Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 29; 2017 > Article
- Review A socioecological framework for research on work and obesity in diverse urban transit operators based on gender, race, and ethnicity
- BongKyoo Choi1, Peter Schnall1, Marnie Dobson1, Haiou Yang1, Dean Baker1, YoungJu Seo2
-
Annals of Occupational and Environmental Medicine 2017;29:15.
DOI: https://doi.org/10.1186/s40557-017-0171-2
Published online: May 17, 2017
1Center for Occupational and Environmental Health, University of California Irvine, 100 Theory, Suite 100, Irvine, CA 92617 USA
2Department of Sociology, University of Massachusetts Amherst, 200 Hicks Way, Amherst, MA 01003 USA
© The Author(s). 2017
Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Abstract
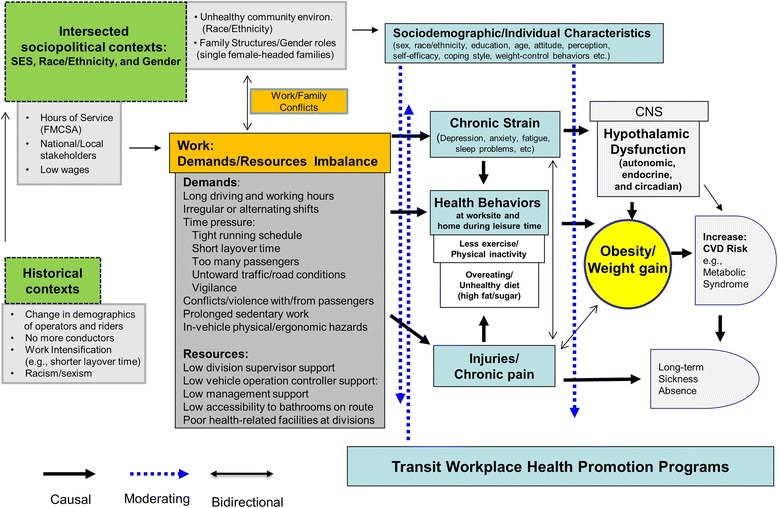
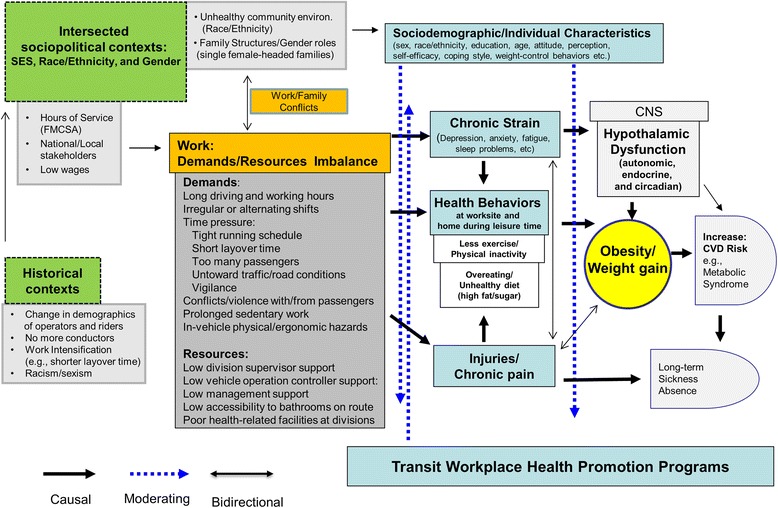
- Urban transit (bus and rail) operators, totaling nearly 700,000 persons, are one of the heaviest occupational groups in the United States (US). Little is known about occupational risk factors for weight gain and obesity and their interrelationship with health-related behaviors, particularly among female minority (African Americans and Hispanics) transit operators who are at greater risk for obesity. As a step towards developing successful obesity interventions among urban transit operators, this paper aims to present a new socioecological framework for studying working conditions, chronic strain, health-related behaviors, weight gain/obesity, and obesity disparity in diverse urban transit operators based on gender, race, and ethnicity. Our framework is a synthesis of several different theories and disciplines: the resource-work load model (work stress), occupational ergonomics, the theory of intersectionality, and worksite health promotion. The framework was developed utilizing an extensive literature review, results from our on-going research on obesity, input from focus groups conducted with Los Angeles transit operators as well as interviews and meetings with transit operator stakeholders (management, unions, and worksite transit wellness program), and ride-along observations. Our hypotheses highlighted in the framework (see Fig. 1) are that adverse working conditions, largely characterized as a combination of high demands and low resources, will increase the risk for weight gain/obesity among transit operators directly through chronic strain and hypothalamic dysfunction (hyper-and hypo-activations), and indirectly through health-related behaviors and injuries/chronic severe pain. We also hypothesize that the observed increase in adiposity among female minority operators is due to their greater exposure to adverse occupational and non-occupational conditions that reflect their intersecting social identities of lower social class and being a minority woman in the US. Our proposed framework could greatly facilitate future transit worksite obesity studies by clarifying the complex and important roles of adverse working conditions in the etiology of weight gain/obesity and obesity disparity among transit operators and other working populations.
Background
Development of a new socioecological framework for studying working conditions, chronic strain, health-related behaviors, weight gain/obesity, and obesity disparity in urban transit operators
Working conditions: detailed work schedules, sedentary work time, time pressure (short intervals between stops, high passenger load, high traffic load, constant threat avoidance vigilance, and short layover time) [61, 66], coworker and supervisor support [14, 116, 142], conflicts with passengers [64, 143], physical demands [142, 144], worksite food/physical activity environment [145], worksite discrimination [146–148], and in-vehicle ergonomic hazards (eight-item scale about the seat, vibration, and heat/cold/draft) [17]
Health behaviors at work and during leisure time: eating behaviors and exercise at worksite and at home [92, 108, 149, 150], including stress-induced overeating, weight control behaviors [151], and impaired exercise/physical activity due to work-related injuries/chronic severe pain in the past year [152]
Health conditions: weight perception (body image), work-related injuries (resulting in > 2 weeks of sickness absence in the past year) [153, 154], chronic severe pain on muscle/joints in the past year (lasting > 30 days) [27, 119, 152], mental health (depression, exhaustion, sleep quality and hours. etc.), and chronic diseases (hypertension, hyperlipidemia, and diabetes)
Community and family variables: neighborhood and community health promotion facilities [155], work-family conflicts [156], and family structure variables including household head, number of young children, and household work hours [129]
Sociodemographic variables: age, gender, race/ethnicity, and individual and household income.
Adiposity (weight, height, and waist circumference). For the calculation of BMI, measured weight and height. Also, waist circumference needs to be measured considering its stronger CVD prediction than BMI [157–159] and a possible overestimation of adiposity by BMI [160–162] in African Americans. Obesity will be defined with the current standard cut-points for BMI (>30 kg/m2) and WC (>40 in. for men and >35 in. for women) [163]
Conclusions
Acknowledgements
Abbreviation
BMI
CVD
FMCSA
FORWARD
LACMTA
REV-ERBα (known as NR1D1)
SMART
TAV
US
- 1. Gillespie RM, Wang X, Brown T. Developing best-practice guidelines for improving bus operator health and retention. 2016.
- 2. http://www.bls.gov/ooh/transportation-and-material-moving/bus-drivers.htm.
- 3. https://www.cdc.gov/niosh/nora/comment/agendas/transwareutil/pdfs/TransWareUtilAug2009.pdf.
- 4. Carban-Martinez AJ, Lee DJ, Fleming LE, Gomez O, LeBlanc W, Pitman T. Obesity in US workers: the national health interview survey, 1986 to 2002. Am J Public Health 2005;95(9):1–9.
- 5. French SA, Harnack LJ, Hannan PJ, Mitchell NR, Gerlach AF, Toomey TL. Worksite environment intervention to prevent obesity among metropolitan transit workers. Prev Med 2010;50(4):180–5. 10.1016/j.ypmed.2010.01.002. 20079369.ArticlePubMedPMC
- 6. Harvey SB, Glozier N, Carlton O, Mykletun A, Henderson M, Hotopf M, Holland-Elliott K. Obesity and sickness absence: results from the CHAP study. Occup Med 2010;60(5):362–8. 10.1093/occmed/kqq031.Article
- 7. Thiese MS, Moffitt G, Hanowski RJ, Kales SN, Porter RJ, Hegmann KT. Commercial driver medical examinations: prevalence of obesity, comorbidities, and certification outcomes. J Occup Environ Med 2015;57(6):659–65. 10.1097/JOM.0000000000000422. 25710607.PubMedPMC
- 8. Rosengren A, Anderson K, Wilhelmsen L. Risk of coronary heart disease in middle-aged male bus and tram drivers compared to men in other occupations: a prospective study. Int J Epidemiol 1991;20(1):82–7. 10.1093/ije/20.1.82. 2066248.ArticlePubMed
- 9. Gu JK, Charles LE, Bang KM, Ma CC, Andrew ME, Violanti JM, Burchfiel CM. Prevalence of obesity by occupation among US workers: the National Health Interview Survey 2004-2011. J Occup Environ Med 2014;56(5):516–28. 10.1097/JOM.0000000000000133. 24682108.PubMedPMC
- 10. Benavides FG, Benach J, Mira M, Sáez M, Barceló A. Occupational categories and sickness absence certified as attributable to common diseases. Eur J Public Health 2003;13(1):51–5. 10.1093/eurpub/13.1.51. 12678314.Article
- 11. Bigert C, Gustavsson P, Hallqvist J, Hogstedt C, Lewné M, Plato N, Reuterwall C, Schéele P. Myocardial infarction among professional drivers. Epidemiology 2003;14(3):333–9. 12859035.ArticlePubMed
- 12. Tse JLM, Flin R, Mearns K. Bus driver well-being review: 50 years of research. Transp Res F 2006;9(2):89–114. 10.1016/j.trf.2005.10.002.Article
- 13. Tüchsen F, Bach E, Marmot M. Occupation and hospitalization with ischaemic heart diseases: a new nationwide surveillance system based on hospital admissions. Int J Epidemiol 1992;21(3):450–9. 10.1093/ije/21.3.450. 1634305.ArticlePubMed
- 14. Winkleby MA, Ragland DR, Syme SL. Self-reported stressors and hypertension: evidence of an inverse association. Am J Epidemiol 1988;127(1):124–34. 10.1093/oxfordjournals.aje.a114772. 3276154.ArticlePubMed
- 15. http://www.gallup.com/poll/161324/physicians-lead-wellbeing-transportation-workers-lag.aspx.
- 16. Krause N, Ragland DR, Greiner BA, Fisher JM, Holman BL, Selvin S. Physical workload and ergonomic factors associated with prevalence of back and neck pain in urban transit operators. Spine 1997;22(18):2117–26. 10.1097/00007632-199709150-00010. 9322324.ArticlePubMed
- 17. Krause N, Rugulies R, Ragland DR, Syme SL. Physical workload, ergonomic problems, and incidence of low back injury: a 7.5-year prospective study of San Francisco transit operators. Am J Ind Med 2004;46(6):570–85. 10.1002/ajim.20094. 15551390.ArticlePubMed
- 18. Bushnell PT, Li J, Landen D. Group medical claims as a source of information on worker health and potentially work-related diseases. J Occup Environ Med 2011;53(12):1430–41. 10.1097/JOM.0b013e3182363bbe. 22076036.ArticlePubMed
- 19. Wei C. Incidence of and risk factors for occupational injury among transit bus operators. 2014.
- 20. Ebrahimi MH, Delvarianzadeh M, Saadat S. Prevalence of metabolic syndrome among Iranian occupational drivers. Diabetes Metab Syndr 2016;10(1 Suppl 1):S46–51. 10.1016/j.dsx.2015.09.011. 26508099.ArticlePubMed
- 21. Shin SY, Lee CG, Song HS, Kim SH, Lee HS, Jung MS, Yoo SK. Cardiovascular disease risk of bus drivers in a city of Korea. Ann Occup Environ Med 2013;25(1):34. 10.1186/2052-4374-25-34. 24472511.ArticlePubMedPMC
- 22. Escoto KH, French SA, Harnack LJ, Toomey TL, Hannan PJ, Mitchell NR. Work hours, weight status, and weight-related behaviors: a study of metro transit workers. Int J Behav Nutr Phys Act 2010;20;7:91. 10.1186/1479-5868-7-91.ArticlePubMedPMC
- 23. Hedberg GE, Wikström-Frisén L, Janlert U. Comparison between two programmes for reducing the levels of risk indicators of heart diseases among male professional drivers. Occup Environ Med 1998;55(8):554–61. 10.1136/oem.55.8.554. 9849543.ArticlePubMedPMC
- 24. Ragland DR, Krause N, Greiner BA, Fisher JM. Studies of health outcomes in transit operators: policy implications of the current scientific database. J Occup Health Psychol 1998;3(2):172–87. 10.1037/1076-8998.3.2.172. 9585916.ArticlePubMed
- 25. Pandalai SP, Schulte PA, Miller DB. Conceptual heuristic models of the interrelationships between obesity and the occupational environment. Scand J Work Environ Health 2013;39(3):221–32. 10.5271/sjweh.3363. 23588858.ArticlePubMed
- 26. Choi B, Schnall P, Dobson M, Israel L, Landsbergis P, Galassetti P, Pontello A, Kojaku S, Baker D. Exploring occupational and behavioral risk factors for obesity in firefighters: a theoretical framework and study design. Saf Health Work 2011;2(4):301–12. 10.5491/SHAW.2011.2.4.301. 22953214.ArticlePubMedPMC
- 27. Anderson R. The back pain of bus drivers. Prevalence in an urban area of California. Spine 1992;17(12):1481–8. 10.1097/00007632-199212000-00007. 1471006.ArticlePubMed
- 28. Edberg M. Essentials of health behavior: social and behavioral theory in public health. 2007, Jones & Bartlett Learning, LLC: Sudbury.
- 29. Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med 2006;62(7):1650–71. 10.1016/j.socscimed.2005.08.044. 16198467.ArticlePubMed
- 30. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q 1988;15(4):351–77. 10.1177/109019818801500401. 3068205.ArticlePubMedPDF
- 31. Schneider M, Stokols D. In: Shumaker SA, Ockene JK, Riekert KA, editors. Multilevel theories of behavior change: a social ecological framework. The handbook of health behavior change. 2009, 3. New York: Springer Publishing Company; 85–105.
- 32.
- 33. Ng MK, Yousuf B, Bigelow PL, Van Eerd D. Effectiveness of health promotion programmes for truck drivers: a systematic review. Health Educ J 2015;74(3):270–86. 10.1177/0017896914533953.ArticlePDF
- 34. Apostolopoulos Y, Sönmez S, Shattell M, Haldeman L, Strack R, Jones V. Barriers to truck drivers’ healthy eating: environmental influences and health promotion strategies. J Workp Behav Health 2011;26(2):122–43. 10.1080/15555240.2011.573754.Article
- 35. Anderson LM, Quinn TA, Glanz K, Ramirez G, Kahwati LC, Johnson DB, Buchanan LR, Archer WR, Chattopadhyay S, Kalra GP, Katz DL; Task Force on Community Preventive Services. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: a systematic review. Am J Prev Med 2009;37(4):340–57. 10.1016/j.amepre.2009.07.003. 19765507.PubMed
- 36. Verweij LM, Coffeng J, van Mechelen W, Proper KI. Meta-analyses of workplace physical activity and dietary behaviour interventions on weight outcomes. Obes Rev 2011;12(6):406–29. 10.1111/j.1467-789X.2010.00765.x. 20546142.ArticlePubMed
- 37. Feltner C, Peterson K, Weber RP, Cluff L, Coker-Schwimmer E, Viswanathan M, Lohr KN. The effectiveness of Total Worker Health interventions: a systematic review for a National Institutes of Health pathways to prevention workshop. Ann Intern Med 2016;165(4):262–9. 10.7326/M16-0626. 27240022.ArticlePubMed
- 38. Wong JY, Gilson ND, Bush RA, Brown WJ. Patterns and perceptions of physical activity and sedentary time in male transport drivers working in regional Australia. Aust N Z J Public Health 2014;38(4):314–20. 10.1111/1753-6405.12214. 24962634.ArticlePubMedPDF
- 39. van Drongelen A, Boot CR, Merkus SL, Smid T, van der Beek AJ. The effects of shift work on body weight change - a systematic review of longitudinal studies. Scand J Work Environ Health 2011;37(4):263–75. 10.5271/sjweh.3143. 21243319.ArticlePubMed
- 40. Solovieva S, Lallukka T, Virtanen M, Viikari-Juntura E. Psychosocial factors at work, long work hours, and obesity: a systematic review. Scand J Work Environ Health 2013;39(3):241–58. 10.5271/sjweh.3364. 23592217.ArticlePubMed
- 41. Morikawa Y, Nakagawa H, Miura K, Soyama Y, Ishizaki M, Kido T, Naruse Y, Suwazono Y, Nogawa K. Effect of shift work on body mass index and metabolic parameters. Scand J Work Environ Health 2007;33:45–50. 10.5271/sjweh.1063. 17353964.ArticlePubMed
- 42. Suwazono Y, Dochi M, Sakata K, Okubo Y, Oishi M, Tanaka K, Kobayashi E, Kido T, Nogawa K. A longitudinal study on the effect of shift work on weight gain in male Japanese workers. Obesity 2008;16(8):1887–93. 10.1038/oby.2008.298. 18535539.ArticlePubMedPDF
- 43. van Amelsvoort LG, Schouten EG, Kok FJ. Duration of shiftwork related to body mass index and waist to hip ratio. Int J Obes Relat Metab Disord 1999;23:973–8. 10.1038/sj.ijo.0801028. 10490804.ArticlePubMedPDF
- 44. Au N, Hauck K, Hollingsworth B. Employment, work hours and weight gain among middle-aged women. Int J Obes 2013;37(5):718–24. 10.1038/ijo.2012.92.ArticlePDF
- 45. Mercan MA. A research note on the relationship between long working hours and weight gain for older workers in the United States. Res Aging 2014;36(5):557–67. 10.1177/0164027513510324. 25651510.ArticlePubMedPDF
- 46. Nakamura K, Shimai S, Kikuchi S, Takahashi H, Tanaka M, Nakano S, et al. Increases in body mass index and waist circumference as outcomes of working overtime. Occup Med 1998;48:169–73. 10.1093/occmed/48.3.169.Article
- 47. Shields M. Long working hours and health. Health Rep 1999;11:33–48. 10618741.PubMed
- 48. Eriksen D, Rosthøj S, Burr H, Holtermann A. Sedentary work--associations between five-year changes in occupational sitting time and body mass index. Prev Med 2015;73:1–5. 10.1016/j.ypmed.2014.12.038. 25575798.ArticlePubMed
- 49. Lin TC, Courtney TK, Lombardi DA, Verma SK. Association between sedentary work and BMI in a U.S. national longitudinal survey. Am J Prev Med 2015;49(6):e117–23. 10.1016/j.amepre.2015.07.024. 26437869.ArticlePubMed
- 50. Picavet HS, Pas LW, van Oostrom SH, van der Ploeg HP, Verschuren WM, Proper KI. The relation between occupational sitting and mental, cardiometabolic, and musculoskeletal health over a period of 15 years--the Doetinchem cohort study. PLoS One 2016;11(1):e0146639. 10.1371/journal.pone.0146639. 26752695.ArticlePubMedPMC
- 51. Pinto Pereira SM, Power C. Sedentary behaviours in mid-adulthood and subsequent body mass index. PLoS One 2013;8(6):e65791. 10.1371/journal.pone.0065791. 23762427.ArticlePubMedPMC
- 52. Pulsford RM, Stamatakis E, Britton AR, Brunner EJ, Hillsdon MM. Sitting behavior and obesity: evidence from the Whitehall II study. Am J Prev Med 2013;44(2):132–38. 10.1016/j.amepre.2012.10.009. 23332328.PubMedPMC
- 53.
- 54. Block JP, He Y, Zaslavsky AM, Ding L, Ayanian JZ. Psychosocial stress and change in weight among US adults. Am J Epidemiol 2009;170:181–92. 10.1093/aje/kwp104. 19465744.ArticlePubMedPMC
- 55. Ishizaki M, Nakagawa H, Morikawa Y, Honda R, Yamada Y, Kawakami N; Japan Work Stress and Health Cohort Study Group. Influence of job strain on changes in body mass index and waist circumference-6-year longitudinal study. Scand J Work Environ Health 2008;34:288–96. 10.5271/sjweh.1267. 18815715.ArticlePubMed
- 56. Gram Quist H, Christensen U, Christensen KB, Aust B, Borg V, Bjorner JB. Psychosocial work environment factors and weight change: a prospective study among Danish health care workers. BMC Public Health 2013;13:43. 10.1186/1471-2458-13-43. 23327287.PubMedPMC
- 57. Choi B, Dobson M, Landsbergis P, Ko SB, Yang H, Schnall P, Baker D. Job strain and obesity. J Intern Med 2014;275(4):438–40. 10.1111/joim.12173. 24330086.ArticlePubMedPDF
- 58. Fujishiro K, Lawson CC, Hibert EL, Chavarro JE, Rich-Edwards JW. Job strain and changes in the body mass index among working women: a prospective study. Int J Obes 2015;39(9):1395–400. 10.1038/ijo.2015.91.ArticlePDF
- 59. Nyberg ST, Heikkilä K, Fransson EI, Alfredsson L, De Bacquer D, Bjorner JB, Bonenfant S, Borritz M, Burr H, Casini A, Clays E, Dragano N, Erbel R, Geuskens GA, Goldberg M, Hooftman WE, Houtman IL, Jöckel KH, Kittel F, Knutsson A, Koskenvuo M, Leineweber C, Lunau T, Madsen IE, Hanson LL, Marmot MG, Nielsen ML, Nordin M, Oksanen T, Pentti J, Rugulies R, Siegrist J, Suominen S, Vahtera J, Virtanen M, Westerholm P, Westerlund H, Zins M, Ferrie JE, Theorell T, Steptoe A, Hamer M, Singh-Manoux A, Batty GD, Kivimäki M; IPD-Work Consortium. Job strain in relation to body mass index: pooled analysis of 160 000 adults from 13 cohort studies. J Intern Med 2012;272(1):65–73. 10.1111/j.1365-2796.2011.02482.x. 22077620.ArticlePubMedPDF
- 60. Brunner EJ, Chandola T, Marmot MG. Prospective effect of job strain on general and central obesity in the Whitehall II Study. Am J Epidemiol 2007;165:828–37. 10.1093/aje/kwk058. 17244635.ArticlePubMed
- 61. Gardell B, Aronsson G, Barklöf K. The working environment for local public transport personnel. 1982.
- 62. http://www.isye.umn.edu/labs/scorlab/pdf/GLW11.pdf.
- 63. Duffy CA, McGoldrick AE. Stress and the bus driver in the UK transport industry. Work Stress 1990;4(1):17–27. 10.1080/02678379008256961.Article
- 64. Wetzel T. Opposition Movement in Los Angeles Transit Union. 2006.
- 65. Belkić K, Savić C, Theorell T, Rakić L, Ercegovac D, Djordjević M. Mechanisms of cardiac risk among professional drivers. Scand J Work Environ Health 1994;20(2):73–86. 10.5271/sjweh.1417. 8079138.ArticlePubMed
- 66. Karasek RA. Job demands, job decision latitude, and mental strain: implications for job redesign. Admin Sci Quart 1979;24:285–308. 10.2307/2392498.Article
- 67. Meijman TF, Kompier MA. Bussy business: how urban bus drivers cope with time pressure, passengers, and traffic safety. J Occup Health Psychol 1998;3(2):109–21. 10.1037/1076-8998.3.2.109. 9585911.ArticlePubMed
- 68. Biggs H, Dingsdag D, Stenson N. Fatigue factors affecting metropolitan bus drivers: A qualitative investigation. Work 2009;32(1):5–10. 19276520.ArticlePubMed
- 69. Hege A, Apostolopoulos Y, Perko M, Sönmez S, Strack R. The work organization of long-haul truck drivers and the association with body mass index. J Occup Environ Med 2016;58(7):712–7. 10.1097/JOM.0000000000000734. 27206124.ArticlePubMed
- 70. Rosso GL, Perotto M, Feola M, Bruno G, Caramella M. Investigating obesity among professional drivers: the high risk professional driver study. Am J Ind Med 2015;58(2):212–9. 10.1002/ajim.22400. 25603943.ArticlePubMedPDF
- 71. Gimeno D, Benavides FG, Mira M, Martinez JM, Benach J. External validation of psychological job demands in a bus driver sample. J Occup Health 2004;46(1):43–8. 10.1539/joh.46.43. 14960829.ArticlePubMedPDF
- 72. Greiner BA, Krause N, Ragland DR, Fisher JM. Objective stress factors, accidents, and absenteeism in transit operators: a theoretical framework and empirical evidence. J Occup Health Psychol 1998;3(2):130–46. 10.1037/1076-8998.3.2.130. 9585913.ArticlePubMed
- 73. Varela-Mato V, Yates T, Stensel DJ, Biddle SJ, Clemes SA. Time spent sitting during and outside working hours in bus drivers: a pilot study. Prev Med Rep 2015;3:36–9. 10.1016/j.pmedr.2015.11.011. 26844184.ArticlePubMedPMC
- 74. http://publictransport.about.com/od/Transit_Employment/a/Transit-101-Extra-Board-Operators.htm.
- 75. Björntorp P. The regulation of adipose tissue distribution in humans. Int J Obes Relat Metab Disord 1996;20:291–302. 8680455.PubMed
- 76. Rosmond R, Björntorp P. Psychosocial and socio-economic factors in women and their relationship to obesity and regional body fat distribution. Int J Obes Relat Metab Disord 1999;23:138–45. 10.1038/sj.ijo.0800782. 10078847.ArticlePubMedPDF
- 77. Björntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev 2001;2:73–86. 10.1046/j.1467-789x.2001.00027.x. 12119665.ArticlePubMed
- 78. Burke HM, Davis MC, Otte C, Mohr DC. Depression and cortisol responses to psychological stress: a meta-analysis. Psychoneuroendocrinology 2005;30(9):846–56. 10.1016/j.psyneuen.2005.02.010. 15961250.ArticlePubMed
- 79. Dodt C, Lönnroth P, Wellhöner JP, Fehm HL, Elam M. Sympathetic control of white adipose tissue in lean and obese humans. Acta Physiol Scand 2003;177:351–7. 10.1046/j.1365-201X.2003.01077.x. 12609006.ArticlePubMedPDF
- 80. Kapit W, Macey RI, Meisami E. The physiology coloring book. 1999, 2. Benjamin Cummings: San Francisco.
- 81. Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Med Rev 2007;11:163–78. 10.1016/j.smrv.2007.01.002. 17442599.ArticlePubMedPMC
- 82. Plotsky PM, Cunningham ET Jr, Widmaier EP. Catecholaminergic modulation of corticotropin-releasing factor and adrenocorticotropin secretion. Endocr Rev 1989;10:437–58. 10.1210/edrv-10-4-437. 2558876.ArticlePubMed
- 83. Pratt LA, Brody DJ. Depression and obesity in the US adult household population, 2005–2010. Women 2014;20:39.
- 84. Pasquali R, Vicennati V, Gambineri A, Pagotto U. Sex-dependent role of glucocorticoids and androgens in the pathophysiology of human obesity. Int J Obes 2008;32(12):1764–79. 10.1038/ijo.2008.129.ArticlePDF
- 85. Bose M, Oliván B, Laferrère B. Stress and obesity: the role of the hypothalamic-pituitary-adrenal axis in metabolic disease. Curr Opin Endocrinol Diabetes Obes 2009;16(5):340–6. 10.1097/MED.0b013e32832fa137. 19584720.ArticlePubMedPMC
- 86. Vicennati V, Pasqui F, Cavazza C, Pagotto U, Pasquali R. Stress-related development of obesity and cortisol in women. Obesity 2009;17(9):1678–83. 10.1038/oby.2009.76. 19300426.ArticlePubMedPDF
- 87. Huang W, Ramsey KM, Marcheva B, Bass J. Circadian rhythms, sleep, and metabolism. J Clin Invest 2011;121(6):2133–41. 10.1172/JCI46043. 21633182.ArticlePubMedPMC
- 88. Campbell JE, Peckett AJ, D’souza AM, Hawke TJ, Riddell MC. Adipogenic and lipolytic effects of chronic glucocorticoid exposure. Am J Physiol Cell Physiol 2011;300(1):C198–209. 10.1152/ajpcell.00045.2010. 20943959.ArticlePubMed
- 89. Froy O. Metabolism and circadian rhythms--implications for obesity. Endocr Rev 2010;31(1):1–24. 10.1210/er.2009-0014. 19854863.PubMed
- 90. Bakopanos E, Silva JE. Opposing effects of glucocorticoids on beta(3)-adrenergic receptor expression in HIB-1B brown adipocytes. Mol Cell Endocrinol 2002;190(1-2):29–37. 10.1016/S0303-7207(02)00027-8. 11997176.PubMed
- 91. Collins S, Surwit RS. The beta-adrenergic receptors and the control of adipose tissue metabolism and thermogenesis. Recent Prog Horm Res 2001;56:309–28. 10.1210/rp.56.1.309. 11237219.PubMed
- 92. Cypess AM, Weiner LS, Roberts-Toler C, Franquet Elía E, Kessler SH, Kahn PA, English J, Chatman K, Trauger SA, Doria A, Kolodny GM. Activation of human brown adipose tissue by a β3-adrenergic receptor agonist. Cell Metab 2015;21(1):33–8. 10.1016/j.cmet.2014.12.009. 25565203.ArticlePubMedPMC
- 93. Himms-Hagen J. Brown adipose tissue thermogenesis and obesity. Prog Lipid Res 1989;28(2):67–115. 10.1016/0163-7827(89)90009-X. 2692032.ArticlePubMed
- 94. Lowell BB, Flier JS. Brown adipose tissue, beta 3-adrenergic receptors, and obesity. Annu Rev Med 1997;48:307–16. 10.1146/annurev.med.48.1.307. 9046964.ArticlePubMed
- 95. Louis SN, Jackman GP, Nero TL, Iakovidis D, Louis WJ. Role of beta-adrenergic receptor subtypes in lipolysis. Cardiovasc Drugs Ther 2000;14(6):565–77. 10.1023/A:1007838125152. 11300357.ArticlePubMedPDF
- 96. Sharma AM, Pischon T, Hardt S, Kunz I, Luft FC. Hypothesis: beta-adrenergic receptor blockers and weight gain: a systematic analysis. Hypertension 2001;37(2):250–4. 10.1161/01.HYP.37.2.250. 11230280.ArticlePubMed
- 97. Fenzl A, Kiefer FW. Brown adipose tissue and thermogenesis. Horm Mol Biol Clin Investig 2014;19(1):25–37. 25390014.ArticlePubMed
- 98. Delezie J, Challet E. Interactions between metabolism and circadian clocks: reciprocal disturbances. Ann N Y Acad Sci 2011;1243:30–46. 10.1111/j.1749-6632.2011.06246.x. 22211891.ArticlePubMed
- 99. Langendonk JG, Pijl H, Toornvliet AC, Burggraaf J, Frölich M, Schoemaker RC, Doornbos J, Cohen AF, Meinders AE. Circadian rhythm of plasma leptin levels in upper and lower body obese women: influence of body fat distribution and weight loss. J Clin Endocrinol Metab 1998;83(5):1706–12. 10.1210/jcem.83.5.4717. 9589680.ArticlePubMed
- 100. Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on physiological rhythms. Rev Neurol (Paris) 2003;159(11 Suppl)):6S11–20. 14646794.PubMed
- 101. Arble DM, Bass J, Laposky AD, Vitaterna MH, Turek FW. Circadian timing of food intake contributes to weight gain. Obesity (Silver Spring) 2009;17(11):2100–2. 10.1038/oby.2009.264. 19730426.ArticlePubMedPMCPDF
- 102. Delezie J, Dumont S, Dardente H, Oudart H, Gréchez-Cassiau A, Klosen P, Teboul M, Delaunay F, Pévet P, Challet E. The nuclear receptor REV-ERBα is required for the daily balance of carbohydrate and lipid metabolism. FASEB J 2012;26(8):3321–35. 10.1096/fj.12-208751. 22562834.ArticlePubMedPDF
- 103. Mauck HP Jr, Hoff EC. Experimental neurogenic arrhythmias. Bull N Y Acad Med 1967;43(12):1097–105. 5235595.PubMedPMC
- 104. Simonson E, Baker C, Burns N, Keiper C, Schmitt OH, Stackhouse S. Cardiovascular stress (electrocardiographic changes) produced by driving an automobile. Am Heart J 1968;75(1):125–35. 10.1016/0002-8703(68)90123-3. 5635042.ArticlePubMed
- 105. Pop C, Manea V, Matei C, Trambitasu R, Mos L. Work stress hypertension and obesity among professional bus drivers: results of a cross-sectional study conducted in an urban Romanian company of transport. J Hypertens Res 2015;1:27–32.
- 106.
- 107. Choi B, Schnall P, Yang H, Dobson M, Landsbergis P, Israel L, Karasek R, Baker D. Psychosocial working conditions and active leisure-time physical activity in middle-aged US workers. Int J Occup Med Environ Health 2010;23(3):239–53. 10.2478/v10001-010-0029-0. 20934957.ArticlePubMed
- 108. Nishitani N, Sakakibara H, Akiyama I. Eating behavior related to obesity and job stress in male Japanese workers. Nutrition 2009;25:45–50. 10.1016/j.nut.2008.07.008. 18834723.ArticlePubMed
- 109. Atkinson G, Fullick S, Grindey C, Maclaren D. Exercise, energy balance and the shift worker. Sports Med 2008;38:671–85. 10.2165/00007256-200838080-00005. 18620467.ArticlePubMedPMC
- 110. Devine CM, Farrell TJ, Blake CE, Jastran M, Wethington E, Bisogni CA. Work conditions and the food choice coping strategies of employed parents. J Nutr Educ Behav 2009;41:365–70. 10.1016/j.jneb.2009.01.007. 19717121.ArticlePubMedPMC
- 111. Morikawa Y, Miura K, Sasaki S, Yoshita K, Yoneyama S, Sakurai M, Ishizaki M, Kido T, Naruse Y, Suwazono Y, Higashiyama M, Nakagawa H. Evaluation of the effects of shift work on nutrient intake: a cross-sectional study. J Occup Health 2008;50:270–8. 10.1539/joh.L7116. 18408349.ArticlePubMedPDF
- 112. Brisson C, Larocque B, Moisan J, Vézina M, Dagenais GR. Psychosocial factors at work, smoking, sedentary behavior, and body mass index: a prevalence study among 6995 white collar workers. J Occup Environ Med 2000;42:40–6. 10.1097/00043764-200001000-00011. 10652687.PubMed
- 113. Kouvonen A, Kivimäki M, Elovainio M, Pentti J, Linna A, Virtanen M, Vahtera J. Effort/reward imbalance and sedentary lifestyle: an observational study in a large occupational cohort. Occup Environ Med 2006;63:422–7. 10.1136/oem.2005.020974. 16497854.ArticlePubMedPMC
- 114. Schneider S, Becker S. Prevalence of physical activity among the working population and correlation with work-related factors: results from the first German National Health Survey. J Occup Health 2005;47:414–23. 10.1539/joh.47.414. 16230835.ArticlePubMedPDF
- 115. Fransson EI, et al. Job strain as a risk factor for leisure-time physical inactivity: an individual-participant meta-analysis of up to 170,000 men and women: the IPD-Work Consortium. Am J Epidemiol 2012;176(12):1078–89. 10.1093/aje/kws336. 23144364.ArticlePubMedPMC
- 116. Choi B, Dobson M, Schnall P, Garcia-Rivas J. 24-h work shifts, sedentary work, and obesity in male firefighters. Am J Ind Med 2016;59(6):486–500. 10.1002/ajim.22572. 26901392.PubMed
- 117. Choi B, Schnall P, Yang H, Dobson M, Landsbergis P, Israel L, Karasek R, Baker D. Sedentary work, low physical job demand, and obesity in US workers. Am J Ind Med 2010;53(11):1088–101. 10.1002/ajim.20886. 20737422.ArticlePubMed
- 118. Church TS, Thomas DM, Tudor-Locke C, Katzmarzyk PT, Earnest CP, Rodarte RQ, Martin CK, Blair SN, Bouchard C. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS One 2011;6(5):e19657. 10.1371/journal.pone.0019657. 21647427.ArticlePubMedPMC
- 119. Szeto GP, Lam P. Work-related musculoskeletal disorders in urban bus drivers of Hong Kong. J Occup Rehabil 2007;17(2):181–98. 10.1007/s10926-007-9070-7. 17273930.ArticlePubMedPDF
- 120. Nobrega S, Champagne N, Abreu M, Goldstein-Gelb M, Montano M, Lopez I, Arevalo J, Bruce S, Punnett L. Obesity/overweight and the role of working conditions: a qualitative, participatory investigation. Health Promot Pract 2016;17(1):127–36. 10.1177/1524839915602439. 26333770.PubMed
- 121. Canivet C, Ostergren PO, Choi B, Nilsson P, Af Sillén U, Moghadassi M, Karasek R, Isacsson SO. Sleeping problems as a risk factor for subsequent musculoskeletal pain and the role of job strain: results from a one-year follow-up of the Malmö Shoulder Neck Study Cohort. Int J Behav Med 2008;15(4):254–62. 10.1080/10705500802365466. 19005925.ArticlePubMed
- 122. Phillips KM, Clark ME, Gironda RJ, McGarity S, Kerns RW, Elnitsky CA, Andresen EM, Collins RC. Pain and psychiatric comorbidities among two groups of Iraq and Afghanistan era Veterans. J Rehabil Res Dev 2016;53(4):413–32. 10.1682/JRRD.2014.05.0126. 27532156.ArticlePubMed
- 123. Sivertsen B, Lallukka T, Petrie KJ, Steingrímsdóttir ÓA, Stubhaug A, Nielsen CS. Sleep and pain sensitivity in adults. Pain 2015;156(8):1433–9. 10.1097/j.pain.0000000000000131. 25915149.ArticlePubMed
- 124. Jahnke SA, Poston WS, Haddock CK, Jitnarin N. Obesity and incident injury among career firefighters in the central United States. Obesity 2013;21(8):1505–08. 10.1002/oby.20436. 23512940.ArticlePubMedPDF
- 125. Poplin GS, Roe DJ, Peate W, Harris RB, Burgess JL. The association of aerobic fitness with injuries in the fire service. Am J Epidemiol 2014;179(2):149–55. 10.1093/aje/kwt213. 24186973.ArticlePubMed
- 126. http://chicagounbound.uchicago.edu/cgi/viewcontent.cgi?article=1052&context=uclf.
- 127. Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med 2014;110:10–7. 10.1016/j.socscimed.2014.03.022. 24704889.ArticlePubMed
- 128. Bowleg L. The problem with the phrase women and minorities: intersectionality-an important theoretical framework for public health. Am J Public Health 2012;102(7):1267–73. 10.2105/AJPH.2012.300750. 22594719.ArticlePubMedPMC
- 129. Aronsson G, Rissler A. Psychophysiological stress reactions in female and male urban bus drivers. J Occup Health Psychol 1998;3(2):122–9. 10.1037/1076-8998.3.2.122. 9585912.ArticlePubMed
- 130. Artazcoz L, Cortès I, Borrell C, Escribà-Agüir V, Cascant L. Gender perspective in the analysis of the relationship between long workhours, health and health-related behavior. Scand J Work Environ Health 2007;33(5):344–50. 10.5271/sjweh.1154. 17973060.ArticlePubMed
- 131. Aguirre-Molina M, Molina CW. Ethnic/racial populations and worksite health promotion. Occup Med 1990;5(4):789. 2237705.PubMed
- 132. Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics 2006;117(2):417–24. 10.1542/peds.2005-0058. 16452361.ArticlePubMedPDF
- 133. Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev 2009;31:7–20. 10.1093/epirev/mxp005. 19589839.ArticlePubMed
- 134. Krieger N, Rowley DL, Herman AA, Avery B, Phillips MT. Racism, sexism, and social class: implications for studies of health, disease, and well-being. Am J Prev Med 1993;9(6 Suppl):82–122. 8123288.ArticlePubMed
- 135. Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans. A biopsychosocial model. Am Psychol 1999;54(10):805–16. 10.1037/0003-066X.54.10.805. 10540593.ArticlePubMed
- 136. Choi B, Schnall P, Yang H, Dobson M, Landsbergis P, Israel L, Karasek R, Baker D. Work stress and overeating coping in the US workforce. Int J Occup Med Environ Health 2009;22(Suppl):43. 19342363.PubMed
- 137. Allan JD. Explanatory models of overweight among African American, Euro-American, and Mexican American women. West J Nurs Res 1998;20(1):45–66. 10.1177/019394599802000104. 9473967.ArticlePubMedPDF
- 138. Fitzgibbon ML, Blackman LR, Avellone ME. The relationship between body image discrepancy and body mass index across ethnic groups. Obes Res 2000;8(8):582–9. 10.1038/oby.2000.75. 11156434.ArticlePubMed
- 139. Cachelin FM, Rebeck RM, Chung GH, Pelayo E. Does ethnicity influence body-size preference? A comparison of body image and body size. Obes Res 2002;10(3):158–66. 10.1038/oby.2002.25. 11886938.ArticlePubMed
- 140. Lopez E, Blix GG, Blix AG. Body image of Latinas compared to body image of non-Latina White women. Health Values 1995;19(6):3–10.
- 141. Airhihenbuwa CO, Kumanyika S, Agurs TD, Lowe A. Perceptions and beliefs about exercise, rest, and health among African-Americans. Am J Health Promot 1995;9(6):426–9. 10.4278/0890-1171-9.6.426. 10150533.ArticlePubMedPDF
- 142. Karasek RA, Gordon G, Pietrokovsky C, Frese M, Pieper C, Schwartz J, et al. Job content questionnaire and user’s guide. 1985, Los Angeles, Lowell: University of Southern California/University of Massachusetts.
- 143. Evans GW. Working on the hot seat: urban bus operators. Accid Anal and Prev 1994;26(2):181–193. 10.1016/0001-4575(94)90088-4.Article
- 144. Belkic K, Savic C. The occupational stress index--An approach derived from cognitive ergonomics applicable to clinical practice. Scand J Work Environ Health 2008;6(Suppl):169–176.
- 145. Shimotsu ST, French SA, Gerlach AF, Hannan PJ. Worksite environment physical activity and healthy food choices: measurement of the worksite food and physical activity environment at four metropolitan bus garages. Int J Behav Nutr Phys Act 2007;4:17. 10.1186/1479-5868-4-17. 17498308.ArticlePubMedPMCPDF
- 146. Cunningham TJ, Berkman LF, Kawachi I, Jacobs DR Jr, Seeman TE, Kiefe CI, Gortmaker SL. Changes in waist circumference and body mass index in the US CARDIA cohort: fixed-effects associations with self-reported experiences of racial/ethnic discrimination. J Biosoc Sci 2013;45(2):267–78. 10.1017/S0021932012000429. 22856616.ArticlePubMed
- 147. Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med 2005;61(7):1576–96. 10.1016/j.socscimed.2005.03.006. 16005789.ArticlePubMed
- 148. Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol 2006;35(4):888–901. 10.1093/ije/dyl056. 16585055.ArticlePubMed
- 149. French SA, Harnack LJ, Toomey TL, Hannan PJ. Association between body weight, physical activity and food choices among metropolitan transit workers. Int J Behav Nutr Phys Act 2007;4:52. 10.1186/1479-5868-4-52. 17980026.ArticlePubMedPMC
- 150.
- 151. Escoto KH, French SA. Unhealthy and healthy weight control behaviours among bus operators. Occup Med 2012;62(2):138–40. 10.1093/occmed/kqr178.ArticlePubMedPMC
- 152. Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sørensen F, Andersson G, Jørgensen K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon 1987;18(3):233–7. 10.1016/0003-6870(87)90010-X. 15676628.ArticlePubMed
- 153. Roos E, Laaksonen M, Rahkonen O, Lahelma E, Lallukka T. Weight change and sickness absence--a prospective study among middle-aged employees. Eur J Public Health 2015;25(2):263–7. 10.1093/eurpub/cku087. 24997201.ArticlePubMed
- 154. Kristensen TS. Sickness absence and work strain among Danish slaughterhouse workers: an analysis of absence from work regarded as coping behaviour. Soc Sci Med 1991;32(1):15–27. 10.1016/0277-9536(91)90122-S. 2008617.ArticlePubMed
- 155. Mujahid MS, Diez Roux AV, Morenoff JD, Raghunathan T. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am J Epidemiol 2007;165(8):858–67. 10.1093/aje/kwm040. 17329713.ArticlePubMed
- 156. Gutek BA, Searle S, Klepa L. Rational versus gender role explanations for work-family conflict. J Appl Psychol 1991;76(4):560–68. 10.1037/0021-9010.76.4.560.Article
- 157. Ford ES, Mokdad AH, Giles WH. Trends in waist circumference among US adults. Obes Res 2003;11:1223–31. 10.1038/oby.2003.168. 14569048.ArticlePubMed
- 158. Lee K, Song YM, Sung J. Which obesity indicators are better predictors of metabolic risk? Healthy twin study. Obesity 2008;16:834–40. 10.1038/oby.2007.109. 18239595.ArticlePubMedPDF
- 159. Vazquez G, Duval S, Jacobs DR Jr, Silventoinen K. Comparison of body mass index, waist circumference, and waist/hip ratio in predicting incident diabetes: A meta-analysis. Epidemiol Rev 2007;29:115–28. 10.1093/epirev/mxm008. 17494056.ArticlePubMed
- 160. Deurenberg P, Yap M, van Staveren WA. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Relat Metab Disord 1998;22:1164–71. 10.1038/sj.ijo.0800741. 9877251.ArticlePubMedPDF
- 161. Jackson AS, Stanforth PR, Gagnon J, Rankinen T, Leon AS, Rao DC, Skinner JS, Bouchard C, Wilmore JH. The effect of sex, age and race on estimating percentage body fat from body mass index: The Heritage Family Study. Int J Obes Relat Metab Disord 2002;26:789–96. 10.1038/sj.ijo.0802006. 12037649.ArticlePubMedPDF
- 162. Prentice AM, Jebb SA. Beyond body mass index. Obes Rev 2001;2:141–7. 10.1046/j.1467-789x.2001.00031.x. 12120099.ArticlePubMed
- 163. World Health Organization (WHO). Obesity: Preventing and managing the global epidemic. 2000, Geneva: WHO.
- 164. Dobson M, Choi B, Schnall PL, Wigger E, Garcia-Rivas J, Israel L, Baker DB. Exploring occupational and health behavioral causes of firefighter obesity: a qualitative study. Am J Ind Med 2013;56(7):776–90. 10.1002/ajim.22151. 23335437.ArticlePubMed
- 165. Choi B, Schnall P, Dobson M. Twenty-four-hour work shifts, increased job demands, and elevated blood pressure in professional firefighters. Int Arch Occup Environ Health 2016;89(7):1111–25. 10.1007/s00420-016-1151-5. 27368424.ArticlePubMedPMCPDF
- 166. Stokols D. Establishing and maintaining healthy environments: toward a social ecology of health promotion. Am Psychol 1992;47(1):6–22. 10.1037/0003-066X.47.1.6. 1539925.ArticlePubMed
- 167. Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot 1996;10(4):282–98. 10.4278/0890-1171-10.4.282. 10159709.ArticlePubMedPDF
- 168. Rydstedt LW, Johansson G, Evans GW. The human side of the road: improving the working conditions of urban bus drivers. J Occup Health Psychol 1998;3(2):161–71. 10.1037/1076-8998.3.2.161. 9585915.ArticlePubMed
- 169. Evans GW, Johansson G, Rydstedt L. Hassles on the job: a study of a job intervention with urban bus drivers. J Organ Behav 1999;20(2):199–208. 10.1002/(SICI)1099-1379(199903)20:2<199::AID-JOB939>3.0.CO;2-I.Article
- 170. Poulsen K, Jensen S, Bach E, Schostak J. Using action research to improve health and the work environment for 3500 municipal bus drivers. Educ Action Res 2007;15(1):75–106. 10.1080/09650790601151228.Article
- 171. Kompier MAJ, Aust B, van den Berg A-M, Siegrist J. Stress prevention in bus drivers: evaluation of 13 natural experiments. J Occup Health Psychol 2000;5(1):11–31. 10.1037/1076-8998.5.1.11. 10658882.ArticlePubMed
- 172. Netterstrøm B. Denmark: self-rule on route 166. Preventing stress, improving productivity: European case studies in the workplace. 1999, London: Routledge; 175–94.
- 173. https://www.cdc.gov/nccdphp/dch/programs/healthycommunitiesprogram/tools/pdf/sdoh-workbook.pdf.
- 174. Han B, Cohen DA, Derose KP, Marsh T, Williamson S, Loy S. Effectiveness of a free exercise program in a neighborhood park. Prev Med Rep 2015;2:255–58. 10.1016/j.pmedr.2015.03.010. 26000236.ArticlePubMedPMC
- 175. Ortega AN, Albert SL, Sharif MZ, Langellier BA, Garcia RE, Glik DC, Brookmeyer R, Chan-Golston AM, Friedlander S, Prelip ML. Proyecto MercadoFRESCO: a multi-level, community-engaged corner store intervention in East Los Angeles and Boyle Heights. J Community Health 2015;40(2):347–56. 10.1007/s10900-014-9941-8. 25209600.ArticlePubMedPMCPDF
REFERENCES
Figure & Data
REFERENCES
Citations

- Facilitators and barriers to achieving dietary and physical activity goals: focus group interviews with city bus drivers and counseling dietitians
Yongmin Jo, Suhyeun Cho, Young-Hee Han, Taisun Hyun
Korean Journal of Community Nutrition.2023; 28(5): 376. CrossRef - Primary Prevention of Weight Gain Among New Bus Operators
Ryan Olson, Sean P. M. Rice, Talya N. Bauer, Brad Wipfli, W. Kent Anger, Todd Bodner, Peter Graven, Leah S. Greenspan
Journal of Occupational & Environmental Medicine.2023; 65(2): 128. CrossRef - Bus Operators’ Body Weight Changes During Their First 2 Years of Work
Ryan Olson, Sean P.M. Rice, Layla R. Mansfield, Brad Wipfli, Todd Bodner, W. Kent Anger, Talya N. Bauer
Journal of Occupational & Environmental Medicine.2021; 63(12): 1093. CrossRef - Burden of tobacco, kola nut and alcohol consumption and its association with periodontal disease, potentially malignant lesions and quality of life among bus drivers, Lagos State, Nigeria
Afolabi Oyapero, Oyejoke Oyapero, Aliru Akinleye
Population Medicine.2020;[Epub] CrossRef - Pilot test of an interactive obesity treatment approach among employed adults in a university medical billing office
Rachel G. Tabak, Jaime R. Strickland, Bridget Kirk, Ryan Colvin, Richard I. Stein, Hank Dart, Graham A. Colditz, Ann Marie Dale, Bradley A. Evanoff
Pilot and Feasibility Studies.2020;[Epub] CrossRef - Obesity and Socioeconomic Disparities
Cecilia M. Jevitt
Journal of Perinatal & Neonatal Nursing.2019; 33(2): 126. CrossRef - Complejidad de la expresión de genes asociados a obesidad en el tejido adiposo humano
Alejandra Rodríguez, Carlos Echandía, Adalberto Sánchez, José María Satizábal, Julio César Montoya, Felipe García Vallejo
Revista Med.2019; 26(1): 14. CrossRef - The Key Role of Work in Population Health Inequities
Paul A. Landsbergis, BongKyoo Choi, Marnie Dobson, Grace Sembajwe, Craig Slatin, Linda Delp, C. Eduardo Siqueira, Peter Schnall, Sherry Baron
American Journal of Public Health.2018; 108(3): 296. CrossRef - Work stress and health problems of professional drivers: a hazardous formula for their safety outcomes
Sergio A. Useche, Boris Cendales, Luis Montoro, Cristina Esteban
PeerJ.2018; 6: e6249. CrossRef - Work organization, health, and obesity in urban transit operators: A qualitative study
Marnie Dobson, BongKyoo Choi, Peter L. Schnall
American Journal of Industrial Medicine.2017; 60(11): 991. CrossRef
 KSOEM
KSOEM

 Cite
Cite

