Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 29; 2017 > Article
- Case Report Cases of acute mercury poisoning by mercury vapor exposure during the demolition of a fluorescent lamp factory
-
Sang Yoon Do1, Chul Gab Lee1, Jae Yoon Kim1, Young Hoon Moon1, Min Sung Kim2, In Ho Bae2, Han Soo Song1

-
Annals of Occupational and Environmental Medicine 2017;29:19.
DOI: https://doi.org/10.1186/s40557-017-0184-x
Published online: June 20, 2017
1Department of Occupational & Environmental Medicine, School of Medicine, Chosun University Hospital, 365 Pilmun-daero Dong-gu, Gwangju, 61453 South Korea
2Department of Dermatology, School of Medicine, Chosun University Hospital, 365 Pilmun-daero Dong-gu, Gwangju, 61453 South Korea
© The Author(s). 2017
Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Abstract
-
Background In 2015, workers dismantling a fluorescent lamp factory in Korea were affected by mercury poisoning from exposure to mercury vapor.
-
Case presentation Eighteen out of the 21 workers who participated in the demolition project presented with symptoms of poisoning and, of these, 10 had persistent symptoms even at 18 months after the initial exposure to mercury vapor. Early symptoms of 18 workers included a general skin rash, pruritus, myalgia, sleep disturbance, and cough and sputum production. Following alleviation of these initial symptoms, late symptoms, such as easy fatigue, insomnia, bad dreams, and anxiety disorder, began to manifest in 10 out of 18 patients. Seven workers underwent psychiatric care owing to sleep disturbance, anxiety disorder, and depression, and three workers underwent dermatologic treatment for hyperpigmentation, erythematous skin eruption, and chloracne-like skin lesions. Furthermore, three workers developed a coarse jerky movement, two had swan neck deformity of the fingers, and two received care at an anesthesiology clinic for paresthesia, such as burning sensation, cold sensation, and pain. Two workers underwent urologic treatment for dysfunction of the urologic system and impotence. However, symptomatic treatment did not result in satisfactory relief of these symptoms.
-
Conclusion Awareness of the perils of mercury and prevention of mercury exposure are critical for preventing health hazards caused by mercury vapor. Chelation therapy should be performed promptly following mercury poisoning to minimize damage.
Background
Case presentation
Patient information
Chief complaint
Past history
Smoking history
Alcohol history
Occupational history
Present illness
Physical examination
Laboratory findings
Progression
Patient information
Chief complaint
Past history
Smoking history
Alcohol history
Occupational history
Present illness
Physical examination
Laboratory findings
Progression
Discussion and conclusions
Acknowledgements
Abbreviations
ALT
ARB
ASGM
AST
BUN
CFL
c-GTP
DITI
DMPS
DMSA
LED
NSAIDs
OEM
OSHRI
UNEP
- 1. https://wedocs.unep.org/bitstream/handle/20.500.11822/11610/HgSupplyTradeDemandJM.pdf?sequence=1&isAllowed=y.
- 2. https://wedocs.unep.org/bitstream/handle/20.500.11822/11517/UNEP_GlobalAtmosphericMercuryAssessment_May2009.pdf?sequence=1&isAllowed=y.
- 3. Gibb H, O'Leary KG. Mercury exposure and health impacts among individuals in the artisanal and small-scale gold mining community: a comprehensive review. Environ Health Perspect 2014;122:667–672. 24682486.ArticlePubMedPMC
- 4. http://wedocs.unep.org//handle/20.500.11822/7984.
- 5. Park J, Kim Y. The history of occupational health service in Korea. Ind Health 1998;36:393–401. 10.2486/indhealth.36.393. 9810157.ArticlePubMed
- 6. Kim EA, Kang SK. Occupational neurological disorders in Korea. J Korean Med Sci 2010;25:S26–S35. 10.3346/jkms.2010.25.S.S26. 21258587.ArticlePubMedPMC
- 7. http://oshri.kosha.or.kr/main?act=VIEW&boardId=4&urlCode=T1%7C%7C5272%7C366%7C366%7C374%7C5272%7C%7C/cms/board/board/Board.jsp?communityKey=B0821&communityKey=B0821.
- 8. Clarkson TW, Magos L. The toxicology of mercury and its chemical compounds. Crit Rev Toxicol 2006;36(8):609–662. 10.1080/10408440600845619. 16973445.ArticlePubMed
- 9. Risher JF, Amler SN. Mercury exposure: evaluation and intervention the inappropriate use of chelating agents in the diagnosis and treatment of putative mercury poisoning. Neurotoxicology 2005;26(4):691–699. 10.1016/j.neuro.2005.05.004. 16009427.ArticlePubMed
- 10. Milne J, Christophers A, de Silva P. Acute mercurial pneumonitis. Br J Ind Med 1970;27(4):334–338. 5488692.ArticlePubMedPMC
- 11. Henningsson C, Hoffmann S, McGonigle L, Winter JS. Acute mercury poisoning (acrodynia) mimicking pheochromocytoma in an adolescent. J Pediatr 1993;122(2):252–253. 10.1016/S0022-3476(06)80125-3. 8429442.ArticlePubMed
- 12. Ozuah PO. Mercury poisoning. Curr Probl Pediatr 2000;30(3):91–99. 10.1067/mps.2000.104054. 10742922.ArticlePubMed
- 13. Monamy B, Donald H, Reginald M, Kenneth MAP. Chronic mercury poisoning. Br J Ind Med 1946;3(2):55–63. 20991165.ArticlePubMedPMC
- 14. Bernhoft RA. Mercury toxicity and treatment: a review of the literature. J Environ Public Health 2012;2012:460508. 10.1155/2012/460508. 22235210.ArticlePubMedPDF
- 15. Wągrowska-Danilewicz M, Danilewicz M, Zbrog Z. Mercury-induced nephrotic syndrome: a case report and review of the literature. Pol J Pathol 2014;65:322–326. 10.5114/pjp.2014.48194. 25693087.PubMed
- 16. Akgül N, Altunkaynak BZ, Altunkaynak ME, Deniz ÖG, Ünal D, Akgül HM. Inhalation of mercury vapor can cause the toxic effects on rat kidney. Ren Fail 2016;38:465–473. 10.3109/0886022X.2016.1138832. 26888214.ArticlePubMed
- 17. Boyd AS, Seger D, Vannucci S, Langley M, Abraham JL, King LE Jr. Mercury exposure and cutaneous disease. J Am Acad Dermatol 2000;43:81–90. 10.1067/mjd.2000.106360. 10863229.ArticlePubMed
- 18. Charruau B, Laulan J, Saint-Cast Y. Lateral band translocation for swan-neck deformity: outcomes of 41 digits after a mean follow-up of eight years. Orthop Traumatol Surg Res 2016;102:S221–S224. 10.1016/j.otsr.2016.03.008. 27036508.ArticlePubMed
- 19. Smith RG, Vorwald AJ, Patil LS, Mooney TF. Effects of exposure to mercury in the manufacture of chlorine. Am Ind Hyg Assoc J 1970;31:687–700. 10.1080/0002889708506315. 5275968.ArticlePubMed
- 20.
- 21. Piikivi L. Cardiovascular reflexes low long-term exposure to mercury vapour. Int Arch Occup Environ Health 1989;61:391–395. 10.1007/BF00381030. 2744870.PubMed
- 22. Friberg L, Hammarstrom S, Nystrom A. Kidney injury after exposure to inorganic mercury. AMA Arch Ind Hyg Occup Med 1953;8:149. 13064872.PubMed
- 23. Seaton A, Bishop CM. Acute mercury pneumonitis. Brit J Industr Med 1978;35:258–265. 698142.ArticlePubMedPMC
- 24. Clarkson TW, Vyas JB, Ballatori N. Mechanisms of mercury disposition in the body. Am J Ind Med 2007;50(10):757–764. 10.1002/ajim.20476. 17477364.ArticlePubMed
- 25. Park JD, Zheng W. Human exposure and health effects of inorganic and elemental mercury. J Prev Med Public Health 2012;45(6):344–352. 10.3961/jpmph.2012.45.6.344. 23230464.ArticlePubMedPMC
- 26. Rooney JP. The retention time of inorganic mercury in the brain--a systematic review of the evidence. Toxicol Appl Pharmacol 2014;274(3):425–435. 10.1016/j.taap.2013.12.011. 24368178.ArticlePubMed
- 27. Kosnett MJ. The role of chelation in the treatment of arsenic and mercury poisoning. J Med Toxicol 2013;9(4):347–354. 10.1007/s13181-013-0344-5. 24178900.ArticlePubMedPMCPDF
REFERENCES
Figure & Data
REFERENCES
Citations

- Potential Impact of Heavy Metals and Microplastics in River Ecosystem on Aquatic Organisms and Human Health, and Sustainable Mitigation Approaches
Himanshu K. Pathak, Kavita Gandhi, Rajeev Pratap Singh
Water, Air, & Soil Pollution.2026;[Epub] CrossRef - Association between heavy metals exposure and depression: findings of the NHANES from 2003 to 2020
Yuanxin Guo, Yixu Chen, Houfeng Zhou, Yuting Fan, Tao Feng, Zhongrui Ma
European Journal of Medical Research.2026;[Epub] CrossRef - Occupational disease monitoring by the Korea Occupational Disease
Surveillance Center: a narrative review
Dong-Wook Lee, Inah Kim, Jungho Hwang, Sunhaeng Choi, Tae-Won Jang, Insung Chung, Hwan-Cheol Kim, Jaebum Park, Jungwon Kim, Kyoung Sook Jeong, Youngki Kim, Eun-Soo Lee, Yangwoo Kim, Inchul Jeong, Hyunjeong Oh, Hyeoncheol Oh, Jea Chul Ha, Jeehee Min, Chul
The Ewha Medical Journal.2025;[Epub] CrossRef - Exposure to heavy metal elements may significantly increase serum prostate-specific antigen levels with overdosed dietary zinc
Yinyi Fang, Chi Chen, Xiaoyue Chen, Jukun Song, Shuangshuang Feng, Zhuang Li, Zhengnan Li, Yuliang Xiong, Qinyi Zhang, Hao Su, Heng Liu, Guohua Zhu, Bin Hu, Wei Wang, Zhangcheng Liu, Ke Jiao, Chang Zhang, Fan Zhang, Kehua Jiang, Jun He, Zhaolin Sun, Dongb
Ecotoxicology and Environmental Safety.2024; 272: 116080. CrossRef - Environmental and genetic predictors of whole blood mercury and selenium concentrations in pregnant women in a UK birth cohort
Kyle Dack, Peiyuan Huang, Caroline M Taylor, Dheeraj Rai, Sarah J Lewis
Environmental Advances.2024; 15: 100469. CrossRef - Promising the potential of β-caryophyllene on mercury chloride–induced alteration in cerebellum and spinal cord of young Wistar albino rats
Ahmad Yahyazadeh, Fatih Mehmet Gur
Naunyn-Schmiedeberg's Archives of Pharmacology.2024; 397(12): 10175. CrossRef - Metal Oxide-Based Adsorbents for Removal of Mercury in Aqueous Media: A Mini-Review
Saheed Abiola Raheem, Emmanuel Anuoluwapo Oke, Olutayo Abiodun Oluyinka, Taofik Adewale Adedosu, Haleema Omolola Adedosu
Chemistry Africa.2024; 7(9): 4683. CrossRef - Genome-Wide Association Study of Blood Mercury in European Pregnant Women and Children
Kyle Dack, Mariona Bustamante, Caroline M. Taylor, Sabrina Llop, Manuel Lozano, Paul Yousefi, Regina Gražulevičienė, Kristine Bjerve Gutzkow, Anne Lise Brantsæter, Dan Mason, Georgia Escaramís, Sarah J. Lewis
Genes.2023; 14(12): 2123. CrossRef - Investigation and monitoring of heavy metal poisoning
Nicola L Barlow, Sally M Bradberry
Journal of Clinical Pathology.2023; 76(2): 82. CrossRef - Clinical and Forensic Signs Resulting from Exposure to Heavy Metals and Other Chemical Elements of the Periodic Table
Carolina de Carvalho Machado, Ricardo Jorge Dinis-Oliveira
Journal of Clinical Medicine.2023; 12(7): 2591. CrossRef - Imprégnation mercurielle lors de travaux de dépollution d’anciens sites de production de chlore : premiers résultats
F. Testud, C. Bidaud, M.F. Arquillière, A. Guéry, M. Winnefeld
Archives des Maladies Professionnelles et de l'Environnement.2023; 84(6): 101878. CrossRef - Fluorescent lamps: A review on environmental concerns and current recycling perspectives highlighting Hg and rare earth elements
Laís Nascimento Viana, Ana Paula Senra Soares, Daniel Lima Guimarães, Wendy Johana Sandoval Rojano, Tatiana Dillenburg Saint'Pierre
Journal of Environmental Chemical Engineering.2022; 10(6): 108915. CrossRef - Mercury Exposure Among Artisanal and Small-Scale Gold Miners in Four Regions in Uganda
Mercy Wendy Wanyana, Friday E. Agaba, Deogratias K. Sekimpi, Victoria N. Mukasa, Geoffrey N. Kamese, Nkonge Douglas, John C. Ssempebwa
Journal of Health and Pollution.2020;[Epub] CrossRef - Mercury exposure in relation to sleep duration, timing, and fragmentation among adolescents in Mexico City
Erica C. Jansen, Emily C. Hector, Jaclyn M. Goodrich, Alejandra Cantoral, Martha María Téllez Rojo, Niladri Basu, Peter X.K. Song, Libni Torres Olascoaga, Karen E. Peterson
Environmental Research.2020; 191: 110216. CrossRef - Nanosized Copper Selenide for Mercury Removal from Indoor Air and Emergency Disposal of Liquid Mercury Leakage
Shengcai Wang, Jianping Yang, Zequn Yang, Wenbing Zhu, Hailong Li, Jianfei Song, Xueyi Guo
Industrial & Engineering Chemistry Research.2019; 58(47): 21881. CrossRef - Exposure routes and health effects of heavy metals on children
Muwaffak Al osman, Fei Yang, Isaac Yaw Massey
BioMetals.2019; 32(4): 563. CrossRef
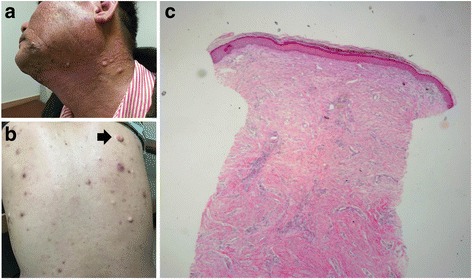

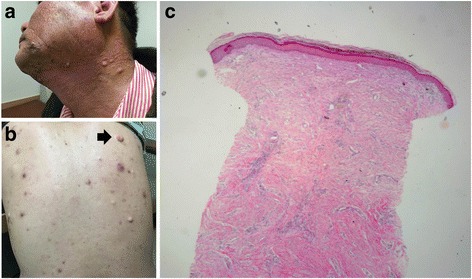
Fig. 1
Fig. 2
| Early symptoms | N | (%) |
|---|---|---|
| Skin rash | 17 | (85%) |
| Pruritus | 9 | (45%) |
| Myalgia | 8 | (40%) |
| Sleep disturbance | 6 | (30%) |
| Cough or Sputum production | 5 | (25%) |
| Paresthesia of the extremities | 4 | (20%) |
| Fatigue | 4 | (20%) |
| Other skin symptoms (scale, scalding, irritation) | 2 | (10%) |
| Headache | 2 | (10%) |
| Gastrointestinal symptoms (dyspepsia, nausea, vomiting) | 2 | (10%) |
| Tooth and gum symptoms (toothache, moving teeth, gum swelling) | 2 | (10%) |
| Urinary symptoms (frequency, incontinence, sensation of incomplete urine voiding) | 1 | (5%) |
| Eye symptoms (red eye, decreased visual acuity) | 1 | (5%) |
| High blood pressure | 1 | (5%) |
| Type of work | N | Working day (day(s)) | Blood Mercurya (μg/L) | Adjusted Urinary mercurya (μg/L·creatinine) | |||
|---|---|---|---|---|---|---|---|
| mean (range) | mean (SD) | mean (SD) | |||||
| Total | 20 | 10.2 | (1–30) | 5.88 | (4.49) | 13.48 | (15.40) |
| Ordering | 3 | 30 | (30) | 5.67 | (3.48) | 12.21 | (12.84) |
| Cutting | 6 | 8.5 | (1–15) | 7.34 | (7.87) | 22.04 | (11.92) |
| Machinery operating | 5 | 2.4 | (1–6) | 5.25 | (2.27) | 0.99 | (0.55) |
| Transporting | 6 | 8.5 | (2–15) | 5.04 | (1.39) | 15.95 | (21.02) |
| Patient | Age | Task | Working day | Symptoms |
|---|---|---|---|---|
| A | 43 | Ordering | 30 | G: severe fatigue, anorexia, non-specific exertional dyspnea M: mercurial tremor, coarse jerky movement of the right arm and leg, mild swan neck deformity of the right hand 3rd, 4th, and 5th fingers P: anxiety, depression, sleeplessness, bad dreams O: decreased visual acuity, blurred vision, - Consultation: neuropsychiatry & ophthalmology |
| B (Case 1) | 40 | Ordering | 30 | G: severe fatigue, dizziness, non-specific exertional dyspnea M: lower limb swelling D: dark skin patches, epidermal cysts, chloracne like skin lesions, pruritus P: anxiety, depression, sleeplessness, bad dreams, - Consultation: neuropsychiatry and dermatology |
| E | 53 | Cutting | 7 | P: sleeplessness, bad dream, loss of memory |
| F | 52 | Cutting | 7 | G: general myalgia M: thumb muscle weakness and numbness, coarse jerky movement of the lower limb P: sleeplessness, sleep-talking |
| G (Case 2) | 60 | Cutting | 15 | G: easy fatigue M: bilateral pain and paresthesia of the feet, swan neck deformity of both fingers without joint pain, coarse jerky movement of the lower limb P: anxiety, sleeplessness, bad dream U: residual urine sense, urine leak, weak urine stream, impotence - Consultation: neuropsychiatry, urology and pain clinic |
| I | 47 | Transporting | 8 | G: easy fatigue D: hyperpigmentation, urticarial dermatitis in whole body skin P: sleeplessness, bad dream, anxiety, depression, suicidal tendency - Consultation: neuropsychiatry and dermatology |
| J | 50 | Transporting | 9 | P: loss of memory, sleeplessness, headache, anxiety - Consultation: neuropsychiatry |
| K | 46 | Transporting | 10 | D: multiple various sized erythematous patches with itching sense O: decreased visual acuity, blurred vision P: headache, anxiety - Consultation: neuropsychiatry & dermatology |
| P | 55 | Cutting | 15 | G: general myalgia and weakness, non-specific exertional dyspnea, easy fatigue, dizziness M: coarse jerky movement of lower limb, bilateral pain and paresthesia of the feet D: skin rash and itching sense, sleeplessness - Consultation: neuropsychiatry and neurology |
| S | 44 | Cutting | 6 | G: general myalgia, sleeplessness, easy fatigue, dyspepsia, dizziness, gum pain M: edema of the dorsal aspect of the foot, hand, eyelid and neck P: anxiety, sleeplessness, bad dreams U: sensation of incomplete voiding after micturition, urine leak, weak urine flow, impotence - Consultation: urology |
a Earliest laboratory values preformed within 200–300 days from the last work day
Ordering: instructing somebody who does other type of task to do their task and cleaning work site
Cutting: dismembering facilities and tearing down
Machinery operating: operating machinery vehicle (including forklifts and high place operating cars)
Transporting: manual laborers who transport dismantled facilities and waste
 KSOEM
KSOEM


 Cite
Cite

