Abstract
-
Background
Rhinitis was the most frequently diagnosed disorder among users of humidifier disinfectants (HDs). The aim of our study was to investigate on the relationship between allergic rhinitis (AR) and HD uses.
-
Methods
Our study used the data from the eighth Panel Study on Korean Children; a total of 1,540 participants were enrolled. The χ2 test and multiple logistic regression analyses were conducted to debunk the association between AR and HD uses.
-
Results
In our analysis, odds ratios (ORs) of doctor-diagnosed AR increased significantly when simply the response of whether HDs were used in the past was considered. When the brands of HD were considered, ORs of doctor-diagnosed AR were found to be increased significantly for those who have used polyhexamethylene guanidine phosphate/oligo(2-[2-ethoxy]-ethoxyethyl)guanidinium-containing HDs (model 3: 1.41, 95% confidence interval [CI]: 1.02–1.95). However, once duration of usage was additionally considered, ORs of doctor-diagnosed AR increased significantly only for those who have used chloromethylisothiazolinone/methylisothiazolinone-containing HDs for more than or equal to 3 months (model 3: 2.08, 95% CI: 1.17–3.69). Further, past use of HD was associated with significantly increased ORs of AR diagnosed before 2013 (model 3: 1.35, 95% CI: 1.02–1.79).
-
Conclusions
Results of our study suggest that past uses of HDs may be associated with an increased risk of AR.
-
Keywords: Humidifier disinfectant; Allergic rhinitis; Environmental chemicals; PSKC; Children
BACKGROUND
In the spring of 2011, atypical cases of severe lung injury among a group of young adults were reported in Korea [
1]. Epidemiological investigations that followed found that various humidifier disinfectants (HD) were the culprits; after the ban in 2011, no additional case of HD lung injury (HDLI) was detected [
2].
As more studies on HD victims were conducted, however, many cases where victims of HD uses suffered from and sought medical care for respiratory disorders other than HDLI were identified. These respiratory disorders included, but were not limited to, rhinitis, asthma, pneumonia; as such, studies to debunk the association between HD uses and aforementioned disorders were called for [
3]. Recently, using 2 independent general population-based birth cohort data, a group revealed the link between early-life HD exposure and asthma [
4].
It has been reported in a general population-based study that alarming percentages (31.1%) of young children in Korea were exposed to HD in the past [
5]. A recent report funded by National Institute of Environmental Research in Korea (NIER) revealed that, among the HD users who volunteered to take an online survey regarding exposure characteristics and health effect following HD exposures, 32.5% responded that they became diagnosed with and treated for rhinitis upon visits to hospital; in fact, rhinitis was the most frequently diagnosed disorder among the users [
3]. Further, according to another NIER-funded study, rhinitis accounted for 9.8% of diagnoses that were registered for compensation process by the victims of HD usage [
6]. However, no study has been published that investigated the association between early-life HD exposures and allergic rhinitis (AR). Therefore, we set out to investigate and delineate this very relationship based on our analysis of the data from Panel Study on Korean Children (PSKC).
METHODS
Study subjects
The eighth PSKC was conducted in 2015 by the Korea Institute of Child Care and Education. PSKC is a longitudinal survey conducted annually on a nationally representative sample of Korean children born between April and July of 2008 and their parents to understand factors that impact a child's development better [
7,
8]. A sample construction scheme for PSKC was as follow: the population consisted of households that gave birth in 2008; households that had children born between April and July of 2008 at medical centers across Korea were included in the study population; for the sampling method, the panel used stratified multi-stage sampling. 2,562 households were selected as the pilot sample, 2,078 for the original sample and 2,150 for the whole sample; further information on PSKC is available in the form of user's manual [
8].
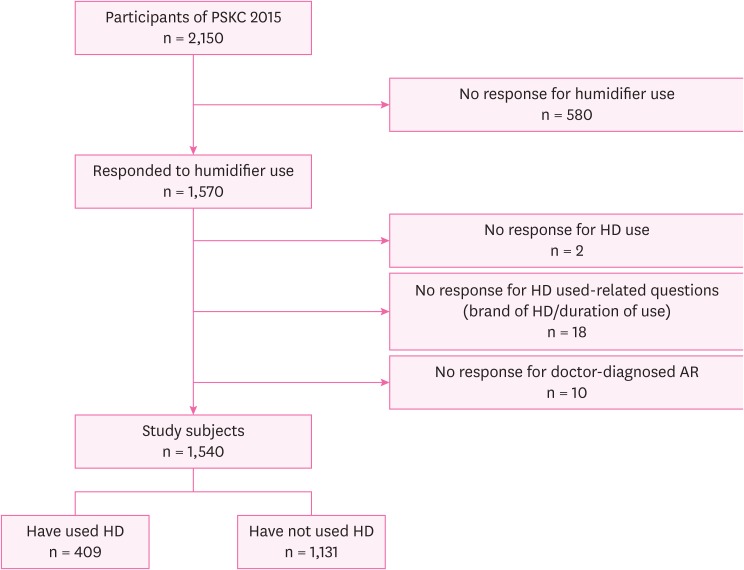
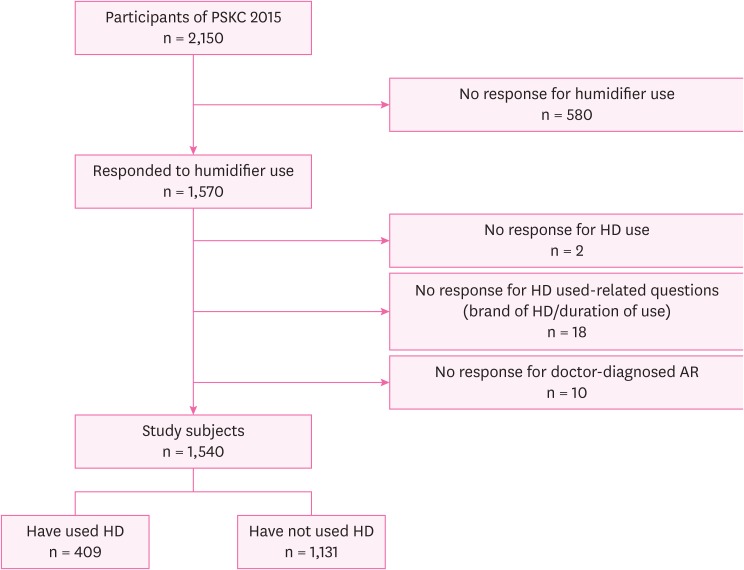
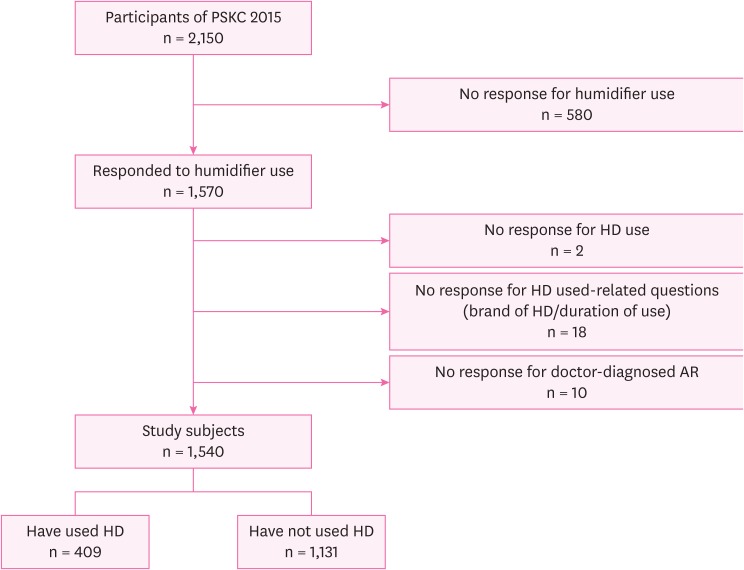
From 2,150 participants of the eighth PSKC, those who lacked responses for humidifier use, HD use, HD use-related questions (brand of HD/duration of use) and doctor-diagnosed AR were excluded. As a result, 1,540 participants became enrolled in our study; 409 participants who responded as having used HD and 1,131 participants who responded as never having used HD were included (
Fig. 1).
Fig. 1
Flow chart of the selection of study subjects.
PSKC: Panel Study on Korean Children; AR: allergic rhinitis; HD: humidifier disinfectant.
Questionnaires
We selected the eighth PSKC for our study as questions on not only the use of humidifier and HD but also the brands of HDs that were used were included that year. The eighth PSKC is composed of 6 surveys: a computer assisted personal interviewing (CAPI) questionnaire for caregiver, a questionnaire for mother, a questionnaire for father, a CAPI questionnaire for child, a questionnaire for health related survey and a computer assisted web interviewing questionnaire for school, each of which is coded as D, E, F, J, K, and L respectively. All questions and responses from aforementioned 6 surveys were examined to sort out variables that were deemed relevant for our study.
Variables of interest
As for socioeconomic variables, study subjects' sex, household incomes, maternal occupation/education and paternal occupation/education were included. Household incomes were allocated into quintiles based on the figures provided by Statistics Korea for the year of 2015. Maternal occupation was classified as 1 of 3 categories: white collar, blue collar or student/housewife. Paternal occupation too was classified as 1 of 3 categories: white collar, blue collar or student/unemployed. Maternal and paternal education were both classified as 1 of 3 levels: high school graduate or less, junior college graduate or bachelor's degree or more.
As for variables on relevant environmental exposures (excluding HD), exposures to passive smoking, presence of visible mold spots at the residence and presence of pet cats or dogs were included. For variables on HD exposures, whether study subjects were exposed to HD or not, brands of HD used and duration of HD use were included.
For variables regarding allergic disorders, whether study subjects were doctor-diagnosed with AR, asthma or atopic dermatitis (AD), whether study subjects have received treatment for AR during 12 months preceding the survey, whether diagnosis of AR was made prior to 2011 (the year at which HDs became banned), whether diagnosis of AR was made prior to 2013 (considering 2 years-long risk period following the exposure to HD) and whether parents have been diagnosed with AR were included for analysis.
Statistical analysis
Descriptive statistical analyses on socioeconomic characteristics and characteristics regarding relevant environmental exposures and allergic disorders of the study subjects were carried out. The χ2 tests were conducted to examine differences in distribution of above characteristics between the group that has used HD and the one that has never used HD.
To assess differences in distribution of doctor-diagnosed AR in respect to different types of HD used and duration of usage, Mantel-Haenszel χ
2 test was carried out. Brand names of HDs that participants responded to have used were utilized to group HDs based on their chemical makeup. For our study, HDs were grouped as either polyhexamethylene guanidine phosphate (PHMG)/oligo(2-[2-ethoxy]-ethoxyethyl)guanidinium (PGH)-containing or chloromethylisothiazolinone (CMIT)/methylisothiazolinone (MIT)-containing or other chemicals-containing HDs, in accordance with the most common chemical substances found in HDs [
9].
Multivariate analysis was implemented to describe the relationship between AR and select covariates. Whether study subjects have been doctor-diagnosed with AR and whether they have received treatment for AR during 12 months preceding the survey were selected as dependent variables. Three sets of covariates were used; each set included either past use of any HD, past use of PHMG/PGH-containing HD or past use of CMIT/MIT-containing HD in a mutually exclusive manner; the rest of covariates were selected by backward elimination method.
To assess for possibility of a dose-response relationship between doctor-diagnosed AR and HD uses, duration of usage was additionally considered in the multivariate analysis. Also, in order to delineate a temporal relationship between past use of HD and diagnosis of AR, we have analyzed whether past use of HDs were associated with significantly increased ORs for diagnosis of AR before 2011 and 2013 respectively. We selected those 2 years as 2011 was when HD sales became banned and as 2013 took into account of the risk period. Risk period refers to the time during which victims remain particularly susceptible to developing health effect due to exposures, and 2 years-long risk period is the standard often used in recognizing interstitial lung disease or asthma following HD exposures among victims [
6]. The odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to quantify the impact past use of any HDs, PHMG/PGH-containing HDs or CMIT/MIT-containing HDs have on diagnosis and treatment of AR.
As multicollinearity among covariates can be of concern while conducting multiple logistic regression, correlation coefficient rho and variance inflation factor (VIF) were calculated to test multicollinearity. We have set the criteria for collinearity at rho ≥ 0.7 and VIF ≥ 5. All statistical analyses were performed in SAS ver. 9.4 software (SAS Institute, Cary, NC, USA).
Ethics statement
This study was conducted after obtaining an approval from the Institutional Review Board (IRB) of Korea University Medical Center (IRB No. 2019AS0180).
RESULTS
Socioeconomic characteristics of subjects
Study subjects who have ever used HD and those who have never used HD did not differ significantly in respect to socioeconomic characters. There were approximately an even number of males and females in both groups. The most common maternal and paternal occupation was student/housewife and white-collar worker respectively, for both groups. High school graduate or less was the most common level of paternal and maternal education for both groups. Household incomes were distributed most dominantly in the mid 3 quintiles for both groups, with only about 10% belonging to the top and the bottom quintiles (
Table 1).
Table 1Socioeconomic characteristics of the subjects
|
Characteristics |
Category |
All subjects (n = 1,540) |
Have ever used HD (n = 409) |
Have never used HD (n = 1,131) |
p-value |
|
Sex |
Male |
791 (51.4) |
210 (51.3) |
581 (51.4) |
0.993 |
|
Female |
749 (48.6) |
199 (48.7) |
550 (48.6) |
|
Maternal occupation |
White-collar |
466 (31.0) |
130 (32.4) |
336 (30.5) |
0.484 |
|
Blue-collar |
190 (12.6) |
55 (13.7) |
135 (12.2) |
|
Student/housewife |
847 (56.4) |
216 (53.9) |
631 (57.3) |
|
Paternal occupation |
White-collar |
694 (49.3) |
197 (53.1) |
497 (47.9) |
0.216 |
|
Blue-collar |
626 (44.5) |
154 (41.5) |
472 (45.5) |
|
Student/unemployed |
88 (6.2) |
20 (5.4) |
68 (6.6) |
|
Maternal education |
Bachelor's degree or more |
444 (29.0) |
110 (26.9) |
334 (29.7) |
0.498 |
|
Junior college graduate |
421 (27.5) |
119 (29.1) |
302 (26.9) |
|
High school graduate or less |
667 (43.5) |
180 (44.0) |
487 (43.4) |
|
Paternal education |
Bachelor's degree or more |
399 (26.4) |
96 (23.8) |
303 (27.3) |
0.393 |
|
Junior college graduate |
304 (20.3) |
85 (21.1) |
222 (20.2) |
|
High school graduate or less |
806 (53.3) |
222 (55.1) |
584 (52.7) |
|
Household income distribution |
I (highest) |
121 (7.9) |
33 (8.2) |
88 (7.8) |
0.717 |
|
II |
531 (34.9) |
140 (34.8) |
391 (34.9) |
|
III |
513 (33.7) |
143 (35.6) |
370 (33.0) |
|
IV |
327 (21.5) |
77 (19.2) |
250 (22.3) |
|
V (lowest) |
31 (2.0) |
9 (2.2) |
22 (2.0) |
Characteristics regarding allergic disorders and relevant environmental exposures of the subjects
Study subjects who have ever used HD and those who have never used HD differed significantly in respect to the followings: exposures to passive smoking, whether their parents have been diagnosed with AR, whether study subjects were doctor-diagnosed with AR and whether they have received treatment for AR during 12 months prior to the survey. In other aspects, 2 groups were similar (
Table 2).
Table 2Characteristics regarding allergic disorders and relevant environmental exposures of the subjects
|
Characteristics |
Category |
All subjects (n = 1,540) |
Have ever used HD (n = 409) |
Have never used HD (n = 1,131) |
p-value |
|
Visible mold spots at the residence |
No |
1,019 (66.8) |
271 (66.9) |
748 (66.8) |
0.963 |
|
Yes |
506 (33.2) |
134 (33.1) |
372 (33.2) |
|
Passive smoking |
No |
942 (61.2) |
279 (68.2) |
663 (58.6) |
0.001 |
|
Yes |
598 (38.8) |
130 (31.8) |
468 (41.4) |
|
Parents' AR |
No |
749 (48.6) |
179 (43.8) |
570 (50.4) |
0.022 |
|
Yes |
791 (51.4) |
230 (56.2) |
561 (49.6) |
|
Presence of pet cats or dogs |
No |
1,401 (91.6) |
374 (91.7) |
1,027 (91.6) |
0.974 |
|
Yes |
128 (8.4) |
34 (8.3) |
94 (8.4) |
|
Doctor-diagnosed asthma |
No |
1,447 (94.1) |
378 (92.7) |
1,069 (94.7) |
0.133 |
|
Yes |
90 (5.9) |
30 (7.3) |
60 (5.3) |
|
Doctor-diagnosed AD |
No |
1227 (79.7) |
317 (77.5) |
910 (80.5) |
0.203 |
|
Yes |
313 (20.3) |
92 (22.5) |
221 (19.5) |
|
Doctor-diagnosed AR |
No |
816 (53.0) |
190 (46.5) |
626 (55.4) |
0.002 |
|
Yes |
724 (47.0) |
219 (53.6) |
505 (44.6) |
|
Diagnosed with AR before 2011 (the year when HDs were banned) |
No |
1,339 (88.6) |
347 (86.5) |
992 (89.3) |
0.137 |
|
Yes |
173 (11.4) |
54 (13.5) |
119 (10.7) |
|
Received treatment for AR during last 12 months |
No |
1,032 (67.1) |
251 (61.5) |
781 (69.2) |
0.005 |
|
Yes |
505 (32.9) |
157 (38.5) |
348 (30.8) |
Exposures to passive smoking were more common to the group that has never used HD (41.4%) than the one that has ever used any HD (31.8%). Parental AR was more common among subjects who have ever used HD (56.2%) than those who have never used HD before (49.6%). Doctor-diagnosed AR was more common among subjects who have used HD (53.6%) than those who have never used HD before (44.6%). Also, study subjects who have used HD before received treatment for AR (38.5%) more so than those who have never used HD before (30.8%) (
Table 2).
Approximately one third of both groups have reported to have visible mold spots at the residence. Less than one tenth of both groups have reported to have pet cats and dogs. The extent of doctor-diagnosed asthma and AD was similar between the 2 groups, which drew contrast with that of doctor-diagnosed AR. Those who were diagnosed with AR before 2011 accounted for 13.5% of participants who have ever used HD and 10.7% of those who have never used HD (
Table 2).
When study subjects were divided on the ground of PHMG/PGH-containing HD usage, significant differences existed in extent of doctor-diagnosed AR (
p-value for trend: < 0.001). Likewise, when study subjects were divided on the basis of CMIT/MIT-containing HD usage, significant differences existed in extent of doctor-diagnosed AR (
p-value for trend: 0.015). When study subjects were classified according to duration of HD usage, significant differences in extent of doctor-diagnosed AR existed as well (
p-value for trend: 0.003) (
Table 3).
Table 3Association between doctor-diagnosed AR and types and duration of HDs used
|
Characteristics |
Category |
Doctor-diagnosed AR |
|
Total |
No |
Yes |
p for trend |
|
Have used PGH/PHMG-containing HDs |
Have never used HD |
768 |
626 (55.4) |
505 (44.6) |
< 0.001 |
|
No, but have used other types |
154 |
81 (52.6) |
73 (47.4) |
|
Yes |
255 |
109 (42.7) |
146 (57.3) |
|
Have used CMIT/MIT-containing HDs |
Have never used HD |
768 |
626 (55.4) |
505 (44.6) |
0.015 |
|
No, but have used other types |
253 |
112 (44.3) |
141 (55.7) |
|
Yes |
156 |
78 (50.0) |
78 (50.0) |
|
Duration of HD use |
Have never used HD |
768 |
626 (55.4) |
505 (44.6) |
0.003 |
|
Less than 3 months |
239 |
115 (48.1) |
124 (51.9) |
|
3–6 months |
70 |
30 (42.9) |
40 (57.1) |
|
Greater than or equal to 6 months |
100 |
45 (45.0) |
55 (55.0) |
Multivariate analysis using multiple logistic regression models
ORs of doctor-diagnosed AR increased at a statistically significant level for those who have ever used HD when compared to those who have never used HD in our final model. When chemical makeup was additionally considered, results diverged a little. ORs of doctor-diagnosed AR increased significantly for those who have used PHMG/PGH-containing HDs (model 3: 1.41, 95% CI: 1.02–1.95). On the other hand, ORs of doctor-diagnosed AR were not increased significantly for those who have used CMIT/MIT-containing HD in comparison to those who have never used any HD (model 3: 1.43, 95% CI: 0.96–2.13) (
Table 4).
Table 4Crude and adjusted OR for doctor-diagnosed AR based on HD use in the past
|
Characteristics |
Category |
Model 1a
|
Model 2b
|
Model 3c
|
|
OR |
95% CI |
OR |
95% CI |
OR |
95% CI |
|
Have ever used HD |
No |
1.00 |
- |
1.00 |
- |
1.00 |
- |
|
Yes |
1.43 |
1.14–1.79 |
1.42 |
1.12–1.82 |
1.33 |
1.02–1.75 |
|
Have used PHMG/PGH-containing HD |
Have never used HD |
1.00 |
- |
1.00 |
- |
1.00 |
- |
|
No, but have used other types of HDs |
1.12 |
0.80–1.57 |
1.20 |
0.83–1.73 |
1.22 |
0.81–1.82 |
|
Yes |
1.66 |
1.26–2.19 |
1.57 |
1.17–2.11 |
1.41 |
1.02–1.95 |
|
Have used CMIT/MIT-containing HD |
Have never used HD |
1.00 |
- |
1.00 |
- |
1.00 |
- |
|
No, but have used other types of HDs |
1.56 |
1.18–2.05 |
1.47 |
1.09–1.97 |
1.28 |
0.93–1.77 |
|
Yes |
1.24 |
0.89–1.73 |
1.36 |
0.95–1.95 |
1.43 |
0.96–2.13 |
ORs of treatment for AR were not found significantly increased for those who have used HD. Even when chemical makeup was taken into consideration, consistently non-significant ORs resulted in our final model (
Supplementary Table 1).
The duration of usage was considered additionally to assess for possibility of a dose-response relationship; 3 months was used as a cut-off in the analysis. ORs of doctor-diagnosed AR were found to be increased at a statistically significant level for study subjects who have used CMIT/MIT-containing HD for more than or equal to 3 months (model 3: 2.08, 95% CI: 1.17–3.69). For those who have used CMIT/MIT-containing HD for less than 3 months, no significant ORs resulted. Further, while ORs of doctor-diagnosed AR showed a tendency to increase as duration of use got longer for those who have used PHMG/PGH-containing HDs, statistical significance was absent (
Table 5).
Table 5Crude and adjusted OR for doctor-diagnosed AR based on HD use in the past further stratified by duration
|
Characteristics |
Category |
Model 1a
|
Model 2b
|
Model 3c
|
|
OR |
95% CI |
OR |
95% CI |
OR |
95% CI |
|
Have ever used HD |
No |
1.00 |
- |
1.00 |
- |
1.00 |
- |
|
Yes (less than 3 months) |
1.34 |
1.01–1.77 |
1.34 |
1.00–1.81 |
1.26 |
0.91–1.75 |
|
Yes (greater than or equal to 3 months) |
1.57 |
1.14–2.17 |
1.55 |
1.09–2.21 |
1.46 |
0.99–2.16 |
|
Have used PHMG/PGH-containing HD |
Have never used HD |
1.00 |
- |
1.00 |
- |
1.00 |
- |
|
No, but have used other types |
1.12 |
0.80–1.57 |
1.20 |
0.83–1.73 |
1.22 |
0.81–1.82 |
|
Yes (less than 3 months) |
1.60 |
1.13–2.27 |
1.52 |
1.05–2.20 |
1.39 |
0.92–2.32 |
|
Yes (greater than or equal to 3 months) |
1.74 |
1.18–2.58 |
1.66 |
1.08–2.54 |
1.45 |
0.90–2.33 |
|
Have used CMIT/MIT-containing HD |
Have never used HD |
1.00 |
- |
1.00 |
- |
1.00 |
- |
|
No, but have used other types |
1.56 |
1.19–2.05 |
1.47 |
1.09–1.97 |
1.28 |
0.93–1.77 |
|
Yes (less than 3 months) |
1.00 |
0.64–1.56 |
1.04 |
0.64–1.69 |
1.04 |
0.61–1.76 |
|
Yes (greater than or equal to 3 months) |
1.59 |
0.99–2.56 |
1.83 |
1.09–3.06 |
2.08 |
1.17–3.69 |
When we analyzed whether HD usage was associated with diagnosis of AR prior to specific years, diverging results ensued. ORs of AR diagnosed prior to 2011, the year at which sales of HD became banned, did not increase significantly for study subjects who have used HD (model 3: 1.21, 95% CI: 0.83–1.76). On the other hand, ORs for AR diagnosed prior to 2013, the year that took into consideration of the risk period of 2 years, increased significantly for those who have used HD (model 3: 1.35, 95% CI: 1.02–1.79) (
Table 6).
Table 6Crude and adjusted OR for doctor-diagnosed AR before 2011 and 2013 based on HD use in the past
|
Characteristics |
Category |
Model 1a
|
Model 2b
|
Model 3c
|
|
OR |
95% CI |
OR |
95% CI |
OR |
95% CI |
|
Diagnosed with AR before 2011 (the year when HDs were banned) |
No |
1.00 |
- |
1.00 |
- |
1.00 |
- |
|
Yes |
1.27 |
0.92–1.83 |
1.36 |
0.94–1.95 |
1.21 |
0.83–1.76 |
|
Diagnosed with AR before 2013 (risk period) |
No |
1.00 |
- |
1.00 |
- |
1.00 |
- |
|
Yes |
1.48 |
1.15–1.89 |
1.46 |
1.12–1.91 |
1.35 |
1.02–1.79 |
Checking for multicollinearity
A correlation matrix among covariates in
Supplementary Table 2 showed that a correlation coefficient rho ranged from −0.1224 to 0.3038 and that VIF ranged from 1.01 to 1.18. Therefore, we assessed multicollinearity to be low.
DISCUSSION
Although AR was the most frequently diagnosed disorder among HD users, well-deserved attention has not been given, perhaps owing to its seemingly indolent clinical course [
3]. However, for pediatric population, AR is more than a seasonal nuisance [
10]. It has been reported that children with AR often presented with a decreased sleep quality, hyperactivity and poor school performance [
11]. Further, studies have revealed that AR was associated with mental complications such as fatigue, mood changes and impairment in psychological well-being [
12,
13]. Hence, we thought it would only be just to delve into the topic.
In our analysis, when simply whether any HDs were used in the past was considered with other covariates, ORs of doctor-diagnosed AR increased at a statistically significant level (model 3: 1.33, 95% CI: 1.02–1.75). When chemical make-up was taken into consideration, ORs of doctor-diagnosed AR increased significantly only for the group of study subjects who have used PHMG/PGH-containing HDs (model 3: 1.41, 95% CI: 1.02–1.95).
When we incorporated a cut-off of 3 months into our analysis to assess for the possibility of a dose response relationship between doctor-diagnosed AR and HD uses, ORs of doctor-diagnosed AR increased significantly only for those who have used CMIT/MIT-containing HDs for more than or equal to 3 months (model 3: 2.08, 95% CI: 1.17–3.69). For those who have used CMIT/MIT-containing HD for less than 3 months or used PHMG/PGH containing HDs regardless of duration, no significant ORs ensued. From our findings, a dose response relationship between doctor-diagnosed AR and CMIT/MIT-containing HD usage could be considered.
Studies that investigated on the association between HDs and AR have never been published; hence a direct comparison of our results with those of other studies that have focused on the identical association is infeasible. However, many studies that shed light on the association between chemical product uses and AR have been published. A study found that subjects with a high antimicrobial exposure score were more likely to have AR [
14]. Another study found that indoor exposures to propylene glycol ethers induced rhinitis [
15]. Exposures to pesticides such as diazinon and petroleum oil herbicide have been associated with an increased risk of rhinitis [
16]. Finally, exposures to a high level of triclosan, an antimicrobial agent found commonly in consumer products, have been found to be associated with rhinitis in Norwegian study [
17]. Thus, it should not come as a total surprise that HDs that were exposed to human via nasal and respiratory passages could be associated with increased ORs for AR.
The discrepancy between CMIT/MIT-containing HDs and PHMG/PGH-containing HDs in regards to statistical significance of ORs for doctor-diagnosed AR is quite interesting. Different extents of other disease outcomes based on HD chemical components have been documented. For HDLI, a nationwide study revealed that HDs containing PHMG and PGH were more frequently associated; a mixture of CMIT/MIT were found to be associated with only 2 cases of HDLI [
10]. In another study, it was found that a survival curve was least favorable for children exposed to PGH, followed by that of children exposed to PHMG and CMIT/MIT [
1].
Regarding pathophysiology of AR, many researches highlighted the roles of allergic axis composed of T-helper 2 cells, immunoglobulin E, mast cells and eosinophils [
18]. Recently, focus has been given to genetic basis of allergic diseases at each layer starting from the barrier of entry to effecter targets [
19]. Evidences for immunoglobulin E for many chemical compounds such as anhydrides and di-isocyanates have been documented [
20]. Various animal toxicity studies have investigated on post-inhalation effect of chemicals included in HDs. As for PHMG, a study using C57BL/7 mice has revealed that acute intra-tracheal exposures of PHMG led to increased pro-inflammatory cytokines and a decreased CD4+/CD8+ cell ratio in the thymus; these findings explained, though in part, the resulting fibrotic changes in the lung [
21]. A study using SD rats has shown that subacute nasal exposures to a high level of PGH led to degenerative changes in nasal epithelium [
22]. Lastly, another report on SD rats has shown that slight rhinitis in the lining of the anterior portion of nasal cavity occurred after the exposure to high dose of CMIT/MIT [
23]. At this point, molecular or cellular studies that could substantiate CMIT/MIT's relative potency over PHMG/PGH in increasing the risk of AR and delineate a clear pathophysiologic link between exposures of aforementioned chemicals and resulting hypersensitivity are needed.
The prohibition of HD sales was dictated in 2011; hence, public exposures to HD came to an end in 2011 as well. In compensating for diseases such as interstitial lung disease or asthma due to HD exposures, however, a risk period of 2 years, the time during which victims could develop diseases without active exposures, was recognized. So, we have adopted this risk period to investigate whether risk of diagnosis of AR before 2013 would increase significantly for those who have used HD, and they increased at a statistically significant level (model 3: 1.35, 95% CI: 1.02–1.79). Since use of HD that was continued until 2011 was associated with an increased risk of AR diagnosed before 2013, temporal precedence of exposures to HD to diagnosis of AR could be established.
On the other hand, ORs for AR diagnosed before 2011 were non-significant. This finding may owe to the small number of cases of AR diagnosed before 2011, which might have resulted in a reduced statistical power and a subsequent loss of statistical significance. Study subjects included in the panel were born in 2008, hence those diagnosed with AR prior to 2011 would have been before they were 3 years old, which is before the age when AR occurs dominantly in pediatric population. We also conjectured that contrasting results above were due to the latency period wedged between exposures to HD and development of nasal tract hypersensitivity and symptoms of AR. The presence of latency period has been documented in cases of work-related rhinitis induced by various chemicals at workplace [
24]. Although sales of HD were discontinued officially in 2011, it might have been that few years needed to have passed for AR to be induced among the users. Another plausible explanation is that, since sensitization to aeroallergen remits rarely, recurrent symptoms that worsened after the ban might have prompted parents to seek for medical diagnosis later [
25]. It is possible that post-2011 exposures to chemical allergens of structural similarities to substances constituting HDs have fueled recurrence of AR symptoms. Further, an alternative argument could be made that clinical progression of AR caused by HDs simply parallels that of AR caused by other allergens. A study has documented that the age-specific prevalence of AR in general peaks at age 3–4, which would explain how proportion of HD users who were diagnosed with AR before they turned 3 years old would constitute a minority regardless of HD use status [
26].
Limitation of our study is that due to its epidemiologic design as a cross-sectional study, causal inferences are limited. Uses of surveys subject our study to certain degrees of recall bias, especially since inquiries on sensitive topics such as past HD uses are involved. However, data that could prove HD uses in an objective manner did not exist for our use. Further, the possibility of selection bias regarding selection of study subjects exists. Our analysis has excluded 28% of the panel who lacked responses to either humidifier or HD usage. Further, the prevalence of AR and AD among study subjects were 47.0% and 20.3% in our analysis, which were different from those of existing literature. The prevalence of AR among Korean pre-school children was reported as 25.7% [
27], and that of AD in 6- to 7-year-old children was 35.6% [
28]. Exclusion of many potential study subjects due to missing values and the discrepancies in prevalence of allergic disease when compared with literature values point to the possibility of selection bias.
Despite these limitations, several strengths of our study also exist. To our knowledge, our study is the first one in literature to investigate on the relationship between AR and HD uses. And in the process, we considered for factors that go beyond the simple yes or no of past HD uses. Chemical makeup of HDs was taken into account to analyze whether uses of different brands of HDs would translate to different degrees of impact on AR. Duration of uses also considered to assess for presence of a dose-response relationship. We also assessed for temporal precedence of HD exposures to diagnosis of AR by conducting analyses that took into account of when the diagnosis of AR was made.
In the future, studies utilizing a larger sample size are called for. Lastly, biochemical and cellular studies that link CMIT/MIT exposures to pathogenesis of AR are also warranted.
CONCLUSIONS
In summary, past uses of any HD or PHMG/PGH-containing HD were associated with significantly increased ORs for doctor-diagnosed AR. When duration of usage was additionally considered, ORs for doctor-diagnosed AR increased significantly for only those who used CMIT/MIT-containing HD for more than or equal to 3 months. In addition, ORs of doctor-diagnosed AR made prior to 2013 increased significantly for those who have used HD before.
Results from our study may not provide a complete set of evidences in proving that a causal relationship exists between past uses of HDs and development of AR, which could be attributed to inherent shortcomings owing to our study's design as a cross-sectional study. However, our analysis does serve as a starting point in that it showed for the first time that past use of HDs was associated with increased ORs for doctor-diagnosed AR.
Abbreviations
computer assisted personal interviewing
chloromethylisothiazolinone
humidifier disinfectant lung injury
Institutional Review Board
National Institute of Environmental Research
oligo(2-[2-ethoxy]-ethoxyethyl)guanidinium
polyhexamethylene guanidine
Panel Study on Korean Children
Variance inflation factor
NOTES
-
Competing interests: The authors declare that they have no competing interests.
-
Availability of data and materials: The datasets analyzed in this study are available on request at the Korea Institute of Child Care and Education (http:// http://panel.kicce.re.kr/kor/index.jsp).
-
Authors contributions:
Conceptualization: Koh TH, Kwak K, Park JT.
Data curation: Koh TH, Kwon D.
Formal analysis: Koh TH, Kwak K.
Supervision: Kwak K.
Writing - original draft: Koh TH, Kwak K.
Writing - review & editing: Kwak K, Park JT, Kwon D.
SUPPLEMENTARY MATERIALS
Supplementary Table 1
Crude and adjusted OR for the treatment of AR based on HD use in the past
aoem-32-e9-s001.xls
Supplementary Table 2
Correlation matrix among covariates of demographic and environmental exposure characteristics
aoem-32-e9-s002.xls
REFERENCES
REFERENCES
- 1. Paek D, Koh Y, Park DU, Cheong HK, Do KH, Lim CM, et al. Nationwide study of humidifier disinfectant lung injury in South Korea, 1994–2011. Incidence and dose-response relationships. Ann Am Thorac Soc 2015;12(12):1813–1821. 26653190.ArticlePubMed
- 2. Kim HJ, Lee MS, Hong SB, Huh JW, Do KH, Jang SJ, et al. A cluster of lung injury cases associated with home humidifier use: an epidemiological investigation. Thorax 2014;69(8):703–708. 24488371.PubMed
- 3. National Institute of Environmental Research. Establishing disease identification and standards criteria to expand the range of health hazards caused by the humidifier sterilizer. Incheon: National Institute of Environmental Research; 2017.
- 4. Yoon J, Lee SY, Lee SH, Kim EM, Jung S, Cho HJ, et al. Exposure to humidifier disinfectants increases the risk of asthma in children. Am J Respir Crit Care Med 2018;198(12):1583–1586.ArticlePubMedPMC
- 5. Yoon J, Cho HJ, Lee E, Choi YJ, Kim YH, Lee JL, et al. Rate of humidifier and humidifier disinfectant usage in Korean children: a nationwide epidemiologic study. Environ Res 2017;155:60–63. 28189074.ArticlePubMed
- 6. National Institute of Environmental Research. Study for improving recognition and judgment standard of health damage of humidifier disinfectant(I). Incheon: National Institute of Environmental Research; 2018.
- 7. Bahk J, Yun SC, Kim YM, Khang YH. Impact of unintended pregnancy on maternal mental health: a causal analysis using follow up data of the Panel Study on Korean Children (PSKC). BMC Pregnancy Childbirth 2015;15(1):85. 25881099.ArticlePubMedPMCPDF
- 8. Korea Institute of Child Care and Education. Panel Study on Korean Children (PSKC) data use manual for 1st–7th study. 2016;Accessed 23 May 2019]. http://www.kicce.re.kr/eng/index.do.
- 9. Lee JH, Kim YH, Kwon JH. Fatal misuse of humidifier disinfectants in Korea: importance of screening risk assessment and implications for management of chemicals in consumer products. Environ Sci Technol 2012;46(5):2498–2500. 22369507.ArticlePubMed
- 10. Greiner AN, Hellings PW, Rotiroti G, Scadding GK. Allergic rhinitis. Lancet 2011;378(9809):2112–2122. 21783242.ArticlePubMed
- 11. Blaiss MS. Pediatric allergic rhinitis: physical and mental complications. Allergy Asthma Proc 2008;29(1):1–6. 18302831.ArticlePubMed
- 12. Marshall PS, O'Hara C, Steinberg P. Effects of seasonal allergic rhinitis on fatigue levels and mood. Psychosom Med 2002;64(4):684–691. 12140359.ArticlePubMed
- 13. Kremer B, den Hartog HM, Jolles J. Relationship between allergic rhinitis, disturbed cognitive functions and psychological well-being. Clin Exp Allergy 2002;32(9):1310–1315. 12220469.ArticlePubMedPDF
- 14. Hong S, Kwon HJ, Choi WJ, Lim WR, Kim J, Kim K. Association between exposure to antimicrobial household products and allergic symptoms. Environ Health Toxicol 2014;29:e2014017. 25420879.ArticlePubMedPMCPDF
- 15. Choi H, Schmidbauer N, Sundell J, Hasselgren M, Spengler J, Bornehag CG. Common household chemicals and the allergy risks in pre-school age children. PLoS One 2010;5(10):e13423. 20976153.ArticlePubMedPMC
- 16. Slager RE, Poole JA, LeVan TD, Sandler DP, Alavanja MC, Hoppin JA. Rhinitis associated with pesticide exposure among commercial pesticide applicators in the Agricultural Health Study. Occup Environ Med 2009;66(11):718–724. 19289390.ArticlePubMedPMC
- 17. Bertelsen RJ, Longnecker MP, Løvik M, Calafat AM, Carlsen KH, London SJ, et al. Triclosan exposure and allergic sensitization in Norwegian children. Allergy 2013;68(1):84–91. 23146048.ArticlePubMedPMC
- 18. Baraniuk JN. Pathogenesis of allergic rhinitis. J Allergy Clin Immunol 1997;99(2):S763–72. 9042069.ArticlePubMed
- 19. Meng JF, Rosenwasser LJ. Unraveling the genetic basis of asthma and allergic diseases. Allergy Asthma Immunol Res 2010;2(4):215–227. 20885906.ArticlePubMedPMC
- 20. Von Mutius E, Martinez FD. Natural history, development, and prevention of allergic disease in childhood. In: Adkinson NF Jr, Yunginger JW, Busse WW, Bochner B, Holgate ST, Simons FER, editors. Middleton's Allergy: Principles and Practice. 4th ed. St. Louis, MO: Mosby; 2003, 1169–1174.
- 21. Song JA, Park HJ, Yang MJ, Jung KJ, Yang HS, Song CW, et al. Polyhexamethyleneguanidine phosphate induces severe lung inflammation, fibrosis, and thymic atrophy. Food Chem Toxicol 2014;69:267–275. 24769016.ArticlePubMed
- 22. National Institute of Environmental Research. Study on hazardous chemical substances in household chemical products and their health impact. 2014;Accessed 10 Jan 2020]. http://webbook.me.go.kr/DLi-File/NIER/06/021/5591231.pdf.
- 23. Scientific Committee on Consumer Safety. Opinion on: the mixture of 5-chloro-2-methylisothiazolin-3(2h)-one and 2-methylisothiazolin-3(2h)-one. 2009;Accessed 10 Jan 2020]. http://ec.europa.eu/health//sites/health/files/scientific_committees/consumer_safety/docs/sccs_o_009.pdf.
- 24. EAACI Task Force on Occupational Rhinitis. Moscato G, Vandenplas O, Gerth Van Wijk R, Malo JL, Quirce S, et al. Occupational rhinitis. Allergy 2008;63(8):969–980. 18691299.ArticlePubMed
- 25. Jacobs KD, Brand PL. Can sensitization to aeroallergens disappear over time in children with allergic disease? Acta Paediatr 2010;99(9):1361–1364. 20222877.ArticlePubMed
- 26. Lim DH. Epidemiology of allergic rhinitis in Korean children. World Allergy Organ J 2015;8(Suppl 1):A41.ArticlePMCPDF
- 27. Kim DH, Park YS, Jang HJ, Kim JH, Lim DH. Prevalence and allergen of allergic rhinitis in Korean children. Am J Rhinol Allergy 2016;30(3):72–78. 27216339.ArticlePubMedPDF
- 28. Pyun BY. Natural history and risk factors of atopic dermatitis in children. Allergy Asthma Immunol Res 2015;7(2):101–105. 25729616.ArticlePubMedPDF
 , Jong-Tae Park1
, Jong-Tae Park1 , Daeil Kwon1
, Daeil Kwon1 , Kyeongmin Kwak1,3
, Kyeongmin Kwak1,3

 KSOEM
KSOEM

 Cite
Cite

