Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 29; 2017 > Article
- Research Article Insomnia and hearing impairment among occupational noise exposed male workers
-
Hyeong-Min Lim1, WonYang Kang1, Won-Ju Park1, Keun-Ho Jang2, Ji-Sung Ann1, Jai-Dong Moon1

-
Annals of Occupational and Environmental Medicine 2017;29:36.
DOI: https://doi.org/10.1186/s40557-017-0195-7
Published online: August 15, 2017
1Department of Occupational and Environmental Medicine, Chonnam National University Hwasun Hospital, 322 Seoyang-ro, Hwasun-gun, Jeollanam-do, 58128 Republic of Korea
2Department of Occupational and Environmental Medicine, Mokpo Christian Hospital, 303 Baengnyeon-daero, Mokpo-si, Jeollanam-do, Republic of Korea 
© The Author(s). 2017
Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Abstract
-
Background The aim of this study was to investigate the association between insomnia and hearing impairment among workers exposed to occupational noise.
-
Methods This study included 809 male workers exposed to occupational noise. The participants underwent audiometric testing, and their insomnia was examined based on the Insomnia Severity Index test. Hearing impairment was defined as hearing threshold >25 dB hearing level in the range of 1–4 kHz.
-
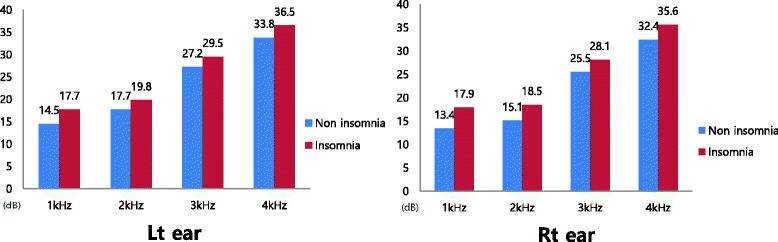
Results According to analysis of covariance, it was observed that pure tone audiometry thresholds at 1–2 kHz in the right ear and at 1 kHz in the left ear were significantly higher among workers with insomnia compared to those with no insomnia. Multiple logistic regression analysis of insomnia for hearing impairments was performed, which showed the odds ratio was 1.806 (95% confidence intervals: 1.022–3.188, p = 0.042) after adjustment for age, working period, noise level, snoring, use of protection devices, diabetes mellitus, hypertension, smoking, alcohol consumption, regular exercise, waist circumference, total cholesterol, triglyceride and high density lipoprotein cholesterol.
-
Conclusion Insomnia could be associated with hearing impairment in workers who are exposed to occupational noise. Additionally, insomnia may be associated with decreased hearing at low frequencies. Especially, more efforts are required to improve the quality of sleep for workers who are exposed to loud occupational noise. Further well- designed prospective studies are needed to clarify the relationship between insomnia and hearing impairment.
Background
Methods
Results
Discussion
Conclusions
Acknowledgements
Abbreviations
ANCOVA
BMI
CI
HDL
ISI
NIHL
OR
- 1. Nelson DI, Nelson RY, Concha-Barrientos M, Fingerhut M. The global burden of occupational noise-induced hearing loss. Am J Ind Med 2005;48:446–458. 10.1002/ajim.20223. 16299704.ArticlePubMed
- 2. http://laborstat.moel.go.kr.
- 3. Johnson J, Robinson ST. In: Ladou J, editor. Hearing loss. Occupational and environmental medicine. 2007, 4th. USA: McGraw-Hill; 104–121.PubMed
- 4. van Kamp I, Davies H. Noise and health in vulnerable groups: a review. Noise Health 2013;15:153–159. 10.4103/1463-1741.112361. 23689296.ArticlePubMed
- 5. van Kamp I, Job RF, Hatfield J, Haines M, Stellato RK, Stansfeld SA. The role of noise sensitivity in the noise-response relation: a comparison of three international airport studies. J Acoust Soc Am 2004;116:3471–3479. 10.1121/1.1810291. 15658698.ArticlePubMedPDF
- 6. Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev 2002;6:97–111. 10.1053/smrv.2002.0186. 12531146.ArticlePubMed
- 7. Ohayon MM, Smirne S. Prevalence and consequences of insomnia disorders in the general population of Italy. Sleep Med 2002;3:115–120. 10.1016/S1389-9457(01)00158-7. 14592229.ArticlePubMed
- 8. Morin CM, LeBlanc M, Daley M, Gregoire JP, Mérette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med 2006;7:123–130. 10.1016/j.sleep.2005.08.008. 16459140.ArticlePubMed
- 9. Simon GE, VonKorff M. Prevalence, burden, and treatment of insomnia in primary care. Am J Psychiatry 1997;154:1417–1423. 10.1176/ajp.154.10.1417. 9326825.ArticlePubMed
- 10. Yeo BK, Perera IS, Kok LP, Tsoi WF. Insomnia in the community. Singap Med J 1996;37:282–284.
- 11. Kim K, Uchiyama M, Okawa M, Liu X, Ogihara R. An epidemiological study of insomnia among the Japanese general population. Sleep 2000;23:41–47. 10.1093/sleep/23.1.1a. 10678464.ArticlePubMed
- 12. Cho YW, Shin WC, Yun CH, Hong SB, Kim J, Earley CJ. Epidemiology of insomnia in korean adults: prevalence and associated factors. J Clin Neurol 2009;5:20–23. 10.3988/jcn.2009.5.1.20. 19513329.ArticlePubMedPMC
- 13. Léger D, Morin CM, Uchiyama M, Hakimi Z, Cure S, Walsh JK. Chronic insomnia, quality-of-life, and utility scores: comparison with good sleepers in a cross-sectional international survey. Sleep Med 2012;13:43–51. 10.1016/j.sleep.2011.03.020. 22093806.ArticlePubMed
- 14. Sarsour K, Morin CM, Foley K, Kalsekar A, Walsh JK. Association of insomnia severity and comorbid medical and psychiatric disorders in a health plan-based sample: insomnia severity and comorbidities. Sleep Med 2010;11:69–74. 10.1016/j.sleep.2009.02.008. 19410512.ArticlePubMed
- 15. Chiang YY, Tsai PY, Chen PC, Yang MH, Li CY, Sung FC, Chen KB. Sleep disorders and traffic accidents. Epidemiology 2012;23:643–644. 10.1097/EDE.0b013e318258cf9a. 22659550.ArticlePubMed
- 16. Laugsand LE, Vatten LJ, Platou C, Janszky I. Insomnia and the risk of acute myocardial infarction: a population study. Circulation 2011;124:2073–2081. 10.1161/CIRCULATIONAHA.111.025858. 22025601.ArticlePubMed
- 17. Laugsand LE, Strand LB, Platou C, Vatten LJ, Janszky I. Insomnia and the risk of incident heart failure: a population study. Eur Heart J 2014;35:1382–1393. 10.1093/eurheartj/eht019. 23462728.ArticlePubMed
- 18. Hasson D, Theorell T, Wallén MB, Leineweber C, Canlon B. Stress and prevalence of hearing problems in the Swedish working population. BMC Public Health 2011;11:130. 10.1186/1471-2458-11-130. 21345187.ArticlePubMedPMCPDF
- 19. Test T, Canfi A, Eyal A, Shoam-Vardi I, Sheiner EK. The influence of hearing impairment on sleep quality among workers exposed to harmful noise. Sleep 2011;34:25–30. 10.1093/sleep/34.1.25. 21203368.ArticlePubMedPMC
- 20. Lee SH, Gu HM, Lee SH, Oh CS, Park WJ. The association between sleeping quality and noise induced hearing loss in aircraft noise exposed workers. J Aerosp Med Cent, ROKAF 2012;2:125–138.
- 21. Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med 2001;2:297–307. 10.1016/S1389-9457(00)00065-4. 11438246.ArticlePubMed
- 22. Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011;34:601–608. 10.1093/sleep/34.5.601. 21532953.ArticlePubMedPMC
- 23. http://www.kosha.or.kr/board.do?menuId=4828.
- 24. Cho YW, Song ML, Morin CM. Validation of a Korean version of the insomnia severity index. J Clin Neurol. 2014;10(3):210–215. 10.3988/jcn.2014.10.3.210. 25045373.ArticlePubMedPMC
- 25. Agrawal Y, Platz EA, Niparko JK. Risk factors for hearing loss in US adults: data from the National Health and Nutrition Examination Survey, 1999 to 2002. Otol Neurotol 2009;30:139–145. 10.1097/MAO.0b013e318192483c. 19092714.PubMed
- 26. Yamane H, Nakai Y, Takayama M, Konishi K, Iguchi H, Nakagawa T, Shibata S, Kato A, Sunami K, Kawakatsu C. The emergence of free radicals after acoustic trauma and strial blood flow. Acta Otolaryngol Suppl 1995;519:87–92. 10.3109/00016489509121877. 7610900.ArticlePubMed
- 27. Van Campen LE, Murphy WJ, Franks JR, Mathias PI, Toraason MA. Oxidative DNA damage is associated with intense noise exposure in the rat. Hear Res 2002;164:29–38. 10.1016/S0378-5955(01)00391-4. 11950522.ArticlePubMed
- 28. Ohinata Y, Miller JM, Altschuler RA, Schacht J. Intense noise induces formation of vasoactive lipid peroxidation products in the cochlea. Brain Res 2000;878:163–173. 10.1016/S0006-8993(00)02733-5. 10996147.ArticlePubMed
- 29. Ohinata Y, Miller JM, Schacht J. Protection from noise-induced lipid peroxidation and hair cell loss in the cochlea. Brain Res 2003;966:265–273. 10.1016/S0006-8993(02)04205-1. 12618349.ArticlePubMed
- 30. Bielefeld EC, Hu BH, Harris KC, Henderson D. Damage and threshold shift resulting from cochlear exposure to paraquat-generated superoxide. Hear Res 2005;207:35–42. 10.1016/j.heares.2005.03.025. 15935579.ArticlePubMedPMC
- 31. Gulec M, Ozkol H, Selvi Y, Tuluce Y, Aydin A, Besiroglu L, Ozdemir PG. Oxidative stress in patients with primary insomnia. Prog Neuro-Psychopharmacol Biol Psychiatry 2012;37:247–251. 10.1016/j.pnpbp.2012.02.011.Article
- 32. Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet 1999;354:1435–1439. 10.1016/S0140-6736(99)01376-8. 10543671.ArticlePubMed
- 33. Amihăesei IC, Mungiu OC. Main neuroendocrine features and therapy in primary sleep troubles. Rev Med Chir Soc Med Nat Iasi 2012;116:862–866. 23272543.PubMed
- 34. Sidman JD, Prazma J, Pulver SH, Pillsbury HC 3rd. Cochlea and heart as end-organs in small vessel disease. Ann Otol Rhinol Laryngol 1988;97:9–13. 10.1177/000348948809700102. 3341708.ArticlePubMedPDF
- 35. Yamasoba T, Kikuchi S, Higo R, O'uchi T, Tokumaru A. Sudden sensorineural hearing loss associated with slow blood flow of the vertebrobasilar system. Ann Otol Rhinol Laryngol 1993;102:873–877. 10.1177/000348949310201110. 8239350.ArticlePubMedPDF
- 36. Härmä M, Tenkanen L, Sjöblom T, Alikoski T, Heinsalmi P. Combined effects of shift work and life-style on the prevalence of insomnia, sleep deprivation and daytime sleepiness. Scand J Work Environ Health 1998;24(4):300–307. 10.5271/sjweh.324. 9754862.ArticlePubMed
- 37. Drake CL, Roehrs T, Richardson G, Walsh JK, Roth T. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep 2004;27(8):1453–1462. 10.1093/sleep/27.8.1453. 15683134.ArticlePubMed
- 38. Johnson EO, Roth T, Schultz L, Breslau N. Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics 2006;117:e247–e256. 10.1542/peds.2004-2629. 16452333.ArticlePubMedPDF
REFERENCES
Notes
Figure & Data
REFERENCES
Citations

- A review of the studies investigating the effects of noise exposure on humans from 2017 to 2022: Trends and knowledge gaps
Mohammad Javad SheikhMozafari, Soqrat Omari Shekaftik, Fatameh Fasih Ramandi, Mohammad Reza Monazzam Esmaeelpour, Jamal Biganeh
Noise Mapping.2025;[Epub] CrossRef - Echoes in the night: How sleep quality influences auditory health
Peng Zhang, Xiaogang An, Runqin Yang, Meihao Qi, Zejun Gao, Xinyu Zhang, Ziqi Wu, Zeyu Zheng, Xinyu Dong, Wenyue Wang, Xiaocheng Wang, Dingjun Zha
Neuroscience.2025; 577: 200. CrossRef - Sleep characteristics and hearing loss in middle-aged and older adults: The National Health and Nutrition Examination Survey 2015–2018
Kening Jiang, Adam P. Spira, Nicholas S. Reed, Frank R. Lin, Jennifer A. Deal
Sleep Epidemiology.2024; 4: 100082. CrossRef - The sound of safety: exploring the determinants of prevention intention in noisy industrial workplaces
Hyeon Jo, Eun-Mi Baek
BMC Public Health.2024;[Epub] CrossRef - The Global Prevalence of Noise Induced Hearing Impairment Among Industrial Workers: A Systematic Review and Meta-Analysis
Nader Salari, Amin Hosseinian-Far, Hosna Zarei, Shabnam Rasoulpoor, Hooman Ghasemi, Hadis Elyasi, Masoud Mohammadi
Indian Journal of Otolaryngology and Head & Neck Surgery.2024; 76(6): 5035. CrossRef - Effects mediated by melatonin and cortisol of artificial light and noise, alone and in combination, on sleep and health
Nahum M. Gabinet
Exploration of Neuroscience.2024; 3(5): 382. CrossRef - Associations of sleep characteristics in late midlife with late-life hearing loss in the Atherosclerosis Risk in Communities-Sleep Heart Health Study (ARIC-SHHS)
Kening Jiang, Adam P. Spira, Rebecca F. Gottesman, Kelsie M. Full, Frank R. Lin, Pamela L. Lutsey, Emmanuel E. Garcia Morales, Naresh M. Punjabi, Nicholas S. Reed, A. Richey Sharrett, Jennifer A. Deal
Sleep Health.2023; 9(5): 742. CrossRef - Duration and Quality of Sleep and Risk of Self-reported Hearing Loss: The UK Biobank Study
Humberto Yévenes-Briones, Francisco Félix Caballero, Daniela B. Estrada-deLeón, Ellen A. Struijk, Arthur Eumann Mesas, José R. Banegas, Fernando Rodríguez-Artalejo, Esther Lopez-García
Ear & Hearing.2023; 44(5): 1182. CrossRef - Sleep quality and sleep-related issues in industrial workers: a global meta-analysis
Sohrab Amiri
International Journal of Occupational Safety and Ergonomics.2023; 29(1): 154. CrossRef - Obstructive sleep apnea risk and hearing impairment among occupational noise-exposed male workers
Seunghyeon Cho, Won-Ju Park, Ji-Sung Ahn, Dae-Young Lim, Su-Hwan Kim, Jai-Dong Moon
Archives of Environmental & Occupational Health.2023; 78(2): 108. CrossRef - Association of nocturnal sleep duration and midday napping with subjective poor hearing among middle-aged and older adults in China
Xiaorui Cui, Zixuan Lu, Xinyue Guo, Neng Dai, Chen Huang, Yahang Liu, Ruilang Lin, Yongfu Yu, Guoyou Qin, Jiaohua Chen
Frontiers in Public Health.2023;[Epub] CrossRef - Association of sleep duration and noise exposure with hearing loss among Chinese and American adults: two cross-sectional studies
E Wu, Juntao Ni, Zhaohui Zhu, Hongquan Xu, Jun Ci, Lin Tao, Tian Xie
BMJ Open.2022; 12(9): e062535. CrossRef - Sleep Characteristics and Hearing Loss in Older Adults: The National Health and Nutrition Examination Survey 2005–2006
Kening Jiang, Adam P Spira, Nicholas S Reed, Frank R Lin, Jennifer A Deal, Lewis Lipsitz
The Journals of Gerontology: Series A.2022; 77(3): 632. CrossRef - Association of sudden sensorineural hearing loss with increased risk of insomnia: a nationwide population-based cohort study
Cha Dong Yeo, Sang Woo Yeom, Yeon Seok You, Jong Seung Kim, Eun Jung Lee
Journal of Clinical Sleep Medicine.2022; 18(5): 1335. CrossRef - Using mobile phones as light at night and noise measurement instruments: a validation test in real world conditions
Nahum M. Gabinet, Hassan Shama, Boris A. Portnov
Chronobiology International.2022; 39(1): 26. CrossRef - Prevalence of current and former smoking in industrial workers worldwide: a systematic review and meta-analysis
Sohrab Amiri, Seyed Morteza Hosseini
Journal of Addictive Diseases.2021; 39(3): 288. CrossRef - The Relationship Between Blast-related Hearing Threshold Shift and Insomnia in U.S. Military Personnel
Andrew J MacGregor, Antony R Joseph, Rachel R Markwald, Amber L Dougherty
Military Medicine.2021; 186(9-10): 844. CrossRef - Risk of hearing loss in patients with fibromyalgia: A nationwide population-based retrospective cohort study
Thi Phuong Le, Ya-Ling Tzeng, Chih-Hsin Muo, Hua Ting, Fung-Chang Sung, Shin-Da Lee, Yu-Kuei Teng, Pilar Serra-Añó
PLOS ONE.2020; 15(9): e0238502. CrossRef - The relationship between hearing loss and insomnia for patients with tinnitus
Hashir Aazh, Marja Heinonen-Guzejev, Brian C. J. Moore
International Journal of Audiology.2020; 59(1): 68. CrossRef - Tinnitus loudness and the severity of insomnia: a mediation analysis
Hashir Aazh, Brian C. J. Moore
International Journal of Audiology.2019; 58(4): 208. CrossRef - Evidence for an Association Between Hearing Impairment and Disrupted Sleep: Scoping Review
Nathan A. Clarke, Derek J. Hoare, Edward C. Killan
American Journal of Audiology.2019; 28(4): 1015. CrossRef
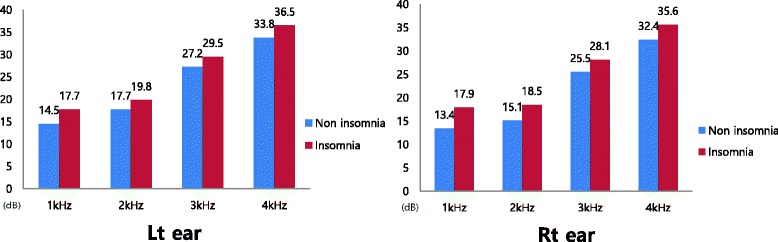
Fig. 1
| Variables | Frequency (%) or mean ± SD | p-value* | |
|---|---|---|---|
| Normal hearing (N = 277) | Hearing impairment (N = 532) | ||
| Age (years) | 43.7 ± 5.8 | 46.8 ± 6.0 | <0.001 |
| Working period (years) | 17.5 ± 6.5 | 22.8 ± 6.1 | <0.001 |
| Noise level (decibel) | 79.1 ± 3.6 | 80.3 ± 2.8 | 0.010 |
| Waist circumference (cm) | 84.8 ± 7.2 | 85.5 ± 7.2 | 0.181 |
| Body mass index (kg/m2) | 24.5 ± 3.0 | 24.7 ± 2.7 | 0.304 |
| Systolic blood pressure (mmHg) | 125.7 ± 11.1 | 125.5 ± 9.3 | 0.781 |
| Diastolic blood pressure (mmHg) | 81.8 ± 6.9 | 81.7 ± 6.9 | 0.809 |
| Total cholesterol (mg/dL) | 195.1 ± 32.5 | 196.1 ± 34.2 | 0.677 |
| Triglyceride (mg/dL) | 167.6 ± 127.4 | 162.3 ± 108.4 | 0.533 |
| HDL cholesterol (mg/dL) | 47.1 ± 9.9 | 48.0 ± 11.0 | 0.295 |
| Glucose (g/dL) | 105.3 ± 17.3 | 108.4 ± 24.4 | 0.063 |
| ISI score | 7.9 ± 4.8 | 8.7 ± 5.3 | 0.039 |
| Smoking | 0.863 | ||
| Non-smoker | 61 (22.0) | 120 (22.6) | |
| Ex- or current smoker | 216 (78.0) | 412 (77.4) | |
| Drinking | 0.924 | ||
| Non-drinker | 71 (25.6) | 138 (25.9) | |
| Drinker | 206 (74.4) | 394 (74.1) | |
| Exercise | 0.892 | ||
| Physical inactivity | 94 (33.9) | 178 (33.5) | |
| Physical activity | 183 (66.1) | 354 (66.5) | |
| Hypertension | 0.058 | ||
| No | 262 (94.6) | 483 (90.8) | |
| Yes | 15 (5.4) | 49 (9.2) | |
| Diabetes mellitus | 0.329 | ||
| No | 268 (96.8) | 507 (95.3) | |
| Yes | 9 (3.2) | 25 (4.7) | |
| Snoring | <0.001 | ||
| No | 208 (75.1) | 280 (52.6) | |
| Yes | 69 (24.9) | 252 (47.4) | |
| Protection device use | 0.001 | ||
| No or seldom | 98 (35.4) | 255 (47.9) | |
| Always | 179 (64.6) | 277 (52.1) | |
| Insomnia | 0.022 | ||
| No | 255 (92.1) | 461 (86.7) | |
| Yes | 22 (7.9) | 71 (13.3) | |
| Frequency | Mean ± SD | p-value* | p-value† | |
|---|---|---|---|---|
| Non insomnia (N = 716) | Insomnia (N = 93) | |||
| Left ear | ||||
| 1 kHz | 14.5 ± 9.8 | 17.7 ± 12.6 | 0.068 | 0.026 |
| 2 kHz | 17.7 ± 12.6 | 19.8 ± 14.9 | 0.139 | 0.191 |
| 3 kHz | 27.2 ± 19.2 | 29.5 ± 19.3 | 0.271 | 0.342 |
| 4 kHz | 33.8 ± 21.2 | 36.5 ± 20.4 | 0.242 | 0.351 |
| Right ear | ||||
| 1 kHz | 13.4 ± 9.0 | 17.9 ± 15.4 | 0.007 | 0.001 |
| 2 kHz | 15.1 ± 10.8 | 18.5 ± 14.2 | 0.028 | 0.004 |
| 3 kHz | 25.5 ± 17.9 | 28.1 ± 18.5 | 0.190 | 0.256 |
| 4 kHz | 32.4 ± 20.9 | 35.6 ± 22.0 | 0.174 | 0.255 |
| B (S.E.) | OR | 95% CI | p-value | |
|---|---|---|---|---|
| Model 1 | 0.031 (0.016) | 1.032 | 1.001 to 1.064 | 0.045 |
| Model 2 | 0.026 (0.016) | 1.026 | 0.994 to 1.060 | 0.112 |
| Model 3 | 0.026 (0.016) | 1.026 | 0.994 to 1.060 | 0.116 |
| Model 4 | 0.025 (0.017) | 1.025 | 0.992 to 1.059 | 0.135 |
| B (S.E.) | OR | 95% CI | p-value | |
|---|---|---|---|---|
| Model 1 | 0.710 (0.274) | 2.033 | 1.190 to 3.476 | 0.009 |
| Model 2 | 0.606 (0.288) | 1.834 | 1.043 to 3.225 | 0.035 |
| Model 3 | 0.611 (0.289) | 1.842 | 1.046 to 3.242 | 0.034 |
| Model 4 | 0.591 (0.290) | 1.806 | 1.022 to 3.188 | 0.042 |
*
*
†
aThe unit of Insomnia Severity Index score is 1 point
Model 1; adjusted for age
Model 2; adjusted for age, working period, noise level, protection device use and snoring. Model 3; adjusted for age, working period, noise level, protection device use, snoring, diabetes mellitus and hypertension
Model 4; adjusted for age, working period, noise level, snoring, protection device use, diabetes mellitus, hypertension, smoking, alcohol consumption, regular exercise, total cholesterol, triglyceride, HDL cholesterol and waist circumference
aInsomnia group was defined as more than Insomnia Severity Index score 14 points
Model 1; adjusted for age
Model 2; adjusted for age, working period, noise level, protection device use and snoring. Model 3; adjusted for age, working period, noise level, protection device use, snoring, diabetes mellitus and hypertension
Model 4; adjusted for age, working period, noise level, snoring, protection device use, diabetes mellitus, hypertension, smoking, alcohol consumption, regular exercise, total cholesterol, triglyceride, HDL cholesterol and waist circumference
 KSOEM
KSOEM

 Cite
Cite

