Radiation-related occupational cancer and its recognition criteria in South Korea
Article information
Abstract
Ionizing radiation is a well-known carcinogen, and is listed as one carcinogenic agent of occupational cancer. Given the increase in the number of workers exposed to radiation, as well as the increase in concern regarding occupational cancer, the number of radiation-related occupational cancer claims is expected to increase. Unlike exposure assessment of other carcinogenic agents in the workplace, such as asbestos and benzene, radiation exposure is usually assessed on an individual basis with personal dosimeters, which makes it feasible to assess whether a worker’s cancer occurrence is associated with their individual exposure. However, given the absence of a threshold dose for cancer initiation, it remains difficult to identify radiation exposure as the root cause of occupational cancer. Moreover, the association between cancer and radiation exposure in the workplace has not been clearly established due to a lack of scientific evidence. Therefore, criteria for the recognition of radiation-related occupational cancer should be carefully reviewed and updated with new scientific evidence and social consensus. The current criteria in Korea are valid in terms of eligible radiogenic cancer sites, adequate latent period, assessment of radiation exposure, and probability of causation. However, reducing uncertainty with respect to the determination of causation between exposure and cancer and developing more specific criteria that considers mixed exposure to radiation and other carcinogenic agents remains an important open question.
Background
Ionizing radiation is classified as a Group 1 carcinogen in humans by the International Agency for Research on Cancer (IARC), and is listed as one carcinogenic agent of occupational cancer by the International Labor Organization (ILO) and the Enforcement Decree of the Labor Standards Act in Korea [1–3]. Ionizing radiation is called “radiation” henceforth in this paper. Radiation is utilized for various purposes, and both the number of radiation-related facilities and the number of radiation workers have also increased by about 10 and 4% per year, respectively [4]. Radiation exposure has been well managed under 5% of the occupational dose limit which is a 100 mSv in 5 years with a maximum of 50 mSv in any single year, in most radiation workers in Korea. However, some occupations, such as workers who perform non-destructive testing (NDT) and radiologists, are exposed to relatively higher radiation levels than other radiation-related occupations [5]. Moreover, due to an increase in social concerns about occupational cancer, the number of occupational cancer claims related to radiation exposure is increasing, especially among semiconductor manufacturing and NDT workers. In general, criteria for the recognition of radiation-related occupational cancer are based on the type of cancer, exposure assessment, probability of causation, and general principles of compensation for occupational diseases. These criteria should be updated with new scientific evidence and social consensus. The aim of this study, therefore, was to review the recognition criteria for radiation-related occupational cancer and identify the characteristics of radiation exposure and diagnosed cases in the workplace in Korea. This review provides a comprehensive reference for understanding criteria for the recognition of radiation-related occupational cancer, which can help to guide reasonable and scientific decision making.
Review
Occupational exposure in Korea
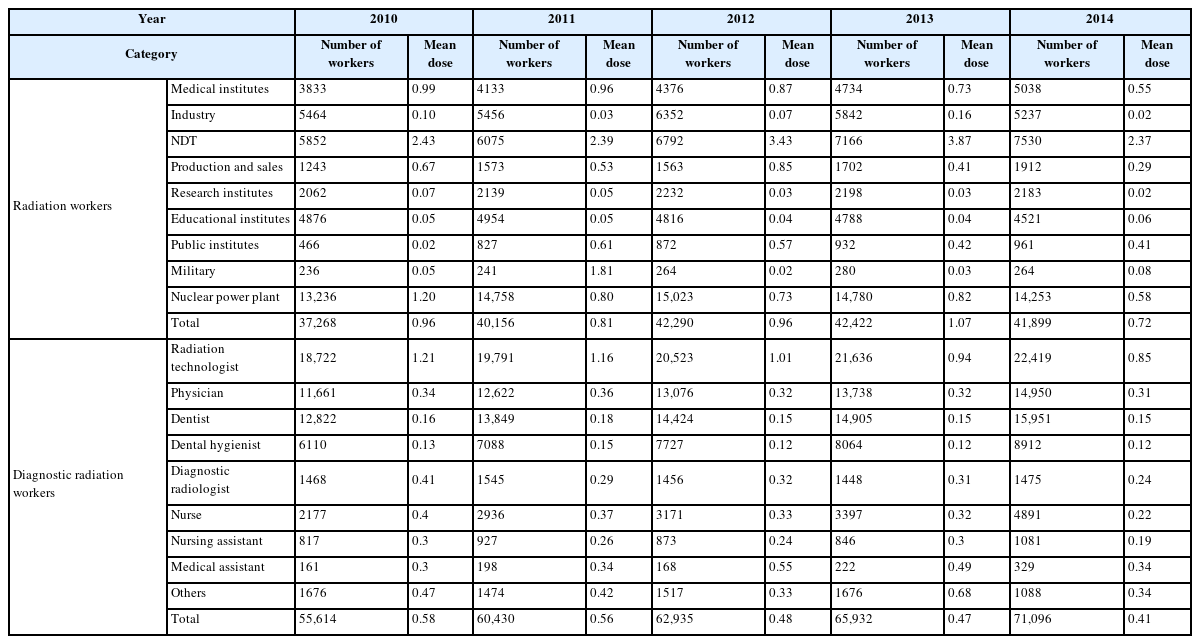
Exposure assessment is essential for identifying whether cancer incidence among workers is caused by harmful agents in the workplace. In Korea, depending on the occupation type, radiation exposure in individual workers has been monitored and managed by two government institutes, the Nuclear Safety and Security Commission (NSSC) and the Centers for Disease Control and Prevention (CDC), with their own National Dose Registries (NDR). To determine whether cancer occurrence in the workplace is associated with radiation exposure, these NDRs are investigated first for radiation exposure assessment. Radiation workers in the NDR who are managed by the NSSC are grouped into nine categories: public institution, educational institution, non-destructive industry, industrial organization, research institute, nuclear power plant, medical institution (except for workers using diagnostic x-ray generators), military, and production and sales [6]. Since the NDR was started in 1984, the average exposure dose for radiation workers has been in steady decline to nearly 1 mSv per year or less, except for NDT workers, whose exposure levels were the highest with average doses of 2.37–3.87 mSv/year in the recent five years (Table 1) [5, 6]. Exposure doses of diagnostic radiation workers, who mainly work with x-ray generators in hospitals, were managed by the CDC’s NDR and grouped into five categories: radiologic technologists, physicians, dentists, dental hygienists, and other radiation workers [7]. Exposure doses have been in steady decline over the last 10 years among diagnostic radiation workers. Exposure levels were highest among radiologic technologists, with average doses of 0.85–1.21 mSv/year in the recent 5 years (Table 1) [8].
Radiation carcinogenesis
The initial mechanism of radiation-induced cancer is not different from the mechanisms of other harmful agents, such as toxic chemicals and ultraviolet radiation, in terms of DNA damage. It is well-known that many innate defense mechanisms against radiation damage occur in various ways (e.g., removal of oxidative stress and damaged cells, DNA repair) in the human body, and damaged cells or DNA that remain may cause tissue or organ dysfunction and malignant disease such as cancer and heritable disease. In general, health risks from radiation exposure are classified into two groups: tissue reactions, which are conventionally referred to as deterministic effects, and stochastic effects. Tissue reaction effects include organ malfunction such as skin burns, bone marrow failure, and intestinal damage, which occur above a threshold dose below which there is no increased risk and are considered non-cancer damaging effects. In contrast, stochastic effects are assumed to have no threshold dose and occur by chance, with the probability of the effect increasing as exposure dose increases. The main risks associated with stochastic effects are cancer and genetic defects, and generally occur 1–2 years after exposure for leukemia and 5–10 years after exposure for solid cancer. Thus, radiation-related occupational cancer can be considered a stochastic effect of radiation exposure.
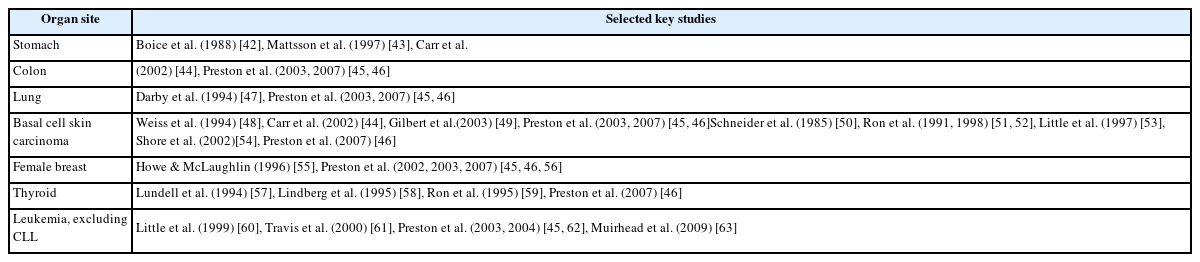
The IARC and the U.S. National Toxicology Program (NTP) classify radiation (commonly referred to as ionizing radiation), including x-rays and gamma rays, as “Group 1” and “Known” carcinogens, respectively, according to their own classification criteria [9]. The European Agency for Safety and Health at Work similarly interprets radiation carcinogenesis according to the classification of carcinogens, mutagens, and reprotoxicants (CMR) substances, based largely on human evidence [10]. Regarding the evaluation of a causal association between radiation exposure (i.e., x-ray and gamma rays) for individual cancer (organ) sites, the IARC has categorized cancer sites into “strong evidence” and “potentially having limited or inadequate evidence” based on up-to-date scientific evidence [9]. Cancer sites with “strong evidence” are listed in Table 2, and these evaluations were carried out based on biological data and epidemiological evidence.
Review of epidemiological studies of cancer risk
Atomic bomb survivors and the Chernobyl accident
One major source of epidemiological data to evaluate health risks from radiation exposure is the Life Span Study (LSS) of atomic bomb survivors, which found a proportional relationship between cancer risk and exposure dose. Although numerous findings from the study provide scientific evidence for increased cancer risk from radiation exposure, radiation-associated cancer risk remains unclear at low-dose ranges under 100 mSv [11]. Studies related to the Chernobyl accident also demonstrated cancer risks from radiation exposure, especially an increase in thyroid cancer among children with high thyroid-absorbed doses. Except for this result, however, no definitive conclusions have been made regarding other cancers among Chernobyl residents who were exposed to low doses of radiation [12–15]. Some studies that have investigated the health of Chernobyl workers exposed to prolonged low to medium doses of radiation (average effective dose of 100 mSv) have reported increased risks of cancer as well as non-cancer diseases, such as cataracts and cardiovascular diseases [16–21]. However, due to screening effects (e.g., medical examinations) and limited sample sizes, it is difficult to draw definitive conclusions from these studies. Thus, it remains necessary to continue follow-ups of these cohorts with accurate assessments of exposure dose, health outcomes, and confounding factors [14, 22].
Occupational exposure in radiation workers
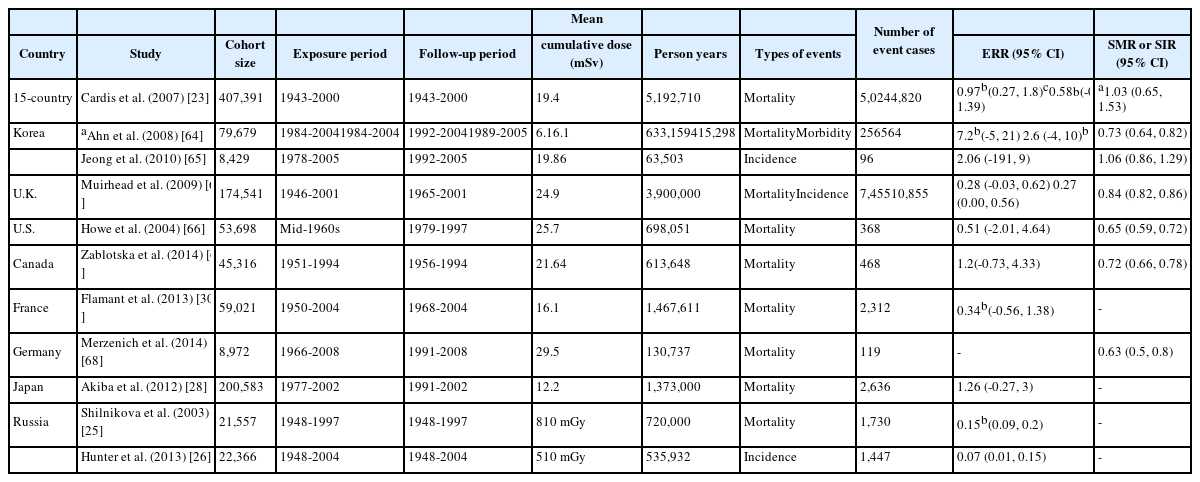
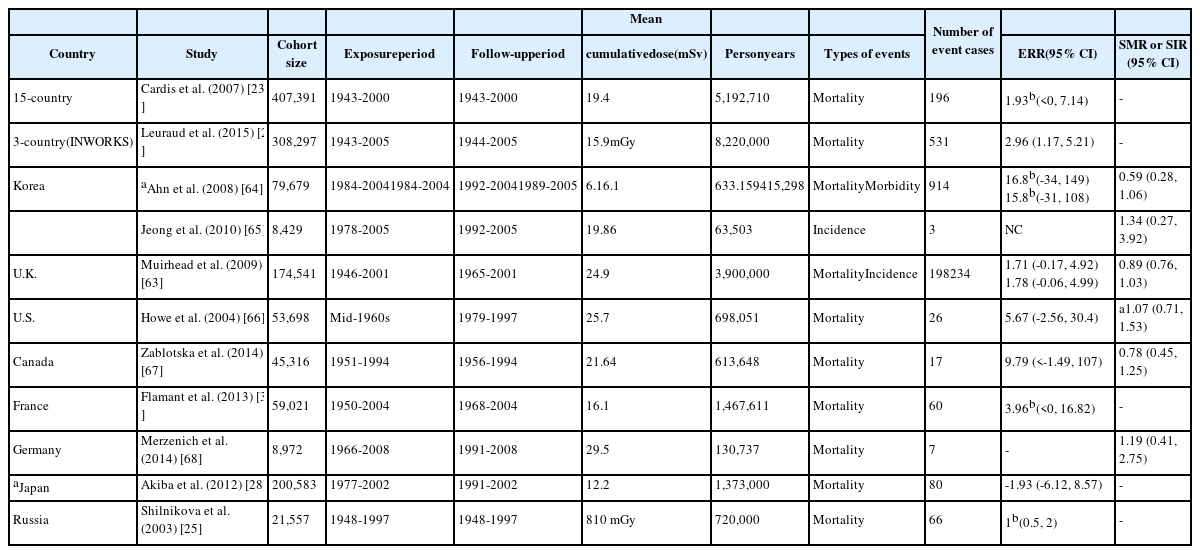
A major distinction between occupational exposure and accidental exposure is the period and dose levels of exposure. Whereas accidental exposure usually involves a single large exposure (acute), occupational exposure involves protracted exposures to low-dose radiation (chronic). A number of epidemiological investigations have been conducted among radiation workers in individual countries as well as in large-scale international cohort studies, and the cancer risk from occupational exposure to radiation continues to be updated. A few studies have reported elevated risks of cancer with statistical significance. One of the largest occupational studies in radiation workers is the 15-country collaborative study, which included 407,391 nuclear industry workers over 5.2 million person-years of follow-up [23]. In this study, an elevated risk of all-cancer mortality was observed, with an excess relative risk (ERR/Sv) of 0.97 (95% CI: 0.27, 1.8). However, this risk diminished after excluding data from workers in Canada, in whom the dose measurement was uncertain, and the observed risk was no longer significant. As a follow-up to the 15-country collaborative study, risks of leukemia and lymphoma were investigated among 308,297 radiation workers in France, the U.K., and the U.S. [24]. The association between exposure dose and cancer mortality was statistically significant with an ERR of 2.96 per Gy (90% CI: 1.17, 5.21) for leukemia, excluding chronic lymphocytic leukemia (CLL). The highest ERR/Gy of 10.45 (90% CI: 4.48, 19.65) was found for chronic myeloid leukemia, indicating a strong association between leukemia mortality and protracted low-dose radiation exposure [24]. Although the ERR of leukemia, excluding CLL, was not attenuated for doses less than 100 mGy, the 90% CIs were too wide to make a definitive conclusion about the low-dose ranges.
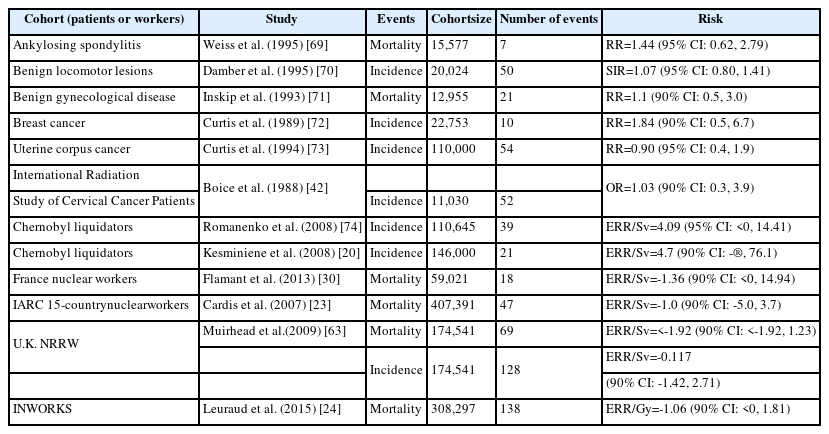
Cohort studies of the Mayak nuclear complex workers also reveal an elevated cancer risk [25–27]. Because this cohort had a broad range of cumulative doses due to high exposure levels during the early stages of the facility operation, the dose-response relationship had a degree of precision that is rarely observed in other studies of radiation workers, who are usually exposed to low-dose levels [26]. In addition to the Mayak cohort studies, other studies of radiation workers have reported increased risks of certain types of cancer, such as leukemia (excluding CLL), esophageal cancer, and lung cancer [28–31]. However, risks for individual cancer sites are inconsistent across most radiation epidemiological studies, and many studies do not find statistically significant results. Cancer risks from major health studies in nuclear workers are summarized in Tables 3 and 4.
Aircrews, such as pilots and flight attendants, are exposed to cosmic radiation. Although aircrews are not included in the national registry for radiation workers in Korea, they should be considered radiation workers and monitored for radiation exposure and health risks, because they are exposed to similar or even higher levels of radiation compared to common radiation-related occupations, such as nuclear workers and radiologists. An average effective dose in an aircrew flying over the poles at high latitudes is estimated to be 2–5 mSv/year, which may reach a cumulative dose of about 75 mSv over the course of a worker’s career [32]. Many interesting health studies have been conducted in aircrews based in Nordic countries, the U.S., and Canada. These studies have reported higher risks of breast cancer, prostate cancer, brain cancer, skin cancer, non-Hodgkin’s lymphoma, and acute myeloid leukemia among aircrews, compared with the general population [33–37]. However, given that no demonstrated dose-response relationship was found, these elevated cancer risks do not imply a causal relationship with radiation exposure.
In summary, despite the existence of several epidemiological studies in radiation workers, cancer risks from occupational exposure, especially for doses less than 100 mSv, remain poorly understood due to uncertainty about exposure dose and confounding factors, possible misclassification of health outcomes, and limited statistical power [24, 38].
Diagnosed cases of radiation-related occupational cancer in Korea
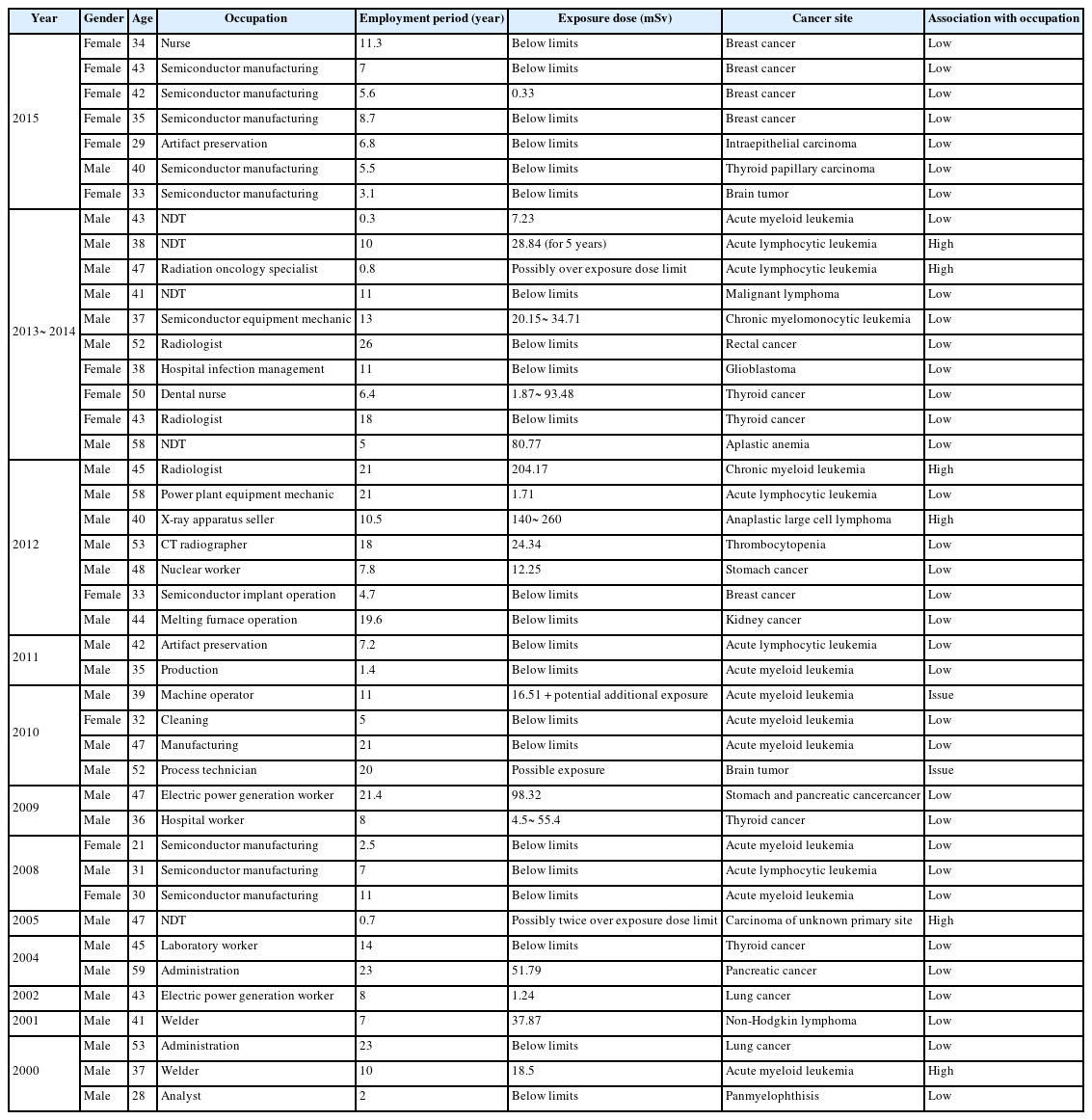
Recognition of work-related disease is made through the Occupational Disease Approval Committee of the Korea Workers’ Compensation and Welfare Service (COMWEL). According to Article 38 of the Industrial Accident Compensation Insurance Act (IACIA) and Article 7 of the enforcement regulations of the IACIA, the following are diseases that do not require deliberation from COMWEL: (1) pneumoconiosis, (2) carbon disulfide poisoning, (3) diseases with serious acute syndromes from acute exposures to high levels of hazardous agents and relevant risk, and (4) obvious occupation-related disease. In general, criteria for the diagnosis of radiation-related cancers include the cancer site, exposure dose, latent period of cancer, and probability of causation. More strict diagnostic criteria have been applied to thyroid cancer because it is the most common type of cancer found by chance. Table 5 summarizes the characteristics of diagnosed cases of radiation-related occupational cancer in Korea from the occupational disease annual reports (2000–2015) of the Korea Occupational Safety and Health Agency (KOSHA). This list excludes acute diseases due to acute exposure to high levels of hazardous agents and relevant risk according to Article 25 of the enforcement regulations of the IACI Act. Of 43 deliberated cases that may possibly be related to occupational exposure, approximately 70% included male workers, six cases were classified as having a “strong relationship” with occupational exposure, and two cases remained classified as “issues”. All eight cases involved male workers, the youngest of whom was 37 years old. Most of these eight cases had leukemia, including acute myeloid leukemia (AML), acute lymphocytic leukemia (ALL), and chronic myeloid leukemia (CML). Cancers other than leukemia included anaplastic large cell lymphoma, brain cancer, and carcinoma with an unknown primary site.
Considerations in the recognition criteria for occupational cancer
Recognition criteria in Korea
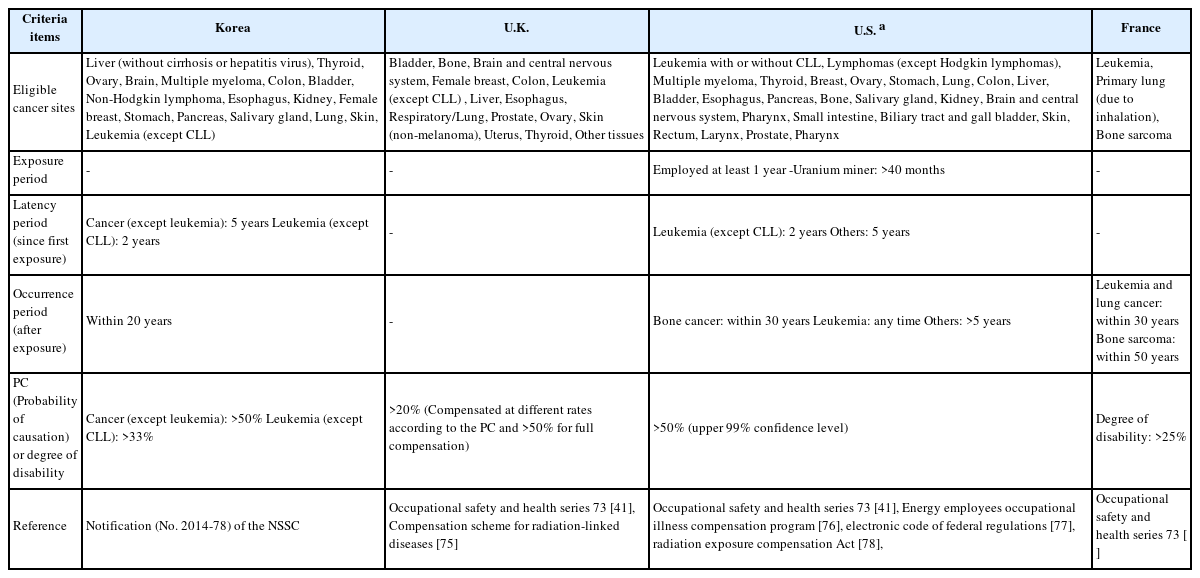
Several criteria should be met cumulatively to obtain the recognition of radiation-related occupational cancer. These criteria are well described in Notification No. 2014-78 of the NSSC regarding regulations on occupational disease among radiation workers. The major criteria are summarized here. First, cancer must be eligible for radiation-induced cancer: liver cancer, except those cancers that involve cirrhosis or the hepatitis virus (e.g., types B or C); thyroid cancer; ovarian cancer; brain cancer; multiple myeloma; colon cancer; bladder cancer; Non-Hodgkin lymphoma; esophagus cancer; kidney cancer; female breast cancer; stomach cancer; pancreatic cancer; salivary gland cancer; lung cancer; skin cancer; and leukemia, excluding CLL. Several cancers are not recognized as radiation-related occupational cancer, namely Hodgkin’s lymphoma, melanoma, malignant mesothelioma, and CLL. These classifications are based mainly on findings from epidemiological studies. For example, mesothelioma is a well-known asbestos-related cancer, and approximately 80–90% of mesotheliomas are caused by long-term inhalation of asbestos [39]. As another example, whereas leukemia is a radiation-sensitive cancer, CLL has not been associated with radiation exposure in most epidemiological studies (Table 6). Second, radiation exposure must be identified by dose assessment or circumstantial evidence. For the assessment of exposure levels, dose records from the NDR are considered a priority. Additional assessments, such as dose reconstruction, are necessary for unclear or omitted cases. Third, a latent period (i.e., time between the first exposure and the appearance of a tumor) must be considered as sufficient or relevant to cancer incidence. For example, solid cancer can be recognized as occupational cancer only if the cancer occurs at least 5 years after the first exposure, whereas leukemia (excluding CLL) can be recognized as occupational cancer only if the cancer occurs at least 2 years after the first exposure and within 20 years after the last exposure. Lastly, the probability of causation (PC), which is defined as the probability that a cancer was caused by occupational radiation exposure during employment, determines whether an individual’s cancer is “at least as likely as not” (i.e., a PC of 50% or greater) related to occupational exposure [40]. The PC is calculated as cancer risk attributable to radiation exposure divided by the sum of baseline cancer risk to the general population plus the risk attributable to radiation exposure, considering personal information (e.g., birth year, gender), medical information (e.g., type of cancer, year of diagnosis), and exposure information (e.g., age at exposure, radiation dose). Given that a threshold dose for cancer has not been identified yet, risks of cancer are stochastic effects, and therefore the PC is an important objective measure to assess a causal relationship with radiation exposure. Based on the current guidelines from the NSSC, PCs for solid cancer and leukemia should exceed 50% and 33%, respectively. However, PC includes an estimation error due to uncertainties about dose and the dose rate effectiveness factor (DDREF), as well as a risk transfer error between different populations; therefore, there exist cases with a PC less than 50% that are fully or partially recognized as occupational cancer in civil litigation.
Recognition criteria in other countries
The recognition criteria for radiation-related occupational cancer are based on scientific evidence. However, ultimately, their acceptable range and levels are often affected by several factors unrelated to science, such as social, cultural, and economic factors. In particular, complex elements, such as the social status of the radiation-related occupation, number of workers, cancer incidence rate in the general population, specific risk perceptions of certain cancers, and economic wealth, factor into the recognition of occupational cancer. For these reasons, recognition criteria differ across countries or even across occupations within the same country. For example, CLL is generally excluded as an occupational cancer due to lack of scientific evidence regarding radiation-induced CLL. However, CLL is considered as being potentially caused by radiation, and hence, as potentially compensable under the Energy Employees Occupational Illness Compensation Program Act of 2000 (EEOICPA), effective March 7, 2012 in the U.S. In addition, eligible cancer sites differ according to occupation (e.g., special exposure cohort, uranium workers, energy employees, soldiers). Regarding the PC, the EEOICPA applies the upper 99% credibility (i.e., confidence) limit of the PC instead of the point estimate (i.e., 50th percentile) to the determination of causation between exposure and cancer, which provides each worker with the benefit of the doubt before a final compensation decision is made. In France, the criteria for recognition or compensation for cases not relevant to the regulatory guidelines are more relaxed through individual case assessments, meaning that cases with non-radiogenic disease or an inadequate latent period can be possibly compensated when the disease is obviously related to occupational exposure and the disability from the disease is over 25% [41]. Major recognition criteria of Korea and other countries are compared in Table 7.
Conclusions
Based on the scientific evidence and compared with the guidelines of other countries, the current recognition criteria for radiation-related occupational cancer in Korea are valid in terms of the eligibility of cancer sites, adequacy of the latent period, assessment of radiation exposure, and probability of causation. However, the exact quantification of exposure dose is often not possible, and therefore the recognition criteria involve some degree of uncertainty. Therefore, it is proposed that exposure doses of all radiation-related workers be carefully monitored without a dead zone in exposure management, and more relaxed criteria be considered for a margin of uncertainty through the use of the upper 95% or 99% credibility limit of the PC. In addition, further recognition criteria are necessary for more complex exposures, e.g., to two or more carcinogenic agents, including radiation.
Abbreviations
ALL
Acute lymphocytic leukemia
AML
Acute myeloid leukemia
CAREX
Carcinogen exposure database
CDC
Centers for Disease Control and Prevention
CLL
Chronic lymphocytic leukemia
CML
Chronic myeloid leukemia
COMWEL
Korea Workers’ Compensation and Welfare Service
DDREF
Dose and the dose rate effectiveness factor
EEOICPA
Energy Employees Occupational Illness Compensation Program Act of 2000
ERR
Excess relative risk
IACIA
Industrial Accident Compensation Insurance Act
IARC
International Agency for Research on Cancer
ILO
International Labor Organization
KOSHA
Korea Occupational Safety and Health Agency
NDR
National Dose Registries
NDT
Non-destructive testing
NSSC
Nuclear Safety and Security Commission
NTP
U.S. National Toxicology Program
PC
Probability of causation
Acknowledgements
This research was supported by the Nuclear Safety Research Program through the Korea Foundation Of Nuclear Safety (KOFONS), granted financial resource from the Nuclear Safety and Security Commission (NSSC), Republic of Korea (No. 1303028 and 1503008).
Funding
This work was supported by the Nuclear Safety Research Program through the Korea Foundation Of Nuclear Safety (KOFONS), granted financial resource from the Nuclear Safety and Security Commission (NSSC), Republic of Korea (No. 1303028 and 1503008).
Availability of data and materials
Data sharing no applicable to this article as no datasets were generated or analysed during the current study.
Authors’ contributions
YWJ and SS designed this study and wrote this manuscript. DL, KMS, and SP contributed to the draft of the manuscript and identification of related references. SGK and JUW provided valuable inputs in developing the study design and contents. All authors reviewed and approved the final manuscript.
Notes
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.