Occupational stress changes and new-onset depression among male Korean manufacturing workers
Article information
Abstract
Background
Studies on the association between occupational stress and depression have been frequently reported. However, the cross-sectional designs of studies limited insight into causal associations. In this study, we investigated the longitudinal association between occupational stress and new-onset depression among employees in a single manufacturing plant.
Methods
The annual health checkup data of employees at a manufacturing plant in Korea were collected. A total of 1,837 male employees without depression who completed a health checkup during two consecutive years were included. Occupational stress was measured using a short form of the Korea Occupational Stress Scale (KOSS-SF), and depression was assessed using a Patient Health Questionnaire-2. The association between occupational stress change over the two years and newly developed depression was investigated using two logistic regression models.
Results
Across all sub-factors of KOSS-SF, employees who reported increased occupational stress had a higher risk of new-onset depression. Newly developed depression was significantly associated with job demand (odds ratio [OR]: 4.34; 95% confidence interval [CI]: 2.37–7.96), job insecurity (OR: 3.21; 95% CI: 1.89–5.48), occupational climate (OR: 3.18; 95% CI: 1.91–5.31), lack of reward (OR: 2.28; 95% CI: 1.26–4.12), interpersonal conflict (OR: 2.14; 95% CI: 1.18–3.86), insufficient job control (OR: 1.93; 95% CI: 1.05–3.56), and the organizational system (OR: 1.84; 95% CI: 1.01–3.36).
Conclusions
For every sub-factor of the KOSS-SF, occupational stress increase and persistent high stress were associated with the risk of developing new-onset depression. Among the seven sub-factors, job demand had the most significant effect. Our results show that occupational stress should be managed to promote employee mental healthcare.
BACKGROUND
Stress at work, or occupational stress, is an abstract concept that includes all types of work-associated stress which was defined as described by Karasek1 who developed the first systematical model in 1979. Furthermore, the relationship between occupational stress and worker health is a topic that has been studied for decades.2
Depression is one of the most common psychiatric disorders and a leading cause of absence from work in many countries.3 And among working-age adults, depression causes reductions in work productivity and represents an indirect economic burden at the national level.4 Much evidence has been presented that severe occupational stress negatively affects worker physical and mental health, and studies conducted in Korea have produced similar results.567
Work environments are stressful in Korea, which is ranked seventh among OECD countries for low work-life balance.8 To analyze occupational stress, cultural and national characteristics should be considered, and various studies have addressed domestic conditions since the development of the Korean Occupational Stress Scale (KOSS).9 In a large-scale study of Korean employees with a range of occupations, poor occupational climate and insufficient social support were identified as risk factors for depression, and in a study conducted on Korean nurses, job insecurity and lack of reward were found to be closely related to depressive symptoms.1011 However, no prospective cohort study on occupational stress and depression has been published, and relatively few longitudinal studies have been attempted.12
In this study, we investigated the longitudinal relationship between occupational stress and depression using consecutive annual health checkup data of male employees at a manufacturing plant by analyzing the longitudinal effects of occupational stress sub-factors on newly developed depression.
METHODS
Study population
In this study, we used the health checkup data of employees at a manufacturing plant in Korea. A total of 1988 individuals completed health checkups without missing data in 2018 and 2019. After excluding 27 females, 1961 male workers were selected for the study. Since we focused on new-onset depression, 124 employees who had depression (based on Patient Health Questionnaire-2 [PHQ-2]) in the baseline year were excluded, and thus the analysis was conducted on the remaining 1837.
Occupational stress (short form of KOSS [KOSS-SF])
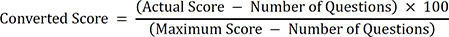
KOSS-SF was used to measure occupational stress.7 The survey questionnaire consisted of 24 self-reported items, which were assessed using a 4-point scale and categorized into 7 sub-factors; job demands, insufficient job control, interpersonal conflict, job insecurity, organizational system, lack of reward, and occupational climate. Each sub-factor was scored using a 100-point scale, where higher numbers indicated higher stress levels.
Depression measures (PHQ-2)
The PHQ-2 is a tool developed in 1999 for screening depression and consists of two items selected from nine PHQ-9 items, namely, how often workers have experienced ‘Little interest or fun at work’ or ‘Feeling depressed or hopeless’ during the previous 2 weeks. Responses were ‘Not at all,’ ‘Several days,’ ‘More than half the days,’ and ‘Nearly every day’ and were rated using a 0–3 scale; thus, total scores ranged from 0–6. Optimum screening cut-off values are debatable, but most studies have used 2 or 3 points.13 A cut-off of 2 points provides higher sensitivity and is more commonly used, but we used a cut-off of 3 points to define depression because of its higher specificity. ‘New-onset depression’ was defined as no depression in the baseline year but depression in the following year.
General characteristics and health behaviors
Previous studies have established that ages, gender, religion, education, income, and marital status are risk factors for depression.14 Due to limitations of the health checkup data used, insufficient information was available. We used information included basically in the health checkup such as ages, smoking status, and alcohol consumption as covariates. Also, we added physical activity because it was recently claimed to affect depression significantly.15 The cut-off value for physical activities was set at 2.5 hours per week in accordance with WHO 2020 guidelines.16
Statistical analysis
The analysis was performed using R for Windows (version 4.2.0 R Foundation for Statistical Computing, Vienna, Austria). Pearson’s χ2 test was used to determine which general characteristics affected new-onset depression, and multiple logistic regression analysis was used to assess the risks posed by these characteristics on new-onset depression after adjusting for potential confounders. It has been proposed that the odds ratio (OR) of a sample provides a good estimate of population relative risk when the outcome is uncommon, typically when the prevalence is under 10%.17
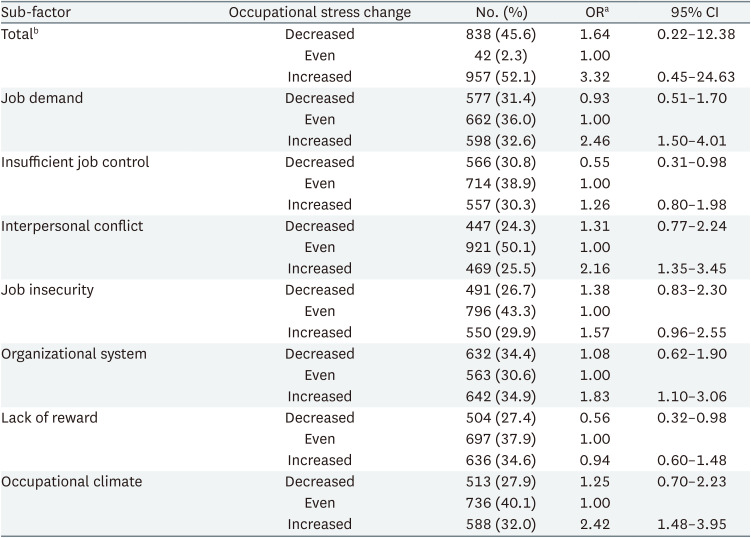
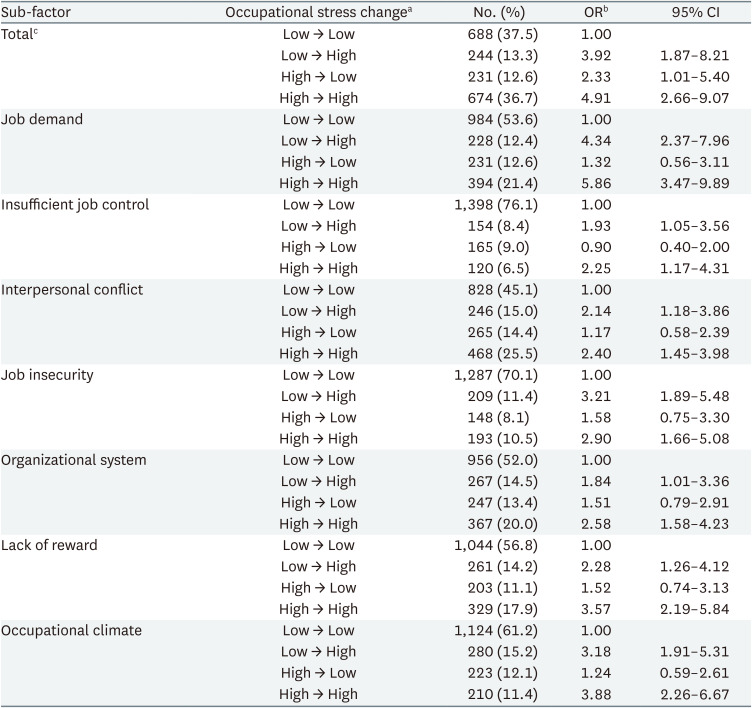
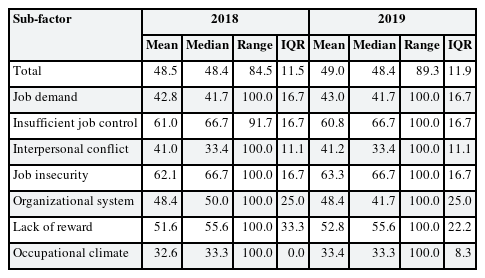
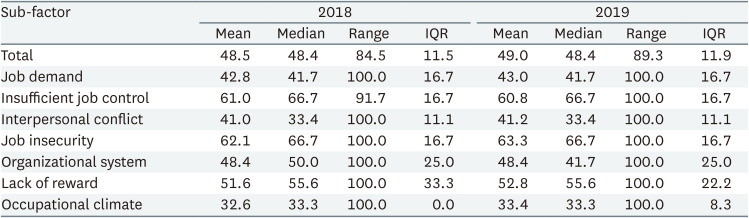
In the first regression model, we classified the scores of the 7 sub-factors of KOSS-SF into 'decreased', 'even', and 'increased' by comparing scores for the first and second years. The odds ratios of decreases and increases were calculated with respect to the even group. In the second model (the modified model), study subjects were re-divided into four high and low occupational stress groups, namely, Low → Low, Low → High, High → Low, or High → High groups, using median scores in the baseline and following year. We calculated and applied the median scores of these study subjects for each sub-factor in order to reflect the specificity of this group (descriptive statistics and median scores are presented in Table 1). We then calculated ORs of new-onset depression for all sub-factors using the Low → Low group as a reference. The null hypothesis of no difference was rejected when p-values were < 0.05.
Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board (IRB) of Inha University Hospital (IRB No. 2023-04-006).
RESULTS
Relations between general characteristics and new-onset depression
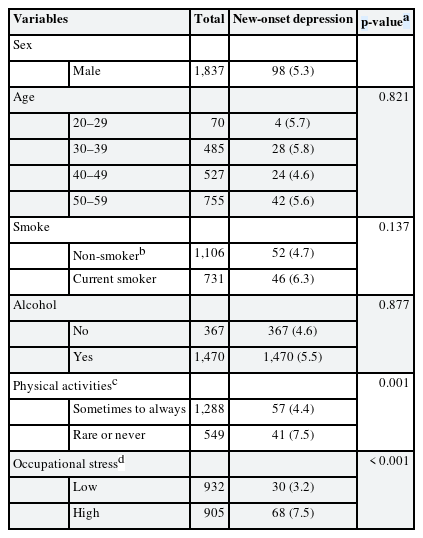
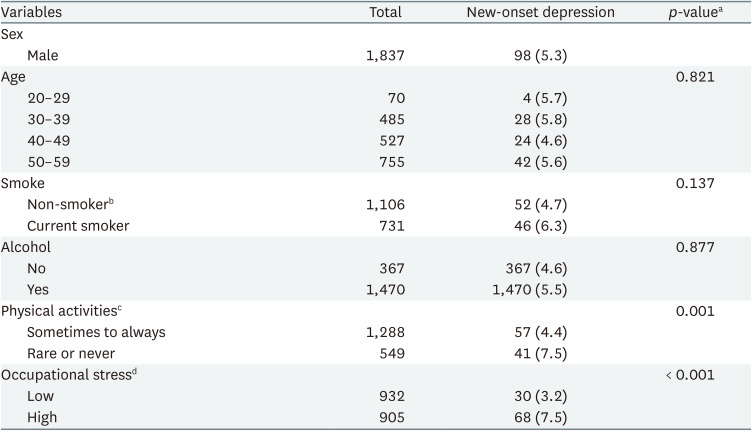
Table 2 presents the general characteristics of participants based on 2018 health checkup data. Of the 1,837 participants, 98 (5.3%) experienced new-onset depression. The p-values of relationships were calculated using the χ2 test for; age, smoking, drinking, and physical activity. Physical activity had a significant effect on new-onset depression, indicating that those who exercised rarely had a higher incidence (7.5%) of new-onset depression than those that exercise adequately (4.4%). Furthermore, analysis of occupational stress total scores showed that employees in the high occupational stress group had a significantly higher incidence of new-onset depression than those in the low occupational stress group (7.5% vs. 3.2%, respectively).
Longitudinal association between occupational stress and new-onset depression
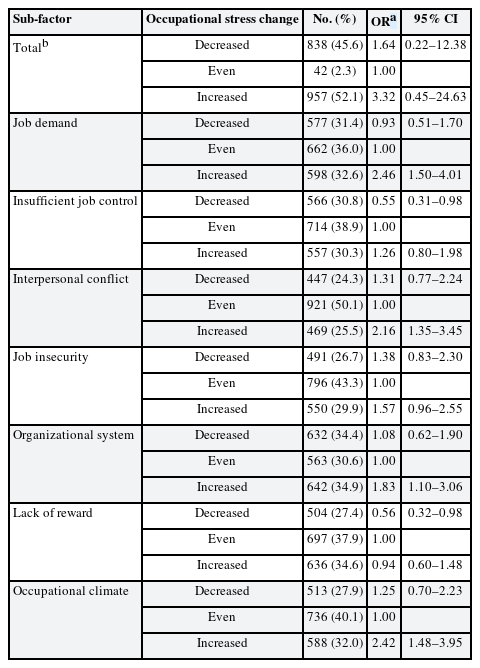
Table 3 shows that the risk of new-onset depression was positively associated with occupational stress scores. For each of the 7 sub-factors, no significant result was obtained for an occupational stress decrease. However, for all increases, ORs were greater than 1, and for job demand (OR: 2.46; 95% confidence interval [CI]: 1.50–4.01), interpersonal conflict (OR: 2.16; 95% CI: 1.35–3.45), organizational system (OR: 1.83; 95% CI: 1.10–3.06), and occupational climate (OR: 2.42; 95% CI: 1.48–3.95) results were significant.
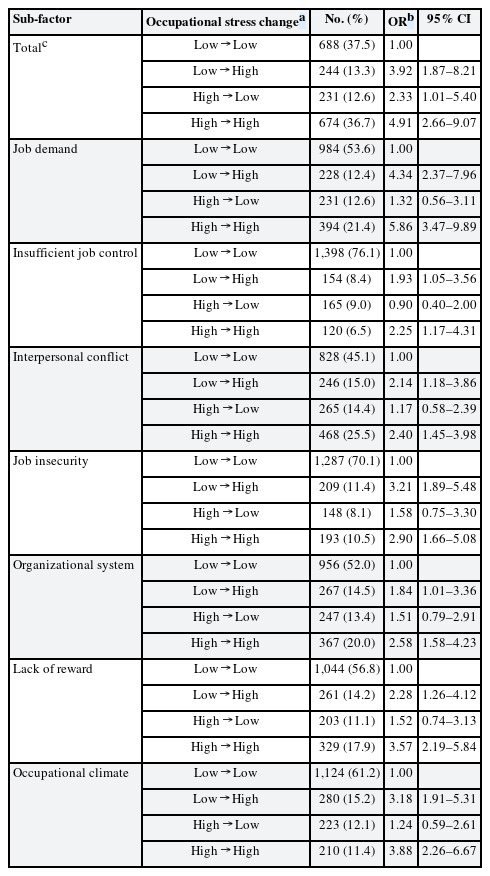
Table 4 shows the results obtained using the second regression model, in which occupational stress changes were compared by dividing scores into low and high categories based on median scores for 2018 and 2019. This modified model provided more significant and consistent results than the first model. For all 7 sub-factors, the ORs of the Low → High and High → High groups were greater than 1, and statistically significant. Sub-factor analysis showed job demand had the highest OR (OR: 4.34; 95% CI: 2.37–7.96), followed by job insecurity (OR: 3.21; 95% CI: 1.89–5.48), occupational climate (OR: 3.18; 95% CI: 1.91–5.31), lack of reward (OR: 2.28; 95% CI: 1.26–4.12), interpersonal conflict (OR: 2.14; 95% CI: 1.18–3.86), insufficient job control (OR: 1.93; 95% CI: 1.05–3.56) and organizational system (OR: 1.84; 95% CI: 1.01–3.36). In addition, we found that for 6 sub-factors, except job insecurity, the ORs of the High → High group were consistently higher than those of the Low → High group, and again, job demand had the highest OR (OR: 5.86; 95% CI: 3.47–9.89) followed by occupational climate (OR: 3.88; 95% CI: 2.26–6.67), lack of reward (OR: 3.57; 95% CI: 2.19–5.84), organizational system (OR: 2.58; 95% CI: 1.58–4.23), interpersonal conflict (OR: 2.40; 95% CI: 1.45–3.98), and insufficient job control (OR: 2.25; 95% CI: 1.17–4.31).
DISCUSSION
This study analyzed the longitudinal effects of occupational stress changes on the incidence of new-onset depression. We found that increased stresses due to job demands, interpersonal conflict, organizational system, and occupational climate were risk factors for new-onset depression. In addition, continued high occupational stress for all sub-factors significantly affected the incidence of new-onset depression.
In the first analysis, we examined the effects of general characteristics suggested in previous studies on new-onset depression. Within our study group, no significant differences were attributed to age, smoking, or drinking, but those that did not exercise regularly had a significantly higher incidence of new-onset depression.14181920 Also, regarding occupational stress, those with higher total stress scores had a higher incidence of new-onset depression, which concurs with previous domestic studies on employees with different occupations.102122
Logistic regression analysis showed that changes in some sub-factors of occupational stress over the year between surveys affected the incidence of new-onset depression. For an occupational stress decrease, only one of the 7 sub-factors (insufficient job control) had a significantly low OR for new-onset depression versus an even stress score. On the other hand, for an occupational stress increase, ORs were significantly higher for the four sub-factors; job demand, interpersonal conflict, organizational system, and occupational climate, which concurs with the results of previous longitudinal studies.2324 This suggests that an increase in occupational stress has a greater effect than a decrease on the development of depression.
A modified model was designed for more detailed analysis based on median group numbers. Occupational stress change was reclassified into 4 groups by dividing stress scores into low and high values at baseline and the following year. The results obtained showed stronger correlations than the first model. For all sub-factors, the OR of depression in the Low → High group was greater than 1 and statistically significant, indicating that the Low → High group contained individuals whose occupational stress increased to a greater extent.
Another notable result was the higher incidence of new-onset depression observed in the High → High group. The ORs of all sub-factors were significant and even higher than in the Low → High group, except for job insecurity. This suggests that even if a change in occupational stress is insignificant, those who continuously experience high stress are at greater risk of developing depression. Conversely, it was suggested in a previous study, which used a similar model, that the risk of new-onset depression is slightly higher when job strain, as assessed using Karasek's Job Content Questionnaire, increases from a low to a high level than when job strain persists at a high level.25 These conflicting results were probably caused by the use of different occupational stress measurement methods and follow-up periods.
In both models, the sub-factor with the highest risk of new-onset depression was job demand. This factor measures job strain and includes time pressure, responsibility, job overload, and job versatility. As defined by Karasek,1 job demand has been consistently considered an important contributor to occupational stress. In a longitudinal study conducted on 3,735 Canadian workers, the risk of new-onset depression was investigated over 2 years using components of Karasek's Job-Content Questionnaire. Job demand was found to increase the risk of new-onset depression significantly, whereas an increase in job control had no significant effect.26 This suggests that our finding that job demand was the most significant sub-factor concurs with the findings of similar studies conducted in Western countries.
On the other hand, the “occupational climate” factor, which had the second highest OR, is believed to reflect Korean culture, which commonly features lack of a rational communication system and groupism (dining out as a group or drinking together). In addition, a cross-sectional study conducted in Korea on the relationship between depressive symptoms and occupational stress found that the occupational climate was the greatest risk factor of depression among male employees and the second highest among female employees.21 We believe that if management pays attention to this finding, improvements can be achieved in workplace atmosphere that would positively influence employee mental health.
In addition, the “Lack of rewards” factor had an impressively high OR. First proposed by Siegrist27 in 1996, the effort-reward imbalance model emphasizes that individual reward significantly affects health. A study conducted among workers from a single press company showed that low rewards were associated with a higher risk of depressive symptoms among male than female workers.28 This gender-associated difference can be interpreted in terms of the male role as the main contributor to family income. A similar tendency was observed in the present study, which was conducted on male workers.
The strength of this study is that it was performed using the data of almost 2,000 employees in the same plant. Normally, survey response rates of longitudinal studies are poor, but the use of data from mandatory annual health checkups in the present study resulted in a high response rate. In addition, we analyzed the effects of various sub-factors of occupational stress as defined by KOSS-SF, which reflects domestic workplace environments.
Nevertheless, the study has several limitations. First, the PHQ-2 contains fewer questions than other evaluation tools, which suggests it is less accurate. Furthermore, self-reporting bias cannot be excluded because psychiatrist-based diagnoses were not considered. Second, we did not consider changes in control variables such as smoking or alcohol use, over the one-year study period. Also, due to health checkup data limitations, we were unable to access information on other previously identified risk factors such as education level, marriage status, medical history, working hours, or work functions, which may have affected our results. Third, participants in this study worked at a single manufacturing plant and were possibly exposed to similar occupational stresses, which introduces the risk of confirmation bias if our findings are applied to other groups. Finally, a one-year follow-up may have been too short to observe the development of new-onset depression. Further longitudinal studies are required to determine the long-term impacts of occupational stress.
CONCLUSIONS
We investigated how changes in occupational stress affect the development of new-onset depression among employees. Our results suggest that occupational stress and a persistently high level of occupational stress increase the risk of depression. Therefore, we stress the importance of managing occupational stress to promote the mental health of employees.
Notes
Competing interests: The authors declare that they have no competing interests.
Author contributions:
Conceptualization: Kim J, Kim HC.
Data curation: Kim HC, Kim J, Yang SC.
Formal analysis: Kim J.
Investigation: Kim J, Kim M, Yang SC.
Supervision: Kim HC, Leem JH, Lee DW.
Writing - original draft: Kim J.
Writing - review & editing: Kim HC, Park SG, Lee DW.
Abbreviations
CI
confidence interval
IRB
Institutional Review Board
KOSS
Korea Occupational Stress Scale
KOSS-SF
a short form of the Korea Occupational Stress Scale
OR
odds ratio
PHQ-2
Patient Health Questionnaire-2

 ) were divided into low and high median scores.
) were divided into low and high median scores.