Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 28; 2016 > Article
- Research Article Effects of shift work on abdominal obesity among 20–39-year-old female nurses: a 5-year retrospective longitudinal study
- Gyeong-Jin Lee, Kunhyung Kim, Se-yeong Kim, Jeong-Ho Kim, Chunhui Suh, Byung-Chul Son, Chae-Kwan Lee, Junghye Choi
-
Annals of Occupational and Environmental Medicine 2016;28:69.
DOI: https://doi.org/10.1186/s40557-016-0148-6
Published online: December 5, 2016
Department of Occupational and Environmental Medicine & Institute of Environmental and Occupational Medicine, Pusan Paik Hospital, Inje University, Busan, Republic of Korea
© The Author(s). 2016
Open AccessThis article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Abstract
-
Background This study aimed to investigate the effects of shift work on abdominal obesity among young and middle-aged female nurses during a 5-year retrospective study.
-
Methods This retrospective study included female nurses (20–39 years old) who worked at a university hospital in Korea and had available health screening results from 2010–2015. Among 2,611 employees, 934 healthy 20–39-year-old female nurses were identified, and data regarding their demographic information (age and date of employment), waist circumferences (WC), and lifestyle factors (alcohol and exercise) were obtained. Abdominal obesity was defined as a WC of ≥80 cm, based on the World Health Organization’s Asia-West Pacific standard in 2000. The mean WC change from baseline was analyzed using the paired t test, and the association between shift work and abdominal obesity was analyzed using the generalized estimating equation.
-
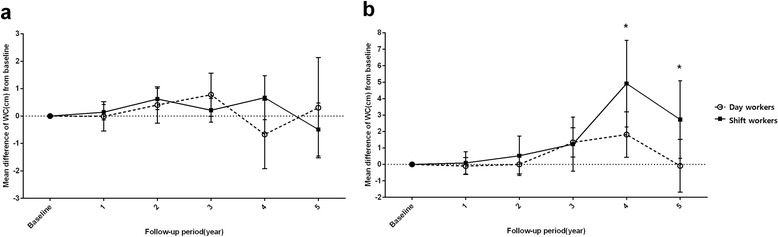
Results Compared to all day workers (both age groups), the 20–29-year-old nurses did not exhibit significant changes in WC at each follow-up. However, among the 30–39-year-old nurses, shift workers exhibited a significant change in WC (vs. baseline) during years 4 and 5, compared to day workers. After adjusting for effective confounders and stratifying the participants according to age, the 20–29-year-old nurses exhibited an odds ratio of 3.21 (95 % confidence interval: 1.29–7.98) for shift work-associated obesity, although the odds ratio for the 30–39-year-old nurses was not statistically significant.
-
Conclusion In the study population, shift work was associated with a significant change in mean WC among 30–39-year-old nurses, and the shift work-associated risk of abdominal obesity was significant among 20–29-year-old nurses. These results indicate that shift work may influence abdominal obesity differently in 20–29-year-old and 30–39-year-old female nurses.
Background
Methods
Results
Discussion
Conclusions
Acknowledgement
Abbreviations
CI
GEE
KNHANES
OR
WC
- 1. Wang XS, Armstrong ME, Cairns BJ, Key TJ, Travis RC. Shift work and chronic disease: the epidemiological evidence. Occup Med (Lond) 2011;61:78–89. 10.1093/occmed/kqr001. 21355031.ArticlePubMedPMC
- 2. Stoner L, Cornwall J. Did the American Medical Association make the correct decision classifying obesity as a disease? Australas Med J 2014;7:462–4. 10.4066/AMJ.2014.2281. 25550718.ArticlePubMedPMC
- 3. van Amelsvoort LG, Schouten EG, Kok FJ. Duration of shiftwork related to body mass index and waist to hip ratio. Int J Obes Relat Metab Disord 1999;23:973–8. 10.1038/sj.ijo.0801028. 10490804.ArticlePubMedPDF
- 4. Pan A, Schernhammer ES, Sun Q, Hu FB. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med 2011;8:e1001141. 10.1371/journal.pmed.1001141. 22162955.ArticlePubMedPMC
- 5. Mohebbi I, Shateri K, Seyedmohammadzad M. The relationship between working schedule patterns and the markers of the metabolic syndrome: comparison of shift workers with day workers. Int J Occup Med Environ Health 2012;25:383–91. 10.2478/s13382-012-0051-5. 23055229.ArticlePubMed
- 6. Lajoie P, Aronson KJ, Day A, Tranmer J. A cross-sectional study of shift work, sleep quality and cardiometabolic risk in female hospital employees. BMJ Open 2015;5:e007327. 10.1136/bmjopen-2014-007327. 25757950.ArticlePubMedPMC
- 7. Proper KI, van de Langenberg D, Rodenburg W, Vermeulen RC, van der Beek AJ, van Steeg H, et al. The relationship between shift work and metabolic risk factors: a systematic review of longitudinal studies. Am J Prev Med 2016;50:e147–57. 10.1016/j.amepre.2015.11.013. 26810355.PubMed
- 8. van Drongelen A, Boot CR, Merkus SL, Smid T, van der Beek AJ. The effects of shift work on body weight change - a systematic review of longitudinal studies. Scand J Work Environ Health 2011;37:263–75. 10.5271/sjweh.3143. 21243319.ArticlePubMed
- 9. Karlsson B, Knutsson A, Lindahl B. Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27,485 people. Occup Environ Med 2001;58:747–52. 10.1136/oem.58.11.747. 11600731.ArticlePubMedPMC
- 10. Porta M. A dictionary of epidemiology. 2014, 6. Oxford: Oxford University Press.
- 11. Niedhammer I, Lert F, Marne MJ. Prevalence of overweight and weight gain in relation to night work in a nurses’ cohort. Int J Obes Relat Metab Disord 1996;20:625–33. 8817356.PubMed
- 12. van Amelsvoort LG, Schouten EG, Kok FJ. Impact of one year of shift work on cardiovascular disease risk factors. J Occup Environ Med 2004;46:699–706. 10.1097/01.jom.0000131794.83723.45. 15247809.ArticlePubMed
- 13. Parkes KR. Shift work and age as interactive predictors of body mass index among offshore workers. Scand J Work Environ Health 2002;28:64–71. 10.5271/sjweh.648. 11871855.ArticlePubMed
- 14.
- 15. Kim MJ, Son KH, Park HY, Choi DJ, Yoon CH, Lee HY, et al. Association between shift work and obesity among female nurses: Korean Nurses’ Survey. BMC Public Health 2013;13:1204. 10.1186/1471-2458-13-1204. 24354395.ArticlePubMedPMCPDF
- 16. Peplonska B, Bukowska A, Sobala W. Association of rotating night shift work with BMI and abdominal obesity among nurses and midwives. PLoS One 2015;10:e0133761. 10.1371/journal.pone.0133761. 26196859.ArticlePubMedPMC
- 17. http://www.wpro.who.int/nutrition/documents/Redefining_obesity/en/.
- 18. https://knhanes.cdc.go.kr/knhanes/index.do.
- 19. Amani R, Gill T. Shiftworking, nutrition and obesity: implications for workforce health- a systematic review. Asia Pac J Clin Nutr 2013;22:505–15. 24231009.ArticlePubMed
- 20. Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 2004;1:e62. 10.1371/journal.pmed.0010062. 15602591.ArticlePubMedPMC
- 21. Morselli LL, Guyon A, Spiegel K. Sleep and metabolic function. Pflugers Arch 2012;463:139–60. 10.1007/s00424-011-1053-z. 22101912.ArticlePubMedPMCPDF
- 22. Lowden A, Moreno C, Holmback U, Lennernas M, Tucker P. Eating and shift work - effects on habits, metabolism and performance. Scand J Work Environ Health 2010;36:150–62. 10.5271/sjweh.2898. 20143038.ArticlePubMed
- 23. Boggild H, Knutsson A. Shift work, risk factors and cardiovascular disease. Scand J Work Environ Health 1999;25:85–99. 10.5271/sjweh.410. 10360463.ArticlePubMed
- 24. Macagnan J, Pattussi MP, Canuto R, Henn RL, Fassa AG, Olinto MT. Impact of nightshift work on overweight and abdominal obesity among workers of a poultry processing plant in southern Brazil. Chronobiol Int 2012;29:336–43. 10.3109/07420528.2011.653851. 22390246.ArticlePubMed
- 25. Antunes Lda C, Jornada MN, Ramalho L, Hidalgo MP. Correlation of shift work and waist circumference, body mass index, chronotype and depressive symptoms. Arq Bras Endocrinol Metabol 2010;54:652–6. 10.1590/S0004-27302010000700010. 21085771.ArticlePubMed
- 26. Reis JP, Loria CM, Lewis CE, Powell-Wiley TM, Wei GS, Carr JJ, et al. Association between duration of overall and abdominal obesity beginning in young adulthood and coronary artery calcification in middle age. JAMA 2013;310:280–8. 10.1001/jama.2013.7833. 23860986.ArticlePubMedPMC
- 27. Manini TM. Energy expenditure and aging. Ageing Res Rev 2010;9:1–11. 10.1016/j.arr.2009.08.002. 19698803.ArticlePubMedPMC
- 28.
- 29.
- 30. Howell DC. Statistical methods for psychology. 2012, 8. Wadsworth: Cengage Learning.
REFERENCES
Figure & Data
REFERENCES
Citations

- Rotating shift work time is directly associated with excess body adiposity
Felipe Reis Stavaux Baudson, Luiz Antônio Alves de Menezes-Júnior, Sílvia Nascimento de Freita, Fausto Aloisio Pedrosa Pimenta, George Luiz Lins Machado-Coelho, Fernando Luiz Pereira de Oliveira, Raimundo Marques do Nascimento Neto, Silvana Mara Luz Turbi
Sleep and Breathing.2024; 28(1): 531. CrossRef - Impaired Melatonin Secretion, Oxidative Stress and Metabolic Syndrome in Night Shift Work
Sorina Hohor, Cristina Mandanach, Andreea Maftei, Corina Aurelia Zugravu, Marina Ruxandra Oțelea
Antioxidants.2023; 12(4): 959. CrossRef - Prevalence of overweight and obesity among health professionals with shift work schedules: A scoping review
Maria Gabriela Tavares Amaro, Ricardo Abdala Conde de Almeida, Bruno Marques Donalonso, Alessandra Mazzo, Carlos Antonio Negrato
Chronobiology International.2023; 40(3): 343. CrossRef - Investigation of Mental and Physical Health of Nurses Associated with Errors in Clinical Practice
Despoina Pappa, Ioannis Koutelekos, Eleni Evangelou, Evangelos Dousis, Georgia Gerogianni, Evdokia Misouridou, Afroditi Zartaloudi, Nikoletta Margari, Georgia Toulia, Polyxeni Mangoulia, Eftychia Ferentinou, Anna Giga, Chrysoula Dafogianni
Healthcare.2022; 10(9): 1803. CrossRef - A Simulated Shift Work Schedule Does Not Increase DNA Double-Strand Break Repair by NHEJ in the Drosophila Rr3 System
Lydia Bergerson, Caleb Fitzmaurice, Tyler Knudtson, Halle McCormick, Alder M. Yu
Genes.2022; 13(1): 150. CrossRef - Shift Work and Obesity Risk—Are There Sex Differences?
Kevin L. Smith, Alexandria B. Danyluk, Sanah S. Munir, Naima Covassin
Current Diabetes Reports.2022; 22(8): 341. CrossRef - Effect of night shift on development of metabolic syndrome among health care workers
Jyotirmayee Bahinipati, Rajlaxmi Sarangi, Mona Pathak, Srikrushna Mohapatra
Journal of Family Medicine and Primary Care.2022; 11(5): 1710. CrossRef - Association of Shift Work with Normal-Weight Obesity in Community-Dwelling Adults
Chul Woo Ahn, Sungjae Shin, Seunghyun Lee, Hye-Sun Park, Namki Hong, Yumie Rhee
Endocrinology and Metabolism.2022; 37(5): 781. CrossRef - Night Work and Breast Cancer Risk in Nurses: Multifactorial Risk Analysis
Juan Gómez-Salgado, Javier Fagundo-Rivera, Mónica Ortega-Moreno, Regina Allande-Cussó, Diego Ayuso-Murillo, Carlos Ruiz-Frutos
Cancers.2021; 13(6): 1470. CrossRef - Prevalence of non-communicable disease risk factors among nurses and para-health professionals working at primary healthcare level of Bangladesh: a cross-sectional study
Mithila Faruque, Lingkan Barua, Palash Chandra Banik, Sharmin Sultana, Animesh Biswas, Abdul Alim, Pradip Kumar Sen Gupta, Liaquat Ali
BMJ Open.2021; 11(3): e043298. CrossRef - Behavioural characteristics and abdominal obesity among Brazilian shift working women
Heloísa Theodoro, Diego Garcia Bassani, Janaína Cristina da Silva, Karina Giane Mendes, Gabriela Hermann Cibeira, Julia Cigana Schenkel, Maria Teresa Anselmo Olinto
Public Health Nutrition.2021; 24(2): 253. CrossRef - Implications of Lifestyle and Occupational Factors on the Risk of Breast Cancer in Shiftwork Nurses
Javier Fagundo-Rivera, Regina Allande-Cussó, Mónica Ortega-Moreno, Juan Jesús García-Iglesias, Adolfo Romero, Carlos Ruiz-Frutos, Juan Gómez-Salgado
Healthcare.2021; 9(6): 649. CrossRef - Morbidities and medications used by practicing nurses during the climacteric
Maria Cristina Tani Beneventi, Sônia Maria Rolim Rosa Lima
Revista da Associação Médica Brasileira.2021; 67(11): 1706. CrossRef - Time of day difference in postprandial glucose and insulin responses: Systematic review and meta-analysis of acute postprandial studies
Gloria K. W. Leung, Catherine E. Huggins, Robert S. Ware, Maxine P. Bonham
Chronobiology International.2020; 37(3): 311. CrossRef - Job-Related Characteristics and Obesity in Australian Employees: Evidence From a Longitudinal Nationally Representative Sample
Syed Afroz Keramat, Khorshed Alam, Jeff Gow, Stuart J. H. Biddle
American Journal of Health Promotion.2020; 34(7): 729. CrossRef - BMI differences between different genders working fixed day shifts and rotating shifts: a literature review and meta-analysis
Wen-Pei Chang, Hsiu-Ju Jen
Chronobiology International.2020; 37(12): 1754. CrossRef - Association between shift work and obesity among nurses: A systematic review and meta-analysis
Qi Zhang, Sek Ying Chair, Suzanne Hoi Shan Lo, Janita Pak-Chun Chau, Mark Schwade, Xiaosu Zhao
International Journal of Nursing Studies.2020; 112: 103757. CrossRef - Relationship between night shift work, eating habits and BMI among nurses in Lebanon
Zeinab Samhat, Randa Attieh, Yonna Sacre
BMC Nursing.2020;[Epub] CrossRef - Napping on night‐shifts among nursing staff: A mixed‐methods systematic review
Huanhuan Li, Yanping Shao, Zhuangjie Xing, Yuan Li, Shouqi Wang, Meiling Zhang, Jie Ying, Ying Shi, Jiao Sun
Journal of Advanced Nursing.2019; 75(2): 291. CrossRef - The Effect of Special Medical Examination for Night Shift Workers and Follow-Up Management Against Hypertension
Won Seon Choi, Ji-Won Lee, Jae Yong Lee, Kyeong Yeon Kim, Jun-Pyo Myong, Won-Chul Lee
International Journal of Environmental Research and Public Health.2019; 16(5): 719. CrossRef - NOCTURNIN Gene Diurnal Variation in Healthy Volunteers and Expression Levels in Shift Workers
Massimo Bracci, Alfredo Copertaro, Veronica Ciarapica, Mariella Barbaresi, Stefano Esposito, Antonella Albanesi, Matteo Valentino, Caterina Ledda, Venerando Rapisarda, Lory Santarelli
BioMed Research International.2019; 2019: 1. CrossRef - A National Study Links Nurses’ Physical and Mental Health to Medical Errors and Perceived Worksite Wellness
Bernadette Mazurek Melnyk, Liana Orsolini, Alai Tan, Cynthia Arslanian-Engoren, Gail D’Eramo Melkus, Jacqueline Dunbar-Jacob, Virginia Hill Rice, Angelica Millan, Sandra B. Dunbar, Lynne T. Braun, JoEllen Wilbur, Deborah A. Chyun, Kate Gawlik, Lisa M. Lew
Journal of Occupational & Environmental Medicine.2018; 60(2): 126. CrossRef - Meta‐analysis on shift work and risks of specific obesity types
M. Sun, W. Feng, F. Wang, P. Li, Z. Li, M. Li, G. Tse, J. Vlaanderen, R. Vermeulen, L. A. Tse
Obesity Reviews.2018; 19(1): 28. CrossRef - Prevalence and factors associated with abdominal obesity among primary health care professional nurses in Eastern Cape, South Africa
Sizeka Monakali, Daniel Ter Goon, Eunice Seekoe, Eyitayo Omolara Owolabi
South African Family Practice.2018; 60(5): 146. CrossRef
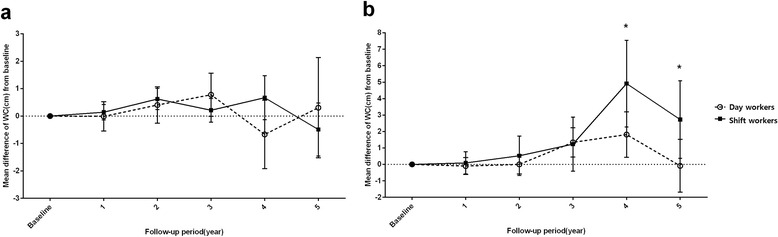
Fig. 1
| Number (%) | |||
|---|---|---|---|
| Total a | Day workers b | Shift workers c | |
| Health screening year | |||
| 2010 | 632 (100.0) | 244 (38.6) | 388 (61.4) |
| 2011 | 667 (100.0) | 245 (36.7) | 422 (63.3) |
| 2012 | 678 (100.0) | 255 (37.6) | 423 (62.4) |
| 2013 | 655 (100.0) | 243 (37.1) | 412 (62.9) |
| 2014 | 669 (100.0) | 225 (33.6) | 444 (66.4) |
| 2015 | 540 (100.0) | 203 (37.6) | 337 (62.4) |
| Follow-up period | |||
| Baseline d | 934 (100.0) | 309 (33.1) | 625 (66.9) |
| 1-year follow-up | 897 (100.0) | 296 (33.0) | 601 (67.0) |
| 2-year follow-up | 716 (100.0) | 270 (37.7) | 446 (62.3) |
| 3-year follow-up | 561 (100.0) | 223 (39.8) | 338 (60.2) |
| 4-year follow-up | 440 (100.0) | 177 (40.2) | 263 (59.8) |
| 5-year follow-up | 333 (100.0) | 140 (42.0) | 193 (58.0) |
| N (%) or mean (SD) | ||||||
|---|---|---|---|---|---|---|
| 20–29 years old | 30–39 years old | |||||
| Total | Day workers | Shift workers | Total | Day workers | Shift workers | |
| 730 (100.0) | 174 (23.8) | 556 (76.2) | 204 (100.0) | 135 (66.2) | 69 (33.8) | |
| Alcohol consumption | ||||||
| Healthy drinking | 702 (96.2) | 170 (97.7) | 532 (95.7) | 199 (97.5) | 130 (96.3) | 69 (100) |
| Unhealthy drinking a | 28 (3.8) | 4 (2.3) | 24 (4.3) | 5 (2.5) | 5 (3.7) | 0 (0) |
| Exercise | ||||||
| Basic b | 239 (32.7) | 59 (33.9) | 180 (32.4) | 83 (40.7) | 53 (39.3) | 30 (43.5) |
| Insufficient c | 73 (10.0) | 18 (10.3) | 55 (9.9) | 38 (18.6) | 27 (20.0) | 11 (15.9) |
| Sufficient d | 418 (57.3) | 97 (55.7) | 321 (57.7) | 83 (40.7) | 55 (40.7) | 28 (40.6) |
| Tenure (years) | 1.3 (2.0) | 1.9 (2.5) | 1.1 (1.8) | 10.4 (4.7) | 10.4 (5.1) | 10.5 (4.0) |
| Waist circumference (cm) | 68.7 (4.2) | 68.4 (4.0) | 68.8 (4.3) | 70.3 (3.9) | 70.1 (3.7) | 70.7 (4.2) |
| Abdominal obesity e | 10(1.4) | 0 (0) | 10 (1.8) | 6 (2.9) | 3 (2.2) | 3 (4.3) |
| 20–29 years old | 30–39 years old | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Work schedule | ||||
| Day work | 1.0 | 1.0 | ||
| Shift work | 3.21* | 1.29–7.98 | 1.46 | 0.78–2.74 |
| Follow-up period (year) | 1.40† | 1.23–1.58 | 1.60† | 1.36–1.87 |
| Exercise | ||||
| Basic | 1.0 | 1.0 | ||
| Insufficient | 0.42* | 0.18–0.98 | 0.33* | 0.14–0.78 |
| Sufficient | 1.04 | 0.64–1.69 | 0.77 | 0.49–1.21 |
a total was defined as all study population (shift workers and day workers)
b day workers were defined as the numbers of nurses who did not include into shift workers
c shift workers were defined as the numbers of nurses who had at least four night shifts per month, or >60 night hours per month during the previous 6 months
d Baseline was defined as the year when each subject was enrolled. Each subject may have different baselines according to her enrollment year
a An average of >5 drinks per week or drinking more than twice per week
b A weekly total exercise score of 4–6 points
c A weekly total exercise score of ≤3 points
d A weekly total exercise score of >7 points
e A waist circumference of ≥80 cm.
* Abbreviations:
*
a Adjusted for work schedule, follow-up period and exercise selected by using backward selection
* Abbreviations:
 KSOEM
KSOEM

 Cite
Cite

