Articles
- Page Path
- HOME > Ann Occup Environ Med > Volume 32; 2020 > Article
- Case Report Severe chemical burns related to dermal exposure to herbicide containing glyphosate and glufosinate with surfactant in Korea
-
Jihyun Shin1
 , Namkyu Lim2
, Namkyu Lim2 , Sangchul Roh1
, Sangchul Roh1
-
Annals of Occupational and Environmental Medicine 2020;32:e28.
DOI: https://doi.org/10.35371/aoem.2020.32.e28
Published online: July 20, 2020
1Department of Occupational and Environmental Medicine, Dankook University Hospital, Cheonan, Korea.
2Department of Plastic and Reconstructive Surgery, Dankook University Hospital, Cheonan, Korea.
- Correspondence: Sangchul Roh. Department of Occupational and Environmental Medicine, Dankook University Hospital, 119 Dandae-ro, Dongnam-gu, Cheonan 31116, Korea. scroh@dku.edu
Copyright © 2020 Korean Society of Occupational & Environmental Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background Glyphosate and glufosinate use widely used as herbicide ingredients. There have been several reported cases of chemical burns caused by dermal exposure to glyphosate-containing herbicide, and patients in these cases were discharged without fatal complications. There were no cases of severe symptoms due to non-oral exposure of glufosinate-containing herbicides. Here, we report a case of fatality accompanied with severe chemical burns in an 81-year-old man who did not wash his skin for more than 48 hours after dermal exposure to herbicide containing glyphosate and glufosinate with surfactant (HGlyGluS).
-
Case presentation An 81-year-old male with no underlying disease was admitted to the emergency department (ED). He had sprayed HGlyGluS with a manual knapsack sprayer 3 days ago and had not wash away the herbicide. On arrival, he was drowsy and had multiple severe corrosive skin lesions. Skin necrosis (10 × 15 cm) on the right shoulder and skin lesions with subcutaneous fat exposure (15 × 20 cm) on the right thigh were observed. Although he was treated including continuous renal replacement therapy, antibiotic apply, debridement operations, and so on, he was unable to recover and expired.
-
Conclusions We suggest that prolonged dermal exposure to HGlyGluS induces fatality. Further studies including prolonged dermal exposure and ingredients of surfactants should be carried out. Also, it is necessary to educate farmers that it is very important to wash immediately after dermal exposure to pesticide.
BACKGROUND
CASE PRESENTATION
Blood test findings conducted at the local hospital at the time of visit
Before the debridement operations, chemical burn wounds on the right side in the left lateral position.

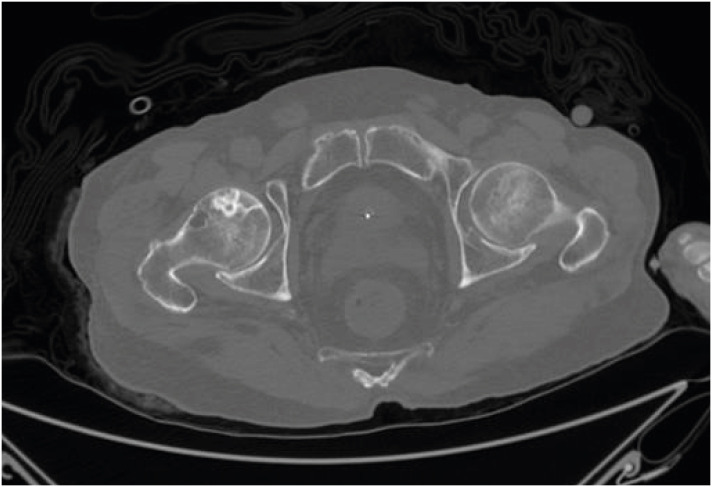
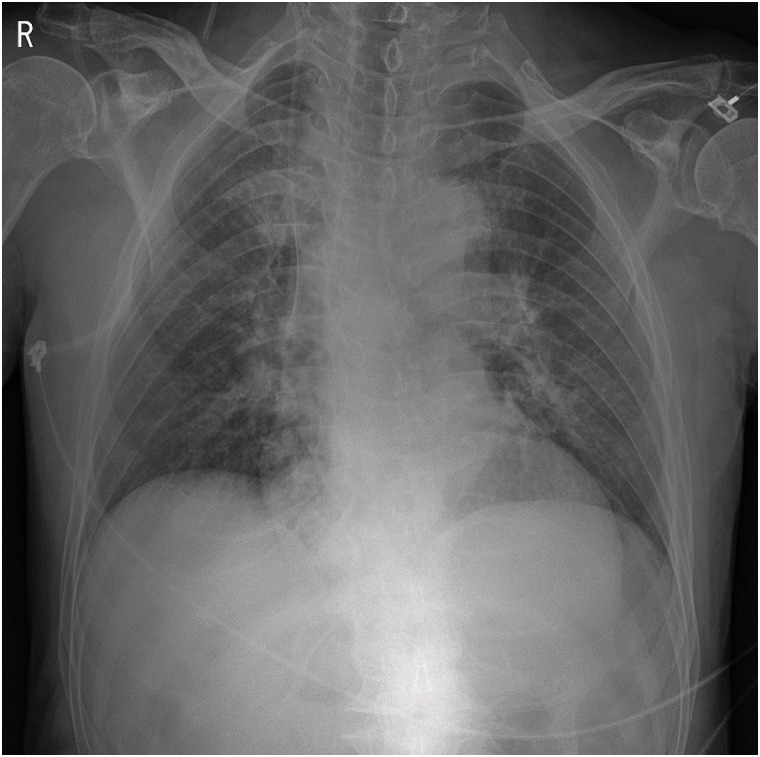
Osteonecrosis of the right femoral head. Abdominal computed tomography axial view (window width: 2501, window level: 250).
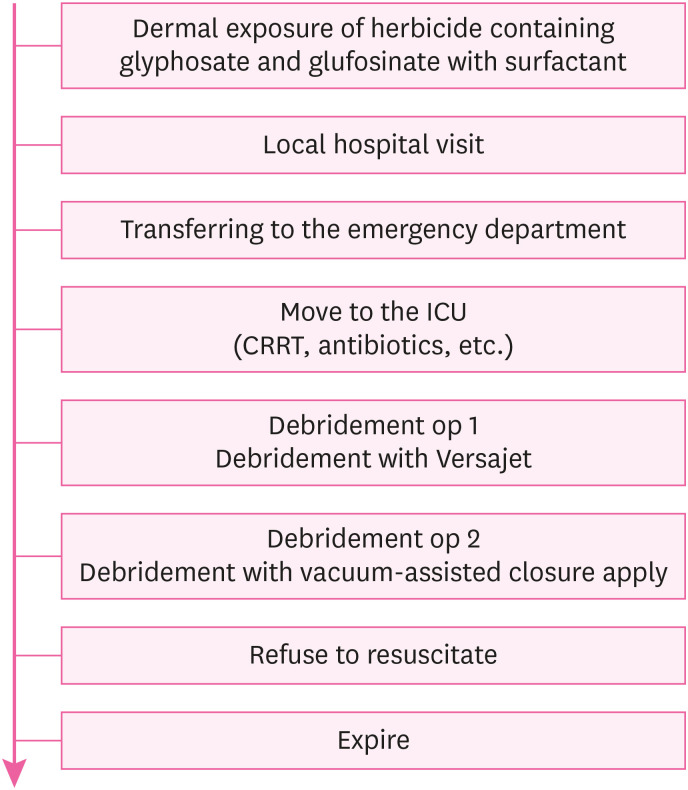
The flow chart from dermal exposure of herbicide to death.
DISCUSSION AND CONCLUSION
-
Competing interests: The authors declare that they have no competing interest.
-
Author Contributions:
Conceptualization: Roh S.
Data curation: Lim N.
Formal analysis: Shin J.
Funding acquisition: Roh S.
Investigation: Roh S.
Methodology: Shin J.
Project administration: Roh S, Lim N.
Resources: Lim N.
Software: Shin J.
Supervision: Roh S, Lim N.
Validation: Roh S, Lim N, Shin J.
Visualization: Lim N, Shin J.
Writing - original draft: Shin J.
Writing - review & editing: Roh S, Lim N.
NOTES
- 1. Bradberry SM, Proudfoot AT, Vale JA. Glyphosate poisoning. Toxicol Rev 2004;23(3):159–167. 15862083.ArticlePubMed
- 2. Ebert E, Leist KH, Mayer D. Summary of safety evaluation toxicity studies of glufosinate ammonium. Food Chem Toxicol 1990;28(5):339–349. 2379893.ArticlePubMed
- 3. Hack R, Ebert E, Ehling G, Leist KH. Glufosinate ammonium--some aspects of its mode of action in mammals. Food Chem Toxicol 1994;32(5):461–470. 8206444.ArticlePubMed
- 4. Amerio P, Motta A, Toto P, Pour SM, Pajand R, Feliciani C, et al. Skin toxicity from glyphosate-surfactant formulation. J Toxicol Clin Toxicol 2004;42(3):317–319. 15362602.ArticlePubMed
- 5. Heras-Mendaza F, Casado-Fariñas I, Paredes-Gascón M, Conde-Salazar L. Erythema multiforme-like eruption due to an irritant contact dermatitis from a glyphosate pesticide. Contact Dermat 2008;59(1):54–56.Article
- 6. Mariager TP, Madsen PV, Ebbehøj NE, Schmidt B, Juhl A. Severe adverse effects related to dermal exposure to a glyphosate-surfactant herbicide. Clin Toxicol (Phila) 2013;51(2):111–113. 23360343.ArticlePubMed
- 7. Mao YC, Hung DZ, Wu ML, Tsai WJ, Wang LM, Ger J, et al. Acute human glufosinate-containing herbicide poisoning. Clin Toxicol (Phila) 2012;50(5):396–402. 22480254.ArticlePubMed
- 8. Inoue Y, Onodera M, Fujita Y, Fujino Y, Kikuchi S, Endo S. Factors associated with severe effects following acute glufosinate poisoning. Clin Toxicol (Phila) 2013;51(9):846–849. 24044532.ArticlePubMed
- 9. National Institute of Agricultural Sciences. Advanced pesticide search. c2020;Accessed 3 Jan 2020]. http://pis.rda.go.kr/registstus/agchmRegistStus/prdlstInqire.do.
- 10. Williams GM, Kroes R, Munro IC. Safety evaluation and risk assessment of the herbicide Roundup and its active ingredient, glyphosate, for humans. Regul Toxicol Pharmacol 2000;31(2 Pt 1):117–165. 10854122.ArticlePubMed
- 11. Song HY, Kim YH, Seok SJ, Gil HW, Yang JO, Lee EY, et al. Cellular toxicity of surfactants used as herbicide additives. J Korean Med Sci 2012;27(1):3–9. 22219606.ArticlePubMedPMCPDF
- 12. Song HY, Kim YH, Seok SJ, Gil HW, Hong SY. In vitro cytotoxic effect of glyphosate mixture containing surfactants. J Korean Med Sci 2012;27(7):711–715. 22787363.ArticlePubMedPMCPDF
- 13. Inoue Y, Onodera M, Fujita Y, Fujino Y, Kikuchi S, Endo S. Factors associated with severe effects following acute glufosinate poisoning. Clin Toxicol (Phila) 2013;51(9):846–849. 24044532.ArticlePubMed
- 14. Mao YC, Hung DZ, Wu ML, Tsai WJ, Wang LM, Ger J, et al. Acute human glufosinate-containing herbicide poisoning. Clin Toxicol (Phila) 2012;50(5):396–402. 22480254.ArticlePubMed
- 15. Weng SF, Hung DZ, Hu SY, Tsan YT, Wang LM. Rhabdomyolysis from an intramuscular injection of glyphosate-surfactant herbicide. Clin Toxicol (Phila) 2008;46(9):890–891. 18787996.ArticlePubMed
- 16. Landis WG, Yu MH. Introduction to environmental toxicology: Impacts of chemicals upon ecological systems. Boca Raton: Lewis Publishers; 1985.
- 17. Heu C, Berquand A, Elie-Caille C, Nicod L. Glyphosate-induced stiffening of HaCaT keratinocytes, a Peak Force Tapping study on living cells. J Struct Biol 2012;178(1):1–7. 22369932.ArticlePubMed
- 18. Lee DH, Choi YH. Severe glyphosate-surfactant intoxication: successful treatment with continuous renal replacement therapy. Hong Kong J Emerg Med 2017;24(1):40–44.ArticlePDF
- 19. Clark A, Neyra JA, Madni T, Imran J, Phelan H, Arnoldo B, et al. Acute kidney injury after burn. Burns 2017;43(5):898–908. 28412129.ArticlePubMed
- 20. Emara SS, Alzaylai AA. Renal failure in burn patients: a review. Ann Burns Fire Disasters 2013;26(1):12–15. 23966893.PubMedPMC
REFERENCES
REFERENCES
Figure & Data
REFERENCES
Citations

- Prospective applications of chitosan and chitosan-based nanoparticles formulations in sustainable agricultural practices
Bhoomika M. Karamchandani, Sunil G. Dalvi, Mahima Bagayatkar, Ibrahim M. Banat, Surekha K. Satpute
Biocatalysis and Agricultural Biotechnology.2024; 58: 103210. CrossRef - Overview of human health effects related to glyphosate exposure
Flavia Silvia Galli, Marta Mollari, Valentina Tassinari, Cristian Alimonti, Alessandro Ubaldi, Camilla Cuva, Daniele Marcoccia
Frontiers in Toxicology.2024;[Epub] CrossRef

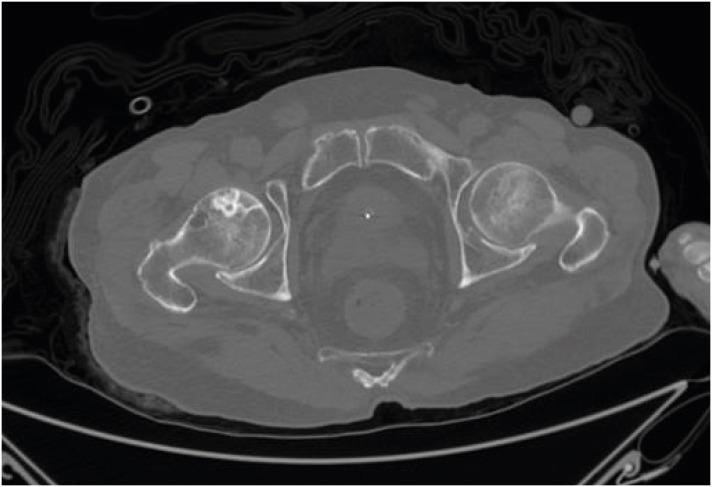
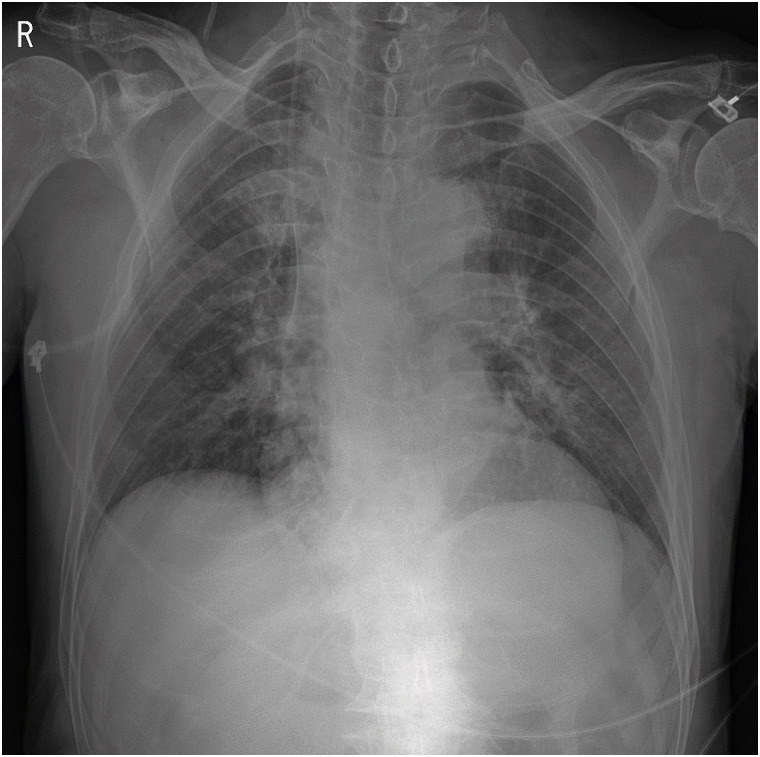
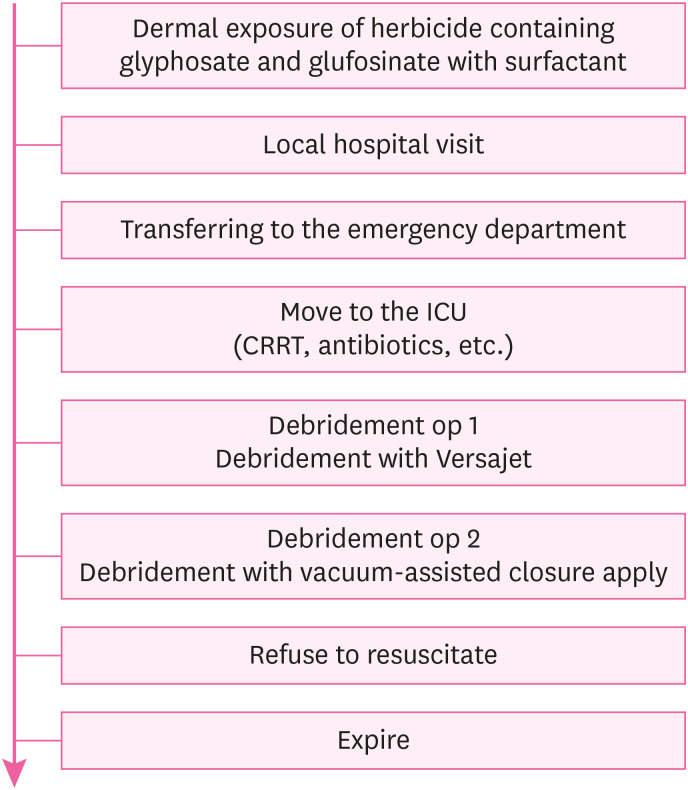
Fig. 1
Fig. 2
Fig. 3
Fig. 4
| Variable | Value | Reference |
|---|---|---|
| AST | 345 U/L | 1–34 U/L |
| ALT | 347 U/L | 10–49 U/L |
| LDH | 3,648 U/L | 208–478 U/L |
| CPK | 16,229 U/L | 32–294 U/L |
| CK-MB | 125 U/L | 0–15 U/L |
| CK-MB/CPK | 0.77% | - |
| Cr | 6.54 mg/dL | 0.7–1.3 mg/dL |
| BUN | 152.2 mg/dL | 9.0–23.0 mg/dL |
| BUN/Cr | 23.27 | - |
| Potassium (K+) | 6.0 mEq/L | 3.5–5.5 mEq/L |
| CRP | 32.96 mg/dL | 0–0.99 mg/dL |
AST: aspartate transaminase; ALT: alanine aminotransferase; LDH: lactate dehydrogenase; CPK: creatinine phosphokinase; CK-MB: creatine kinase MB; Cr: creatinine; BUN: blood urea nitrogen; CRP: C-reactive protein.
 KSOEM
KSOEM

 Cite
Cite

