Increased breast cancer incidence among nurses in a tertiary university hospital in South Korea
Article information
Abstract
Background
A series of breast cancer cases were recently reported in a tertiary university hospital in South Korea. Nurses are generally exposed to risk factors for breast cancer such as night shift work, antineoplastic agents, and job strain. However, the epidemiological evidence of excess incidence among nurses remains lacking. This study aims to investigate the excess incidence of breast cancer among nurses in a tertiary university hospital and provide epidemiological evidence of occupational risk factors.
Methods
A retrospective cohort was developed using personnel records of female workers in the nursing department who worked from January 2011 to June 2021 in a tertiary university hospital in South Korea. Sick leave records were used to identify cases of breast cancer. The standardized incidence ratio of breast cancer among nurses was compared to the general population.
Results
A total of 5,509 nurses were followed up for 30,404 person-years, and 26 breast cancer cases were identified. This study revealed a significantly increased breast cancer incidence among all included nurses, with a standardized incidence ratio of 1.65 (95% confidence interval [CI]: 1.08–2.41), compared to the general population. Workers, who handle antineoplastic agents in their representative department and current and/or former department, had significantly elevated breast cancer standardized incidence ratios of 2.73 (95% CI: 1.008–5.94) and 3.39 (95% CI: 1.46–6.68), respectively.
Conclusions
This study provides significant evidence of increased breast cancer risk among nursing staff in a hospital setting, particularly those who handle antineoplastic drugs. Measures that reduce exposure to risk factors should be implemented, especially anticancer drugs, to protect healthcare professionals. Further research at a national level that focuses on healthcare workers is necessary to validate breast cancer incidence and its contributing factors.
BACKGROUND
Nurses could be exposed to various physical, chemical, and psychological hazards. Generally, occupational risk factors for breast cancer include ionizing radiation, electromagnetic fields, night shift work, ethylene oxide exposure, perfluorinated compounds, antineoplastic drugs, metals, and job strain.12 Among these factors, night shift work, anticancer drug exposure, and job strain were identified as potential exposures through previously conducted in-depth interviews with the cases.
Recently, 4 workers in the department that handles antineoplastic agents in a tertiary university hospital were reported. The nursing department includes registered nurses and nurse assistants and represents the largest proportion of employees within the organization. The total workforce at the hospital accounted for 8,690 in 2020, including 2,922 (33.6%) working in the nursing department. Among them, the majority are females (n = 2,798), accounting for > 90%. Identifying harmful working conditions through these cases and accordingly establishing a safe working environment in the hospital is important because of the high proportion of the labor force.
An updated report by the International Agency for Research on Cancer (IARC) in 2019 on night shift work revealed an association with breast cancer, but epidemiological evidence in humans was lacking due to large heterogeneity among studies.34 Meanwhile, a prospective cohort study that involves nurses revealed a significantly increased incidence of breast cancer among nurses who work night shifts for > 30 years.5 Anticancer agents (e.g., busulfan, chlorambucil, cyclophosphamide, etoposide) demonstrated sufficient evidence to cause cancer in humans.6 Epidemiological studies have revealed an excess incidence of cancer in nurses who handle antineoplastic drugs.78 A Swedish study revealed an increased risk of breast cancer among women in full-time employment who experienced job strain,9 but the association between breast cancer and job strain has been inconsistent among other studies.1011
Some studies on the incidence or mortality of breast cancer among healthcare workers, including nurses, consistently revealed an increase in the risk of breast cancer.121314 In particular, a nationwide retrospective cohort study in Korea confirmed a significantly increased incidence of breast cancer among female healthcare workers in hospitals.14 However, these studies evaluated nurses as a single group and did not differentiate or assess their risks separately.
Therefore, this study aimed to present epidemiological evidence of occupational risk factor exposure within a tertiary university hospital by investigating the excess incidence of breast cancer among employees in the nursing department and comparing them to the general population.
METHODS
Cohort definition
We used personnel records from the hospital to construct a retrospective cohort of nursing department workers in a tertiary university hospital in South Korea. . These records included demographic information (birth date and gender), work history (entry/exit dates and workplace), sick leave history (reason and start/end dates), and annual leave history (number of days and start/end dates). This study included female employees in the nursing department who worked at the hospital from January 1, 2011, to June 30, 2021. This open cohort study enrolled newly hired employees during the cohort follow-up period as new study participants. This study excluded workers who were not affiliated with the Nursing Department or male workers. Finally, the cohort included a total of 5,509 qualified individuals.
The point of entry for those who joined the hospital before that date and the actual date of employment for those who joined afterward was January 1, 2011. The first sick leave due to breast cancer during the observation period was used as the cut-off point for follow-up observation, or the resignation date within the follow-up period for retired employees, or June 30, 2021, for the employees who remained even after that day.
Event definition
Sick leave records during the follow-up period defined breast cancer occurrence. The disease names in the records were inconsistently entered in both English and Korean, and a variety of terms for breast cancer were utilized. Therefore, cases were classified as breast cancer if they contained both words indicating a target organ (breast) and a target disease (cancer). The onset of breast cancer was the date of the first sick leave request due to breast cancer.
We applied no disease clearance period because we were unable to ascertain the occurrence of breast cancer before the cohort entry point. Further, we did not consider a latent period.
Workplace classification for exposure assessment
Of the occupational risk factors for breast cancer among nurses, night shift work, anticancer drug exposure, and job strain were identified as potential exposures through previously conducted in-depth interviews with the cases. This study used the workplace as a proxy for exposure to these risk factors because we could not directly evaluate the above-mentioned exposures.
Workers’ representative workplace is where the worker served the longest during the follow-up period. The workplace was classified as “none” if the workplace was not listed in the personnel records during the follow-up period. The workplace could be tracked annually through personnel records, but mid-year changes could not be verified.
The representative workplaces were categorized based on four criteria: 1) workplaces that handle antineoplastic agents, including the hematology ward, and those related to anticancer treatment, versus other workplaces, 2) 4 classifications by main function: ward, outpatient/support, surgery/procedure/treatment, and emergency/intensive care, 3) annual leave usage by workplace: upper, middle, and lower thirds, and 4) average employee tenure by workplace: upper and lower 50%.
Workplaces that handle anticancer drugs were analyzed to understand the risk of work experience in these workplaces, associated with breast cancer incidence. The workplace used in personnel records may have been named for administrative convenience and may not accurately reflect the exact duties, thus the main tasks performed in each workplace were comprehensively considered, and the workplaces were categorized into four major functions. Furthermore, someone’s absences were expected to minimally affect workplaces with high annual leave usage. Therefore, we used the annual leave usage of the workplace as an indirect workplace job demand indicator. Additionally, the average tenure of the workplace refers to the mixed effect of indirect risk factor exposure.
Furthermore, the use of their representative workplace as exposure could neglect their previous work experience, although that period would be relatively shorter. Therefore, the workers were classified based on their experience in a workplace that handles anticancer drugs after joining the hospital. This study defines a previous work experience as serving in a specific workplace in the personnel record, which was updated yearly. This, their record in the specific workplace in the specific year indicates that they worked in that workplace for at least ≥ 1 month in that year.
Statistical analysis
Indirect standardization methods were used to calculate age-standardized breast cancer incidence ratios because of the different age distributions among the groups.1516 Having prior knowledge of the incidence rates within the standard population is necessary. The expected number of cases within the study population can be calculated based on this information, and the ratio of observed cases to expected cases should be computed. We used the female population of the middle of 2015 from Statistics Korea as the standard population because the follow-up period was from January 1, 2011, to June 30, 2021. Age-specific breast cancer incidence in the general population was sourced from Cancer Statistics published by the Ministry of Health and Welfare in Korea. The standardized incidence ratio was calculated as the ratio of the observed number of cases in each representative workplace classification to the expected number of cases derived from each 5-year age group. A Poisson model was used to calculate the 95% confidence interval (CI) and significance level (p-value).17 Further, the standardized incidence ratio (SIR) was calculated based on past work experience in specific workplaces to verify robustness. We provided the hospital with an Excel worksheet that would compute the age-SIR of breast cancer once the necessary data was inputted because raw data was inaccessible. We then received the summary statistics of the results. SAS STDRATE procedures (Version 9.3; SAS Institute INC., Cary, NC, USA) were used for statistical analysis.
Ethics statement
The Institutional Review Board (IRB) of Seoul National University Hospital waived the need for written informed consent to exempt the review of this study (IRB No. E-2109-032-1252).
RESULTS
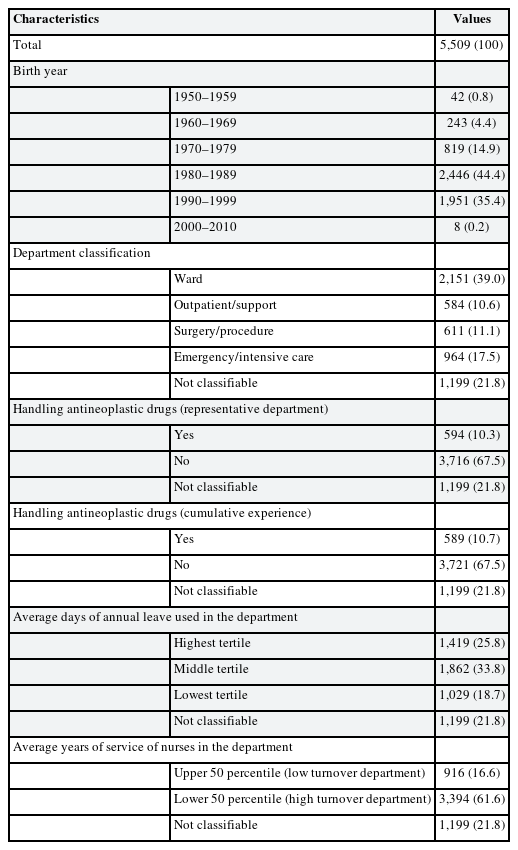
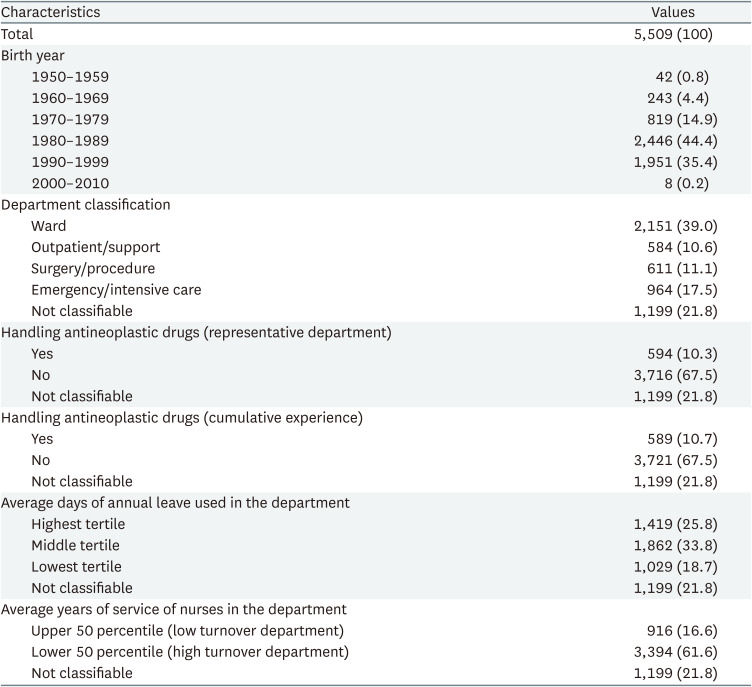
The study cohort consisted of 5,509 workers, contributing to an overall observation time of 30,404 person-years, equating to an average observation period of 5.5 years per person. Their average age with standard deviation at entry to the hospital was 24.5 ±3.9 years and the average employment duration was 8.8 ± 8.8 years. We observed 26 cases of breast cancer during the follow-up period. The cohort primarily consisted of those born in the 1980s (44.4%) and 1990s (34.4%), followed by the 1970s (14.9%) and 1960s (4.4%). We classified the work assignments of 4,310 workers, thereby leaving 1,199 individuals unclassified due to missing workplace records.
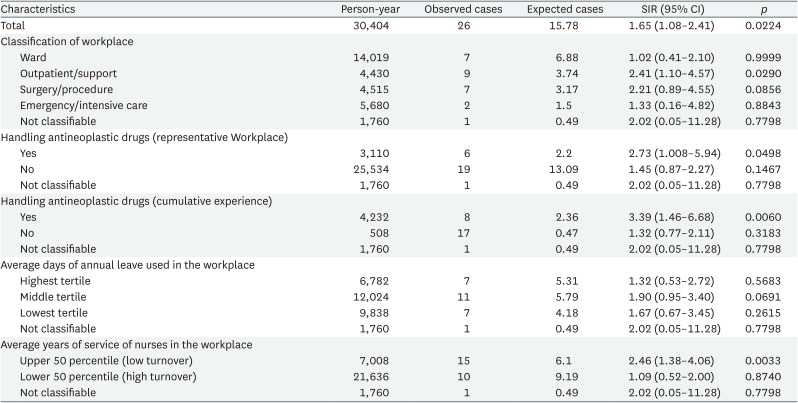
Workers from workplaces that handle these agents accounted for 10.34% (n = 594) when representative workplaces were categorized into those handling antineoplastic agents and those who are not. Functional workplace categorization revealed that the largest group consisted of those working in the ward (39.0%, n = 2,151 of the total workforce), followed by those serving in emergency or intensive care units (17.5%, n = 964). Workers from outpatient/support and surgery/procedure/treatment workplaces have similar distributions of 584 (10.6%) and 611 (11.1%) individuals, respectively (Table 1).
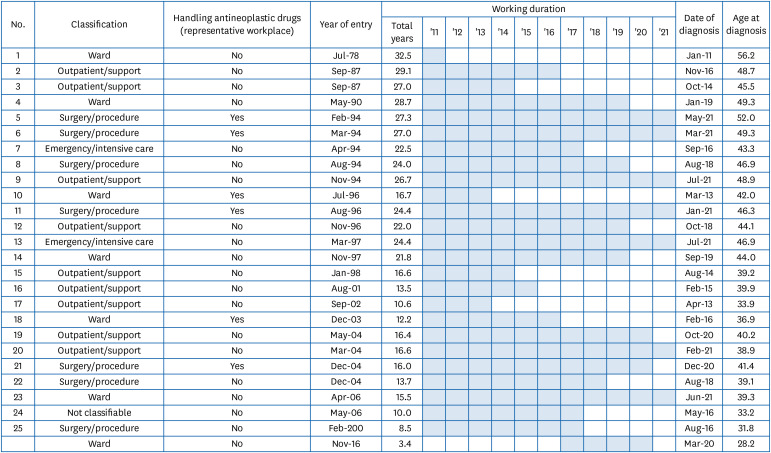
Fig. 1 shows the characteristics of the 26 participants who were diagnosed with breast cancer. Of the 26 total cases, 9 (32.1%) were observed in outpatient workplaces. Both ward workers and surgery/procedure/treatment workers accounted for 21.8% each, consisting of 7 cases each. Additionally, we confirmed 2 cases in the emergency/intensive care workplace and 1 case among the unclassified worker group. Workers in the representative workplace that frequently handles anti-neoplastic agents accounted for 23.1% (6 cases) and the other workers were 76.9% (20 cases). The date of entry to the hospital was between July 1978 and November 2016, while the average working duration was 19.5 ± 7.3 years. The mean age at diagnosis was 42.5 ± 6.5 years.
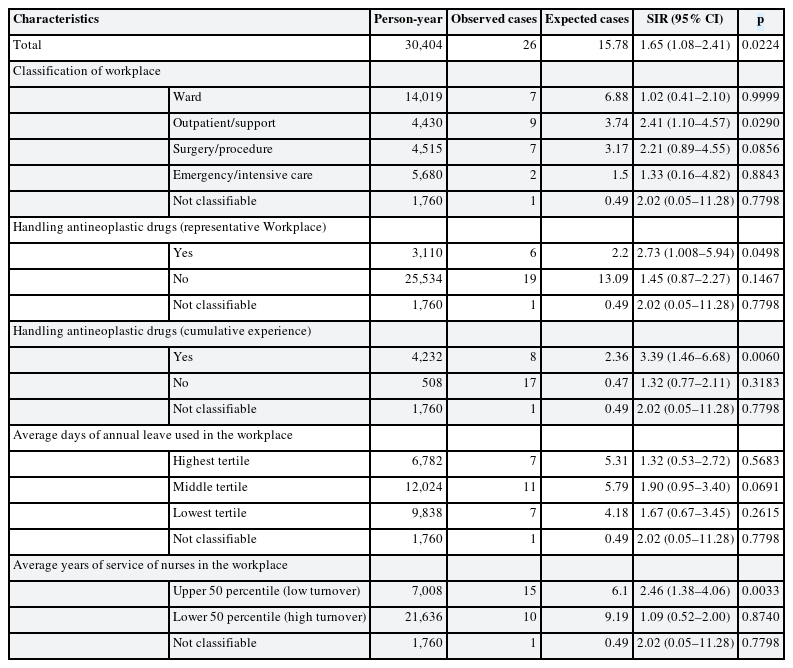
The indirect standardization method was used to calculate SIRs, with the general population as a comparison group. The SIR of the total workers in the Nursing Department in the hospital was significantly elevated at 1.65 (95% CI: 1.08–2.41). The SIR was statistically significantly high at 2.73 (95% CI: 1.00–5.94) when we identified the representative workplace as frequently handling antineoplastic agents, and 3.39 (95% CI: 1.46–6.68) when we identified the cumulative experience on that workplace. However, workplaces that do not engage with antineoplastic agents reported SIRs of 1.45 (95% CI: 0.87–2.27) based on the representative workplace and 0.47 (95% CI: 0.77–2.11) based on the cumulative experience (Table 2). Only the outpatient/support workplaces exhibited a significantly higher SIR at 2.41 (95% CI: 1.10–4.57) when we categorized the representative workplace into four major functions. Other functional categories were not significant. SIRs did not demonstrate significant differences among upper, middle, and lower groups when we categorized workers based on tertiles of annual leave usage by the workplace. The SIR was significantly higher for workers in workplaces in the upper 50% of average tenure at 2.46 (95% CI: 1.38–4.06) when we categorized the workers into the upper and lower 50% groups based on average tenure by workplace (Table 2).
DISCUSSION
We developed a retrospective cohort of 5,509 female nurses using personnel records from a tertiary university hospital. The comparison of breast cancer incidence in our study population to that of the general population revealed a higher incidence in the total study population (SIR: 1.65; 95% CI: 1.08–2.41) and among workers who handle antineoplastic agents (SIR: 2.73; 95% CI: 1.00–5.94).
Studies consistently revealed higher rates of breast cancer incidence among healthcare workers, including nurses. Rix and Lynge12 investigated cancer incidence in Danish healthcare workers using census and cancer register records and revealed a high incidence of breast cancer among female registered nurses (SIR: 1.19; 95% CI: 1.08–1.30). A cohort study in Taiwan included physicians and revealed an increased breast cancer risk among females (hazard ratio: 2.00; 95% CI: 1.11–3.62).13 A study in Korea that used a nationwide health insurance database to construct a retrospective cohort of 107,646 female healthcare workers in hospitals revealed a significantly increased SIR for breast cancer compared to the entire worker population (SIR: 1.21, 95% CI: 1.09–1.36).14 These results are congruent with our study findings, where the SIR for breast cancer in female workers in the nursing department as a whole was significantly higher at 1.65 (95% CI: 1.08–2.41).
Night shift work should be considered an occupational risk factor for breast cancer in nursing positions.1 A meta-analysis study in Denmark revealed that the risk ratio between night shift workers for a relatively short period of < 8 years and general workers was 1.21, but with no statistical significance (95% CI: 0.97–1.32).18 Other systematic reviews and meta-analysis studies revealed a relatively increased risk of breast cancer by 1.21–1.91 times with experience of night shift work, and the risk of breast cancer increases by approximately 3% for every additional 5 years of night shift work.19 A prospective cohort study with 114,559 nurses in the United States revealed no significance in the breast cancer risk ratio of 0.94 for night shift nurses for 15–29 years (95% CI: 0.81–1.10), but the ratio was significantly higher at 1.40 (95% CI: 1.00–1.10) for those with > 30 years of night shift work.5
This study revealed that workers in the workplace with higher employment tenure have a higher risk of breast cancer incidence. The mixed effect of many potential risk factors for breast cancer among nurses explains this finding. The night work shift is one of the important factors in breast cancer occurrence. A high proportion of the subjects may have been exposed to night shift work, considering that 69.7% of nurses working in tertiary hospitals in Korea are known to work on a 3-shift basis according to nationwide survey results.20 Therefore, as the average years of service of workers in the workplace increased, their exposure to night shift work for a longer period is estimated to increase, which could affect breast cancer development.
Moreover, antineoplastic agents should be considered as occupational risk factors for breast cancer, to which the nurses in this study could have potentially been exposed. In 1979, Falck et al. in Finland reported significantly higher levels of mutagenic substances in the urine of nurses working with antineoplastic drugs compared to psychologists and office clerks.7 A meta-analysis revealed cyclophosphamide detection in 11 out of 12 studies that analyzed the urine of nurses and other workers who handle antineoplastic drugs.21 Additionally, a cohort study of 56,213 Canadian female nurses from 1974 to 2000 demonstrated epidemiological evidence of an increased risk of breast cancer among nurses who work in cancer centers or oncology nursing units.7
Our study did not measure biological antineoplastic drug exposure, but we confirmed that nurses, who predominantly handle these drugs, had a 2.73 times higher risk (95% CI: 1.00–5.94) of developing breast cancer compared to the general population. This trend was even more pronounced for nurses at the Oncology Daycare Center and Injections and Treatment Unit of the Cancer Hospital, where the risk surged as high as 12.90 times. A sensitivity analysis of workers who were previously employed in antineoplastic drug-handling workplaces revealed the robustly maintained risk of breast cancer at 8.54 times. These results indirectly indicate that antineoplastic drug exposure at worksites may contribute to breast cancer incidence. However, these results should be cautiously interpreted because of the shorter observation years of the study workplaces (342 person-years) compared to the total observation years (30,404 person-years), which might cause unstable ratio measurements.
The association between job strain and breast cancer has been inconsistent, but it is considered plausible. Some studies revealed no significant association between breast cancer and job strain.1011 However, a cohort study with 36,332 Swedish females defined a group with high job demand and low job autonomy as a group with high job strain. The group with high job strain had a significantly higher risk of breast cancer at 1.2 times.9 Our study conducted a subgroup analysis based on the workplace’s annual leave usage but revealed no significant association with breast cancer risk. This analysis hypothesized that annual leave usage indirectly shows the job demand in the workplace. However, qualitative research seems necessary to gain a more accurate understanding of the job demands of each workplace.
Breast cancer is more likely to be detected earlier with increased screening frequencies. This potentially introduces a detection bias that tends to increase the disease prevalence among nurses. Previous studies in Korea reported a breast imaging examination rate of 15.7% among nurses at 5 hospitals in 2002 and a 15.3% periodic breast mammography rate at another two hospitals in 2008,2223 which was notably lower compared to the national cancer screening rate of 33.2% and 49.3% in 2004 and 2008, respectively, among females aged > 40 years. A study in Taiwan revealed that < 10% of nurses reported being screened for breast cancer within the past 2 years in 2017, which is lower than the screening rate of 38.0% among general females aged 45–69 in 2015–2016.24 Thus, these results confirmed that the screening rate of the breast cancer among our subjects was not significantly higher than the general population. Additionally, this study revealed that 53.8% of breast cancer was diagnosed in the 40s, which does not significantly differ from the epidemiologically confirmed prevalent age group in South Korea.25 Considering these factors, we conclude a low likelihood of early detection bias due to frequent screening in the study population.
This study confirmed the excess risk of breast cancer by tracking and observing a considerable number of hospital staff in South Korea. The result, in comparison to the general population, is also meaningful despite the presence of the healthy worker effect, which can potentially bias results toward null. Previous studies have revealed higher breast cancer incidence and mortality rates among nurses in South Korea as a whole.1426 However, this study indirectly confirmed the risk of some occupational hazards (antineoplastic drugs, job strain, and night shift work) for breast cancer by understanding the characteristics of the affiliated workplaces and tasks within a single large tertiary hospital based on internal personnel data.
However, this study has several limitations. This study is based on the personnel records of a specific institution. A personnel record-based cohort cannot confirm the exposure to risk factors and medical history before the worker’s admission, and tracking individuals after resignation is also impossible. Therefore, this study may be biased in both directions. Further, we were unable to adjust for individual factors, including reproductive history, familial history, hormone intake, smoking status, alcohol drinking,27 and obesity, because information on such risk factors was unavailable. Additionally, we considered no disease clearance period due to a lack of data before cohort entry. Access to data with longer periods could generate more robust and comprehensive results in the future.
Our study applied no latent period because each occupational risk factor may have distinct latent periods. In particular, night shift work among nurses for > 30 years significantly increases the risk of breast cancer.5 However, other risk factors included in our study contained no well-established information regarding their specific latent periods.
The anticancer drugs are known to be associated with the development of various cancer types, including acute myeloid lymphoma. However, this study did not comprehensively evaluate these potential associations.28
Confirming the exposure to risk factors requires additional methods, such as working environment measurement or biological monitoring, because the exposure to risk factors was not qualitatively evaluated, but categorized based on the workplace characteristics. The event definition might have a bias that converges toward null, as detection is only possible when the ill worker applies for sick leave. This causes missed cases or reports to be filed later than the actual diagnosis, thereby extending the follow-up time. However, this study revealed the very high incidence of breast cancer in workers from the workplace that handles antineoplastic drugs, which tends to have little effect on the study results.
We compared the risk of breast cancer incidence only to the general population. This result would become robust if we compared the subjects to another group, such as all female workers or female office workers in the same hospital. Alternatively, comparing the nursing staff with all employees within the hospital could have minimized the bias due to the healthy worker effect and enhanced comparability.
Finally, regional or institution-specific factors could influence our results that were drawn from a single university hospital, thus our results may not represent all healthcare institutions in the country. Future longitudinal studies that analyze the risk of cancer occurrence according to occupation and tasks among the Korean medical workforce are required through nationwide multi-institutional research.
CONCLUSIONS
This study significantly revealed that hospital employees in South Korea face an increased risk of developing breast cancer, particularly among nursing staff who handle antineoplastic drugs. Our results provide an essential step toward better understanding and managing the occupational risks of healthcare professionals. We recommend the implementation of comprehensive protective measures, such as rigorous procedures when handling antineoplastic drugs, reduced night shift schedules, and extensive job strain management programs, which may reduce the risk of breast cancer in hospital staff. Additionally, more regular and focused cancer screening programs should be implemented for staff who are exposed to higher occupational hazards. Further validation through nationwide studies is warranted to fully understand the depth of occupational hazards in the medical field and develop appropriate preventive strategies.
Notes
Funding: This research was supported by Seoul National University Hospital.
Competing interests: The authors declare that they have no competing interests.
Author Contributions:
Conceptualization: Lee DW.
Data curation: Lee DW.
Formal analysis: Choi J.
Funding acquisition: Lee DW, Hong YC.
Investigation: Choi J.
Methodology: Lee DW.
Project administration: Lee DW, Hong YC.
Supervision: Kim T.
Validation: Lee DW.
Writing - original draft: Choi J, Choi BY, Ryoo SW.
Writing - review & editing: Lee DW, Hong YC.
Abbreviations
CI
confidence interval
IARC
International Agency for Research on Cancer
SIR
standardized incidence ratio