Abstract
-
Background
Injuries caused by humidifier disinfectants (HDs) can no longer be grouped under the concept of HD lung injury. Focusing on individual cases, we were able to evaluate the relevance not only of diseases for which epidemiological correlation is recognized but also all diseases and symptoms that the victims complain of.
-
Methods
In-depth interviews and reassessment of 113 HD-exposed patients who had not been acknowledged as victims by the government were conducted, and their medical records were reviewed. Based on these processes, an assessment questionnaire for the injuries related to HDs was completed and the involvement of HDs was assessed either as “strong association,” “association,” or “no association.”
-
Results
In this study, of the 113 patients included who claimed damages, 78 (69.0%) had HD-related injuries. Among the cases of 22 patients who applied for injury acknowledgment due to upper respiratory inflammation that was not included among the acknowledged diseases, 17 (77.3%) were judged to be HD-related injuries (strong association vs. association: 10 [45.5%] vs. 7 [31.8%]). When the cases of 12 rhinitis patients were reassessed, 9 were HD-related injuries (strong association vs. association: 4 [33.3%] vs. 5 [41.7%]). When the cases of 18 asthma patients unacknowledged as a victim were reassessed, 17 (94.4%) were humidifier-related injuries (strong association vs. association: 12 [66.6%] vs. 5 [27.8%]). Among 4 interstitial lung disease patients unacknowledged as a victim, 2 (50.0%) were HD-related injuries.
-
Conclusions
HD-related health injuries should be assessed through both individual interviews and detailed chart reviews for more accurate injury acknowledgment. In the future, efforts should go beyond existing methods based on the adherence to acknowledgment criteria to directly listen to the victims.
-
Keywords: Humidifier disinfectant; Humidifier disinfectant lung injury (HDLI); Humidifier disinfectant related health injury
BACKGROUND
Since humidifier disinfectants (HDs) were identified as the cause of unknown lung disease in 2011, many of the victims have complained of various types of related injuries. In a recent study, it was estimated that 8.94 million people were exposed to HDs and 0.95 million people experienced adverse health effects, which translates to approximately 1 in 5 and 1 in 50 Koreans respectively.
1 Nevertheless, there is still a lack of understanding of the injuries caused by exposure to HDs. A total of 7,419 Korean patients have applied for injury acknowledgment due to HD exposure (as of April 16, 2021). However, the government has acknowledged only 4,114 (55.5%) of these patients.
2 Thus, the real size of the affected population remains unclear, and the acknowledgment rate remains low.
1 There has been persistent criticism of the narrow criteria used for injury acknowledgment.
As time passes since the ban on the use of HDs, the evidence of HDs related injuries has been diminishing and the past medical records are also being lost and destroyed because of the closure of small clinics and storage period mandated by law. The previous process of identifying HDs injury does not consider the overall circumstances involved in the exposure of each individual victim but depends only on the past medical records, since the decision was to acknowledge injury based solely on adherence to the HD lung injury (HDLI) diagnostic criteria.
3 The limitations of this process are that the patient was evaluated only through a medical record review without an individual interview. The submitted medical records are often incomplete. Additionally, because some patients ignore or forget which hospital, they received treatment in medical records are hard to place. Therefore, individual interviews with each patient are a better way to investigate their situation at the time of exposure and the subsequent clinical situations. Although objections to the aforementioned process have been raised repeatedly, several victims are still unable to receive injury acknowledgment.
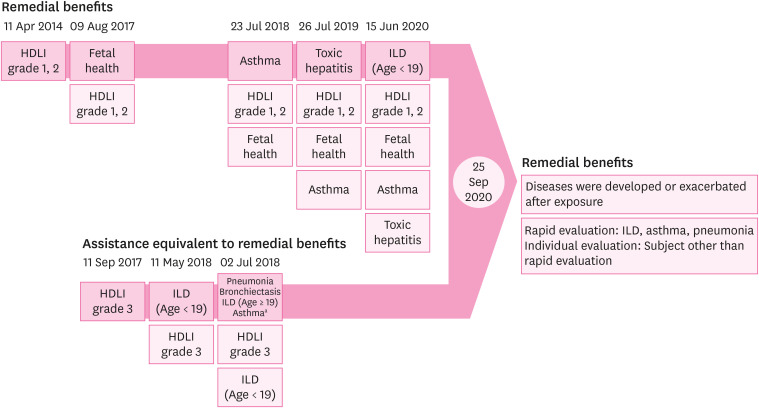
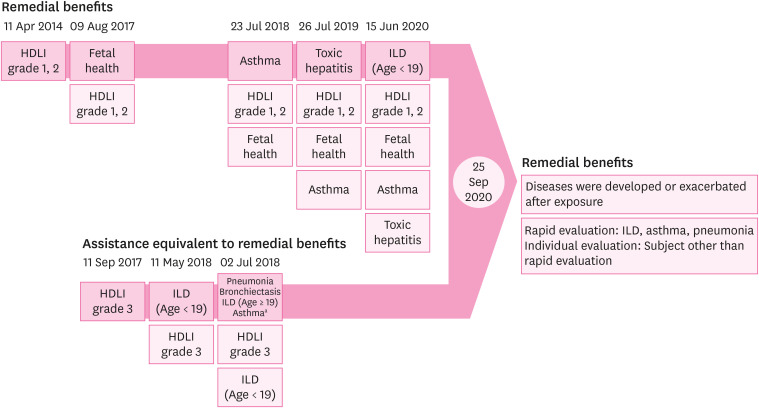
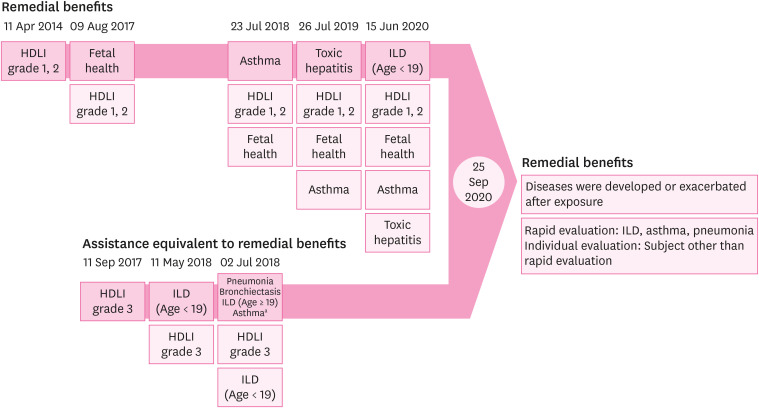
4 In the Special Act on Remedy for Damage Caused by Humidifier Disinfectants, the government defined victims as patients that were acknowledged by either remedial benefits or assistance equivalent to remedial benefits. The scope of recognized HD-related injuries was expanded from HDLI (HDLI decision definite, probable) to include asthma, fetal injury, toxic hepatitis, interstitial lung disease (ILD), bronchiectasis, and pneumonia.
5 Diseases that developed or were exacerbated after exposure as well as those with a confirmed epidemiological association with HDs exposure were also included (
Fig. 1).
5,6 Assessment based on the revised Special Act on Remedy for Damage Caused by Humidifier Disinfectants is conducted as a rapid evaluation of the meeting of specific criteria
7; no individualized evaluations are made to allow for a more in-depth, case-by-case analysis. Under this scheme, exposure investigation data are used only to determine the timing of diagnosis after exposure for each disease and its accuracy. Although the subject that is not conducted as a rapid evaluation should be conducted as individual evaluation, it has not been carried into execution until now.
7
Fig. 1
Expansion history of humidifier disinfectant-related injuries acknowledged by government.
HDLI: humidifier disinfectant lung injury; ILD: interstitial lung disease.
aThe asthma other than asthma recognized as a relief benefits.
There are a number of epidemiological
8,9,10,11,12,13 and toxicological
14,15,16,17 studies to assess the causal relationship of HDs exposure with HDLI.
10,11,12,13,16,17 There are also several studies on asthma showing causality.
18,19,20 However, little is known about other non-specific respiratory injuries.
21 Judgment on injury due to HDs should be based not only on whether the patient meets certain criteria for acknowledgment but also on the diverse clinical circumstances experienced by each individual victim. To this end, it is crucial that the principles for acknowledging the health injuries of exposure to HDs be expanded to cases in which exposure to HDs is substantially likely to be a significant factor in aggravating, contributing to, or causing the illnesses or health conditions.
7
This study aimed to investigate the proportion of people classified as victims of injury due to HD exposure and their characteristics, by evaluating the relevance of exposure to HDs through individual victim-based evaluation in those unacknowledged as victims by the government. In this way, we would like to investigate the benefits of individual-based evaluation when assessing the relevance not only of diseases for which epidemiological correlation is recognized but also all diseases and symptoms that victims complain of.
METHODS
Among those applying for acknowledgment of injury due to HDs, we identified 533 patients confirmed to have been exposed to HDs (via the Humidifier Disinfectant Public Health Center) and who had been allocated to Kangbuk Samsung Hospital for the monitoring of HD victims' health. The 533 qualifying patients were sent instructions for testing by post, after which their intent to participate was confirmed by individual phone calls. Of these, 200 patients (37.5%) had visited the hospital and participated in an in-depth interview. The final study population of 113 patients (56.5%) included those who were unacknowledged as victims by the government. Reasons for exclusion were having been acknowledged already as victims by the government, had health problems, changed the monitoring institution, did not have enough time to participate, did not require additional treatment based on the follow-up outcome at another institution, lived a long distance away, and failure to respond to contact.
For each patient, the claimed diseases/symptoms and HDs-related injury status were checked by chart review, and the patient was subjected to health monitoring examinations, such as lung function tests, high-resolution computed tomography, and blood tests (complete blood count, liver function tests, lipid profile, and others for the purpose of providing health care services, including hemoglobin levels used to correct lung diffusion capacity). The initial interviews were performed by a resident in the Occupational & Environmental Medicine department and all patients were also subjected to a second interview by an attending physician in the same department. Subsequently, the results of the interviews conducted by 4 residents and 1 attending physician were verified by evaluating the relevance of the HD-related injury as the result of agreement of all 5 physicians. Using an HD injury assessment questionnaire (
Table 1), each case was assessed by 4 residents using the same method and the association with HDs was rated as “strong association,” “association,” or “no association” using the same algorithm.
Table 1 Association between humidifier disinfectant exposure and health injury assessment questionnaire
|
Questions |
Contents |
|
A |
There was a disease/symptom related to the claimed disease prior to exposure. |
|
A1 |
Symptom/disease worsened while using humidifier disinfectant. |
|
A2 |
The causal relationship is medically explainable. |
|
A3 |
It is confirmed as an objective evidence. |
|
A4 |
The person's statement is consistent and reliable. |
|
B |
There was a disease/symptom related to the claimed disease during exposure. |
|
B1 |
Symptom/disease improved after the exposure was stopped. |
|
B2 |
The causal relationship is medically explainable. |
|
B3 |
It is confirmed as an objective evidence. |
|
B4 |
The person's statement is consistent and reliable. |
|
C |
The symptom/disease related to the claimed disease occurred or worsened after the exposure was stopped. |
|
C1 |
Incubation period of the claimed disease occurred after the exposure was stopped. |
|
C2 |
The causal relationship is medically explainable. |
|
C3 |
It is confirmed as an objective evidence. |
|
C4 |
The person's statement is consistent and reliable. |
We developed the HD injury assessment questionnaire with reference to the Hill criteria, including temporality, plausibility, and coherence (with existing knowledge), that are used to establish causality (
Table 1).
22 Temporality refers to the temporal order of exposure to HDs and claimed diseases/symptoms, and was assessed by whether the disease/symptoms developed during or after exposure (question B and C) or, in the event of an existing disease, whether the diseases/symptoms worsened after exposure (question A and A1). In the event of a disease/symptom that developed during the period of exposure, we assessed whether the diseases/symptom improved after the exposure ceased (question B1).
Plausibility was assessed by whether exposure to HDs and the diseases/symptoms could be explained medically (question A2, B2, and C2) and, in the event of a disease/symptom that developed after stopping the exposure, by assessing the time from the start/end of exposure to diagnosis (question C1). To assess coherence with existing knowledge, we reviewed previous studies on human who were exposed to HDs and the results of animal experiments.
The reliability of the applicants' claims during the interview was assessed. If the applicant's claims satisfied the conditions described above (temporality, plausibility, and coherence) and could be verified by objective data (previous medical records among others; question A3, B3, and C3), this was categorized as “strong association.” If, while satisfying the above conditions, the applicant's claims could not be verified by objective data, but the statements were consistent and judged to be credible (question A4, B4, and C4), this was categorized as “association.” If the applicant's claims did not satisfy the conditions described above, this was categorized as “no association.” Statements were judged to be consistent and reliable if the record of the investigator in exposure assessment, the statement in the HDLI evaluation, the statement in past health monitoring, and the statement in the current year's health monitoring matched each other. The combination of various factors was considered during the interview, including the presence or absence of HD victims among the patient's family and exposure characteristics, such as the duration and frequency of HD use.
Ethics statement
The study was approved by the Institutional Review Board of Kangbuk Samsung Hospital (approval NO. KBSMC 2018-10-024). Written informed consent forms were signed by the patients.
RESULTS
Of the 533 patients allocated to our hospital for health monitoring, we interviewed 200 patients, with a participation rate of 37.5% (
Table 2). Of the 200 patients, 3 (1.5%), 8 (4.0%), 8 (4.0%), and 173 (86.5%), had HDLI decision definite, probable, possible, and unlikely, respectively and 8 (4.0%) were indeterminate. 28 (14.0%) patients with HD-related injuries were acknowledged for asthma. 50 (25.0%) patients' injuries could be acknowledged for assistance equivalent to remedial benefits that could be granted to 1 patient for several diseases. Excluding duplicates, we identified 27 (13.5%) cases of pneumonia, 14 (7.0%) cases of bronchiectasis, 11 (5.5%) cases of ILD, 5 (2.5%) cases of asthma, and 5 (2.5%) cases of HDLI decision possible. Excluding all the patients with duplicate acknowledgments, 87 (43.5%) patients were acknowledged as victims by the government and 113 (56.5%) patients were not. However, when we conducted individual interviews and reassessed the applicants at our hospital during the health monitoring procedure, we identified 159 (79.5%) patients who were judged to have had injuries due to HDs.
Table 2 Characteristics of the monitored patients
|
Category |
Number of patients |
Proportion (%) |
|
Association of humidifier disinfectant-related health injuries |
|
|
|
Strong association |
118 |
59.0 |
|
Association |
41 |
20.5 |
|
No association |
41 |
20.5 |
|
Age at diagnosis (years) |
|
|
|
< 1 |
19 |
9.5 |
|
1–20 |
49 |
24.5 |
|
21–40 |
59 |
29.5 |
|
41–60 |
56 |
28.0 |
|
> 60 |
15 |
7.5 |
|
Unknown |
2 |
1.0 |
|
Sex |
|
|
|
Male |
103 |
51.5 |
|
Female |
97 |
48.5 |
|
HDLI decision |
|
|
|
Definite |
3 |
1.5 |
|
Probable |
8 |
4.0 |
|
Possible |
8 |
4.0 |
|
Unlikely |
173 |
86.5 |
|
Indeterminate |
8 |
4.0 |
|
Asthma decision |
|
|
|
Acknowledged |
28 |
14.0 |
|
Unacknowledged |
142 |
71.0 |
|
Indecision |
30 |
15.0 |
|
Assistance equivalent to remedial benefits |
|
|
|
Pneumonia |
27 |
13.5 |
|
Bronchiectasis |
14 |
7.0 |
|
Interstitial lung disease |
11 |
5.5 |
|
Asthma |
5 |
2.5 |
|
HDLI possible |
5 |
2.5 |
|
Acknowledged as a victim of humidifier disinfectant |
|
|
|
Acknowledged |
87 |
43.5 |
|
Unacknowledged |
113 |
56.5 |
Through in-depth interviews with 113 patients whose injuries were unacknowledged using the HD-related injury assessment questionnaire, we analyzed the disease/symptom cited for applying for injury acknowledgment due to HDs (
Table 3). The claimed diseases of patients whose injuries were unacknowledged included upper respiratory inflammation (URI) for 22 patients (19.5%), asthma for 18 patients (15.9%), and rhinitis for 12 patients (10.6%). There were 19 patients (16.8%) who claimed injury based on respiratory symptoms alone, such as cough.
Table 3 Categories of those unacknowledged as victims of humidifier disinfectant
|
Health injury |
Association of humidifier disinfectant-related health injuries |
|
Total |
Overall association |
Strong association |
Association |
No association |
|
URI |
22 |
17 (77.3) |
10 (45.5) |
7 (31.8) |
5 (22.7) |
|
Asthma |
18 |
17 (94.4) |
12 (66.6) |
5 (27.8) |
1 (5.6) |
|
Respiratory symptom |
19 |
18 (94.7) |
3 (15.8) |
15 (78.9) |
1 (5.3) |
|
Rhinitis |
12 |
9 (75.0) |
4 (33.3) |
5 (41.7) |
3 (25.0) |
|
Pneumonia |
7 |
7 (100.0) |
7 (100.0) |
0 (0.0) |
0 (0.0) |
|
ILD |
4 |
2 (50.0) |
2 (50.0) |
0 (0.0) |
2 (50.0) |
|
COPD |
4 |
3 (75.0) |
2 (50.0) |
1 (25.0) |
1 (25.0) |
|
Lung cancer |
4 |
0 (0.0) |
0 (0.0) |
0 (0.0) |
4 (100.0) |
|
Tuberculosis |
3 |
0 (0.0) |
0 (0.0) |
0 (0.0) |
3 (100.0) |
|
Bronchiectasis |
2 |
1 (50.0) |
1 (50.0) |
0 (0.0) |
1 (50.0) |
|
Radiologic abnormality |
2 |
0 (0.0) |
0 (0.0) |
0 (0.0) |
2 (100.0) |
|
NTM |
1 |
0 (0.0) |
0 (0.0) |
0 (0.0) |
1 (100.0) |
|
HP |
1 |
1 (100.0) |
1 (100.0) |
0 (0.0) |
0 (0.0) |
|
Other disease |
13 |
3 (23.1) |
3 (23.1) |
0 (0.0) |
10 (76.9) |
|
No disease |
1 |
0 (0.0) |
0 (0.0) |
0 (0.0) |
1 (100.0) |
|
Total |
113 |
78 (69.0) |
45 (39.8) |
33 (29.2) |
35 (31.0) |
When we reassessed the 18 unacknowledged asthma patients, the 17 (94.4%) patients showed strong association or association (12 [66.6%] and 5 [27.8%], respectively). All 7 pneumonia patients (100.0%) showed strong association. Among the 22 patients who claimed injury for URI, which is not included among acknowledged diseases, 17 (77.3%) showed strong association or association with HD exposure (10 [45.5%] and 7 [31.8%], respectively).
When we reassessed the 12 rhinitis patients, 9 showed strong association (4 [33.3%]) or association (5 [41.7%]). Among 19 patients with respiratory symptoms, such as cough, sputum, or dyspnea but no specific disease, due to the lack of objective evidence, 3 (15.8%) showed a strong association, and 15 (78.9%) showed an association. For chronic obstructive pulmonary disease (COPD), although the assessed patients were few, 2 (50.0%) showed a strong association, 1 (25.0%) showed an association and 1 (25.0%) showed a no association. Lung cancer, tuberculosis, and nontuberculous mycobacteria were evaluated as having no association because of insufficient research results and lack of medical plausibility.
Other diseases included missed abortion, breast cancer, pneumoconiosis, angioedema, systemic fatigue, cerebral hemorrhage, lung abscess, hemoptysis due to Takayasu arteritis, pneumothorax, lymphangioleiomyomatosis, myasthenia gravis, developmental disorders, urticaria, and angina. Of these, the 3 diseases that showed a strong association with HDs were lung abscess, hemoptysis due to Takayasu arteritis, and pneumothorax. We could determine that it had exacerbated or contributed to their development, rather than HDs causing these diseases.
Of the 18 asthma patients whose injuries were unacknowledged, the 15 (83.3%) patients had symptoms during exposure but only 5 (27.8%) patients diagnosed asthma during exposure (
Table 4). Of the 9 patients who diagnosed asthma more than 2 years after stopping exposure, 7 patients experienced their symptoms during exposure (
Supplementary Table 1). Detailed characteristics of the asthma patients were shown in
Supplementary Tables 1 and
2.
Table 4 Characteristics of asthma those unacknowledged as victims of humidifier disinfectant
|
Category |
Number of patients |
Proportion (%) |
|
Association of humidifier disinfectant-related health injuries |
|
|
|
Strong association |
12 |
66.7 |
|
Association |
5 |
27.8 |
|
No association |
1 |
5.5 |
|
Symptom onset during exposure |
|
|
|
Yes |
15 |
83.3 |
|
No |
3 |
16.7 |
|
Diagnosis during exposure |
|
|
|
Yes |
5 |
27.8 |
|
No |
13 |
72.2 |
|
Exposure end (diagnosis period) |
|
|
|
< 2 years |
4 |
30.8 |
|
≥ 2 years |
9 |
69.2 |
When we reassessed the 4 unacknowledged patients with ILD, 2 (
Supplementary Table 3; #3 and #4) showed no association with HDs. Patient #3's HD exposure investigation was not reliable, and it was impossible to verify whether she had been exposed. Patient #4's exposure duration was too short (1 month) and it was not judged to induce ILD; however, there were findings that showed suspicion of usual interstitial pneumonia caused by exposure to silica, based on occupational history (
Supplementary Table 3).
None of the 4 lung cancer patients was acknowledged as a victim by the government and we also judged that these patients' diseases had no association with HDs, since there was insufficient scientific evidence to offer a medical explanation. Nevertheless, it is notable that 2 of these 4 patients were nonsmokers and nonsmoking patient #4 developed lung cancer at the young age of 31 (
Supplementary Table 4).
DISCUSSION
In this study, we conducted individual interviews to reassess patients who had not been acknowledged as victims of injury due to HDs by the government. We determined that 78 of 113 claimants (69.0%) had shown health injuries related to HDs. In particular, 17 of 78 patients (21.8%) and 9 of 78 patients (11.5%) had URI and rhinitis that had not previously been acknowledged by the government as HD-related injuries but were added in July 2020.
23 Of the 200 patients who participated in HD victims' health monitoring, 157 (78.5%) could be identified as victims when reassessed. This is much higher than the 87 (43.5%) originally acknowledged by the government.
Recently, the Panel Study on Korean Children reported a correlation between the use of HDs and diagnosis of allergic rhinitis,
12,24 and also revealed a correlation with upper respiratory disease, which is a precursor to lower respiratory disease.
12 In addition to respiratory disease, there have also been experimental results demonstrating the possibility of systemic toxic effects.
25 Moreover, it has been suggested that the various adverse health effects associated with HDs should be called Humidifier Disinfectant Syndrome.
26 Currently, the injuries caused by HDs are expanding into the field of mental health and this contributes to the illogical nature of the existing victim classification system.
27,28 This demonstrates the need to expand the list of acknowledged HD-related injuries in a bid to assess individual's claims by conducting individual-based evaluation to listen to the victim's account and to comprehensively assess their diseases.
One advantage of this study is that, through the HD victims' health monitoring program, we conducted individual interviews and chart reviews for 200 patients and recorded their statements. In previous studies, researchers did not conduct individual patient interviews but only reviewed the submitted medical records and applied strict criteria to identify lung diseases related to HDs.
3,29,30,31
Through assessment using our HD-related health injury questionnaire, 157 (78.5%) patients of 200 were judged to have experienced health injuries related to HDs. Asthma and pneumonia showed high rates of association with HDs (asthma: 94.4%; pneumonia: 100.0%). This high rate of association was possible because we assessed only whether a disease was caused by HDs, but also whether HDs contributed to the development of disease or exacerbated an existing disease.
In the case of mild diseases such as rhinitis URI, and respiratory symptoms, because many patients received treatment at primary medical institutions, past medical records were often missing.
32 As a result, some patients in this group showed an association, rather than a strong association, which requires a certain level of objective evidence. However, it is worth paying attention to the fact that even victims with such mild diseases/symptoms experienced respiratory symptoms caused by HDs. We believe that more patients would show a strong association if data from the National Health Insurance Service were used.
Because the existing acknowledgement criteria for asthma stated that HD-related asthma had to have developed within 2 years of stopping exposure, there were gaps between acknowledged and unacknowledged asthma patients.
33 There were many instances of patients who exhibited mild symptoms during HD use but did not visit a medical institution or, if they visited the hospital, did not undergo lung function tests, meaning that asthma was not diagnosed, and the patients' injuries were unacknowledged. In this study we could find out the association between the disease and exposure to HDs in unacknowledged asthma patients. Although asthma patients had started symptoms during exposure, they were diagnosed asthma after the exposure ceased. Because we investigated the several related facts, such as the onset time of the symptoms after the start of HDs usage and a treatment history at a medical institution, we were able to identify an association even for asthma cases that developed more than 2 years after stopping exposure. Individual-based evaluation is not only used to confirm the presence or absence of exposure, exposure period, and duration until diagnosis after discontinuation of exposure but also to confirm whether symptoms occurred during exposure. Through individual-based evaluation, we can confirm that these symptoms are a manifestation of the development of disease.
ILD is a generic term for various diseases accompanied by inflammation and fibrosis of the pulmonary interstitial space by various causes. Even if ILD is comprehensively acknowledged by the government, a multidisciplinary approach is needed to consider the characteristics of each patient's HDs exposure. In previous assessment methods, exposure investigations are only used to confirm exposure. Therefore, it is difficult to evaluate the reliability of exposure and possibility of disease occurrence depending on the duration of exposure.
Because it is not proved about the association between HDs exposure and lung cancer, lung cancer patients until now were all judged to show no association. Recently, a study in rats on the occurrence of lung cancer due to polyhexamethylene guanidine (PHMG) exposure reported that PHMG exposure increases the expression of lung cancer-related genes and histological changes to tumors.
34 Since lung cancer takes a long time to develop, long term follow-up and further research are needed.
This study had some limitations. First, this study does not intend to demonstrate causation between health injury and HDs. The strict existing remedy for damage which acknowledged victims based on causation has been criticized a lot.
35,36,37 Given that the scope of HD health injuries is not precisely known at present, selecting victims based on causation would not cover the real victims. Therefore, we focused on the association instead of causation. Second, because each resident interviewed the patients independently, although adjustments could be made through the second interview with an attending physician and discussion, it was still difficult to ensure unanimous objectivity. We used an assessment questionnaire to ensure more objective assessments. Third, there is a risk of selection bias, in which injury claimants who visit for HD victims' health monitoring may be more likely to be people who perceive themselves as victims but who had not been acknowledged. In addition, there is a limit to comparing the differences between participants and non-participants because it is not possible to investigate the characteristics of non-participants. Nevertheless, the acknowledgment rate among the participants was 43.5% (87 of 200), while the rate among non-participants was 41.4% (138 of 333), which was not significantly different (
p = 0.141). Fourth, because patients voluntarily applied for health injuries acknowledgment, there may be a recall bias due to the desire for damage acknowledgment. We tried to review the medical records to make the assessment of victims more objective. Nevertheless, there are many victims who experienced mild symptoms in the past that did not lead to actual medical visits. We considered it meaningful, even if it was mild damage that was not confirmed by objective data. As for as we know, the severity of the disease is a different scope from the judgment of its relevance.
The revised Special Act on Remedy for Damage Caused by Humidifier Disinfectants expanded the definition of HD-related health injury in article 2 to include injury caused or exacerbated by exposure to HDs.
6 In addition, in article 5, it is stated that causation can be assumed in cases where there is an epidemiological association between HD exposure and a disease that developed or was exacerbated after exposure, provided that the responsible company cannot demonstrate that the injury had a different underlying cause.
6 In this study, we assessed injury claimants according to the definition of health injury in the revised Special Act on Remedy for Damage Caused by Humidifier Disinfectants. Thus, as shown by the results of our investigation, we anticipate that a considerable number of previously unacknowledged applicants will be able to have their injuries acknowledged due to the expanded scope of HD-related injuries defined in the revised act through individual-based evaluation.
No previous studies have collected individual interview data for HD-related health injury claimants and assessed the association with HD exposure for each patient. Therefore, we believe that our study has considerable value as the first of its kind. Our study will help with future decisions regarding individual health injury victims.
CONCLUSIONS
Through individual-based evaluation, various HD-related health injuries by the previous criteria, such as respiratory symptoms and upper respiratory disease were found that were not covered by the criteria for the previous acknowledgment criteria. HDs-related health injuries cannot be accurately assessed without conducting individual interviews and detailed chart reviews for each claimant because of the various circumstances of individual victims. Accurate assessment requires both the review of medical records and personal interviews. In the future, efforts should go beyond existing methods based on the adherence to acknowledgment criteria to directly listen to the victims.
Abbreviations
acute respiratory distress syndrome
bronchiolitis obliterans organizing pneumonia
chronic obstructive pulmonary disease
humidifier disinfectant lung injury
hypersensitivity pneumonitis
interstitial lung disease
interstitial pulmonary fibrosis
non-specific interstitial pneumonia
nontuberculous mycobacteria
polyhexamethylene guanidine
upper respiratory inflammation
NOTES
-
Funding: Humidifier disinfectant victims' health monitoring was funded by the National Institute of Environmental Research of Korea.
-
Competing interests: The authors declare that they have no competing interests.
-
Author Contributions:
Conceptualization: Kim HC, Park S.
Investigation: Kim HC, Kim H, Lee Y, Mun E.
Writing - original draft: Kim HC, Park S.
Writing - review & editing: Kim H, Lee Y, Mun E.
SUPPLEMENTARY MATERIALS
REFERENCES
REFERENCES
- 1. Byeon J, Kim HS, Park MY, Lee KM, Hong MG, Choi YY. An estimation of population at risk of exposure to humidifier disinfectant and associated health effects. J Environ Health Sci 2020;46(4):457–469.
- 2. Korea Environmental Industry & Technology Institute. Humidifier disinfectant damage support portal statistics of victims. Updated 2021]. Accessed August 19, 2020]. https://www.healthrelief.or.kr/home/content/stats01/view.do.
- 3. Paek D, Koh Y, Park DU, Cheong HK, Do KH, Lim CM, et al. Nationwide study of humidifier disinfectant lung injury in South Korea, 1994–2011. Incidence and dose-response relationships. Ann Am Thorac Soc 2015;12(12):1813–1821. 26653190.ArticlePubMed
- 4. Choi JE, Hong SB, Do KH, Kim HJ, Chung S, Lee E, et al. Humidifier disinfectant lung injury, how do we approach the issues? Environ Health Toxicol 2016;31:e2016019. 27608716.ArticlePubMedPMCPDF
- 5. Ministry of Environment. Special act on remedy for damage cause by humidifier disinfectants. Updated 2019]. Accessed August 19, 2020]. https://www.law.go.kr/LSW/lsInfoP.do?lsiSeq=204194&urlMode=engLsInfoR&viewCls=engLsInfoR#0000.
- 6. Ministry of Environment. Special act on remedy for damage caused by humidifier disinfectants. Updated 2020]. Accessed August 19, 2020]. https://www.law.go.kr/LSW/lsInfoP.do?lsiSeq=215909&efYd=20200925&ancYnChk=0#0000.
- Ministry of Environment. Notification of decision on payment of relief benefits for humidifier disinfectants. Updated 2020]. Accessed November 10, 2020]. https://www.law.go.kr/LSW/admRulLsInfoP.do?admRulSeq=2100000193149.
- 8. Kim HJ, Lee MS, Hong SB, Huh JW, Do KH, Jang SJ, et al. A cluster of lung injury cases associated with home humidifier use: an epidemiological investigation. Thorax 2014;69(8):703–708. 24488371.PubMed
- 9. Park JH, Kim HJ, Kwon GY, Gwack J, Park YJ, Youn SK, et al. Humidifier disinfectants are a cause of lung injury among adults in South Korea: a community-based case-control study. PLoS One 2016;11(3):e0151849. 26990641.ArticlePubMedPMC
- 10. Ha M, Lee SY, Hwang SS, Park H, Sheen S, Cheong HK, et al. Evaluation report on the causal association between humidifier disinfectants and lung injury. Epidemiol Health 2016;38:e2016037. 27733036.ArticlePubMedPMC
- 11. Yoon J, Cho HJ, Lee E, Choi YJ, Kim YH, Lee JL, et al. Rate of humidifier and humidifier disinfectant usage in Korean children: a nationwide epidemiologic study. Environ Res 2017;155:60–63. 28189074.ArticlePubMed
- 12. Yon DK, Lee SW, Woo A, Koh HY, Jee HM, Ha EK, et al. Exposure to humidifier disinfectants is associated with upper and lower airway diseases. Pediatr Allergy Immunol 2020;31(5):578–582. 32068913.ArticlePubMedPDF
- 13. Yang HJ, Kim HJ, Yu J, Lee E, Jung YH, Kim HY, et al. Inhalation toxicity of humidifier disinfectants as a risk factor of children's interstitial lung disease in Korea: a case-control study. PLoS One 2013;8(6):e64430. 23755124.ArticlePubMedPMC
- 14. Park S, Lee K, Lee EJ, Lee SY, In KH, Kim HK, et al. Humidifier disinfectant-associated interstitial lung disease in an animal model induced by polyhexamethylene guanidine aerosol. Am J Respir Crit Care Med 2014;190(6):706–708. 25221883.ArticlePubMed
- 15. Park DU, Friesen MC, Roh HS, Choi YY, Ahn JJ, Lim HK, et al. Estimating retrospective exposure of household humidifier disinfectants. Indoor Air 2015;25(6):631–640. 25557769.ArticlePubMedPMC
- 16. Song JA, Park HJ, Yang MJ, Jung KJ, Yang HS, Song CW, et al. Polyhexamethyleneguanidine phosphate induces severe lung inflammation, fibrosis, and thymic atrophy. Food Chem Toxicol 2014;69:267–275. 24769016.ArticlePubMed
- 17. Buxbaum A, Kratzer C, Graninger W, Georgopoulos A. Antimicrobial and toxicological profile of the new biocide Akacid plus. J Antimicrob Chemother 2006;58(1):193–197. 16751199.PubMed
- 18. Yoon J, Lee SY, Lee SH, Kim EM, Jung S, Cho HJ, et al. Exposure to humidifier disinfectants increases the risk for asthma in children. Am J Respir Crit Care Med 2018;198(12):1583–1586. 30192634.ArticlePubMedPMC
- 19. Lee SY, Ahn HS, Kim EM, Kim KK, Kang MJ, Park MJ, et al. Different characteristics of childhood asthma related to polyhexamethylene guanidine hydrochloride (PHMG) exposure. Ann Am Thorac Soc Forthcoming. 2021.
- 20. Yon DK, Lee SW, Woo A, Koh HY, Jee HM, Ha EK, et al. Exposure to humidifier disinfectants is associated with upper and lower airway diseases. Pediatr Allergy Immunol 2020;31(5):578–582. 32068913.ArticlePubMedPDF
- 21. Leem JH, Joh JS, Hong YS, Kim J, Park S, Lim S, et al. Characteristics of a new respiratory syndrome associated with the use of a humidifier disinfectant: humidifier disinfectant-related respiratory syndrome (HDRS). Int J Occup Med Environ Health 2020;33(6):829–839. 33052143.ArticlePubMed
- 22. Hill AB. The environment and disease: association or causation? 1965. J R Soc Med 2015;108(1):32–37. 25572993.ArticlePubMedPMCPDF
- 23. Ministry of Environment. 11 Additional humidifier disinfectant victims recognized 930 total. Updated 2020]. Accessed August 17, 2020]. http://www.me.go.kr/home/web/board/read.do;jsessionid=bLEFTAsRrXi-CzBbSgtOz2fY.mehome1?pagerOffset=0&maxPageItems=10&maxIndexPages=10&searchKey=&searchValue=&menuId=286&orgCd=&boardId=1384220&boardMasterId=1&boardCategoryId=39&decorator=.
- 24. Koh TH, Park JT, Kwon D, Kwak K. Association between use of humidifier disinfectant and allergic rhinitis in Korean children: a cross-sectional study based on the eighth Panel Study on Korean Children (PSKC). Ann Occup Environ Med 2020;32(1):e9. 32161652.ArticlePubMedPMCPDF
- 25. Leem JH, Kim HC. Mitochondria disease due to humidifier disinfectants: diagnostic criteria and its evidences. Environ Anal Health Toxicol 2020;35(2):e2020007. 32693559.ArticlePubMedPMCPDF
- 26. Leem JH, Lee JH. Humidifier disinfectant-associated specific diseases should be called together as “humidifier disinfectant syndrome”. Environ Health Toxicol 2017;32:e2017017. 29026061.ArticlePubMedPMCPDF
- 27. Lee YS, Nam MW, Kim HI, Kim HC, Mun EC, Park SY. Mental health impact on a humidifier disinfectant disaster victim: a case report. Ann Occup Environ Med 2020;32(1):e15. 32676193.ArticlePubMedPMCPDF
- 28. Yoo S, Sim M, Choi J, Jeon K, Shin J, Chung S, et al. Psychological responses among humidifier disinfectant disaster victims and their families. J Korean Med Sci 2019;34(4):e29. 30686951.ArticlePubMedPMCPDF
- 29. Kim S, Paek D. Humidifier disinfectant disaster: what is known and what needs to be clarified. Environ Health Toxicol 2016;31:e2016025. 28111422.ArticlePubMedPDF
- 30. Park D, Leem J, Lee K, Lim H, Choi Y, Ahn JJ, et al. Exposure characteristics of familial cases of lung injury associated with the use of humidifier disinfectants. Environ Health 2014;13(1):70. 25178403.ArticlePubMedPMCPDF
- 31. Lee E, Lee SY, Hong SJ. The past, present, and future of humidifier disinfectant-associated interstitial lung diseases in children. Clin Exp Pediatr 2020;63(7):251–258. 32024320.ArticlePubMedPMCPDF
- 32. Ministry of Health and Welfare. Medical Service Use Status as of 2019. Sejong, Korea: Ministry of Health and Welfare; 2021.
- 33. Ministry of Environment. Notification of decision on payment of relief benefits for humidifier disinfectants. Updated 2018]. Accessed November 10, 2020]. https://www.law.go.kr/LSW/admRulLsInfoP.do?admRulSeq=2100000140210.
- 34. Kim C, Jeong SH, Kim J, Lee KY, Cha J, Lee CH, et al. Evaluation of polyhexamethylene guanidine-induced lung injuries by chest CT, pathologic examination, and RNA sequencing in a rat model. Sci Rep 2021;11(1):6318. 33737587.ArticlePubMedPMCPDF
- 35. Asian Citizen's Center for Environment and Health. Change humidifier disinfectant injury acknowledgment criteria like this, complement the damage relief act and pass the National Assembly of the Republic of Korea. Updated 2017]. Accessed April 28, 2021]. http://eco-health.org/bbs/board.php?bo_table=sub02_02&wr_id=622.
- 36. Choi Y. A new approach for the relation criteria. Updated 2017]. Accessed April 28, 2021]. http://weekly.khan.co.kr/khnm.html?mode=view&dept=115&art_id=201702071123451.
- 37. Jeon SY. A terrible tragedy brought about by lies. Updated 2021]. Accessed April 28, 2021]. https://www.ntoday.co.kr/news/articleView.html?idxno=77485.
 , Hyunil Kim
, Hyunil Kim , Eun-Chan Mun
, Eun-Chan Mun , Yesung Lee
, Yesung Lee , Soyoung Park
, Soyoung Park


 KSOEM
KSOEM

 Cite
Cite

