Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 31; 2019 > Article
- Research Article The effect of diabetes on 4-year changes of hearing thresholds in male workers exposed to noise in a single company: a longitudinal study
-
Dae Yun Kim1
 , A Ram Kim1
, A Ram Kim1 , Joo Hyun Sung2
, Joo Hyun Sung2 , Choong Ryeol Lee1
, Choong Ryeol Lee1 , Jiho Lee1
, Jiho Lee1
-
Annals of Occupational and Environmental Medicine 2019;31:e11.
DOI: https://doi.org/10.35371/aoem.2019.31.e11
Published online: June 28, 2019
1Department of Occupational and Environmental Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
2Department of Occupational and Environmental Medicine, Institute of Health Sciences, Gyeongsang National University Changwon Hospital, Gyeongsang National University College of Medicine, Jinju, Korea.
- Correspondence: Jiho Lee. Department of Occupational and Environmental Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, 877 Bangeojinsunhwando-ro, Dong-gu, Ulsan 44033, Korea. oemdoc@naver.com
Copyright © 2019 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background Recently, several studies have assessed the association between diabetes and hearing impairment. However, the effect of diabetes on hearing impairment is not well known in diabetic patients exposed to noise, a typical cause of hearing impairment. The aim of this study is to longitudinally analyze the effect of diabetes on hearing impairment in workers exposed to similar noise levels from 2013 to 2017 who had experienced little change in their working conditions.
-
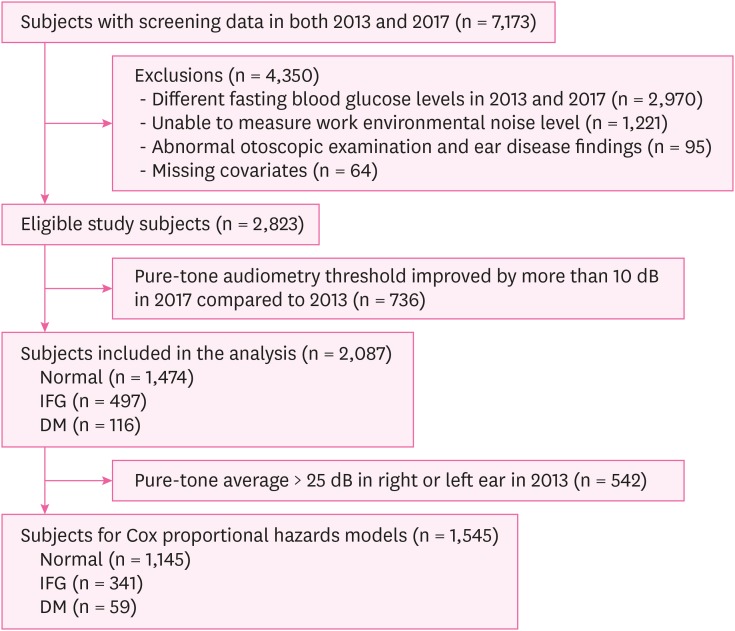
Methods The study subjects included 2,087 male workers exposed to noise in a single company and who underwent health examinations at the same hospital in Ulsan city in 2013 and 2017. Hearing impairment was defined that a pure-tone average of pure-tone audiometry (PTA) thresholds at 1,000, 2,000, 3,000, and 4,000 Hz was 25 dB and over in both ears. Statistical analyses were conducted using χ2 tests, ANOVA, and Cox proportional hazard models. We analyzed covariates that might affect hearing impairment, including age; working period; levels of total cholesterol, triglyceride, and serum creatinine; smoking and alcohol history; and noise level.
-
Results The average PTA thresholds and their average changes between 2013 and 2017 were significant in the diabetes mellitus (DM) group than those in the normal and impaired fasting glucose group. Among the subjects with the same status of fasting glucose group in 2013 and 2017, the adjusted hazard ratios for incident hearing impairment among those in the DM group compared to normal group were 3.35 (95% confidence interval [CI], 1.54–7.29) in the left ear and 5.66 (95% CI, 2.01–15.98) in the right ear.
-
Conclusions This study suggested that the risk of hearing impairment in the DM group was significantly higher than that in the normal group in both ears, even when exposed to similar noise levels.
BACKGROUND
METHODS
 ) and defined pure-tone average > 25 dB as hearing impairment and ≤ 25 dB as normal hearing [21]. Fasting blood samples were collected after at least 8 hours of fasting. Subjects with fasting blood glucose below 100 mg/dL were defined as the normal group, while subjects with fasting blood glucose between 100 and 125 mg/dL were defined as the IFG group. Subjects with fasting blood glucose over 125 mg/dL and those taking anti-diabetic medications and with a self-reported history of diabetes were defined as the DM group [15,18]. Blood pressure was analyzed as a continuous variable by calculating the mean arterial pressure (
) and defined pure-tone average > 25 dB as hearing impairment and ≤ 25 dB as normal hearing [21]. Fasting blood samples were collected after at least 8 hours of fasting. Subjects with fasting blood glucose below 100 mg/dL were defined as the normal group, while subjects with fasting blood glucose between 100 and 125 mg/dL were defined as the IFG group. Subjects with fasting blood glucose over 125 mg/dL and those taking anti-diabetic medications and with a self-reported history of diabetes were defined as the DM group [15,18]. Blood pressure was analyzed as a continuous variable by calculating the mean arterial pressure ( ) which reflects the average effective pressure [22]. Smoking history was classified as smokers or non-smokers, in which smokers were defined as those participants who had smoked more than 100 cigarettes and those who currently smoked cigarettes [23]. Drinking history was classified as high-risk alcohol intake or non-alcohol intake, in which high-risk alcohol intake was defined as a minimum of 7 shots on average in 1 seating with a minimum of 2 drinking sessions per week for men [23].
) which reflects the average effective pressure [22]. Smoking history was classified as smokers or non-smokers, in which smokers were defined as those participants who had smoked more than 100 cigarettes and those who currently smoked cigarettes [23]. Drinking history was classified as high-risk alcohol intake or non-alcohol intake, in which high-risk alcohol intake was defined as a minimum of 7 shots on average in 1 seating with a minimum of 2 drinking sessions per week for men [23].RESULTS
General characteristics of study subjects according to fasting blood glucose groups in 2013
Pure-tone audiometry thresholds changes on individual subjects according to the same fasting glucose groups in 2013 and 2017
Adjusted HRs of hearing impairment by pure-tone average compared to normal fasting glucose group
DISCUSSION
CONCLUSIONS
Acknowledgements
Abbreviations
PTA
DM
CI
IFG
MAP
HR
4FA
OR
-
Competing interests: The authors declare that they have no competing interests.
-
Availability of data and materials: Please contact author for data request.
-
Author Contributions:
Conceptualization: Lee JH, Lee CR, Kim DY.
Data curation: Kim DY.
Formal analysis: Kim DY.
Investigation: Kim DY, Kim AR.
Methodology: Lee JH, Lee CR, Sung JH, Kim DY.
Project administration: Lee JH, Lee CR.
Resources: Sung JH, Kim DY, Kim AR.
Software: Kim DY, Kim AR.
Supervision: Lee JH, Lee CR.
Validation: Lee JH, Lee CR, Kim DY.
Visualization: Kim DY.
Writing - original draft: Kim DY.
Writing - review & editing: Lee JH, Lee CR, Sung JH.
NOTES
- 1. Verhoeff M, van der Veen EL, Rovers MM, Sanders EA, Schilder AG. Chronic suppurative otitis media: a review. Int J Pediatr Otorhinolaryngol 2006;70(1):1–12. 16198004.ArticlePubMed
- 2. Palomar García V, Abdulghani Martínez F, Bodet Agustí E, Andreu Mencía L, Palomar Asenjo V. Drug-induced otoxicity: current status. Acta Otolaryngol 2001;121(5):569–572. 11583387.ArticlePubMed
- 3. Konigsmark BW. Genetic hearing loss with no associated abnormalities: a review. J Speech Hear Disord 1972;37(1):89–99. 4559857.ArticlePubMed
- 4. Sliwinska-Kowalska M, Davis A. Noise-induced hearing loss. Noise Health 2012;14(61):274–280. 23257577.ArticlePubMed
- 5. Kidd Iii AR, Bao J. Recent advances in the study of age-related hearing loss: a mini-review. Gerontology 2012;58(6):490–496. 22710288.ArticlePubMedPMCPDF
- 6. National Law Information Center. Occupational safety and health act enforcement rule (attached Table 11-5). Sejong: National Law Information Center; 2017, Accessed 14 May 2019]. http://www.law.go.kr/법령/산업안전보건법시행규칙.
- 7. Ministry of Employment and Labor. Ministry of Labor and Employment amended by notice No. 2018-62. Sejong: Ministry of Employment and Labor; 2018.
- 8. Guski R, Schreckenberg D, Schuemer R. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and annoyance. Int J Environ Res Public Health 2017;14(12):E1539. 29292769.ArticlePubMedPMC
- 9. World Health Organization. Diabetes. Geneva: World Health Organization; 2018, Accessed 21 Dec 2018]. http://www.who.int/mediacentre/factsheets/fs312/en/.
- 10. Vijan S. In the clinic. Type 2 diabetes. Ann Intern Med 2010;152(5):ITC31–ITC15. 20194231.PubMed
- 11. Kaźmierczak H, Doroszewska G. Metabolic disorders in vertigo, tinnitus, and hearing loss. Int Tinnitus J 2001;7(1):54–58. 14964957.PubMed
- 12. Samelli AG, Santos IS, Moreira RR, Rabelo CM, Rolim LP, Bensenõr IJ, et al. Diabetes mellitus and sensorineural hearing loss: is there an association? Baseline of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Clinics (Sao Paulo) 2017;72(1):5–10. 28226026.ArticlePubMedPMC
- 13. Engdahl B, Aarhus L, Lie A, Tambs K. Cardiovascular risk factors and hearing loss: the HUNT study. Int J Audiol 2015;54(12):958–966. 26642893.ArticlePubMed
- 14. Hodgson MJ, Talbott E, Helmkamp JC, Kuller LH. Diabetes, noise exposure, and hearing loss. J Occup Med 1987;29(7):576–579. 3612333.PubMed
- 15. Kim MB, Zhang Y, Chang Y, Ryu S, Choi Y, Kwon MJ, et al. Diabetes mellitus and the incidence of hearing loss: a cohort study. Int J Epidemiol 2017;46(2):717–726. 27818377.ArticlePubMedPMCPDF
- 16. Akinpelu OV, Mujica-Mota M, Daniel SJ. Is type 2 diabetes mellitus associated with alterations in hearing? A systematic review and meta-analysis. Laryngoscope 2014;124(3):767–776. 23945844.ArticlePubMedPDF
- 17. Horikawa C, Kodama S, Tanaka S, Fujihara K, Hirasawa R, Yachi Y, et al. Diabetes and risk of hearing impairment in adults: a meta-analysis. J Clin Endocrinol Metab 2013;98(1):51–58. 23150692.ArticlePubMed
- 18. Jang TW, Kim BG, Kwon YJ, Im HJ. The association between impaired fasting glucose and noise-induced hearing loss. J Occup Health 2011;53(4):274–279. 21670562.ArticlePubMedPDF
- 19. Mitchell P, Gopinath B, McMahon CM, Rochtchina E, Wang JJ, Boyages SC, et al. Relationship of type 2 diabetes to the prevalence, incidence and progression of age-related hearing loss. Diabet Med 2009;26(5):483–488. 19646187.ArticlePubMed
- 20. Botelho CT, Carvalho SA, Silva IN. Increased prevalence of early cochlear damage in young patients with type 1 diabetes detected by distortion product otoacoustic emissions. Int J Audiol 2014;53(6):402–408. 24564623.ArticlePubMed
- 21. Cheng YJ, Gregg EW, Saaddine JB, Imperatore G, Zhang X, Albright AL. Three decade change in the prevalence of hearing impairment and its association with diabetes in the United States. Prev Med 2009;49(5):360–364. 19664652.ArticlePubMed
- 22. Jung SJ, Woo KH, Park WD, Yu JY, Choi TS, Kim SW, et al. Related factors of high frequency hearing loss in the noise-exposed male workers. Korean J Occup Environ Med 2000;12(2):187–197.ArticlePDF
- 23. Korea Centers for Disease Control and Prevention. The Sixth Korea National Health and Nutrition Examination Survey (KNHANES VI-2). Cheongju: Korea Centers for Disease Control and Prevention; 2015.
- 24. Sommer J, Brennan-Jones CG, Eikelboom RH, Hunter M, Davis WA, Atlas MD, et al. A population-based study of the association between dysglycaemia and hearing loss in middle age. Diabet Med 2017;34(5):683–690. 28135010.ArticlePubMedPDF
- 25. Doosti A, Lotfi Y, Bakhshi E. Effects of hyperlipidemia on noise induced hearing loss (NIHL). Indian J Otolaryngol Head Neck Surg 2016;68(2):211–213. 27340639.ArticlePubMedPMCPDF
- 26. Chang NC, Yu ML, Ho KY, Ho CK. Hyperlipidemia in noise-induced hearing loss. Otolaryngol Head Neck Surg 2007;137(4):603–606. 17903577.ArticlePubMedPDF
- 27. Bener A, Al-Hamaq AO, Abdulhadi K, Salahaldin AH, Gansan L. Interaction between diabetes mellitus and hypertension on risk of hearing loss in highly endogamous population. Diabetes Metab Syndr 2017;11(Suppl 1):S45–S51. 27614865.ArticlePubMed
- 28. Lin BM, Curhan SG, Wang M, Eavey R, Stankovic KM, Curhan GC. Hypertension, diuretic use, and risk of hearing loss. Am J Med 2016;129(4):416–422. 26656761.ArticlePubMedPMC
- 29. Kakarlapudi V, Sawyer R, Staecker H. The effect of diabetes on sensorineural hearing loss. Otol Neurotol 2003;24(3):382–386. 12806288.ArticlePubMed
- 30. Fukushima H, Cureoglu S, Schachern PA, Paparella MM, Harada T, Oktay MF. Effects of type 2 diabetes mellitus on cochlear structure in humans. Arch Otolaryngol Head Neck Surg 2006;132(9):934–938. 16982969.ArticlePubMed
- 31. Guerci B, Kearney-Schwartz A, Böhme P, Zannad F, Drouin P. Endothelial dysfunction and type 2 diabetes. Part 1: physiology and methods for exploring the endothelial function. Diabetes Metab 2001;27(4 Pt 1):425–434. 11547216.PubMed
- 32. Taslipinar A, Yaman H, Yilmaz MI, Demirbas S, Saglam M, Taslipinar MY, et al. The relationship between inflammation, endothelial dysfunction and proteinuria in patients with diabetic nephropathy. Scand J Clin Lab Invest 2011;71(7):606–612. 21864054.ArticlePubMed
- 33. Sonneville R, den Hertog HM, Güiza F, Gunst J, Derese I, Wouters PJ, et al. Impact of hyperglycemia on neuropathological alterations during critical illness. J Clin Endocrinol Metab 2012;97(6):2113–2123. 22442271.ArticlePubMed
- 34. Vaughan N, James K, McDermott D, Griest S, Fausti S. Auditory brainstem response differences in diabetic and non-diabetic veterans. J Am Acad Audiol 2007;18(10):863–871. 18496995.ArticlePubMed
- 35. Yamasoba T, Oka Y, Tsukuda K, Nakamura M, Kaga K. Auditory findings in patients with maternally inherited diabetes and deafness harboring a point mutation in the mitochondrial transfer RNA(Leu) (UUR) gene. Laryngoscope 1996;106(1 Pt 1):49–53. 8544627.ArticlePubMed
- 36. Newkirk JE, Taylor RW, Howell N, Bindoff LA, Chinnery PF, Alberti KG, et al. Maternally inherited diabetes and deafness: prevalence in a hospital diabetic population. Diabet Med 1997;14(6):457–460. 9212310.ArticlePubMed
- 37. Khardori R, Stephens JW, Page OC, Dow RS. Diabetes mellitus and optic atrophy in two siblings: a report on a new association and a review of the literature. Diabetes Care 1983;6(1):67–70. 6839924.ArticlePubMedPDF
- 38. Shim HJ. Noise-induced hearing loss. Hanyang Med Rev 2015;35(2):84–91.Article
- 39. McBride DI, Williams S. Audiometric notch as a sign of noise induced hearing loss. Occup Environ Med 2001;58(1):46–51. 11119634.ArticlePubMedPMC
- 40. Sellick PM, Patuzzi R, Johnstone BM. Measurement of basilar membrane motion in the guinea pig using the Mössbauer technique. J Acoust Soc Am 1982;72(1):131–141. 7108035.ArticlePubMedPDF
- 41. Yamasoba T, Lin FR, Someya S, Kashio A, Sakamoto T, Kondo K. Current concepts in age-related hearing loss: epidemiology and mechanistic pathways. Hear Res 2013;303:30–38. 23422312.ArticlePubMedPMC
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Individual and combined effects of noise exposure and diabetes mellitus on hearing
Lan Zhang, Hui Liao, Zongnan Li, Jianhui Yuan
Noise and Health.2024; 26(123): 449. CrossRef - Noise-induced Hearing Loss among Non-Medical Workers in a Healthcare Institution
Manju Deena Mammen, Ann Mary Augustine, Anjali Lepcha, Jessie Sophia Sharma, Arockiaraj Arul Prakash, Ajay Philip
The Indonesian Journal of Occupational Safety and Health.2023; 13(1): 13. CrossRef
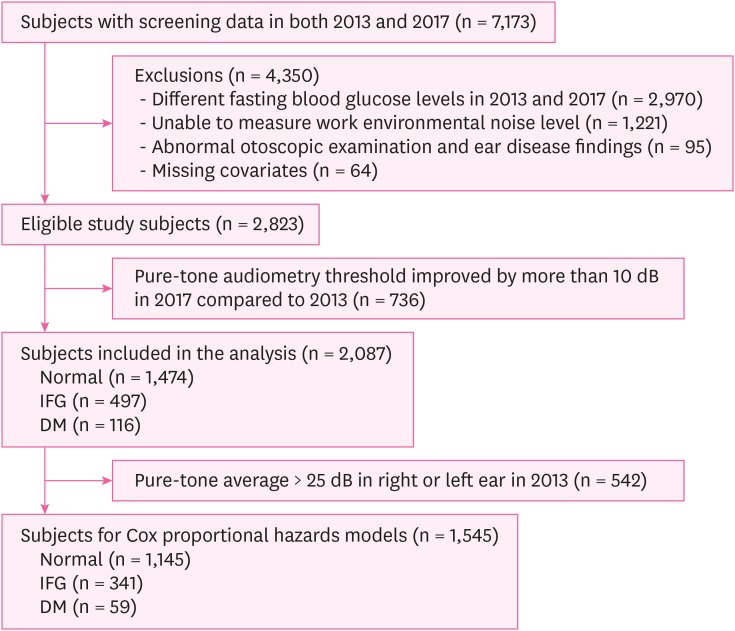
Fig. 1
| Classification variables | Normala (n=1,474) | IFGb (n=497) | DMc (n=116) | Total (n=2,087) | p-value* | Post-hoc comparison | |
|---|---|---|---|---|---|---|---|
| Age (years) | 41.5 ± 9.5 | 44.5 ± 9.9 | 49.3 ± 7.9 | 42.6 ± 9.7 | < 0.001 | a < b < c | |
| Working period (years) | 15.9 ± 11.3 | 19.2 ± 11.4 | 24.4 ± 8.6 | 17.2 ± 11.4 | < 0.001 | a < b < c | |
| Noise level (decibel) | 83.1 ± 5.5 | 82.8 ± 5.3 | 81.8 ± 5.3 | 83.0 ± 5.4 | 0.036 | c < a | |
| Mean arterial pressure (mmHg) | 91.8 ± 8.6 | 93.9 ± 8.1 | 95.5 ± 8.2 | 92.5 ± 8.5 | < 0.001 | a < b, c | |
| Fasting blood glucose (mg/dL) | 92.1 ± 5.7 | 109.7 ± 6.6 | 132.2 ± 28.8 | 98.5 ± 14.2 | < 0.001 | a < b < c | |
| Total cholesterol (mg/dL) | 200.6 ± 32.0 | 204.3 ± 31.5 | 183.0 ± 39.2 | 200.5 ± 32.6 | < 0.001 | c < a, b | |
| Triglyceride (mg/dL) | 120.0 ± 76.9 | 140.5 ± 109.7 | 134.5 ± 91.4 | 125.7 ± 87.0 | < 0.001 | a < b | |
| Serum creatinine (mg/dL) | 1.0 ± 0.1 | 1.0 ± 0.1 | 1.0 ± 0.3 | 1.0 ± 0.1 | 0.035 | a, b < c | |
| Noise level (dB) | 0.103 | ||||||
| ≤ 79.9 | 384 (26.1) | 139 (28.0) | 43 (37.1) | 566 (27.1) | |||
| 80.0–84.9 | 563 (38.2) | 188 (37.8) | 42 (36.2) | 793 (38.0) | |||
| ≥ 85.0 | 527 (35.8) | 170 (34.2) | 31 (26.7) | 728 (34.9) | |||
| Working period (years) | < 0.001 | ||||||
| ≤ 14.9 | 738 (50.1) | 193 (38.8) | 23 (19.8) | 954 (45.7) | |||
| 15.0–29.9 | 528 (35.8) | 197 (39.6) | 66 (56.9) | 791 (37.9) | |||
| ≥ 30.0 | 208 (14.1) | 107 (21.5) | 27 (23.3) | 342 (16.4) | |||
| Smoking | 0.006 | ||||||
| No | 736 (49.9) | 274 (55.1) | 70 (60.3) | 1,080 (51.7) | |||
| Yes | 738 (50.1) | 223 (44.9) | 46 (39.7) | 1,007 (48.3) | |||
| High-risk alcohol intake | 0.954 | ||||||
| No | 1,104 (74.9) | 343 (69.0) | 98 (84.5) | 1,545 (74.0) | |||
| Yes | 370 (25.1) | 154 (31.0) | 18 (15.5) | 542 (26.0) | |||
| Frequencies | Normala (n=1,474) | IFGb (n=497) | DMc (n=116) | Total (n=2,087) | p-value* | Post-hoc comparison | ||
|---|---|---|---|---|---|---|---|---|
| Left ear (dB) | ||||||||
| 1,000 Hz | ||||||||
| 2013 | 13.2 ± 9.5 | 14.0 ± 8.9 | 17.0 ± 13.9 | 13.6 ± 9.7 | < 0.001 | a, b < c | ||
| 2017 | 13.9 ± 11.4 | 15.3 ± 11.3 | 19.3 ± 15.4 | 14.5 ± 11.7 | < 0.001 | a, b < c | ||
| Changes | 0.7 ± 4.8 | 1.3 ± 4.6 | 2.2 ± 6.0 | 0.9 ± 4.8 | < 0.001 | a, b < c | ||
| 2,000 Hz | ||||||||
| 2013 | 15.0 ± 12.1 | 16.1 ± 11.9 | 20.6 ± 16.3 | 15.6 ± 12.4 | < 0.001 | a, b < c | ||
| 2017 | 16.2 ± 14.3 | 18.2 ± 14.2 | 24.2 ± 17.9 | 17.1 ± 14.6 | < 0.001 | a, b < c | ||
| Changes | 1.2 ± 5.1 | 2.1 ± 5.5 | 3.6 ± 5.7 | 1.5 ± 5.2 | < 0.001 | a, b < c | ||
| 3,000 Hz | ||||||||
| 2013 | 19.6 ± 16.6 | 22.8 ± 18.0 | 30.0 ± 20.2 | 21.0 ± 17.3 | < 0.001 | a, b < c | ||
| 2017 | 20.8 ± 18.4 | 24.2 ± 19.0 | 32.3 ± 21.0 | 22.2 ± 18.9 | < 0.001 | a, b < c | ||
| Changes | 1.1 ± 5.2 | 1.4 ± 4.7 | 2.2 ± 4.9 | 1.3 ± 5.0 | 0.059 | a, b < c | ||
| 4,000 Hz | ||||||||
| 2013 | 24.9 ± 19.7 | 28.6 ± 20.4 | 37.1 ± 21.3 | 26.5 ± 20.2 | < 0.001 | a, b < c | ||
| 2017 | 27.1 ± 21.1 | 30.7 ± 21.4 | 40.4 ± 22.2 | 28.7 ± 21.5 | < 0.001 | a, b < c | ||
| Changes | 2.2 ± 5.6 | 2.2 ± 5.3 | 3.3 ± 5.8 | 2.2 ± 5.5 | 0.091 | a, b < c | ||
| Right ear (dB) | ||||||||
| 1,000 Hz | ||||||||
| 2013 | 13.1 ± 8.5 | 14.5 ± 12.1 | 16.7 ± 14.6 | 13.7 ± 9.9 | < 0.001 | a, b < c | ||
| 2017 | 13.7 ± 10.6 | 16.2 ± 13.9 | 19.0 ± 16.3 | 14.6 ± 11.9 | < 0.001 | a < b < c | ||
| Changes | 0.6 ± 4.6 | 1.7 ± 5.2 | 2.2 ± 5.2 | 0.9 ± 4.9 | 0.004 | a < b, c | ||
| 2,000 Hz | ||||||||
| 2013 | 14.5 ± 11.4 | 16.2 ± 14.3 | 19.8 ± 16.6 | 15.2 ± 12.5 | < 0.001 | a, b < c | ||
| 2017 | 15.4 ± 13.5 | 18.3 ± 16.3 | 22.6 ± 17.8 | 16.5 ± 14.6 | < 0.001 | a, b < c | ||
| Changes | 0.9 ± 4.7 | 2.1 ± 5.3 | 2.8 ± 5.3 | 1.3 ± 5.0 | 0.002 | a < b, c | ||
| 3,000 Hz | ||||||||
| 2013 | 18.6 ± 16.1 | 22.5 ± 19.4 | 28.0 ± 19.3 | 20.1 ± 17.3 | < 0.001 | a < b < c | ||
| 2017 | 19.5 ± 17.8 | 24.2 ± 20.6 | 30.3 ± 20.5 | 21.2 ± 18.9 | < 0.001 | a < b < c | ||
| Changes | 0.9 ± 4.6 | 1.7 ± 4.6 | 2.3 ± 5.1 | 1.2 ± 4.6 | < 0.001 | a < c | ||
| 4,000 Hz | ||||||||
| 2013 | 23.9 ± 19.6 | 28.8 ± 22.1 | 35.2 ± 20.3 | 25.7 ± 20.5 | < 0.001 | a < b < c | ||
| 2017 | 25.2 ± 20.6 | 30.6 ± 22.5 | 38.0 ± 21.8 | 27.2 ± 21.4 | < 0.001 | a < b < c | ||
| Changes | 1.3 ± 5.1 | 1.8 ± 4.8 | 2.8 ± 6.2 | 1.5 ± 5.1 | 0.003 | a, b < c | ||
| Fasting blood glucose group | Events/No. of subjects | Model 1* | Model 2† | Model 3‡ | |
|---|---|---|---|---|---|
| Left ear | |||||
| Normal | 32/1,145 | Reference | Reference | Reference | |
| IFG | 19/341 | 1.29 (0.73–2.29) | 1.31 (0.74–2.32) | 1.35 (0.76–2.41) | |
| DM | 10/59 | 2.76 (1.33–5.72) | 2.80 (1.35–5.80) | 3.35 (1.54–7.29) | |
| Right ear | |||||
| Normal | 17/1,145 | Reference | Reference | Reference | |
| IFG | 10/341 | 1.30 (0.59–2.85) | 1.32 (0.60–2.89) | 1.54 (0.69–3.44) | |
| DM | 6/59 | 3.19 (1.23–8.29) | 3.24 (1.25–8.41) | 5.66 (2.01–15.98) | |
Data are shown as mean ± standard deviation or number (%).
IFG: impaired fasting glucose; DM: diabetes mellitus.
*
Data are shown as mean ± standard deviation or number (%).
IFG: impaired fasting glucose; DM: diabetes mellitus.
*
Data are shown as HR (95% confidence interval).
IFG: impaired fasting glucose; DM: diabetes mellitus; HR: hazard ratio.
*Model 1, adjusted for age, working period; †Model 2, further adjusted for noise level; ‡Model 3, further adjusted for mean arterial pressure, total cholesterol, triglyceride, serum creatinine, smoking, high-risk alcohol intake.
 KSOEM
KSOEM

 Cite
Cite

