Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 34; 2022 > Article
- Original Article The effect of blood cadmium levels on hypertension in male firefighters in a metropolitan city
-
Ye-eun Jeon1
 , Min Ji Kim1
, Min Ji Kim1 , Insung Chung1,2
, Insung Chung1,2 , Jea Chul Ha1,2
, Jea Chul Ha1,2
-
Annals of Occupational and Environmental Medicine 2022;34:e37.
DOI: https://doi.org/10.35371/aoem.2022.34.e37
Published online: November 8, 2022
1Department of Occupational and Environment Medicine, Keimyung University Dongsan Medical Center, Daegu, Korea.
2Department of Occupational and Environment Medicine, Keimyung University School of Medicine, Daegu, Korea.
- Correspondence: Jea Chul Ha. Department of Occupational and Environmental Medicine, Keimyung University School of Medicine, 1035 Dalgubeol-daero, Dalseo-gu, Daegu 42601, Korea. imitate2017@gmail.com
Copyright © 2022 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background This study investigated the effect of dispatch frequency on blood cadmium levels and the effect of blood cadmium levels on hypertension in male firefighters in a metropolitan city.
-
Methods We conducted a retrospective longitudinal study of male firefighters who completed the regular health checkups, including a health examination survey and blood cadmium measurements. We followed them for 3 years. To investigate the effect of dispatch frequency on blood cadmium levels and the effect of blood cadmium levels on hypertension, we estimated the short-term (model 1) and long-term (model 2) effects of exposure and hypothesized a reversed causal pathway model (model 3) for sensitivity analysis. Sequential conditional mean models were fitted using generalized estimating equations, and the odds ratios (ORs) and the respective 95% confidence intervals (CIs) were calculated for hypertension for log-transformed (base 2) blood cadmium levels and quartiles.
-
Results Using the lowest category of dispatch frequency as a reference, we observed that the highest category showed an increase in blood cadmium levels of 1.879 (95% CI: 0.673, 3.086) μg/dL and 0.708 (95% CI: 0.023, 1.394) μg/dL in models 2 and 3, respectively. In addition, we observed that doubling the blood cadmium level significantly increased the odds of hypertension in model 1 (OR: 1.772; 95% CI: 1.046, 3.003) and model 3 (OR: 4.288; 95% CI: 1.110, 16.554). Using the lowest quartile of blood cadmium levels as a reference, the highest quartile showed increased odds of hypertension in model 1 (OR: 2.968; 95% CI: 1.121, 7.861) and model 3 (OR: 33.468; 95% CI: 1.881, 595.500).
-
Conclusions We found that dispatch frequency may affect blood cadmium levels in male firefighters, and high blood cadmium levels may influence hypertension in a dose-response manner.
BACKGROUND
METHODS
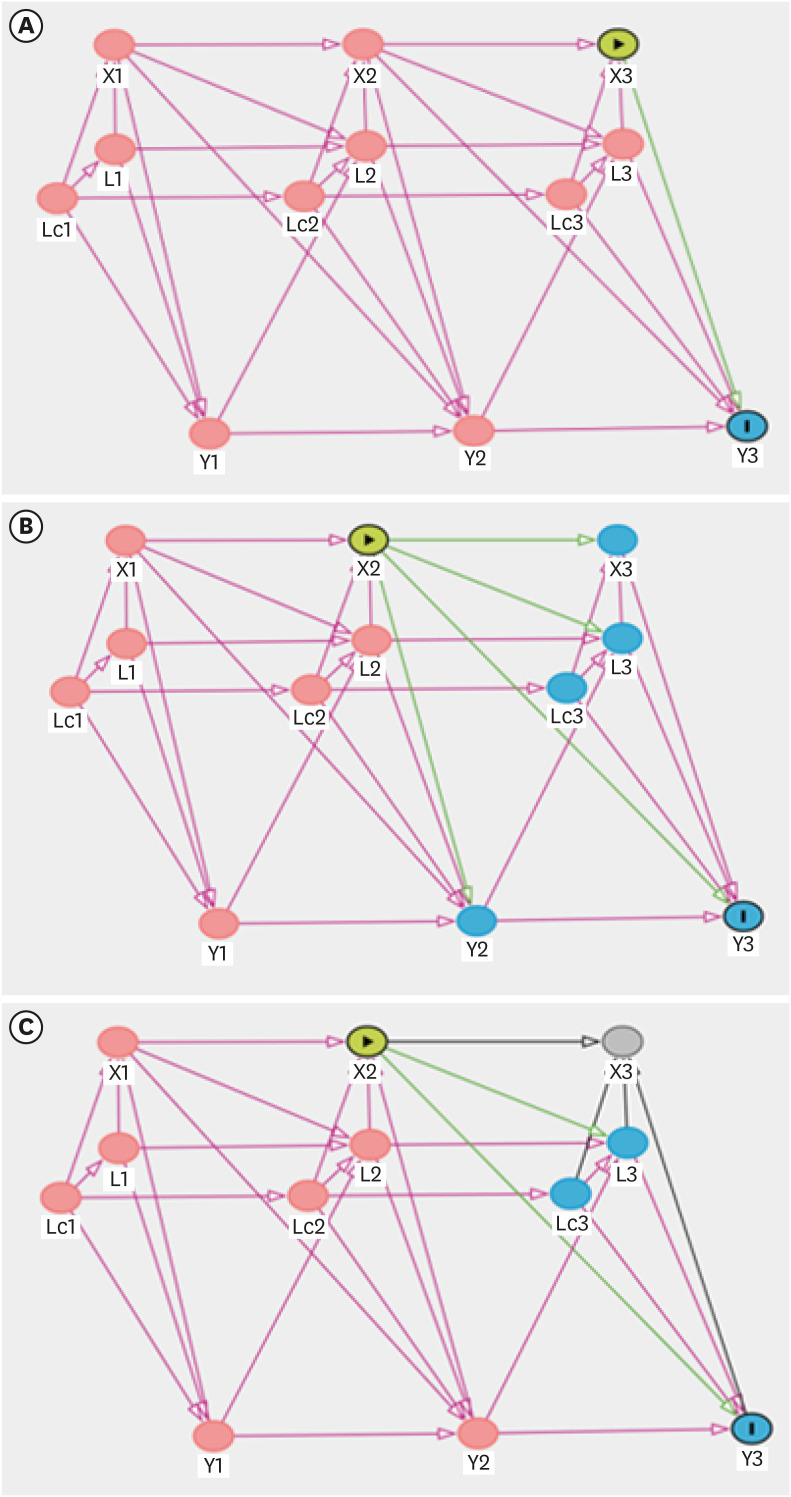
Directed acyclic graphs for three models to investigate the effect of the frequency of dispatch on blood cadmium levels. (A) Model 1 (short-term effect); (B) Model 2 (long-term effect); (C) Model 3 (reversed causal pathway model).
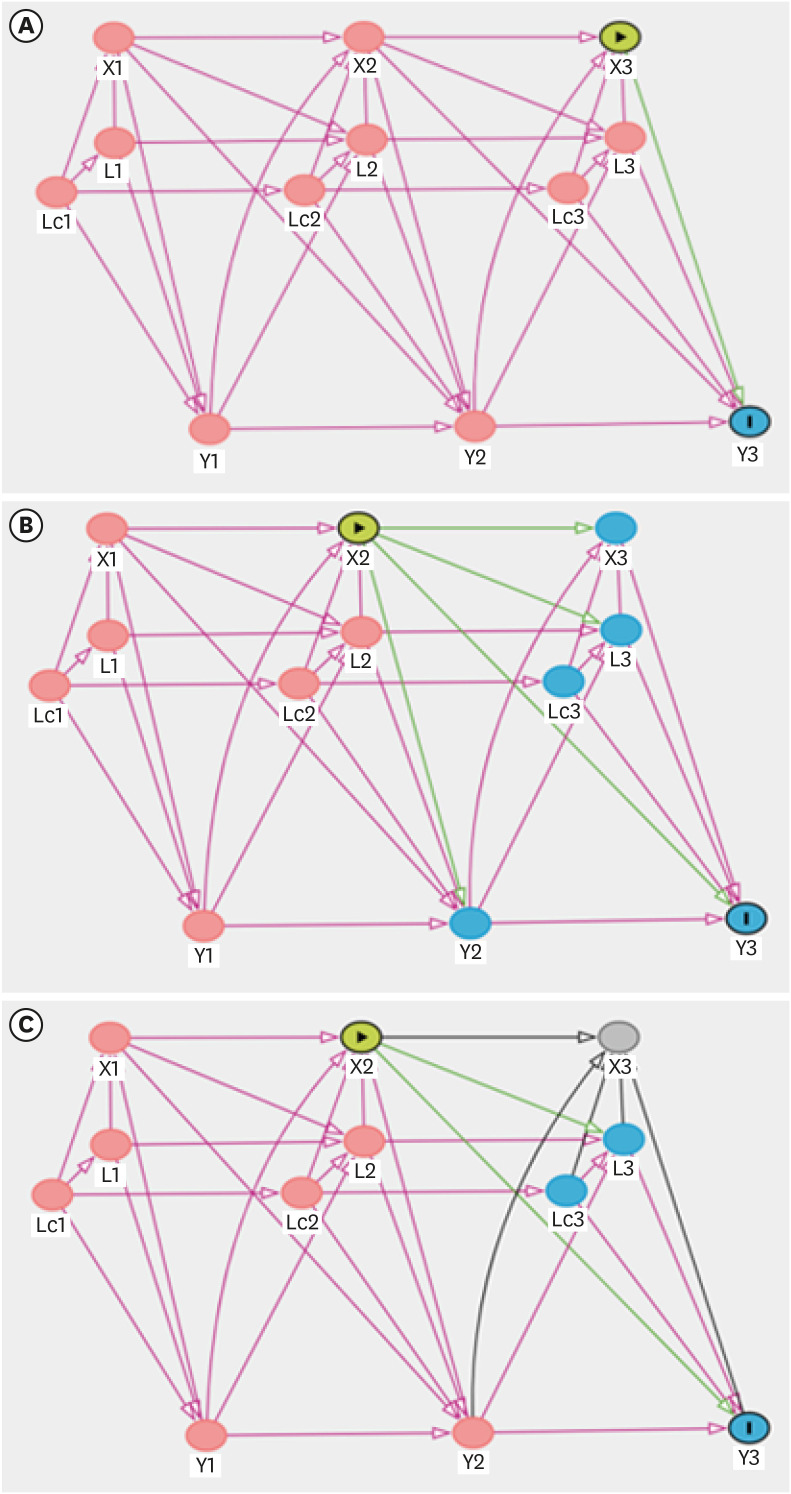
Directed acyclic graphs for three models to investigate the effect of blood cadmium levels on hypertension. (A) Model 1 (short-term effect); (B) Model 2 (long-term effect); (C) Model 3 (reversed causal pathway model).
Dispatch frequency and blood cadmium levels
-
(1) L(t) affects X(t), L(t+1), and Y(t): it follows the definition of confounders.
• L(t) affects X(t): work schedule and work department affect dispatch frequency.
• L(t) affects Y(t): work schedule and work department affect blood cadmium levels.
• Lc(t) affects X(t), L(t), Lc(t+1), and Y(t): age and education level affect other confounders.
• Lc(t) affects X(t): age and education level affect dispatch frequency. Depending on the age and education level of firefighters, they may have different work positions, which affects dispatch frequency.
Lc(t) affects L(t): age and education level affect the work schedule and work department.
• Lc(t) affects Y(t): age and education level affect blood cadmium levels.
-
(2) Y(t) affects L(t+1) and Y(t+1)
• Y(t) affects L(t+1): recognition of blood cadmium level affects smoking, alcohol consumption, exercise level, BMI, diabetes mellitus, work schedule, and work department through lifestyle modification and post-examination health care management; recognition of blood cadmium does not directly affect the frequency of dispatch, so the effect of Y(t) on X(t+1) is excluded.
-
(3) X(t) affects X(t+1), L(t+1), Y(t), and Y(t+1)
Blood cadmium levels and hypertension
-
(1) L(t) affects X(t), L(t+1), and Y(t): it follows the definition of confounders.
• L(t) affects X(t): smoking, alcohol consumption, exercise level, BMI, work schedule, work department, and diabetes mellitus affect blood cadmium levels.
• L(t) affects Y(t): smoking, alcohol consumption, exercise level, BMI, work schedule, work department, and diabetes mellitus affect hypertension.
• Lc(t) affects X(t), L(t), Lc(t+1), and Y(t): age and education affect other confounders.
• Lc(t) affects X(t): age and education level affect blood cadmium levels.
• Lc(t) affects L(t): age and education level affect smoking, alcohol consumption, exercise level, BMI, work schedule, work department, and diabetes mellitus.
• Lc(t) affects Y(t): age and education level affect hypertension.
-
(2) Y(t) affects X(t+1), L(t+1), and Y(t+1)
• Y(t) affects X(t+1): hypertension reduces the glomerular filtration rate, which increases blood cadmium levels.
• Y(t) affects L(t+1): diagnosis of hypertension affects smoking, alcohol consumption, exercise level, BMI, diabetes mellitus, work schedule, and work department through lifestyle modification and post-examination health care management.
-
(3) X(t) affects X(t+1), L(t+1), Y(t), and Y(t+1)
• X(t) affects L(t+1): recognition of blood cadmium level affects smoking, alcohol consumption, exercise level, BMI, diabetes mellitus, work schedule, and work department through lifestyle modification and post-examination health care management.
• X(t) affects Y(t+1): blood cadmium levels have a long-term direct effect on hypertension.
RESULTS
General characteristics of the participants at baseline (2015)
The regression coefficients (95% CI) for blood cadmium levels across categories of dispatch frequency
The ORs (95% CI) for hypertension per doubling of blood cadmium level
| OR (95% CI) for hypertension | ||||
|---|---|---|---|---|
| Crude | Model 1a | Model 2a | Model 3a | |
| Blood cadmium per doubling | 1.469 (1.132, 1.906) | 1.772 (1.046, 3.003) | 2.924 (0.777, 10.991) | 4.288 (1.110, 16.554) |
The ORs (95% CI) for hypertension across quartiles of blood cadmium levels
DISCUSSION
CONCLUSIONS
Abbreviations
BMI
Cd
CI
DAG
EDTA
GEE
JNC
KOSHA
NHANES
OR
PPE
SCMM
-
Competing interests: The authors declare that they have no competing interests.
-
Author Contributions:
NOTES
SUPPLEMENTARY MATERIALS
Supplementary Table 1
Supplementary Table 2
Supplementary Table 3
Supplementary Table 4
Supplementary Fig. 1
- 1. Alharbi BH, Pasha MJ, Al-Shamsi MAS. Firefighter exposures to organic and inorganic gas emissions in emergency residential and industrial fires. Sci Total Environ 2021;770:145332. 33515879.ArticlePubMed
- 2. Fabian TZ, Borgerson JL, Gandhi PD, Baxter CS, Ross CS, Lockey JE, et al. Characterization of firefighter smoke exposure. Fire Technol 2014;50(4):993–1019.ArticlePDF
- 3. Kim JM, Lee HJ. Hazards exposed to firefighters in fire-physical, chemical, and biologic factors. J Korean Med Assoc 2008;51(12):1072–1077.Article
- 4. Keir JLA, Akhtar US, Matschke DMJ, White PA, Kirkham TL, Chan HM, et al. Polycyclic aromatic hydrocarbon (PAH) and metal contamination of air and surfaces exposed to combustion emissions during emergency fire suppression: implications for firefighters’ exposures. Sci Total Environ 2020;698:134211. 31514022.ArticlePubMed
- 5. Gagas DF. Characterization of Contaminants on Firefighter’s Protective Equipment: A Firefighter’s Potential Exposure to Heavy Metals during a Structure Fire. Richmond, VA, USA: Eastern Kentucky University; 2015.
- 6. Soteriades ES, Smith DL, Tsismenakis AJ, Baur DM, Kales SN. Cardiovascular disease in US firefighters: a systematic review. Cardiol Rev 2011;19(4):202–215. 21646874.PubMed
- 7. Noh J, Lee CJ, Hyun DS, Kim W, Kim MJ, Park KS, et al. Blood pressure and the risk of major adverse cardiovascular events among firefighters. J Hypertens 2020;38(5):850–857. 31972671.ArticlePubMed
- 8. Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA 2017;317(2):165–182. 28097354.PubMed
- 9. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360(9349):1903–1913. 12493255.ArticlePubMed
- 10. Lip GYH, Coca A, Kahan T, Boriani G, Manolis AS, Olsen MH, et al. Hypertension and cardiac arrhythmias: executive summary of a consensus document from the European Heart Rhythm Association (EHRA) and ESC Council on Hypertension, endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulación Cardíaca y Electrofisiología (SOLEACE). Eur Heart J Cardiovasc Pharmacother 2017;3(4):235–250. 28541499.ArticlePubMed
- 11. Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet 2014;383(9932):1899–1911. 24881994.ArticlePubMedPMC
- 12. Lee BK, Ahn J, Kim NS, Lee CB, Park J, Kim Y. Association of blood pressure with exposure to lead and cadmium: analysis of data from the 2008-2013 Korean National Health and Nutrition Examination Survey. Biol Trace Elem Res 2016;174(1):40–51. 27087554.ArticlePubMedPDF
- 13. Tsoi MF, Lo CWH, Cheung TT, Cheung BMY. Blood lead level and risk of hypertension in the United States National Health and Nutrition Examination Survey 1999-2016. Sci Rep 2021;11(1):3010. 33542319.ArticlePubMedPMCPDF
- 14. Garner RE, Levallois P. Associations between cadmium levels in blood and urine, blood pressure and hypertension among Canadian adults. Environ Res 2017;155:64–72. 28189876.ArticlePubMed
- 15. Mallongi A, Birawida AB, Astuti RDP, Saleh M. Effect of lead and cadmium to blood pressure on communities along coastal areas of Makassar, Indonesia. Enferm Clin 2020;30:313–317.Article
- 16. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289(19):2560–2572. 12748199.ArticlePubMed
- 17. Park JT. Analysis of Fire Fighter’s Work Intensity of Scene Activities and Their Physiological Changes. Seoul, Korea: National Emergency Management Agency; 2014.
- 18. Han L, Wang X, Han R, Xu M, Zhao Y, Gao Q, et al. Association between blood lead level and blood pressure: an occupational population-based study in Jiangsu province, China. PLoS One 2018;13(7):e0200289. 29979755.ArticlePubMedPMC
- 19. An HC, Sung JH, Lee J, Sim CS, Kim SH, Kim Y. The association between cadmium and lead exposure and blood pressure among workers of a smelting industry: a cross-sectional study. Ann Occup Environ Med 2017;29(1):47. 29034097.ArticlePubMedPMCPDF
- 20. Jee Y, Cho SI. Associations between socioeconomic status and blood cadmium levels in Korea. Epidemiol Health 2019;41:e2019018. 31096749.ArticlePubMedPMC
- 21. Staessen J, Bulpitt CJ, Roels H, Bernard A, Fagard R, Joossens JV, et al. Urinary cadmium and lead concentrations and their relation to blood pressure in a population with low exposure. Br J Ind Med 1984;41(2):241–248. 6372852.ArticlePubMedPMC
- 22. Souza RV, Sarmento RA, de Almeida JC, Canuto R. The effect of shift work on eating habits: a systematic review. Scand J Work Environ Health 2019;45(1):7–21. 30088659.ArticlePubMed
- 23. Kurihara I, Kobayashi E, Suwazono Y, Uetani M, Inaba T, Oishiz M, et al. Association between exposure to cadmium and blood pressure in Japanese peoples. Arch Environ Health 2004;59(12):711–716. 16789481.PubMed
- 24. Eum KD, Lee MS, Paek D. Cadmium in blood and hypertension. Sci Total Environ 2008;407(1):147–153. 18845316.ArticlePubMed
- 25. Oliver-Williams C, Howard AG, Navas-Acien A, Howard BV, Tellez-Plaza M, Franceschini N. Cadmium body burden, hypertension, and changes in blood pressure over time: results from a prospective cohort study in American Indians. J Am Soc Hypertens 2018;12(6):426–437.e9. 29605538.ArticlePubMedPMC
- 26. Yeom JH, Sim CS, Lee J, Yun SH, Park SJ, Yoo CI, et al. Effect of shift work on hypertension: cross sectional study. Ann Occup Environ Med 2017;29(1):11. 28400961.ArticlePubMedPMCPDF
- 27. Keogh RH, Daniel RM, VanderWeele TJ, Vansteelandt S. Analysis of longitudinal studies with repeated outcome measures: adjusting for time-dependent confounding using conventional methods. Am J Epidemiol 2018;187(5):1085–1092. 29020128.ArticlePubMed
- 28. Newsome SJ, Keogh RH, Daniel RM. Estimating long-term treatment effects in observational data: a comparison of the performance of different methods under real-world uncertainty. Stat Med 2018;37(15):2367–2390. 29671915.ArticlePubMedPMCPDF
- 29. Nair AR, Lee WK, Smeets K, Swennen Q, Sanchez A, Thévenod F, et al. Glutathione and mitochondria determine acute defense responses and adaptive processes in cadmium-induced oxidative stress and toxicity of the kidney. Arch Toxicol 2015;89(12):2273–2289. 25388156.ArticlePubMedPDF
- 30. Satarug S, Nishijo M, Lasker JM, Edwards RJ, Moore MR. Kidney dysfunction and hypertension: role for cadmium, p450 and heme oxygenases? Tohoku J Exp Med 2006;208(3):179–202. 16498227.ArticlePubMed
- 31. Thévenod F, Friedmann JM. Cadmium-mediated oxidative stress in kidney proximal tubule cells induces degradation of Na+/K+-ATPase through proteasomal and endo-/lysosomal proteolytic pathways. FASEB J 1999;13(13):1751–1761. 10506578.ArticlePubMedPDF
- 32. Satarug S, Vesey DA, Gobe GC. Kidney cadmium toxicity, diabetes and high blood pressure: the perfect storm. Tohoku J Exp Med 2017;241(1):65–87. 28132967.ArticlePubMed
- 33. Perry HM Jr, Erlanger MW. Sodium retention in rats with cadmium-induced hypertension. Sci Total Environ 1981;22(1):31–38. 7336200.PubMed
- 34. Kaji T, Suzuki M, Yamamoto C, Mishima A, Sakamoto M, Kozuka H. Severe damage of cultured vascular endothelial cell monolayer after simultaneous exposure to cadmium and lead. Arch Environ Contam Toxicol 1995;28(2):168–172. 7710289.ArticlePubMedPDF
- 35. Varoni MV, Palomba D, Gianorso S, Anania V. Cadmium as an environmental factor of hypertension in animals: new perspectives on mechanisms. Vet Res Commun 2003;27(Suppl 1):807–810. 14535527.ArticlePubMed
- 36. Kisling GM, Kopp SJ, Paulson DJ, Tow JP. Cadmium-induced attenuation of coronary blood flow in the perfused rat heart. Toxicol Appl Pharmacol 1993;118(1):58–64. 8430424.ArticlePubMed
- 37. Perry HM Jr, Erlanger MW. Elevated circulating renin activity in rats following doses of cadmium known to induce hypertension. J Lab Clin Med 1973;82(3):399–405. 4353877.PubMed
- 38. Prentice RC, Hawley PL, Glonek T, Kopp SJ. Calcium-dependent effects of cadmium on energy metabolism and function of perfused rat heart. Toxicol Appl Pharmacol 1984;75(2):198–210. 6474458.ArticlePubMed
- 39. Tellez-Plaza M, Navas-Acien A, Crainiceanu CM, Guallar E. Cadmium exposure and hypertension in the 1999-2004 National Health and Nutrition Examination Survey (NHANES). Environ Health Perspect 2008;116(1):51–56. 18197299.ArticlePubMedPMC
- 40. Staessen JA, Kuznetsova T, Roels HA, Emelianov D, Fagard R. Public Health and Environmental Exposure to Cadmium Study Group. Exposure to cadmium and conventional and ambulatory blood pressures in a prospective population study. Am J Hypertens 2000;13(2):146–156. 10701814.ArticlePubMed
- 41. Wang Q, Wei S. Cadmium affects blood pressure and negatively interacts with obesity: findings from NHANES 1999-2014. Sci Total Environ 2018;643:270–276. 29936168.ArticlePubMed
- 42. Chen X, Zhu G, Lei L, Jin T. The association between blood pressure and blood cadmium in a Chinese population living in cadmium polluted area. Environ Toxicol Pharmacol 2013;36(2):595–599. 23834962.ArticlePubMed
- 43. Lee BK, Kim Y. Association of blood cadmium with hypertension in the Korean general population: analysis of the 2008-2010 Korean National Health and Nutrition Examination Survey data. Am J Ind Med 2012;55(11):1060–1067. 22692952.ArticlePubMed
- 44. Noor N, Zong G, Seely EW, Weisskopf M, James-Todd T. Urinary cadmium concentrations and metabolic syndrome in U.S. adults: the National Health and Nutrition Examination Survey 2001-2014. Environ Int 2018;121(Pt 1):349–356. 30243183.ArticlePubMedPMC
- 45. Wu W, Jiang S, Zhao Q, Zhang K, Wei X, Zhou T, et al. Associations of environmental exposure to metals with the risk of hypertension in China. Sci Total Environ 2018;622-623:184–191. 29216461.ArticlePubMed
- 46. Mordukhovich I, Wright RO, Hu H, Amarasiriwardena C, Baccarelli A, Litonjua A, et al. Associations of toenail arsenic, cadmium, mercury, manganese, and lead with blood pressure in the normative aging study. Environ Health Perspect 2012;120(1):98–104. 21878420.ArticlePubMedPMC
- 47. Vallée A, Gabet A, Grave C, Blacher J, Olié V. Associations between urinary cadmium levels, blood pressure, and hypertension: the ESTEBAN survey. Environ Sci Pollut Res Int 2020;27(10):10748–10756. 31950414.ArticlePubMedPDF
- 48. Ahn J, Kim NS, Lee BK, Park J, Kim Y. Association of blood pressure with blood lead and cadmium levels in Korean adolescents: analysis of data from the 2010-2016 Korean National Health and Nutrition Examination Survey. J Korean Med Sci 2018;33(44):e278. 30369859.ArticlePubMedPMCPDF
- 49. Gallagher CM, Meliker JR. Blood and urine cadmium, blood pressure, and hypertension: a systematic review and meta-analysis. Environ Health Perspect 2010;118(12):1676–1684. 20716508.ArticlePubMedPMC
- 50. Martins ACB, Almeida Lopes AC, Urbano MR, Carvalho MFH, Silva AMR, Tinkov AA, et al. An updated systematic review on the association between Cd exposure, blood pressure and hypertension. Ecotoxicol Environ Saf 2021;208:111636. 33396156.ArticlePubMedPMC
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Sex Differences in the Effects of Cadmium and Uric Acid Levels on Hypertension Risk: A Dose–Response Relationship and Synergistic Effect Study
Ruiqi Yang, Yiling Chen, Xu Hui, Xin Fan, Xiaonan Li, Weize Kong, Qian Liu, Yizhuo Chen, Kaiwen Wang, Xinyi Li, Peijing Yan, Jinhui Tian, Yongbin Lu
Journal of Evidence-Based Medicine.2025;[Epub] CrossRef - Internal Flames: Metal(loid) Exposure Linked to Alteration of the Lipid Profile in Czech Male Firefighters (CELSPAC-FIREexpo Study)
Nina Pálešová, Katarína Řiháčková, Jan Kuta, Aleš Pindur, Ludmila Šebejová, Pavel Čupr
Environmental Science & Technology Letters.2024; 11(7): 679. CrossRef - Cadmium exposure and risk of hypertension: A systematic review and dose-response meta-analysis
Pietro Verzelloni, Vincenzo Giuliano, Lauren A. Wise, Teresa Urbano, Claudia Baraldi, Marco Vinceti, Tommaso Filippini
Environmental Research.2024; 263: 120014. CrossRef - Heavy metal exposure linked to metabolic syndrome in Korean male firefighters: FRESH cohort cross-sectional analysis
Jee Eun Choi, Mun-Joo Bae, Mi-Ji Kim, Sung Soo Oh, Ki Soo Park, Chan Joo Lee, Sungha Park, Sang-Baek Koh, Jaelim Cho, Changsoo Kim
Scientific Reports.2023;[Epub] CrossRef
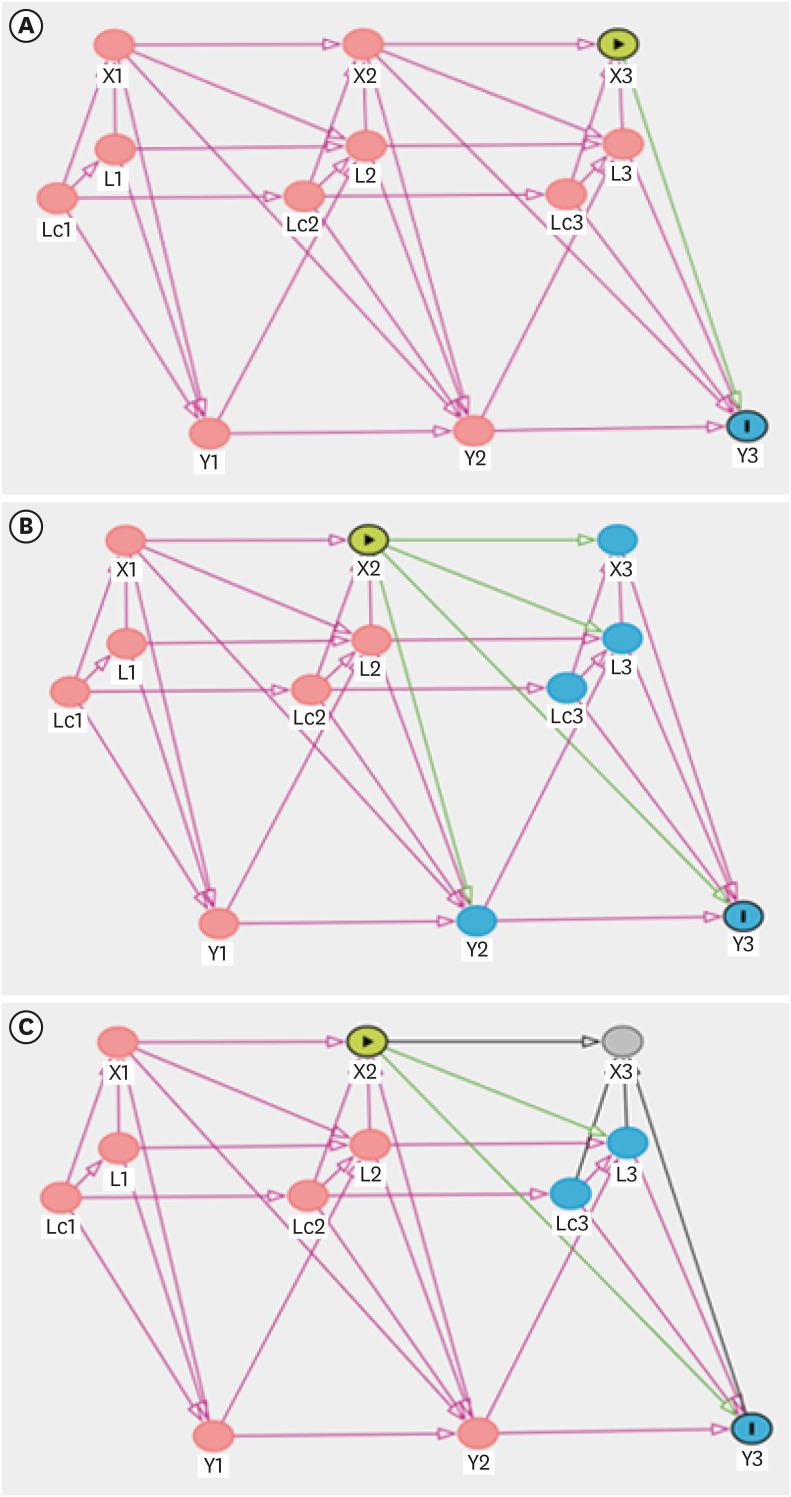
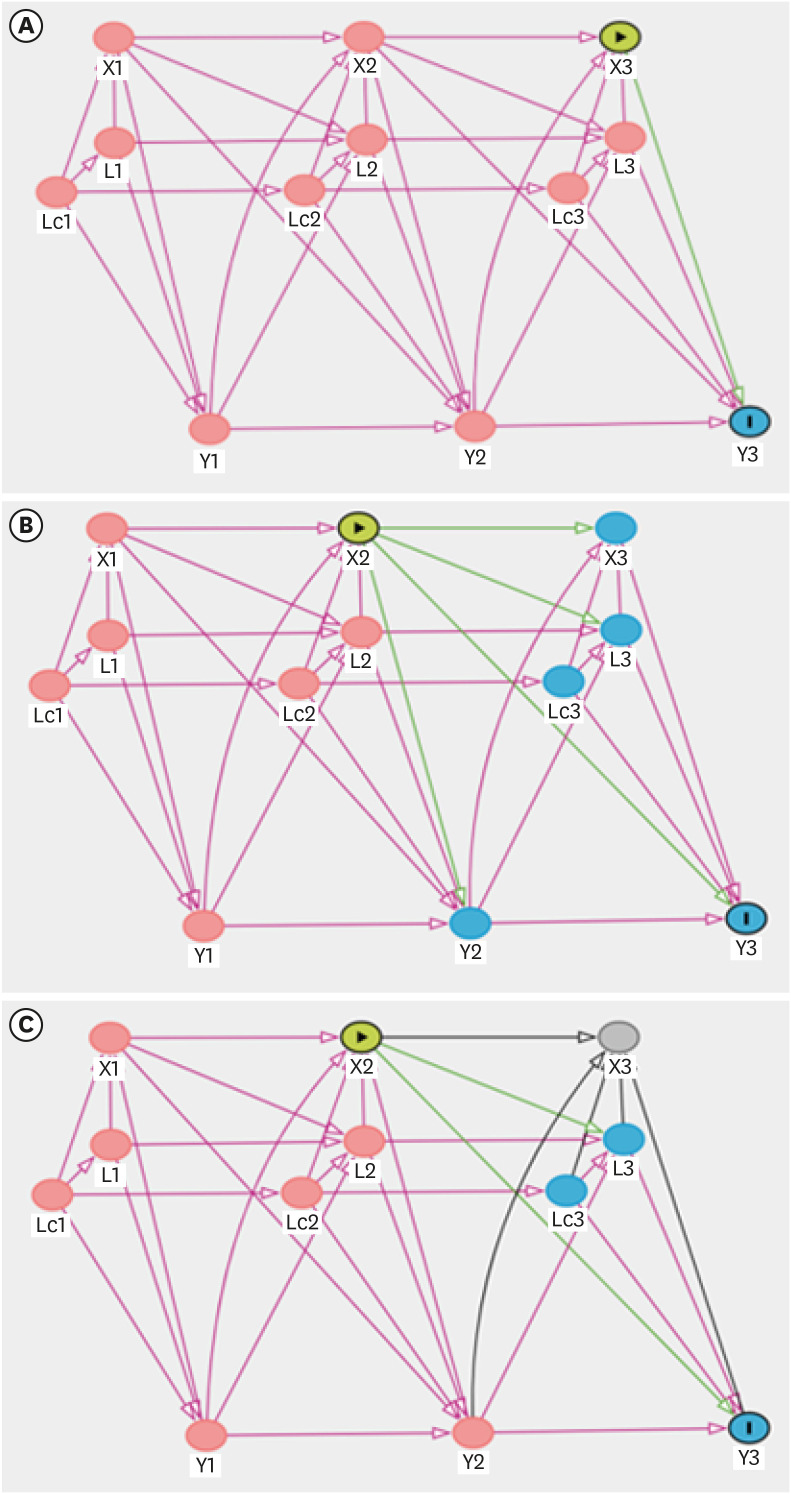
Fig. 1
Fig. 2
| Variable | Blood cadmium quartile (μg/dL) | ||||||
|---|---|---|---|---|---|---|---|
| Total (0.22–24.06) | Q1 (0.22–3.47) | Q2 (3.51–5.14) | Q3 (5.87–7.02) | Q4 (7.03–24.06) | |||
| No. of participants | 215 | 54 | 54 | 54 | 53 | ||
| Age (yr) | 42.0 ± 8.25 | 37.9 ± 8.49 | 42.6 ± 7.65 | 43.2 ± 7.49 | 44.5 ± 7.98 | < 0.001 | |
| BMI (kg/m2) | 24.5 ± 2.53 | 24.5 ± 2.68 | 24.3 ± 2.46 | 24.8 ± 2.35 | 24.6 ± 2.66 | 0.640 | |
| Education | 0.324 | ||||||
| ≤ High school | 46 (21.4) | 11 (20.4) | 11 (20.4) | 10 (18.5) | 14 (26.4) | ||
| College | 57 (26.5) | 12 (22.2) | 17 (31.5) | 12 (22.2) | 16 (30.2) | ||
| ≥ University | 112 (52.1) | 31 (57.4) | 26 (48.2) | 32 (59.3) | 23 (43.4) | ||
| Smoking status | 0.002 | ||||||
| Non-smoker | 118 (54.9) | 36 (66.7) | 31 (57.4) | 33 (61.1) | 18 (34.0) | ||
| Ex-smoker | 62 (28.8) | 12 (22.2) | 15 (27.8) | 14 (25.9) | 21 (39.6) | ||
| Current smoker | 35 (16.3) | 6 (11.1) | 8 (14.8) | 7 (13.0) | 14 (26.4) | ||
| Alcohol intake (per week) | 0.343 | ||||||
| Never | 74 (34.4) | 21 (38.9) | 19 (35.2) | 20 (37.0) | 14 (26.4) | ||
| < 1 | 67 (31.2) | 16 (29.6) | 15 (27.8) | 16 (29.6) | 20 (37.7) | ||
| 1–2 | 70 (32.6) | 16 (29.6) | 20 (37.0) | 17 (31.5) | 17 (32.1) | ||
| ≥ 3 | 4 (1.9) | 1 (1.9) | 0 (0.0) | 1 (1.9) | 2 (3.8) | ||
| Exercise level (per week) | 0.595 | ||||||
| < 1 | 23 (10.7) | 8 (14.8) | 6 (11.1) | 5 (9.3) | 4 (7.6) | ||
| 1–2 | 97 (45.1) | 23 (42.6) | 24 (44.4) | 24 (44.4) | 26 (49.1) | ||
| ≥ 3 | 95 (44.2) | 23 (42.6) | 24 (44.4) | 25 (46.3) | 23 (43.4) | ||
| Diabetes mellitus | 0.828 | ||||||
| No | 210 (97.7) | 54 (100.0) | 51 (94.4) | 53 (98.2) | 52 (98.1) | ||
| Yes | 5 (2.3) | 0 (0.0) | 3 (5.6) | 1 (1.9) | 1 (1.9) | ||
| Hypertension | 0.364 | ||||||
| No | 163 (75.8) | 45 (83.3) | 38 (70.4) | 41 (75.9) | 39 (73.6) | ||
| Yes | 52 (24.2) | 9 (16.7) | 16 (29.6) | 13 (24.1) | 14 (26.4) | ||
| Work schedule | 0.788 | ||||||
| Day work | 49 (22.8) | 15 (27.8) | 7 (13.0) | 13 (24.1) | 14 (26.4) | ||
| Shift work | 166 (77.2) | 37 (72.2) | 47 (87.0) | 41 (75.9) | 39 (73.6) | ||
| Work department | 0.480 | ||||||
| Administrative | 57 (26.5) | 19 (35.2) | 9 (16.7) | 16 (29.6) | 13 (24.5) | ||
| Non-administrative | 158 (73.5) | 35 (64.8) | 45 (83.3) | 38 (70.4) | 40 (75.5) | ||
| Dispatch frequency | 0.242 | ||||||
| < 50% | 103 (47.9) | 30 (55.6) | 22 (40.7) | 29 (53.7) | 22 (41.5) | ||
| 50%–75% | 51 (23.7) | 12 (22.2) | 16 (29.6) | 10 (18.5) | 13 (24.5) | ||
| ≥ 75% | 61 (28.4) | 12 (22.2) | 16 (29.6) | 15 (27.8) | 18 (34.0) | ||
| Dispatch frequency | Coefficients (95% CI) for blood cadmium levels (μg/dL) | |||
|---|---|---|---|---|
| Crude | Model 1a | Model 2a | Model 3a | |
| < 50% | Reference | Reference | Reference | Reference |
| 50%–75% | 1.393 (0.662, 2.124) | 1.425 (0.502, 2.347) | 2.417 (1.162, 3.672) | 0.189 (−0.756, 0.378) |
| ≥ 75% | 0.870 (0.233, 1.507) | 0.901 (−0.039, 1.833) | 1.879 (0.673, 3.086) | 0.708 (0.023, 1.394) |
| OR (95% CI) for hypertension | ||||
|---|---|---|---|---|
| Crude | Model 1a | Model 2a | Model 3a | |
| Blood cadmium per doubling | 1.469 (1.132, 1.906) | 1.772 (1.046, 3.003) | 2.924 (0.777, 10.991) | 4.288 (1.110, 16.554) |
| Blood cadmium | OR (95% CI) for hypertension | |||
|---|---|---|---|---|
| Crude | Model 1a | Model 2a | Model 3a | |
| < 25% | Reference | Reference | Reference | Reference |
| 25%–50% | 1.570 (0.894, 2.755) | 1.133 (0.461, 2.785) | 5.182 (0.195, 137.642) | 7.112 (0.483, 104.733) |
| 50%–75% | 1.570 (0.876, 2.813) | 1.582 (0.687, 3.640) | 8.666 (0.446, 168.397) | 17.047 (1.131, 256.787) |
| ≥ 75% | 2.120 (1.145, 3.924) | 2.968 (1.121, 7.861) | 15.299 (0.776, 301.607) | 33.468 (1.881, 595.500) |
Values are presented as mean ± standard deviation or number (%).
BMI: body mass index.
CI: confidence interval; Model 1: short-term effect model; Model 2: long-term effect model; Model 3: reversed causal pathway model.
aAdjusted for age, education level, work department, and work schedule.
OR: odds ratio; CI: confidence interval; Model 1: short-term effect model; Model 2: long-term effect model; Model 3: reversed causal pathway model.
aAdjusted for age, body mass index, smoking status, alcohol intake, exercise level, education level, work schedule, work department, and diabetes mellitus.
OR: odds ratio; CI: confidence interval; Model 1: short-term effect model; Model 2: long-term effect model; Model 3: reversed causal pathway model.
aAdjusted for age, body mass index, smoking status, alcohol intake, exercise level, education level, work schedule, work department, and diabetes mellitus.
 KSOEM
KSOEM

 Cite
Cite

