Association between irregular working hours and work-related musculoskeletal pain: results from the 6th Korean Working Conditions Survey
Article information
Abstract
Background
Recently, irregular working hours have become controversial issues in Korea. The health impact of irregular working hours on the work-related musculoskeletal pain (MSP) is scarcely researched before. We sought to investigate the association between irregular working hours and work-related MSP among South Korean workers.
Methods
This study used data from the sixth Korean Working Conditions Survey in 2020. The prevalence of work-related MSP was analyzed using the χ2 test. A multiple logistic regression analysis was conducted to assess the association between irregular working hours and work-related MSP. We conducted stratified analysis by gender, weekly working hours, and workers’ control over their working hours. We calculated the adjusted odds ratios (ORs) of work-related MSP for irregular working hours combined with weekly working hours.
Results
The OR for work-related MSP was significantly higher in the population with irregular working hours than in the population with regular working hours (OR: 1.43, 95% confidence interval [CI]: 1.29–1.58). Irregular and long (> 52 hours/week) working hours have the highest risk of work-related MSP in both genders (in men, OR: 3.48 [95% CI: 2.53–4.78]; in women, OR: 2.41 [95% CI: 1.46–4.00]).
Conclusions
Irregular working hours were associated with work-related MSP in Korea. The association was magnified with long working hours. Reform of the Korean Labor Standards Act leading to increase irregular working hours may induce adverse health outcome.
BACKGROUND
Recently, irregular working hours, or flexible working hours have become a controversial issue in Korea. Long working hours have brought a serious social burden in Korea, with a substantial negative impact on occupational health.1 Since 2018, a policy has been implemented to lower the upper limit of weekly working hours from 68 hours to 52 hours, that is, to 40 standard working hours and 12 maximum overtime working hours by labor-management agreements. Meanwhile, the business world has continued to request relief from the 52-hour regulations, claiming management difficulties owing to the company’s wage burden of additional employment and the coronavirus disease 2019 crisis. Governments tend to actively reflect these needs.2 The Future Labor Market Research Association, which has been researching improvements to the nation’s labor market, recommended several policies to increase the flexibility of working hours on December 12, 2022, including removing the 12-hour restriction on weekly overtime and the 52-hour cap. In addition, the Korean government pre-announced new policy reflecting that Association’s reports. This policy allows employees to work for > 52 hours in a certain week if the working hours of the following weeks are < 52 hours so that the average weekly working hours during the unit period are < 52 hours. The unit period for averaging is maximum 1 year in the pre-announced policy. However, this policy may lead to irregularities in the working environment.
Irregular working hours are controversial in terms of their health effects as they have both positive and negative effects on occupational health.3 Some recent studies have shown that who decides the working hours is a key factor: company or employee. Costa et al.4 confirmed that working time flexibility, determined by individual autonomy, increases work satisfaction, leading to a beneficial impact on health. However, company-oriented irregularity has consistently been reported to have adverse health effects.56 Meanwhile, the working hours analyzed in European studies are shorter than those in Korean studies, making it difficult to apply the results directly to the Korean labor market context.
Musculoskeletal disorders are an important disease group in occupational health, accounting for 56.8% of the approved cases of occupational diseases in 2021 in South Korea.7 According to the World Health Organization, musculoskeletal pain (MSP) imposes the highest disease burden on years lived with disability (YLDs), accounting for 17% of YLDs worldwide.8 In addition to conventional ergonomic risk and physical workload, psychosocial factors and the characteristics of working hours, such as overwork or shift work, are also related to MSP.91011 Previous studies on the musculoskeletal system and regularity of working hours have focused on shift work or precarious work; therefore, it is difficult to interpret the impact of irregular working hours itself.111213 Two studies have investigated the association between irregular working hours and accidents or mental health.1415 However, musculoskeletal disorders, which are highly prevalent, have not yet been studied.
Therefore, this study analyzed the association between irregular working hours and work-related MSP and additionally investigated the combined effects of long working hours on this association.
METHODS
Study design and participants
This study used data from the sixth Korean Working Conditions Survey (KWCS), a cross-sectional national survey conducted by the Korean Occupational Safety and Health Agency in 17 cities and metropolitan areas of Korea between October 2020 and January 2021. A previous study investigated the validity and reliability of this survey data.16
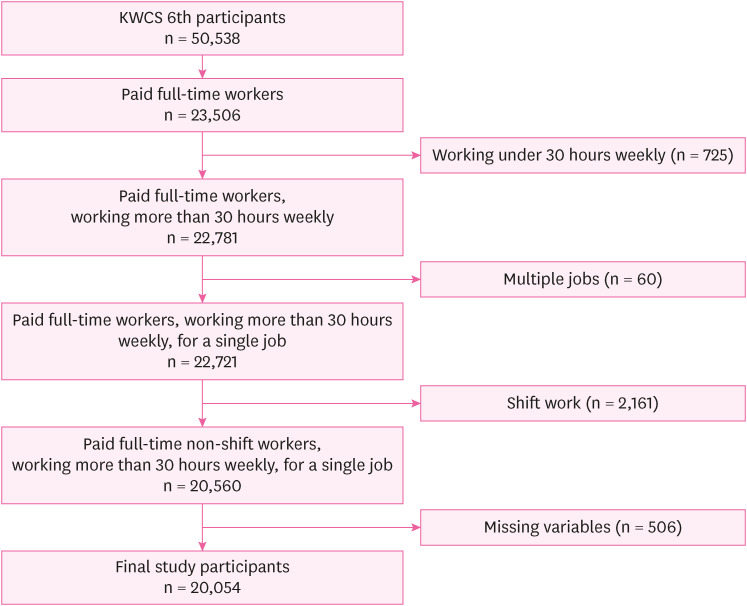
Of the 50,538 responders, 23,506 were full-time paid workers. To control for the confounding effects of precarious jobs, we excluded those who worked < 30 hours/week (n = 725) and having multiple jobs (n = 60). In order to interpret the impact of irregular working hours itself, the scope of this study is focused on those who work irregularly among non-shift workers. Therefore, we excluded shift workers (n = 2,161). After missing variables (n = 506) were excluded, 20,054 samples were included in the analysis (Fig. 1).
Work-related MSP
MSP and work-related MSP were investigated using 2 questions: “In the past year, have you experienced any of the following health problems?” and “If you have, did it happen because of your job?” These questions comprised 3 sub-questions: A) low back pain, B) upper limb pain, and C) lower limb pain.
If a person answered any of the 3, responding both “Yes, I have experienced pain” and “Yes, it was related to work” we counted that person as having work-related MSP.
Irregular working hours
Having irregular working hours was determined through questions on whether the participants worked the same number of hours every day, worked the same number of hours every week, worked the same number of days every week, or worked for fixed start and end times for each shift. If a responder answered “no” to any of these 4 questions, we defined that responder’s work schedule as irregular. A responder who answered “yes” to all these questions was regarded as having regular working hours.
Weekly working hour and worker’s control over working hours
Working hours were determined using questions regarding the number of hours people worked per week. As there are no confirmed criteria for long working hours, this study used social criteria for overwork as elucidated by the Labor Standards Act in Korea. We classified weekly working hours into 3 groups: i) 31–40 hours, ii) 41–52 hours, and iii) > 52 hours per week because 40 hours is the standard working hour per week according to the law, and 52 hours is the upper limit, with some exceptions. This criterion was used in the same manner as that in several recent studies.1417 Workers working < 30 hours a week were excluded from this study because their characteristics may be completely different from those of general workers because of reduced working hours due to reasons such as childcare, health problems, or unstable employment.
Previous studies have reported inconsistent outcomes between irregular working hours and health effects depending on whether the work schedule variability is employer-oriented or worker-initiated.34 Workers’ control over working hours is found to be one of the most important factors to be assessed. The KWCS asked whether the responder has control over working hours: “How is your working schedule arranged?” The answers were as follows: 1) The company sets the schedule and there is no possibility of changing it; 2) The company sets schedules and I can choose among them; 3) I can choose my working time by following some restrictions; and 4) I can decide my working time without any restrictions. The population was classified as having control over working hours if they answered 2), 3), or 4), and if they chose 1), the population was defined as having a rigid schedule.
Other variables
The analytic models of this study considered the following covariates: age (< 30, 30–39, 40–49, 50–59, or ≥ 60), gender (men or women), occupation, education (under high school, high school, or above high school), tenure (< 1, 1–5, 5–10, or ≥ 10 years), scale of workplace (< 10, 10–50, 50–300, or ≥ 300 workers), and physical and ergonomic occupational hazards. Occupation was coded by 9 major classifications (management, professional, clerical, service, sales, agriculture/forestry/fisheries, craft, machine operating/assembling, and elementary work), according to the Korean Standard Classification of Occupation.
Statistical analysis
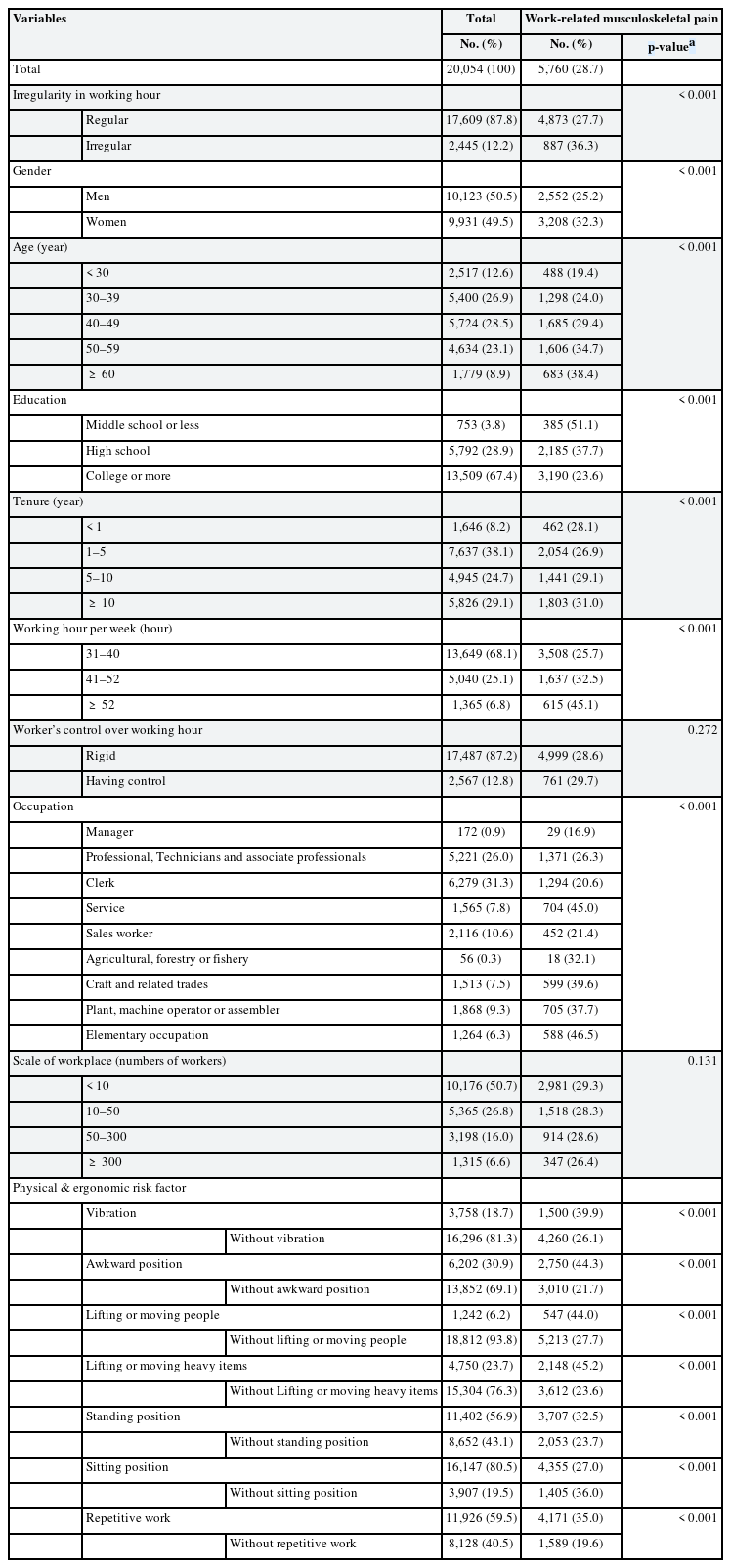
The prevalence of work-related MSP was presented according to demographic and occupational variables, including gender, age, education level, tenure, occupation, and control over working hours, and was analyzed using the χ2 test.
We drew a directed acyclic graph for the associations between possible covariates to determine confounders (Supplementary Fig. 1). The possible covariate candidates included demographic factors (gender, age, education level, and tenure), workplace factors (occupation and company scale), weekly working hours, control over working hours, work-related psychosocial factors (demand, control, and social support), work-related mental health, and ergonomic and physical hazards. Finally, demographic factors (age, gender, education level, and tenure), workplace factors (occupation and company scale), ergonomic and physical hazards, and control over working hours were adjusted for. Work-related psychosocial factors were not corrected because they were considered possible mediators.
A multiple logistic regression analysis was conducted to assess the association between irregular working hours and work-related MSP. We calculated the odds ratios (ORs) and 95% confidence intervals (CIs) of irregular working hours and work-related MSP, adjusted for age, gender, occupation, education, tenure, workplace scale, physical and ergonomic hazards, and control over working hours. We analyzed work-related MSP (work-related pain regardless of the anatomical part), work-related lower back pain, work-related upper limb pain, and work-related lower limb pain.
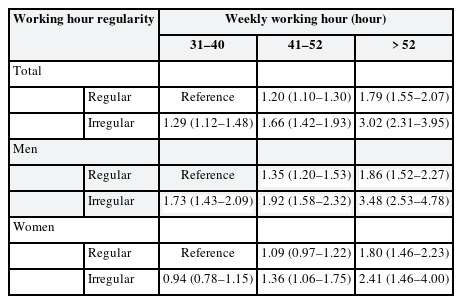
We conducted stratified analysis by gender, weekly working hours, and workers’ control over their working hours. All values were adjusted for age, education, occupation, tenure, company scale, and physical and ergonomic hazards (Fig. 2).
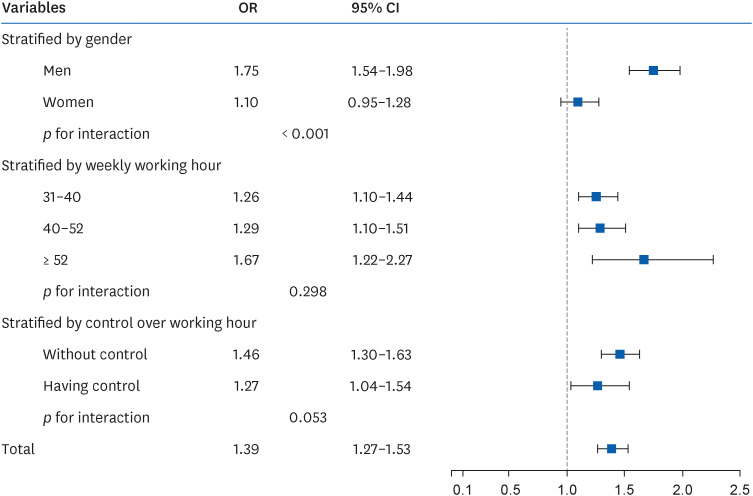
OR (95% CI) of work-related musculoskeletal pain according to working hour irregularity, stratified by gender, weekly working hours, or worker’s control over working hour. This result was adjusted for age, education, occupation, company size and physical and ergonomic hazards.
OR: odds ratio; CI: confidence interval.
Korean version of this article is available with the Online-only Data Supplement (Download PDF).
We presented the adjusted ORs of work-related MSP for irregular working hours combined with working hours (< 40 hours, 40–52 hours, and > 52 hours per week) stratified by gender, with the reference group working tolerable hours weekly (< 40 hours) and with a fixed schedule. All the analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC, USA) and p-values < 0.05 were considered statistically significant.
Ethics statement
This study used open data downloaded from websites based on the sixth KWCS results offered by the Korean Occupational Safety and Health Agency. This original study was approved with an exemption of ethical deliberation by the Institutional Review Board of Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea (exemption number: KC23ZASI0046).
RESULTS
Characteristics of study participants
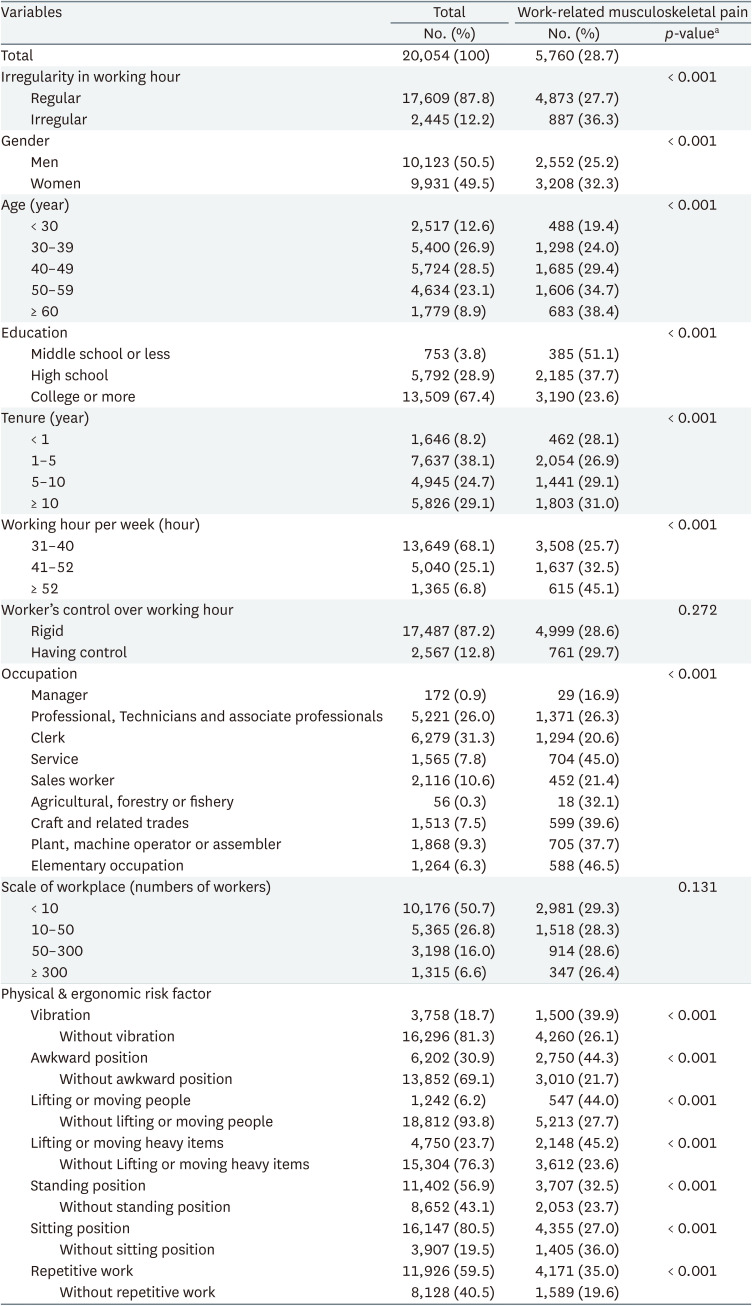
The number of work-related MSP reported in the total sample was 5,760 (28.7%), with 2,552 in men (25.2%) and 3,208 in women (32.3%). The characteristics of the study participants and the prevalence of work-related MSP in each population are presented in Table 1. The association between each variable and work-related MSP was calculated using the χ2 test (Table 1).
The population who worked irregularly had a higher prevalence of work-related MSP (36.3%) than those who worked regularly (27.7%). A higher prevalence of work-related MSP was observed in individuals with long working hours.
Association of irregular working hours and work-related MSP
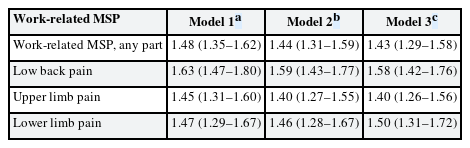
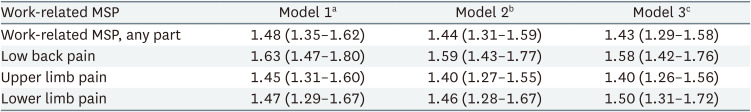
Table 2 shows the ORs of work-related MSP (95% CI) for any part, low back pain, upper limb pain, and lower limb pain. All results were statistically significant. The ORs of Models 2 and 3, with the latter additionally adjusted for control over working hours, were similar.
Fig. 2 presents the ORs of work-related MSP (95% CI) according to irregularity in daily or weekly working hours, stratified by gender, weekly working hours, and workers’ control over working hours. In men, the OR for work-related MSP was significantly higher in the population with irregular working hours than in the population with regular working hours (OR: 1.75, 95% CI: 1.54–1.98). When stratified by weekly working hours, those who worked longer had higher ORs (p-value for interaction = 0.30).
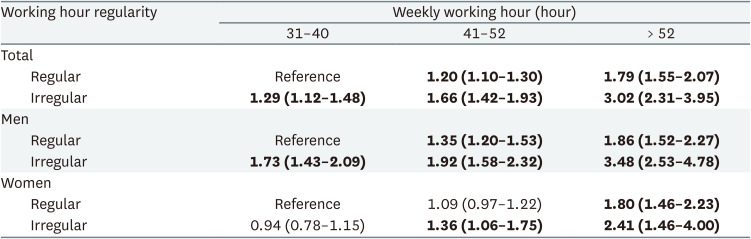
Table 3 shows that the groups with irregular and long (> 52 hours/week) working hours have the highest risk of work-related MSP in both genders (in men, OR: 3.48 [95% CI: 2.53–4.78]; in women, OR: 2.41 [95% CI: 1.46–4.00]). The impact was higher in men.
DISCUSSION
The risk of work-related MSP was higher in workers with irregular working hours than in those with regular working hours. This result is in line with those of previous studies on the association between irregular working hours and mental health and injury, revealing adverse health effects.1415 However, this is in contrast to a recent study by Garza et al.18 that reported no significant association between working time characteristics and MSP. This inconsistency may be because the sample size in Garza’s study18 is 316, with only 1.13% of participants working > 48 hours per week, whereas the final number of our participants is 20,054.
A plausible mechanism by which irregular working hours negatively affect work-related MSP is the overwork which is inevitable for a particular duration. The relationship between overtime work and the musculoskeletal system has been well established in previous studies.1119 In addition, overwork can increase the risk of work-related MSP even with a relatively short period. One recent longitudinal study reported that quantitative demands can increase MSP rapidly for a relatively short period of 4 weeks.20 Moreover, overwork can bring about insufficient rest outside working hours during the working period, as researchers have revealed it as a potential musculoskeletal hazard.1121
Another possible explanation is that psychosocial factors may mediate the higher risk of work-related MSP.22 Irregular working hours have been found to be related to workers’ depression and anxiety.14 In addition, employer-oriented irregular working hours can cause work-life conflicts. Hämmig et al.23 found that work-life conflict is a major factor related to MSP, mediated by stress.35 Therefore, the higher risk of work-related MSP in the population with irregular working hours may have been mediated by psychosocial stress.
Employer-oriented irregular working hours and employee-initiated working hour flexibility are frequently distinguished, and flexibility is considered to have a positive effect on health.4 In the stratified analysis, the association between irregular working hours and work-related MSP became weaker when workers had control over their work schedule (Fig. 2). This suggests that controlling the working schedule can alleviate work-related MSP. However, the effect of control may need to be carefully analyzed along with other factors, such as the combination of working hours, rather than interpreted alone.
The OR of work-related MSP with irregular working hours was higher when combined with long working hours. This association was confirmed in the same direction when stratified by gender. In particular, men with irregular working hours and working > 52 hours had an OR of 3.48 (95% CI: 2.53–4.78), compared to men in the reference group who had regularly worked 31–40 hours a week. This relationship was confirmed when stratified according to work type (white collar, OR: 3.26 [95% CI: 1.97–5.38]; pink collar, OR: 2.26 [95% CI: 1.36–3.78]; blue collar, OR: 3.35 [95% CI: 2.25–5.01]) (Supplementary Table 1). This suggests that in Korea, where long working hour is common, the adverse effects of irregular working hours can be magnified. Moreover, irregular working hours may be a separate health hazard factor since the OR was statistically significant even when stratified into 31–40 hours (OR: 1.26, 95% CI: 1.10–1.44), which is a comparatively permissive range.
The OR of work-related MSP in women was smaller than that in men. The possibility of a selection bias should be considered. Korean women are forced to drop out of the labor market more easily when working conditions become unfavorable, as suggested in previous studies.2425 Hence, women employees having work-related MSP had high possibility of quitting their jobs, which is related to a selection bias.
To the best of our knowledge, this is the first study to show an association between irregular working hours and MSP. The strength of this study is that it examined the general working population using Korean national data. Consistent results were observed when the subtypes of MSP at each site was analyzed. However, this study has several limitations. First, as a cross-sectional study, it has limitations regarding causality. In this regard, there is a need for additional research with longitudinal data to address this causal relationship. Second, information on symptoms and exposure was obtained using self-administered questionnaires; this method relies on the accuracy of the responder’s memory and may be subject to non-response and recall biases. Specifically, having irregular working hours was defined and categorized operationally using unstructured questions; hence, the responses only provided contextual information and not quantitative data. Third, this study evaluated MSP with a particular focus on irregular working hours without considering key confounding factors such as medication use, history of musculoskeletal diseases, and other health behaviors (e.g., hobbies and leisure-time physical activity) because the information provided in the survey did not include these variables.
CONCLUSIONS
Irregular working hours have a substantial relationship with work-related MSP, and this relationship becomes more remarkable when combined with long working hours and lack of control over working hours. This has an implication on Korea, confronting the social requirement of reducing working hours, in that the adverse effects of irregular working hours should be carefully considered.
This study showed the association between irregular working hour and work-related MSP was strengthened when combined with long working hours. In 2021, Korean employees worked 1,910 hours, the fourth longest number of hours among the member countries of the Organization for Economic Co-operation and Development (OECD). One hundred ninety-four hours are more than the average of OECD countries’ working hours, which was 1,716.26 Under these circumstances, the results of this study suggest that policies that increase irregular working hours are not suitable for enhancing occupational health with respect to MSP.
Acknowledgements
The authors appreciate the Occupational Safety and Health Research Institute for providing the raw data from the 6th Korean Working Conditions Survey.
Notes
Funding: This research is supported by National Research Foundation of Korea (NRF-2022R1F1A1066498).
Competing interests: The authors declare that they have no competing interests.
Authors contributions:
Conceptualization: Kang MY.
Data curation: Yang M.
Formal analysis: Yang M.
Validation: Kang MY.
Visualization: Yang M.
Writing - original draft: Yang M.
Writing - review & editing: Myong JP, Lee J, Park MY, Kang MY.
Abbreviations
CI
confidence interval
KWCS
Korean Working Conditions Survey
MSP
musculoskeletal pain
OECD
Organization for Economic Co-operation and Development
OR
odds ratio
YLD
year lived with disability
References
SUPPLEMENTARY MATERIALS
Supplementary Data 1
Korean version paper
Supplementary Table 1
Odds ratioa (95% confidence interval) of work-related musculoskeletal pain according to irregularity in working hour combined with weekly working hour, stratified by types of work
Supplementary Fig. 1
Directed acyclic graph figure for association between working hour irregularity and work-related MSP. Green color line refers to the suggestive causal pathway.