Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 34; 2022 > Article
- Original Article Impacts of presenteeism on work-related injury absence and disease absence
-
Youna Won1
 , Hwan-Cheol Kim1,2
, Hwan-Cheol Kim1,2 , Jiho Kim1
, Jiho Kim1 , Minsun Kim1
, Minsun Kim1 , Seong-Cheol Yang1,2
, Seong-Cheol Yang1,2 , Shin-Goo Park1,2
, Shin-Goo Park1,2 , Jong-Han Leem1,2
, Jong-Han Leem1,2
-
Annals of Occupational and Environmental Medicine 2022;34:e25.
DOI: https://doi.org/10.35371/aoem.2022.34.e25
Published online: September 23, 2022
1Department of Occupational and Environmental Medicine, Inha University Hospital, Incheon, Korea.
2Departments of Social and Preventive Medicine, School of Medicine, Inha University, Incheon, Korea.
- Address for Correspondence: Hwan-Cheol Kim. Department of Occupational and Environmental Medicine, School of Medicine, Inha University Hospital, 27 Inhang-ro, Jung-gu, Incheon 22332, Republic of Korea. carpediem@inha.ac.kr
Copyright © 2022 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background Many studies have been conducted on presenteeism and absenteeism, but the relationship between presenteeism and absenteeism is unclear. This study was undertaken to investigate the effect of presenteeism on future absenteeism.
-
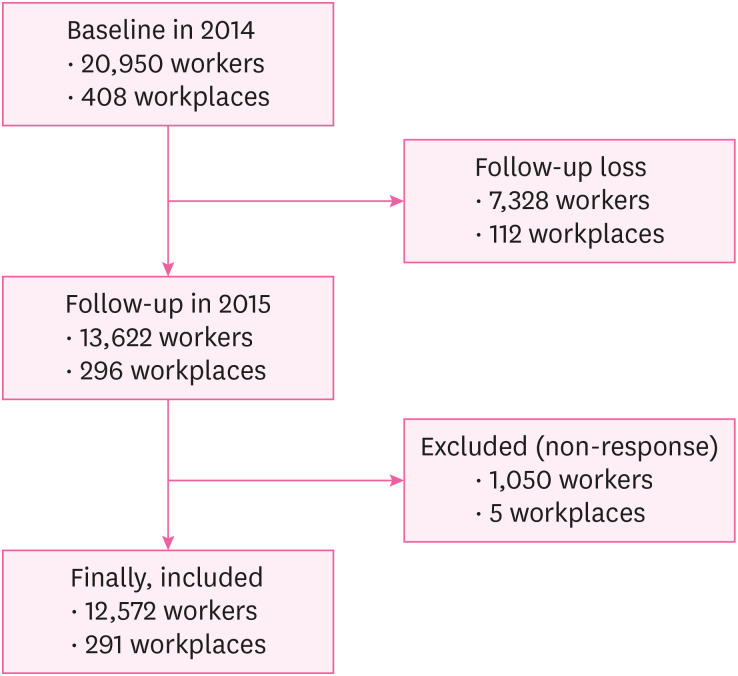
Methods This study was conducted on non-white collar workers that underwent general health examinations in 2014 and 2015. We asked subjects to fill out a questionnaire about their experiences of presenteeism for the past one year in 2014. In 2015, it was checked whether the same subjects had any experience of absence from work due to injury or disease during the past year. The χ2 test was used to analyze relationships between sociodemographic and occupational characteristics, presenteeism, and absence. Odds ratios (ORs) were calculated by logistic regression analysis controlled for confounding factors.
-
Results A total of 12,572 workers were included in the study. For workers who experienced presenteeism, the OR for injury absence was 2.705 (95% confidence interval [CI]: 2.044–3.581), and the OR for disease absence was 4.906 (95% CI: 3.996–6.024) after adjusting for sociodemographic and occupational confounding factors. For men that experienced presenteeism, the OR for injury absence was 3.035 (95% CI: 2.258–4.081), and the OR for disease absence was 5.508 (95% CI: 4.340–6.989). For women that experienced presenteeism, the OR for injury absence was 1.322 (95% CI: 0.577–3.028), which was not significant, and the OR for disease absence was 3.629 (95% CI: 2.405–5.475).
-
Conclusions This study suggests that presenteeism can influence future absenteeism. The effect of presenteeism may depend on cause of absence. Men who experienced presenteeism showed greater effects on injury and disease absence than women. For women, experience of presenteeism had a significant effect on disease absence but not on injury absence.
BACKGROUND
METHODS
RESULTS
Sociodemographic and occupational characteristics of the study subjects
Sociodemographic and occupational characteristics of the study subjects according to absence due to injury
Sociodemographic and occupational characteristics of the study subjects according to absence due to disease
Associations between presenteeism with or without adjustment for confounding variables and absence due to injury or disease
Associations between presenteeism and absence due to injury or disease in men and women with or without adjustment for confounding variables
DISCUSSION
CONCLUSIONS
-
Competing interests: The authors declare that they have no competing interests.
-
Author Contributions:
NOTES
- 1. Karanika-Murray M, Cooper CL. Presenteeism: an introduction to a prevailing global phenomenon. Updated 2018]. Accessed May 14, 2021]. http://irep.ntu.ac.uk/id/eprint/33625/1/8260_Karanika-Murray.pdf .
- 2. Taloyan M, Aronsson G, Leineweber C, Magnusson Hanson L, Alexanderson K, Westerlund H. Sickness presenteeism predicts suboptimal self-rated health and sickness absence: a nationally representative study of the Swedish working population. PLoS One 2012;7(9):e44721. 22984547.ArticlePubMedPMC
- 3. Boles M, Pelletier B, Lynch W. The relationship between health risks and work productivity. J Occup Environ Med 2004;46(7):737–745. 15247814.ArticlePubMed
- 4. Hemp P. Presenteeism: at work--but out of it. Harv Bus Rev 2004;82(10):49–58. 155. 15559575.PubMed
- 5. Lohaus D, Habermann W. Presenteeism: a review and research directions. Hum Resour Manage Rev 2019;29(1):43–58.Article
- 6. Bielecky A, Chen C, Ibrahim S, Beaton DE, Mustard CA, Smith PM. The impact of co-morbid mental and physical disorders on presenteeism. Scand J Work Environ Health 2015;41(6):554–564. 26392307.ArticlePubMed
- 7. Krane L, Larsen EL, Nielsen CV, Stapelfeldt CM, Johnsen R, Risør MB. Attitudes towards sickness absence and sickness presenteeism in health and care sectors in Norway and Denmark: a qualitative study. BMC Public Health 2014;14(1):880. 25160059.ArticlePubMedPMCPDF
- 8. Kim MS, Park JB, Min KB, Lee KJ, Kwon K. Presenteeism among self-employed workers: Korean working conditions survey. Ann Occup Environ Med 2014;26:32. 25852942.ArticlePubMedPMCPDF
- 9. Aronsson G, Gustafsson K, Dallner M. Sick but yet at work. An empirical study of sickness presenteeism. J Epidemiol Community Health 2000;54(7):502–509. 10846192.ArticlePubMedPMC
- 10. Leineweber C, Westerlund H, Hagberg J, Svedberg P, Alexanderson K. Sickness presenteeism is more than an alternative to sickness absence: results from the population-based SLOSH study. Int Arch Occup Environ Health 2012;85(8):905–914. 22270388.ArticlePubMedPDF
- 11. Allebeck P, Mastekaasa A. Swedish Council on Technology Assessment in Health Care (SBU). Chapter 5. Risk factors for sick leave - general studies. Scand J Public Health Suppl 2004;63:49–108. 15513654.PubMed
- 12. Veazie MA, Smith GS. Heavy drinking, alcohol dependence, and injuries at work among young workers in the United States labor force. Alcohol Clin Exp Res 2000;24(12):1811–1819. 11141040.ArticlePubMed
- 13. Buvik K, Moan IS, Halkjelsvik T. Alcohol-related absence and presenteeism: beyond productivity loss. Int J Drug Policy 2018;58:71–77. 29864644.ArticlePubMed
- 14. Cheng WJ, Huang MC, Cheng Y, Chen CH, Chen CJ. Consumption of alcoholic energy drinks is associated with work-related injury or disease among manual workers in Taiwan. Alcohol Alcohol 2015;50(4):458–462. 25780028.ArticlePubMed
- 15. Barnes AJ, Zimmerman FJ. Associations of occupational attributes and excessive drinking. Soc Sci Med 2013;92:35–42. 23849277.ArticlePubMedPMC
- 16. Lincoln AE, Smith GS, Amoroso PJ, Bell NS. The effect of cigarette smoking on musculoskeletal-related disability. Am J Ind Med 2003;43(4):337–349. 12645091.ArticlePubMedPMC
- 17. Lee JJ, Patel R, Biermann JS, Dougherty PJ. The musculoskeletal effects of cigarette smoking. J Bone Joint Surg Am 2013;95(9):850–859. 23636193.ArticlePubMed
- 18. Jang SW, Kim HC, Kim JH, Kim MS, Won Y, Ju H, et al. Association between nicotine dependency with occupational injury in Korean men. Ann Occup Environ Med 2021;33:e14. 34754475.ArticlePubMedPMCPDF
- 19. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380(9859):2224–2260. 23245609.PubMedPMC
- 20. Bhattacherjee A, Chau N, Sierra CO, Legras B, Benamghar L, Michaely JP, et al. Relationships of job and some individual characteristics to occupational injuries in employed people: a community-based study. J Occup Health 2003;45(6):382–391. 14676418.ArticlePubMedPDF
- 21. Johns G. Presenteeism in the workplace: a review and research agenda. J Organ Behav 2010;31(4):519–542.ArticlePDF
- 22. Kim HC, Min JY, Min KB, Park SG. Job strain and the risk for occupational injury in small- to medium-sized manufacturing enterprises: a prospective study of 1,209 Korean employees. Am J Ind Med 2009;52(4):322–330. 19142960.ArticlePubMed
- 23. Bergström G, Bodin L, Hagberg J, Aronsson G, Josephson M. Sickness presenteeism today, sickness absenteeism tomorrow? A prospective study on sickness presenteeism and future sickness absenteeism. J Occup Environ Med 2009;51(6):629–638. 19448572.ArticlePubMed
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Present but Overlooked: A Scoping Review of Instruments and Approaches for Measuring Presenteeism Related to Alcohol, Tobacco, and Drug Use
Kirrilly Thompson, Md Abdul Ahad, Gianluca Di Censo, Sonia Hines, Nicholas Rich, Alice McEntee, Jacqueline Bowden
Journal of Occupational Rehabilitation.2025;[Epub] CrossRef - Number of side jobs and self-reported occupational injuries or diseases risk among young workers: a cross-sectional study in Japan
Takahiro Mori, Tomohisa Nagata, Kiminori Odagami, Koji Mori
Safety Science.2025; 192: 106982. CrossRef - Association between sickness presenteeism and depressive symptoms: a cross-sectional study using the 6th Korean working conditions survey
Myeong-Hun Lim, Min-Seok Kim, Seong-Uk Baek, Tae-Yeon Kim, Jong-Uk Won, Jin-Ha Yoon
International Archives of Occupational and Environmental Health.2024; 97(5): 537. CrossRef - Self-Esteem Trajectories After Occupational Injuries and Diseases and Their Relation to Changes in Subjective Health: Result From the Panel Study of Workers’ Compensation Insurance (PSWCI)
Seong-Uk Baek, Won-Tae Lee, Min-Seok Kim, Myeong-Hun Lim, Jin-Ha Yoon, Jong-Uk Won
Journal of Korean Medical Science.2023;[Epub] CrossRef
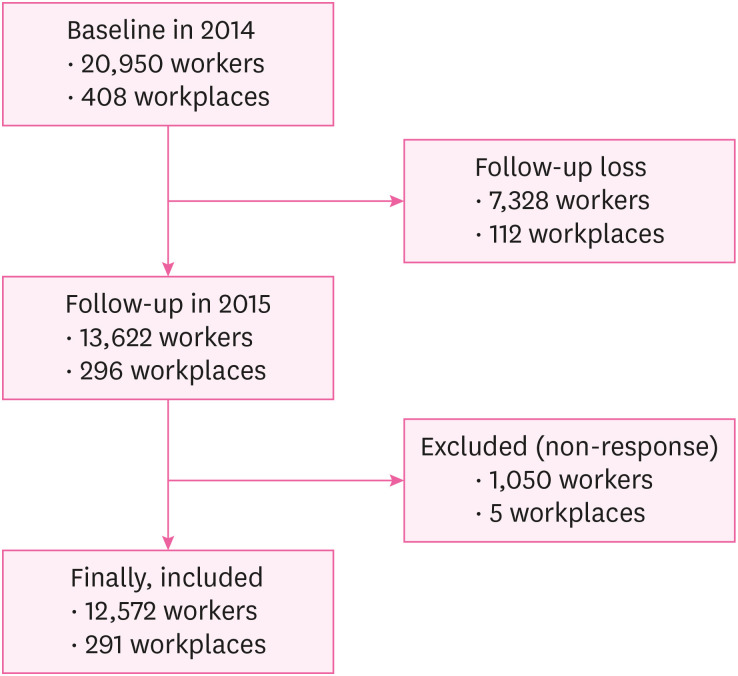
Fig. 1
| Characteristics | Presenteeism | Total | ||||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| No. of subject | 2,823 (22.5) | 9,749 (77.5) | 12,572 (100.0) | |||
| General characteristics | ||||||
| Sex | < 0.001 | |||||
| Male | 1,681 (17.7) | 7,841 (82.3) | 9,522 (100.0) | |||
| Female | 1,142 (37.4) | 1,908 (62.6) | 3,050 (100.0) | |||
| Age (yr) | < 0.001 | |||||
| < 30 | 606 (31.2) | 1,338 (68.8) | 1,944 (100.0) | |||
| 30–39 | 1,015 (27.2) | 2,722 (72.8) | 3,737 (100.0) | |||
| 40–49 | 728 (20.2) | 2,871 (79.8) | 3,599 (100.0) | |||
| 50–59 | 448 (14.7) | 2,595 (85.3) | 3,043 (100.0) | |||
| > 59 | 26 (10.4) | 223 (89.6) | 249 (100.0) | |||
| Chronic disease | 0.001 | |||||
| No | 2,406 (23.0) | 8,046 (77.0) | 10,452 (100.0) | |||
| Yes | 417 (19.7) | 1,703 (80.3) | 2,120 (100.0) | |||
| Smoking | < 0.001 | |||||
| Never smoker | 1,412 (26.7) | 3,880 (73.3) | 5,292 (100.0) | |||
| Former smoker | 443 (15.7) | 2,376 (84.3) | 2,819 (100.0) | |||
| Current smoker | 968 (21.7) | 3,493 (78.3) | 4,461 (100.0) | |||
| Alcohol consumption (time/week) | 0.208 | |||||
| 0–2 | 2,339 (22.6) | 8,033 (77.4) | 10,372 (100.0) | |||
| 3–4 | 391 (21.3) | 1,442 (78.7) | 1,833 (100.0) | |||
| 5–6 | 93 (25.3) | 274 (74.7) | 367 (100.0) | |||
| Occupational characteristics | ||||||
| Industry classification | < 0.001 | |||||
| Manufacturing | 1,150 (24.1) | 3,622 (75.9) | 4,772 (100.0) | |||
| Water, sewage and waste treatment, raw material recycling | 3 (15.0) | 17 (85.0) | 20 (100.0) | |||
| Construction industry | 2 (14.3) | 12 (85.7) | 14 (100.0) | |||
| Wholesale and retail | 32 (13.8) | 200 (86.2) | 232 (100.0) | |||
| Transport and warehousing | 387 (15.2) | 2,152 (84.8) | 2,539 (100.0) | |||
| Information and communication business | 41 (17.4) | 194 (82.6) | 235 (100.0) | |||
| Professional, scientific and technical services | 81 (23.8) | 260 (76.2) | 341 (100.0) | |||
| Business facility management, business support and rental service business | 468 (27.5) | 1,232 (72.5) | 1,700 (100.0) | |||
| Public administration, defense and social security administration | 25 (12.7) | 172 (87.3) | 197 (100.0) | |||
| Education service industry | 8 (21.1) | 30 (78.9) | 38 (100.0) | |||
| Health industry and social welfare service industry | 485 (40.3) | 717 (59.7) | 1,202 (100.0) | |||
| Associations and organizations, repair and other personal service businesses | 141 (11.0) | 1,141 (89.0) | 1,282 (100.0) | |||
| Size of the workplace | 0.506 | |||||
| Less than 300 | 912 (22.8) | 3,085 (77.2) | 3,997 (100.0) | |||
| 300 or more | 1,911 (22.3) | 6,664 (77.7) | 8,575 (100.0) | |||
| Characteristics | Injury absence | Total | ||||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| No. of subject | 219 (1.7) | 12,353 (98.3) | 12,572 (100.0) | |||
| Presenteeism | < 0.001 | |||||
| No | 129 (1.3) | 9,620 (98.7) | 9,749 (100.0) | |||
| Yes | 90 (3.2) | 2,733 (96.8) | 2,823 (100.0) | |||
| General characteristics | ||||||
| Sex | < 0.001 | |||||
| Male | 194 (2.0) | 9,328 (98.0) | 9,522 (100.0) | |||
| Female | 25 (0.8) | 3,025 (99.2) | 3,050 (100.0) | |||
| Age (yr) | 0.087 | |||||
| < 30 | 26 (1.3) | 1,918 (98.7) | 1,944 (100.0) | |||
| 30–39 | 59 (1.6) | 3,678 (98.4) | 3,737 (100.0) | |||
| 40–49 | 60 (1.7) | 3,539 (98.3) | 3,599 (100.0) | |||
| 50–59 | 70 (2.3) | 2,973 (97.7) | 3,043 (100.0) | |||
| > 59 | 4 (1.6) | 245 (98.4) | 249 (100.0) | |||
| Chronic disease | 0.706 | |||||
| No | 180 (1.7) | 10,272 (98.3) | 10,452 (100.0) | |||
| Yes | 39 (1.8) | 2,081 (98.2) | 2,120 (100.0) | |||
| Smoking | < 0.001 | |||||
| Never smoker | 56 (1.1) | 5,236 (98.9) | 5,292 (100.0) | |||
| Former smoker | 45 (1.6) | 2,774 (98.4) | 2,819 (100.0) | |||
| Current smoker | 118 (2.6) | 4,434 (99.4) | 4,461 (100.0) | |||
| Alcohol consumption (time/week) | 0.297 | |||||
| 0–2 | 172 (1.7) | 10,200 (98.3) | 10,372 (100.0) | |||
| 3–4 | 39 (2.1) | 1,794 (97.9) | 1,833 (100.0) | |||
| 5–6 | 8 (2.2) | 359 (97.8) | 367 (100.0) | |||
| Occupational characteristics | ||||||
| Industry classification | < 0.001 | |||||
| Manufacturing | 112 (2.3) | 4,660 (97.7) | 4,772 (100.0) | |||
| Water, sewage and waste treatment, raw material recycling | 0 (0.0) | 20 (100.0) | 20 (100.0) | |||
| Construction industry | 0 (0.0) | 14 (100.0) | 14 (100.0) | |||
| Wholesale and retail | 2 (0.9) | 230 (99.1) | 232 (100.0) | |||
| Transport and warehousing | 56 (2.2) | 2,483 (97.8) | 2,539 (100.0) | |||
| Information and communication business | 0 (0.0) | 235 (100.0) | 235 (100.0) | |||
| Professional, scientific and technical services | 3 (0.9) | 338 (99.1) | 341 (100.0) | |||
| Business facility management, business support and rental service business | 31 (1.8) | 1,669 (98.2) | 1,700 (100.0) | |||
| Public administration, defense and social security administration | 2 (1.0) | 195 (99.0) | 197 (100.0) | |||
| Education service industry | 1 (2.6) | 37 (97.4) | 38 (100.0) | |||
| Health industry and social welfare service industry | 6 (0.5) | 1,196 (99.5) | 1,202 (100.0) | |||
| Associations and organizations, repair and other personal service businesses | 6 (0.5) | 1,276 (99.5) | 1,282 (100.0) | |||
| Size of the workplace | 0.011 | |||||
| Less than 300 | 87 (2.2) | 3,910 (97.8) | 3,997 (100.0) | |||
| 300 or more | 132 (1.5) | 8,443 (98.5) | 8,575 (100.0) | |||
| Characteristics | Disease absence | Total | ||||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| No. of subject | 410 (3.3) | 12,162 (96.7) | 12,572 (100.0) | |||
| Presenteeism | < 0.001 | |||||
| No | 174 (1.8) | 9,575 (98.2) | 9,749 (100.0) | |||
| Yes | 236 (8.4) | 2,587 (91.6) | 2,823 (100.0) | |||
| General characteristics | ||||||
| Sex | 0.378 | |||||
| Male | 303 (3.2) | 9,219 (96.8) | 9,522 (100.0) | |||
| Female | 107 (3.5) | 2,943 (96.5) | 3,050 (100.0) | |||
| Age (yr) | 0.265 | |||||
| < 30 | 75 (3.9) | 1,869 (96.1) | 1,944 (100.0) | |||
| 30–39 | 126 (3.4) | 3,611 (96.6) | 3,737 (100.0) | |||
| 40–49 | 109 (3.0) | 3,490 (97.0) | 3,599 (100.0) | |||
| 50–59 | 96 (3.2) | 2,947 (96.8) | 3,043 (100.0) | |||
| > 59 | 4 (1.6) | 245 (98.4) | 249 (100.0) | |||
| Chronic disease | 0.639 | |||||
| No | 337 (3.2) | 10,115 (96.8) | 10,452 (100.0) | |||
| Yes | 73 (3.4) | 2,047 (96.6) | 2,120 (100.0) | |||
| Smoking | < 0.001 | |||||
| Never smoker | 146 (2.8) | 5,146 (97.2) | 5,292 (100.0) | |||
| Former smoker | 77 (2.7) | 2,742 (97.3) | 2,819 (100.0) | |||
| Current smoker | 187 (4.2) | 4,274 (95.8) | 4,461 (100.0) | |||
| Alcohol consumption (time/week) | 0.052 | |||||
| 0–2 | 320 (3.1) | 10,052 (96.9) | 10,372 (100.0) | |||
| 3–4 | 74 (4.0) | 1,759 (96.0) | 1,833 (100.0) | |||
| 5–6 | 16 (4.4) | 351 (95.6) | 367 (100.0) | |||
| Occupational characteristics | ||||||
| Industry classification | < 0.001 | |||||
| Manufacturing | 241 (5.1) | 4,531 (94.9) | 4,772 (100.0) | |||
| Water, sewage and waste treatment, raw material recycling | 0 (0.0) | 20 (100.0) | 20 (100.0) | |||
| Construction industry | 0 (0.0) | 14 (100.0) | 14 (100.0) | |||
| Wholesale and retail | 9 (3.9) | 223 (96.1) | 232 (100.0) | |||
| Transport and warehousing | 52 (2.0) | 2,487 (98.0) | 2,539 (100.0) | |||
| Information and communication business | 1 (0.4) | 234 (99.6) | 235 (100.0) | |||
| Professional, scientific and technical services | 17 (5.0) | 324 (95.0) | 341 (100.0) | |||
| Business facility management, business support and rental service business | 48 (2.8) | 1,652 (97.2) | 1,700 (100.0) | |||
| Public administration, defense and social security administration | 2 (1.0) | 195 (99.0) | 197 (100.0) | |||
| Education service industry | 2 (5.3) | 36 (94.7) | 38 (100.0) | |||
| Health industry and social welfare service industry | 26 (2.2) | 1,176 (97.8) | 1,202 (100.0) | |||
| Associations and organizations, repair and other personal service businesses | 12 (0.9) | 1,270 (99.1) | 1,282 (100.0) | |||
| Size of the workplace | 0.473 | |||||
| Less than 300 | 137 (3.4) | 3,860 (96.6) | 3,997 (100.0) | |||
| 300 or more | 273 (3.2) | 8,302 (96.8) | 8,575 (100.0) | |||
| Presenteeism | Injury absence | Disease absence | ||||
|---|---|---|---|---|---|---|
| Unadjusted OR (95% CI) | Adjusted ORa (95% CI) | Adjusted ORb (95% CI) | Unadjusted OR (95% CI) | Adjusted ORa (95% CI) | Adjusted ORb (95% CI) | |
| No | 1 | 1 | 1 | 1 | 1 | 1 |
| Yes | 2.456 (1.870–3.225) | 2.996 (2.260–3.971) | 2.705 (2.044–3.581) | 5.020 (4.108–6.135) | 5.176 (4.227–6.338) | 4.906 (3.996–6.024) |
| Variables | Men | Women | |||||
|---|---|---|---|---|---|---|---|
| Unadjusted OR (95% CI) | Adjusted ORa (95% CI) | Adjusted ORb (95% CI) | Unadjusted OR (95% CI) | Adjusted ORa (95% CI) | Adjusted ORb (95% CI) | ||
| Injury absence | |||||||
| Presenteeism | |||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | |
| Yes | 3.387 (2.532–4.530) | 3.204 (2.391–4.293) | 3.035 (2.258–4.081) | 1.115 (0.499–2.490) | 1.336 (0.588–3.032) | 1.322 (0.577–3.028) | |
| Disease absence | |||||||
| Presenteeism | |||||||
| No | 1 | 1 | 1 | 1 | 1 | 1 | |
| Yes | 5.990 (4.747–7.559) | 5.740 (4.543–7.253) | 5.508 (4.340–6.989) | 3.601 (2.388–5.430) | 3.629 (2.405–5.475) | 3.629 (2.405–5.475) | |
Values are presented as number (%).
a
Values are presented as number (%).
a
Values are presented as number (%).
a
OR: odds ratio, CI: confidence interval.
aORs were calculated by logistic regression analysis for absence due to injury or disease after adjusting for sex, age, chronic disease, smoking, and alcohol consumption.
bORs were calculated by logistic regression analysis for absence due to injury or disease after adjusting for sex, age, chronic disease, smoking, alcohol consumption, industry classification, and workplace size.
OR: odds ratio, CI: confidence interval.
aORs were calculated by logistic regression analysis for absence due to injury or disease after adjusting for age, chronic disease, smoking, and alcohol consumption.
bORs were calculated by logistic regression analysis for absence due to injury or disease after adjustment for age, chronic disease, smoking, alcohol consumption, industry classification, and workplace size.
 KSOEM
KSOEM

 Cite
Cite

