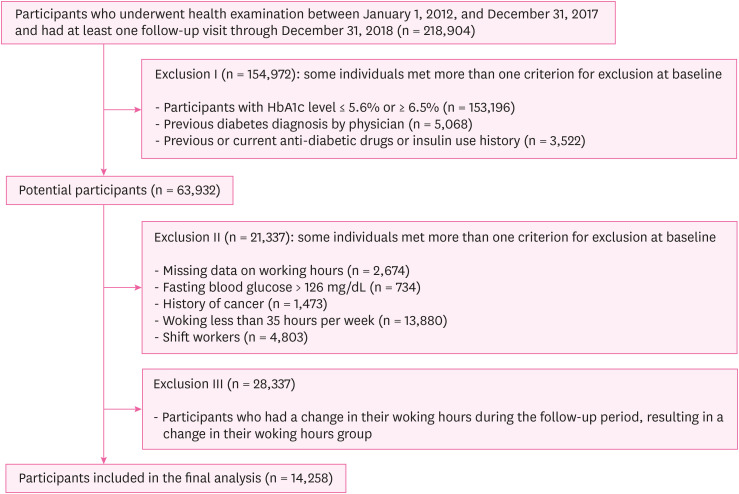
Fig. 1
| Characteristics | Overall | Weekly working hours | |||
|---|---|---|---|---|---|
| 35–40 | 41–52 | > 52 | |||
| Number | 14,258 | 5,460 (38.3) | 6,960 (48.8) | 1,838 (12.9) | |
| Age (years) | 40.9 ± 8.3 | 43.6 ± 8.7 | 38.9 ± 7.4 | 40.1 ± 8.2 | < 0.001 |
| Men | 10,075 (70.7) | 2,792 (51.1) | 5,738 (82.4) | 1,545 (84.1) | < 0.001 |
| Current-smoker | 3,404 (23.9) | 941 (17.2) | 1,836 (26.4) | 627 (34.1) | < 0.001 |
| Heavy alcohol drinkinga | 2,299 (16.1) | 845 (15.5) | 1,071 (15.4) | 383 (20.8) | 0.002 |
| Regular exerciseb | 1,775 (12.5) | 795 (14.6) | 791 (11.4) | 189 (10.3) | < 0.001 |
| Marital status (married) | 12,155 (85.3) | 4,934 (90.4) | 5,708 (82.0) | 1,513 (82.3) | < 0.001 |
| High education levelc | 12,284 (86.2) | 4,349 (79.7) | 6,325 (90.9) | 1,610 (87.6) | < 0.001 |
| High household incomed | 5,473 (38.4) | 2,211 (40.5) | 2,521 (36.2) | 741 (40.3) | 0.001 |
| Medication of hypertension | 1,060 (7.4) | 524 (9.6) | 392 (5.6) | 144 (7.8) | < 0.001 |
| Medication of dyslipidemia | 624 (4.4) | 288 (5.3) | 248 (3.6) | 88 (4.8) | 0.011 |
| Obesitye | 5,675 (39.8) | 1,827 (33.5) | 2,961 (42.5) | 887 (48.3) | < 0.001 |
| Fasting glucose (mg/dL) | 97.4 ± 9.2 | 97.0 ± 9.6 | 97.6 ± 9.0 | 98.2 ± 9.2 | < 0.001 |
| HbA1c (%) | 5.83 ± 0.16 | 5.84 ± 0.16 | 5.83 ± 0.15 | 5.84 ± 0.17 | 0.191 |
| HOMA-IRf* | 1.47 (0.95–2.21) | 1.35 (0.88–2.01) | 1.54 (1.00–2.31) | 1.58 (1.00–2.37) | < 0.001 |
| hsCRP (mg/L)* | 0.05 (0.03–0.11) | 0.05 (0.03–0.10) | 0.06 (0.03–0.11) | 0.06 (0.03–0.13) | 0.003 |
| Weekly working hours | PY | Incident cases | Incidence density (per 100 PY) (95% CI) | Multivariable-adjusted HR (95% CI) | ||
|---|---|---|---|---|---|---|
| Model 1a | Model 2b | Model 3c | ||||
| 35–40 | 18,302.3 | 229 | 1.25 (1.10–1.42) | 1.00 | 1.00 | 1.00 |
| 41–52 | 23,171.5 | 389 | 1.68 (1.52–1.85) | 1.22 (1.02–1.46) | 1.23 (0.99–1.53) | 1.28 (1.00–1.64) |
| > 52 | 5,151.4 | 158 | 3.07 (2.62–3.58) | 2.33 (1.88–2.88) | 2.03 (1.57–2.63) | 2.00 (1.50–2.67) |
| < 0.001 | < 0.001 | < 0.001 | ||||
| Subgroup | PY | Incident cases | Incidence density (per 100 PY) (95% CI) | Weekly working hours | |||||
|---|---|---|---|---|---|---|---|---|---|
| 35–40 | 41–52 | > 52 | |||||||
| Age (years) | 0.527 | ||||||||
| < 40 (n = 6,835) | 23,621.0 | 294 | 1.24 (1.11–1.40) | 1.00 | 1.20 (0.78–1.83) | 1.75 (1.06–2.89) | 0.023 | ||
| ≥ 40 (n = 7,423) | 23,004.2 | 482 | 2.10 (1.92–2.29) | 1.00 | 1.16 (0.86–1.57) | 2.16 (1.51–3.08) | < 0.001 | ||
| Sex | 0.527 | ||||||||
| Men (n = 10,075) | 32,603.5 | 682 | 2.09 (1.94–2.25) | 1.00 | 1.23 (0.94–1.60) | 1.89 (1.39–2.57) | < 0.001 | ||
| Women (n = 4,183) | 14,021.8 | 94 | 0.67 (0.55–0.82) | 1.00 | 1.89 (0.98–3.64) | 2.94 (1.16–7.46) | 0.007 | ||
| Household income | 0.731 | ||||||||
| < 6 million KRW (n = 6,598) | 22,476.8 | 384 | 1.71 (1.55–1.89) | 1.00 | 1.30 (0.95–1.78) | 2.28 (1.55–3.34) | < 0.001 | ||
| ≥ 6 million KRW (n = 5,473) | 17,136.3 | 291 | 1.70 (1.51–1.90) | 1.00 | 1.29 (0.88–1.90) | 1.89 (1.22–2.94) | 0.004 | ||
Data are expressed as mean ± standard deviation, median (interquartile range) or percentage.
HbA1c: hemoglobinA1c; HOMA-IR: homeostasis model assessment of insulin resistance; hsCRP: high-sensitivity C-reactive protein.
aWomen ≥ 20 g/day, men ≥ 30 g/day; b ≥ 3 times/week; c ≥ College graduate; dTotal monthly income ≥ 6 million KRW; ebody mass index (≥ 25 kg/m2); fHomeostasis model assessment of insulin resistance.
PY: person-years; HR: hazard ratio; CI: confidence interval.
aModel 1: age, sex adjusted; bModel 2: model 1 plus adjusted for alcohol consumption, smoking, regular exercise, medication for hypertension or dyslipidemia, body mass index, homeostasis model assessment of insulin resistance, and high-sensitivity C-reactive protein; cModel 3: model 2 plus adjusted for education, marital status, and household income.
CI: confidence interval; PY: person-years.
Estimated from Cox proportional hazard models adjusted for age, sex, alcohol consumption, smoking, regular exercise, medication for hypertension or dyslipidemia, body mass index, homeostasis model assessment of insulin resistance, high-sensitivity C-reactive protein, education, marital status, and household income.
 KSOEM
KSOEM

 Cite
Cite

