Association between shift work and the risk of hypothyroidism in adult male workers in Korea: a cohort study
Article information
Abstract
Background
Shift work has been reported to have several harmful effects on the human body. However, a small number of studies have evaluated the association between shift work and adverse effects on the thyroid. In our longitudinal study, we examined the causal association between shift work and the risk of hypothyroidism.
Methods
A Kangbuk Samsung Cohort Study was conducted on 112,648 men without thyroid disease at baseline who were followed up at least once between 2012 and 2019. Shift work status and shift schedule types were categorized using standardized questionnaires. Hypothyroidism was defined using the reference ranges of serum thyroid-stimulating hormones and free thyroxine levels. Hazard ratios (HRs) and 95% confidence intervals (CIs) for incident hypothyroidism were estimated using Cox proportional hazards regression analyses with the daytime work group as the reference.
Results
During the 501,237 person-years of follow-up, there were 6,306 incident cases of hypothyroidism (incidence density, 1.26 per 100 person-years). The multivariable-adjusted HR of incident hypothyroidism for the shift work total group that included all shifts compared with the daytime work group was 1.27 (95% CI: 1.15–1.40). For the fixed evening, fixed night, rotating shift, and other shift workers, the multivariable-adjusted HRs (95% CI) were 1.11 (0.76–1.61), 2.18 (1.20–3.93), 1.39 (1.23–1.56), and 1.00 (0.82–1.22), respectively. In subgroup analyses by age, the association between shift work and hypothyroidism was more pronounced in younger participants (< 40 years; HR: 1.31; 95% CI: 1.16–1.47).
Conclusions
Our large-scale cohort study showed an association between shift work and the incidence of hypothyroidism, especially in younger workers with night shifts.
BACKGROUND
Nowadays, in many industry sectors, including transportation, health care, manufacturing, and services, shift work is necessary to ensure that 24-hour consumption and production can continue.1 Shift work is defined by the International Labor Organization as the organization of working time wherein workers succeed one another at the workplace so that the establishment can operate longer than the hours of work of individual workers, with workers assigned different daytime and night hours.2 Night shift work is a type of shift work, and the Labor Standards Act of Korea defines night work as the work performed between 10 PM and 6 AM the following morning.3 The world over, shift work is a typical work schedule, and in developed nations worldwide, it is estimated that about 15%–20% of employers use the shift system.4 According to the 2017 data from the European Union, shift work was estimated at 21% of the workforce, and in Korea, approximately 10% of workers work in shifts.56
In 2019, night shift work was classified as a probable human carcinogen by the International Agency for Research on Cancer (a group 2A carcinogen).1 According to changes in sleep/wake cycles, shift work, especially night shift work, is known to have negative effects on the human body.78 Many previous studies have reported that shift work can cause several adverse health effects, such as sleep disorders, cardiovascular, gastrointestinal, and neuropsychiatric diseases, and the risk of cancer.9101112131415 Although thyroid-stimulating hormone (TSH) secretion shows distinct circadian rhythmicity,16 evidence for the relationship between circadian discrepancy and adverse effects on the thyroid is lacking.
Hypothyroidism is widespread across the world, affecting up to 5% of the general population, and an additional 5% are estimated to be undiagnosed.17 From 2013 to 2015, 3.8% of people in Korea had hypothyroidism, according to the Korea National Health and Nutrition Examination Survey (KNHANES VI).18 With increasing awareness of the prevention of hypothyroidism, which can affect cardiovascular, cognitive, and other metabolic conditions, shift work has been identified as an occupational risk factor by epidemiological studies on hypothyroidism.1920 However, a small number of studies have evaluated the association between shift work and thyroid-related diseases, and most of the earlier research used a cross-sectional design that was limited in explaining causality.
Therefore, the aim of this study is to evaluate the causal association between shift work and hypothyroidism by cohort design using data from the Kangbuk Samsung Cohort Study.
METHODS
Study design and participants
The Kangbuk Samsung Cohort Study is a cohort study of Koreans aged at least 18 years who underwent annual or biennial comprehensive health screening examinations at the Kangbuk Samsung Hospital Total Healthcare Center in Seoul and Suwon, Korea. Most participants were employees of various companies and local governmental organizations and their spouses. The Occupational Safety and Health Act in Korea requires that all employees receive free annual or biennial health medical examinations. Other examinees underwent health medical check-ups voluntarily at the healthcare center.
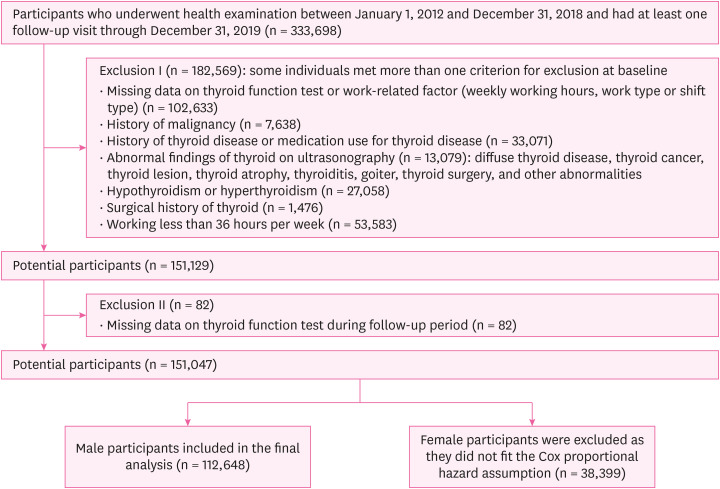
Our study included a total of 333,698 participants who underwent health examinations from January 1, 2012, to December 31, 2018, and had undergone at least one other screening exam before December 31, 2019. First, we excluded 182,569 participants who had any of the following conditions at baseline (Fig. 1): missing data on thyroid function tests or work-related factors, history of malignancy, history of thyroid disease or medication use for thyroid disease, abnormal thyroid findings on ultrasonography, hypothyroidism or hyperthyroidism at baseline, surgical history of the thyroid, working less than 36 hours per week. Second, among 151,129 potential participants, we further excluded 82 participants who had missing data on thyroid function tests during follow-up. We conducted Cox proportional hazards regression analyses on 151,047 potential participants and excluded 38,399 female participants as they did not fit the proportional hazard assumption. Finally, 112,648 male participants were eligible for the study at baseline.
Measurement and definition of variables
All examinations were conducted at the Kangbuk Samsung Hospital Total Healthcare Screening Center in Seoul and Suwon. At each visit, information was collected on demographic characteristics, working characteristics, smoking status, alcohol consumption, medical history, and medication use using standardized, self-administered questionnaires. Smoking status was categorized as non-current and current smokers. For alcohol consumption, heavy drinking was categorized as ≥ 30 g/day for men and ≥ 20 g/day for women. Cardiovascular disease was defined as a self-reported history of cardiovascular disease or current use of medications for cardiovascular disease.
Shift work was identified using the following self-reported questionnaire: “In the past year, during which time of the day did you work the most?” Participants who answered, “I worked mostly during the day (between 6 AM and 6 PM)” were defined as daytime workers. Participants who answered, “I worked during other hours” were defined as shift workers. Among shift workers, shift schedule types were categorized as the fixed evening shift (between 2 PM and midnight), fixed night shift (between 9 PM and 8 AM the next day), regular day and night rotating shift, 24 hours rotating shift, irregular rotating shift, split shift (working ≥ 2 shifts/day), and other shifts. Shift workers were subdivided into 4 subgroups by the shift schedule type: fixed evening shift work, fixed night shift work, rotating shift work (night rotating shift, 24 hours rotating shift, and irregular rotating shift), and other shift work (split shift and other shifts). Those who responded that they were working on shifts but did not specify the shift schedule type were also classified as others. Information on the weekly working hours was obtained using the following question: “How many hours did you work in a week on average in your job for the past year, including overtime?”
Blood pressure, weight, and height were measured by trained nurses. Obesity was defined as a body mass index (BMI) ≥ 25 kg/m2. Hypertension was defined as a systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, self-reported history of hypertension, or the current use of anti-hypertensive medications. Fasting blood measurements included glucose, thyroid-TSH, and free thyroxine (fT4) levels. Diabetes was defined as a fasting serum glucose level of ≥ 126 mg/dL, self-reported history of diabetes, or the current use of anti-diabetic medications.
Thyroid function tests were performed regularly at each visit. Serum TSH (normal range: 0.25–5.0 μIU/mL) and fT4 (normal range: 0.93–1.7 ng/dL) levels were measured by radioimmunoassay using a commercial kit (RIA-gnost® hTSH, fT4; Schering-Cis Bio International, Gif-sur-Yvette, France), with lower detection limits of 0.025 μIU/mL and 0.06 ng/dL, respectively. The intra-assay and inter-assay coefficients of variation for quality control specimens were 1.2%–5.7% and 2.4%–5.4%, respectively, for TSH, and 2.3%–4.4% and 2.1%–5.7%, respectively, for fT4.21 Hypothyroidism was defined as a serum TSH level above the upper reference limit with a normal serum fT4 level (subclinical hypothyroidism) or a serum fT4 level below the lower reference limit (overt hypothyroidism).22
Statistical analysis
Descriptive statistics were used to summarize the characteristics of participants categorized by shift work schedule (daytime worker vs. shift worker). The primary endpoint was the development of incident hypothyroidism (subclinical or overt hypothyroidism). Participants were followed up from the baseline until the endpoint visit or to the last available visit until December 31, 2019, whichever came first. Incidence density was calculated as the number of incident cases divided by the number of person-years in follow-up.
Hazard ratios (HRs) and 95% confidence intervals (CIs) for incident hypothyroidism were estimated using Cox proportional hazards regression analyses. Initially, only age was adjusted in the crude model. Model 1 was further adjusted for age, alcohol intake, and smoking status. To adjust for the potential confounders, Model 2 was further adjusted for diabetes, hypertension, cardiovascular disease, and BMI. Lastly, to adjust for other occupational risk factors, Model 3 was further adjusted for working hours. The proportional-hazards assumption was assessed by examining graphs of estimated log (-log) survival and by using the “estat phtest” command based on Schoenfeld residuals; no violation of the assumption was found.
To explore whether the associations between long working hours and hypothyroidism differed, subgroup analyses were performed by age (< 40 vs. ≥ 40 years), and weekly working hours (≤ 52 vs. > 52 hours). Interactions between the groups of working hours and subgroup characteristics were tested using likelihood ratio tests, which compared models with and without multiplicative interaction terms.
Statistical analyses were performed using STATA version 18.0 (StataCorp LP, College Station, TX, USA). All reported p-values were 2-tailed. A p-value < 0.05 was considered statistically significant.
Ethics statement
This study was approved by the Institutional Review Board (IRB) of Kangbuk Samsung Hospital (IRB No. KBSMC 2023–03–034), which waived the requirement for informed consent. This was because we accessed only de-identified data routinely collected as part of health screening examinations.
RESULTS
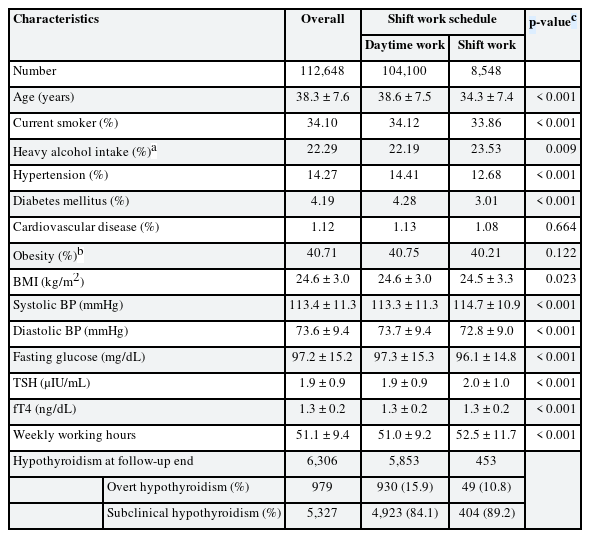
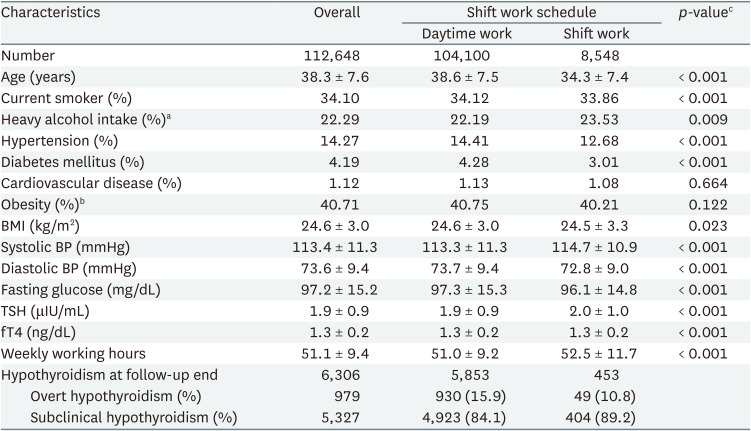
In Table 1, the mean ± standard deviation of age, serum TSH, and fT4 levels at baseline were 38.3 ± 7.6 years, 1.9 ± 0.9 μIU/mL, and 1.3 ± 0.2 ng/dL, respectively. Age, high-risk drinking rate, obesity rate, BMI, diastolic blood pressure, fasting blood sugar level, and working hours per week were higher in the shift work group than in the daytime work group at the first visit. Conversely, rates of smokers, hypertension, diabetes, and systolic blood pressure were lower. At the end of the observation, there were 979 cases of overt hypothyroidism and 5,327 cases of subclinical hypothyroidism, with more subclinical hypothyroidism cases.
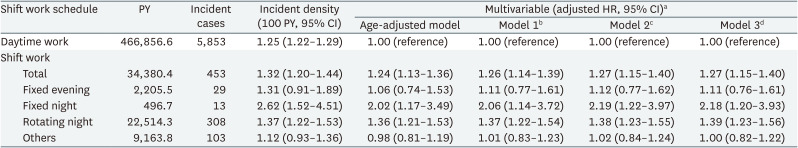
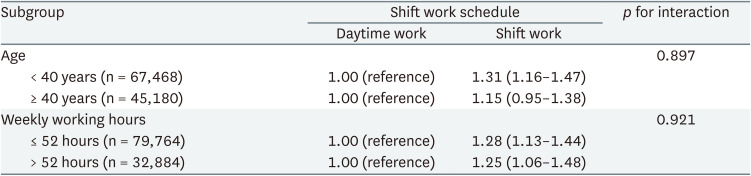
The association between shift work and the risk of incident hypothyroidism is shown in Table 2. In a total of 112,648 participants, there were 6,306 incident cases of hypothyroidism (incidence density, 1.26 per 100 person-years) over 501,237 person-years of the follow-up period (median, 4.74 years; interquartile range, 2.32–6.27). All models showed a significantly higher risk of hypothyroidism in the shift work total group than in the daytime work group. In addition, when categorized according to the different shift schedule types, all models showed a significantly higher risk of hypothyroidism, especially in the fixed night and rotating shift groups. In Model 3, even after adjusting all possible confounders considered in the study, the multivariable-adjusted HR of incident hypothyroidism for the shift work total group that included all shifts compared with the daytime work group was 1.27 (95% CI: 1.15–1.40). For the fixed evening, fixed night, rotating shift, and other shift workers, the multivariable-adjusted HRs (95% CI) were 1.11 (0.76–1.61), 2.18 (1.20–3.93), 1.39 (1.23–1.56), and 1.00 (0.82–1.22), respectively, in Model 3.
Development of hypothyroidism according to the shift work schedule and shift schedule type in study participants
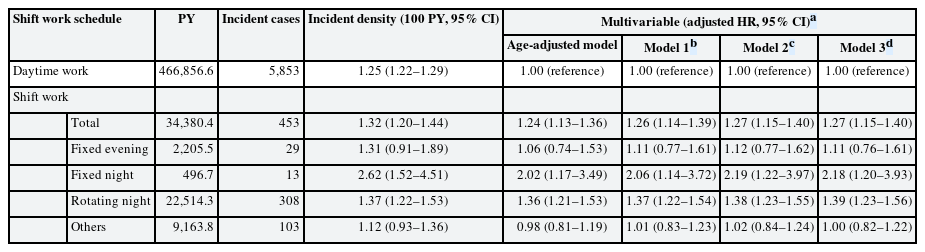
In subgroup analyses, a significant association between shift work and incident hypothyroidism compared with daytime work was shown among participants in all clinically relevant subgroups. The association between shift work and hypothyroidism was more pronounced in younger participants (< 40 years; HR: 1.31; 95% CI: 1.16–1.47). For participants working less than 52 hours, the multivariable-adjusted HR was 1.28 (95% CI: 1.13–1.44) and for those working over 52 hours, it was 1.25 (95% CI: 1.06–1.48). There was no interaction within subgroup analyses (Table 3).
Hazard ratio (95% confidence interval) for hypothyroidism by the shift work schedule in clinically relevant subgroups
Although we could not obtain or present the HRs of female participants as they did not fit the proportional hazard assumption, we could calculate the incidence density value through person-time and incident cases during the observation period in the cohort. As a result, the shift work total group showed a higher incidence of hypothyroidism than the daytime work group, and in detail, the incidence density was high in the order of fixed evening, fixed night, and rotating night (Supplementary Table 1).
DISCUSSION
In this longitudinal study, we compared the incidence of hypothyroidism in the daytime work group and the shift work group with healthy adult men. There was a statistically significant association between shift work and the incidence of hypothyroidism. Even after adjustment, the association was significant, and when divided according to the shift schedule type, the fixed night and rotating shift groups showed a particularly significant association. The fixed night and rotating shift groups may be considered equivalent to the night shift work group, and therefore, this study’s results showed that shift work including nights was more associated with an incidence of hypothyroidism.
Previous studies have investigated the relationship between shift work and thyroid hormonal changes or disease development. In a retrospective study conducted on female workers of a university hospital in Korea, Moon et al.23 suggested that night shift work was associated with increased TSH levels and had a 1.399-fold higher risk of subclinical hypothyroidism compared to non-night shift work. Furthermore, a study on Indian healthcare professionals showed that the mean TSH levels were significantly higher in night shift workers than in day shift workers.24 Magrini et al.,25 in a study carried out in a large teaching Italian hospital, demonstrated a significant increase in subclinical autoimmune hypothyroidism in shift workers than in daytime workers. However, some other studies showed inconsistent results; for example, in a more recent study in an Italian teaching hospital, there were no significant differences in thyroid hormones between rotating night shifts and day workers.26 In this context, a systematic review pointed to the different features of shift work, the “healthy worker” effect, and heterogeneity in the enrolled populations resulting in inconsistent results.20
Although the underlying mechanisms for these effects are not fully understood, we hypothesize that night shifts may cause alterations in sleep patterns and quality that disturb the regular circadian rhythm and result in abnormal TSH secretion. Thyroid function is regulated by the hypothalamic-pituitary-thyroid axis, as hypothalamic thyrotropin-releasing hormone (TRH) stimulates the secretion of TSH, which affects the thyroid gland to synthesize thyroid hormone.27 TSH is regulated by the central circadian pacemaker of the suprachiasmatic nuclei and shows clear circadian rhythmicity under normal sleeping conditions, which increases several hours before sleep, showing the highest concentration in the middle of the night, and then decreases during the remainder of the sleep period until it reaches low daytime levels.1628 Sleep deprivation after the night shift may lead to changes in TSH daily rhythmicity, which can result in an increase in hormone levels in regard to the suppressive effect of sleep on TSH secretion.29 Additionally, previous studies have shown a significantly higher prevalence of subclinical autoimmune hypothyroidism and abnormal anti-thyroperoxidase (TPO) antibody levels in shift workers than in daytime workers, which may activate the autoimmune system, increasing the risk of autoimmune disease.25 Furthermore, irregular eating patterns and late-night snack habits in night shift workers may be related to hormonal changes, including TSH secretion.30
The prevalence of hypothyroidism is known to increase with age.3132 This is related to alterations in thyroid function and the increasing incidence and prevalence of autoimmune thyroiditis with aging.33 Previous studies of thyroid function profiles reported that TSH concentrations increase and free triiodothyronine levels fall with age.34 Additionally, the prevalence of positive anti-TPO and anti-thyroglobulin antibodies increases with aging, contributing to an increase in the prevalence of subclinical hypothyroidism.35 In our subgroup analyses, there was a pronounced relationship between shift work and the incidence of hypothyroidism in those aged 18–39 years. This demonstrates that shift work is a significant risk factor for hypothyroidism, regardless of age-related thyroid dysfunction.
A previous large-scale cohort study at the Kangbuk Samsung Cohort Study reported a significant relationship between the incidence of hypothyroidism and long working hours.36 A meta-analysis investigating the effects of long working hours on occupational health problems suggested the strongest association between long working hours and short sleep duration, which was revealed to be harmful to both physical and psychological health.37 Prolonged psychological stress leads to the hypothalamic-pituitary-adrenal axis activation and dysregulation, inducing imbalanced T3 and T4 thyroid hormones and hypothyroidism.38 In our study, even after adjusting the weekly working hour, there was little difference in the HR for all the shift schedule types. Furthermore, in our subgroup analyses, after dividing the weekly working hours into 52 hours, the maximum statutory working hours per week in Korea, there was no significant difference in the association between shift work and the incidence of hypothyroidism. These results suggest that there is an association between shift work and hypothyroidism regardless of long working hours, which is a risk factor for hypothyroidism.
Women are known to be vulnerable to hypothyroidism.19 A previous study reported that primary hypothyroidism can occur about 8–9 times more frequently in women compared to men.17 However, in our study, since female participants were excluded because they did not fit the proportional hazard assumption, it was difficult to find an association between shift work and hypothyroidism based on sex. Peplonska et al.39 demonstrated that postmenopausal women who work long-term night shifts may have increased estradiol levels. Furthermore, the TSH response to TRH is known to be enhanced by estrogens, and estrogen may have direct actions in thyroid cells by regulating proliferation and function.4041 Therefore, the hormonal alterations related to shift work are more pronounced in women, which may be a significant confounding variable during analyses. Future investigations should additionally consider female hormonal conditions such as menstrual cycles when studying female groups.
There were a few limitations to the present study. First, since the participants responded to the questions on the type of work and several covariates through self-reported questionnaires, the possibility of information bias cannot be ruled out. However, since the participants had no advantages or disadvantages in responding to questions on these variables, misclassification is likely to be non-differential in our findings. Second, the participants’ responses could have indicated different work schedules at each visit. However, approximately 90% of the participants in our study did not alter their responses in terms of categorized shift schedule type during follow-up. Therefore, the bias would not significantly affect the result of this study. Third, we only examined male workers, and it is difficult to generalize the results as it limits the investigation of sex-based differences. Fourth, we did not consider detailed characteristics of work conditions such as duration of employment and possible occupational confounding factors that could be very sensitive to the thyroid. In addition, although this study did not investigate the family history of hypothyroidism, it can be considered in future studies.
Nevertheless, our study has several strengths. First, due to the large sample size of our cohort study, it more clearly indicated the temporality. Additionally, most earlier studies on the relationship between shift work and hypothyroidism were cross-sectional. Second, we further investigated the types of shift work, which included fixed evening shift work, fixed night shift work, rotating shift work, and other shift work. Therefore, it was possible to supplement the shift schedule type that previous studies suggested as a limitation for heterogeneous results. Third, since our study participants were relatively young (mean age = 38.3 years) and healthy, the effects of age-related thyroid dysfunction and underlying diseases could be minimal. Furthermore, by age-specific subgroup analysis, hypothyroidism was shown to have a significant relationship with shift work in relatively young and healthy people. Finally, since hypothyroidism was assessed based on laboratory results rather than a symptom or questionnaire, we could obtain more objective outcomes.
CONCLUSIONS
In conclusion, this large-scale cohort study showed an association between shift work and the incidence of hypothyroidism. Therefore, workplace risk assessment and proper precautions to prevent adverse health impacts, including thyroid disease, are needed for shift workers, especially those who work nights. In addition, since the risk of hypothyroidism was observed to be higher in younger shift workers, further precautions need to be taken. Future investigations should consider more detailed work conditions and possible co-exposures, as well as sex sensitivity. We expect that this study will serve as a basis for future investigations on shift work and thyroid-related health effects.
Notes
Competing interests: The authors declare that they have no competing interests.
Authors contributions:
Conceptualization: Lee W.
Investigation: Kwon S, Lee W, Lee Y, Kim J, Seo E, Kim D, Lee J, Jeong Y.
Methodology: Kwon S, Lee W, Lee Y.
Supervision: Jeong J.
Writing - original draft: Kwon S.
Writing - review & editing: Lee W.
Abbreviations
BMI
body mass index
BP
blood pressure
CI
confidence interval
fT4
free thyroxine
HR
hazard ratio
IRB
Institutional Review Board
PY
person-years
TPO
thyroperoxidase
TRH
thyrotropin-releasing hormone
TSH
thyroid-stimulating hormone
References
SUPPLEMENTARY MATERIAL
Supplementary Table 1
Development of hypothyroidism according to the shift work schedule and shift schedule type in women participants