Associations of chronotype and insomnia with menstrual problems in newly employed nurses at university hospitals in the Republic of Korea
Article information
Abstract
Background
Dysmenorrhea and menstrual cycle changes occur in women working shifts. Circadian rhythm disruption and sleep disturbances associated with shift work leads to health problems. We identified chronotypes and the occurrence of insomnia among newly employed university hospital nurses and investigated the association of these factors with menstrual problems.
Methods
We conducted pre-placement health examinations for shift workers using self-reported questionnaires between 2018 and 2020. A total of 463 nurses were included in the study. Sociodemographic data, shift work experience, and information on insomnia were collected from health examination data. In addition, details regarding chronotype, dysmenorrhea, irregular and abnormal menstrual cycles, amenorrhea, and contraceptive use were obtained from the questionnaire. Multiple logistic regression analysis was performed to study the association between chronotype, insomnia, and menstrual problems after controlling for age, body mass index, contraceptive use, amenorrhea, and prior shift work.
Results
The prevalence rates of dysmenorrhea, irregular menstrual cycles, and longer menstrual cycles were 23.8%, 14.9%, and 4.1%, respectively. The risk of dysmenorrhea increased in the evening-type (odds ratio [OR]: 3.209; 95% confidence interval [CI]: 1.685–6.113) and those with insomnia (OR: 1.871; 95% CI: 1.074–3.261). Additionally, the risk of an irregular menstrual cycle (OR: 2.698; 95% CI: 1.167–6.237) increased in the evening-type, and the risk of a longer menstrual cycle (OR: 4.008; 95% CI: 1.354–11.864) increased in individuals with insomnia.
Conclusions
Our findings suggest that dysmenorrhea is promoted in the evening-type and insomnia individuals. There may be an increased risk of irregular menstrual cycles among evening-type nurses and an increased risk of longer menstrual cycles among those with insomnia. Therefore, factors such as evening-type and insomnia should be considered for the prevention of menstrual problems in women performing shift work.
BACKGROUND
Health problems among nurses are directly related to patient safety. Therefore, managing health problems is a high priority to ensure optimal public health outcomes. Nurses who perform shift work may also experience chronic health problems. The adverse health effects of shift work may be mediated by behavioral mechanisms such as altered light exposure, diet, and sleep patterns. Altered light exposure, such as light at night and darkness during the day, could change hormones regulated by light and sleep (for example, prolactin, cortisol, and melatonin). Altered sleep patterns, such as short day sleeps and early wake times can disturb sleep. Shift work also increases risk behaviors and psychosocial stress. These factors cause physiological effects such as neuroendocrine stress, cardiac metabolic stress, altered immune function, cellular stress, and psychological effects such as cognitive impairment.1 As a result, shift work increases nurses’ risk of developing chronic diseases and falling victim to medical accidents.2
Circadian rhythm refers to the 24-hour internal clock in the brain that regulates cycles of alertness and sleepiness by responding to light changes in the environment.3 The chronotype is the expression of an individual’s circadian rhythm, which is generally characterized by one’s preference for activities at a particular time during a 24-hour cycle.4 For example, the morning-type prefers to sleep at night, wake up early, and become active in the morning, whereas the evening-type prefers the opposite.5
It is known that the determination of chronotype was mainly influenced by unchanging factors like age, sex, and polygenetic variation.6 It could be also influenced by environmental factors such as shift work. There is a view that health problems such as insomnia may occur when individual circadian rhythms are inconsistent with the social schedule.7 Chronotype shows variability, but the mechanism and extent are not yet clear.
Sleep disturbances include disorders of excessive somnolence; disorders of the sleep-wake schedule; dysfunctions associated with sleep, sleep stages, partial arousals; and insomnia.8 Regarding the relationship between chronotype and sleep, there are theories that chronotype contributes to sleep time and duration,7 and the theory that sleep characteristics are well explained by polygenetic factors including chronotype genes.9
Important health issues affecting nurses who perform shift work are dysmenorrhea and changes in menstrual cycles.10 Dysmenorrhea is defined as a painful cramp of uterine origin that occurs during menstruation.11 The menstrual cycle is an essential life rhythm governed by the interaction of sex hormone levels and promotes stability through a feedback mechanism involving circadian rhythm and sleep,12 and menstrual problems are not only important indicators of female reproductive health but are also significant factors affecting quality of life.131415
Dysmenorrhea is a debilitating condition observed in many women that can result in reduced productivity16 and increased visits to medical institutions.15 Menstrual cycle changes are associated with gynecological diseases, including infertility.17 Furthermore, menstrual cycle changes increase the risk of severe health problems, such as breast cancer,18 type 2 diabetes,19 cardiovascular disease,20 and premature mortality.21 Circadian rhythm and sleep are associated with menstrual problems. Although there have been reports of an increased risk of dysmenorrhea in the evening-type,2223 these findings were not sufficient to establish a relationship between circadian rhythm and dysmenorrhea. The results of several studies suggest an association between sleep disturbances and menstrual problems in the general population.2425 In the case of shift work, previous studies have shown increased dysmenorrhea and changes in the amount of menstruation.2627 However, few studies have examined the direct relationship between sleep disturbance and menstrual problems in female workers.
Although previous studies have suggested that menstrual cycle changes may be affected by circadian rhythms, the statistical significance of this association has been mixed.2829 For example, in a previous study, the evening-type had a longer menstrual cycle than others, and the morning-type had a shorter duration of menstrual bleeding.28 Therefore, it is necessary to further evaluate the association between circadian rhythms and menstrual cycle. Studies have reported an association between menstrual cycle irregularity and sleep disturbances such as short sleep duration25 and insomnia symptoms.24 Based on these findings, we further assessed the association between insomnia and abnormalities in menstrual cycle duration.
In this study, we aimed to identify the prevalence of menstrual problems and related factors, such as chronotype and insomnia, among nurses who were newly employed in hospitals. We also explored the relationship between these factors and menstrual problems such as dysmenorrhea and irregular menstrual cycles.
METHODS
Study population
The study population was newly employed at 2 university hospitals in Seoul, Korea. They underwent a pre-placement health examination and completed a self-reported questionnaire. Also, they underwent health checks before being assigned to shift work from March 1, 2018 to October 31, 2020. They had never worked shifts at the 2 university hospitals. However, some had experience working shifts at their previous hospitals, while the rest just graduated from nursing school and got their first jobs.
Of the 537 participants who completed the questionnaire, 463 were included in the final analysis. First, 18 people without body mass index (BMI) information were removed from the health examination data. Twenty-nine male workers were excluded because menstrual problems could not be assessed. Participants who reported that they had not menstruated in the past year were also excluded. Among the remaining 489 patients, 14 patients with irregular bleeding, who had less than 9 menstrual periods for 1 year in the menstrual questionnaire, were excluded as secondary causes could be suspected. Among the 475 patients, those without Dysmenorrhea score (n = 1) or circadian rhythm information (n = 12) were also excluded.
Study variables
Independent variables
To confirm the circadian rhythm type, the Korean Translation of the Composite Scale (KtCS), a structured measurement tool, was included in the questionnaire to evaluate the preferred times for various activities. There are 13 items in the KtCS; 3 items are scored on a 1–5-point scale, and the remaining ten items on a 1–4-point scale. The total score ranged from 13 to 55 points. A lower score indicated evening-type with a high preference for evening activities, and a higher score indicated morning-type with a greater morning preference.30 Referring to previous studies, a total score of ≤ 24 points (below the 10th percentile) was defined as the evening-type, and a total score of > 37 points (exceeding the 90th percentile) as the morning-type. The remaining score ranges were intermediate types.5 As mentioned above, the evening-type is related to dysmenorrhea2223 and menstrual cycle changes28; hence, we divided the chronotypes into the evening-type and non-evening-type (morning-type or intermediate-type). The points of participants who answered more than 80% of the question items in the questionnaire were corrected by converting the ratio.31 Four hundred forty-seven nurses responded to 100% of the KtCS questionnaire, 16 nurses whose KtCS score was corrected by ratio conversion because they responded between 80%–100%, and 12 were excluded because they responded less than 80%. The 12 nurses excluded from the study showed no significant differences in demographic characteristics compared with the nurses included in the analysis.
To evaluate insomnia, the Insomnia Severity Index, developed by Morin that includes a preplacement health examination, was applied.32 Seven items related to insomnia were used (severity of sleep onset, sleep maintenance, early morning awakening problems, sleep dissatisfaction, interference of sleep difficulties with daytime functioning, noticeability of sleep problems by others, and distress caused by sleep difficulties). Scores are added from 0 on a 4-point scale, and the distribution ranges from 0 to 28, with higher scores indicating severe insomnia. This study classified insomnia as a score of 8.
Dependent variables
Dysmenorrhea was defined as the pain intensity of menstruation for the past year measured on a numerical pain intensity scale of 0–10, and the top 25% score was 7 points (interquartile range 4–7 points). A score of < 7 and ≥ 7 was classified as absence and presence of dysmenorrhea, respectively. To evaluate the menstrual cycle, the question “What was your menstrual cycle over the past year?” was answered using the following 6 options: within 21 days, 21–25 days, 26–31 days, 32–39 days, ≥ 40 days, and irregular.21 Only those who answered “irregular” were defined as having an irregular menstrual cycle. A shorter menstrual cycle was defined as a menstrual period of < 21 days, and a longer menstrual cycle was defined as a menstrual period of > 40 days.19
Confounding variables
Shift work experience, age, BMI, smoking, alcohol consumption, exercise, and alcohol consumption were identified using preplacement health examination data. Prior shift work experience information was obtained in units of months from doctor’s history taken during pre-placement health examinations for shift workers. If the past shift work history was 0 month, it was classified as “never,” and if it was more than 1 month, it was classified as “ever.” According to World Health Organization standards, alcohol consumption is classified as non-drinker, moderate drinker (within 20 g of alcohol per time for women, drinking less than once a week), and risky drinkers. The degree of physical activity was classified as low, moderate, or high according to the Korean version of the International Physical Activity Questionnaire, a measurement tool for health checkups of the National Health Insurance.33
The questionnaire identified contraception and amenorrhea experiences over the past year. Participants answered “yes” or “no” to the questions “Have you used contraception in the past year?” and “Have you not had menstruation for more than 90 days in the past year?”
Statistical analysis
All statistical analyses were performed using Statistical Package for the Social Sciences 22.0 (IBM SPSS: IBM SPSS version 22.0; IBM Corp., Armonk, NY, USA). Nurses were categorized as having a chronotype or insomnia. For basic comparisons of categorical variables, sociodemographic characteristics and the prevalence of menstrual problems were examined using χ2 tests, except for shift work experience, contraception, and amenorrhea; these thresholds were evaluated using Fisher’s exact test. Multiple logistic regression analysis was performed to evaluate the association between chronotype and insomnia and 3 menstrual problems: dysmenorrhea, irregular menstrual cycles, and abnormal menstrual cycles. Age, BMI, contraceptive experience in the past year, amenorrhea experience in the past year, and prior shift work experience were selected as confounding variables by reviewing previous studies on risk factors for dysmenorrhea34 and menstrual cycle.35 Multiple logistic regression analyses were performed on 420 nurses, excluding those with amenorrhea, to identify risk factors for menstrual irregularity and on 373 nurses without menstrual irregularity to identify risk factors for menstrual cycle abnormalities. The confounders included in these models were the aforementioned variables, with the exception of amenorrhea.
Ethics statement
This study was approved by the Institutional Review Board (IRB 2018-05-017-021) of the Ewha Womans University Mokdong Hospital and conducted in accordance with the Declaration of Helsinki of the World Medical Association. The study protocol was explained to the participants who provided written informed consent. Participants voluntarily agreed to complete the questionnaire.
RESULTS
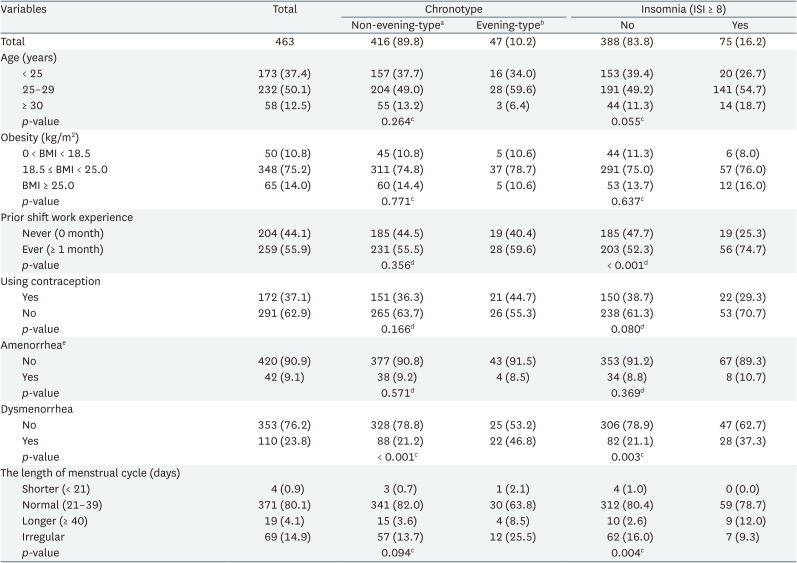
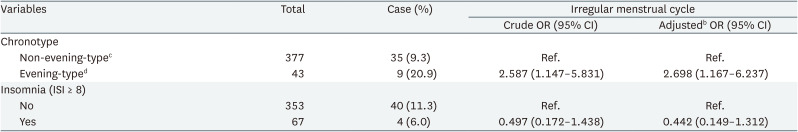
The general characteristics of the study participants are summarized in Table 1. Of the 463 nurses, 16.2% reported having insomnia. Participants were aged < 25 years (37.4%), 25–29 years (50.1%), and > 30 years (12.5%). According to BMI, 10.8% had a BMI below 18.5, 75.2% had a BMI between 18.5 and 24.9, and 14.0% had a BMI > 30. There were 55.9% nurses with prior shift work experience and 23.8% with dysmenorrhea. Regarding the length of the menstrual cycle, the proportion of shorter cycles (< 21 days) was 0.9%, longer cycles (≥ 40 days) was 4.1%, and irregular menstrual cycles was 14.9%. The proportion of nurses with dysmenorrhea was higher in the evening-type group (p < 0.001). The proportion of nurses with prior shift work experience (p < 0.001), dysmenorrhea (p = 0.003), and late periods (p = 0.004) was higher in the insomnia group than in the non-insomnia group. In the 2 groups divided by evening-type, the proportions of general characteristics were not significantly different, except for dysmenorrhea. There were no statistically significant differences in age, obesity, contraceptive use, or amenorrhea between the nurses with and without insomnia.
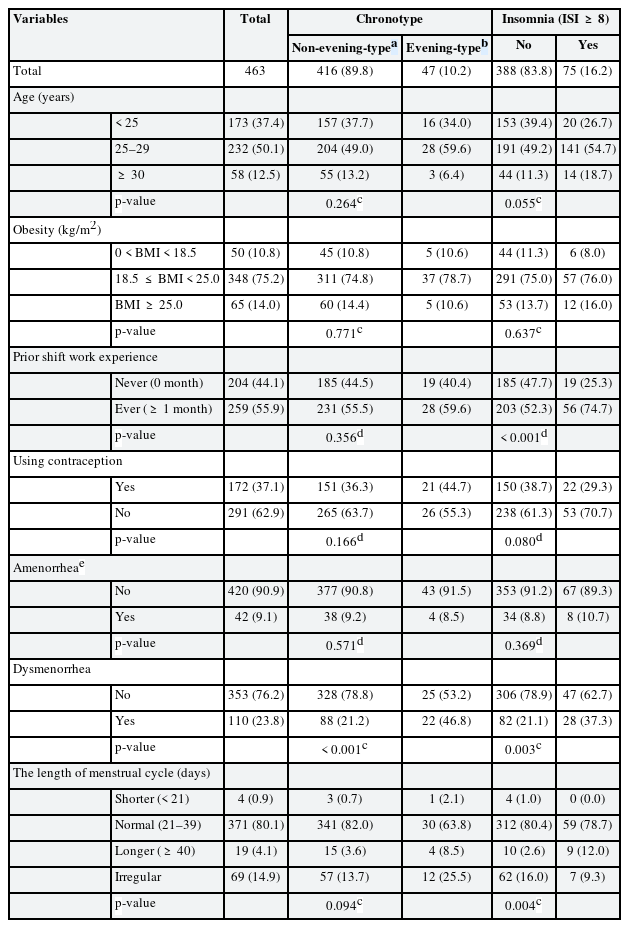
Prevalence of the study population according to chronotype and insomnia among 463 newly employed nurses
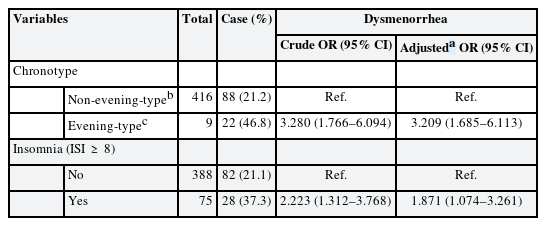
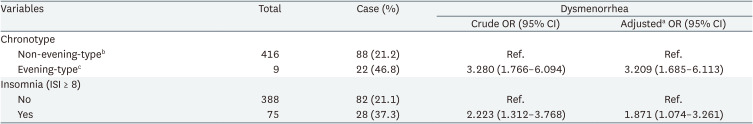
The associations between dysmenorrhea, insomnia symptoms, and circadian rhythms are shown in Table 2. Age, contraceptive experience, and BMI, which are the individual risk factors related to dysmenorrhea34 and menstrual cycle,35 were adjusted. In addition, prior shift work experience, which may affect the occurrence of insomnia symptoms and circadian rhythms, was corrected.22 The risk of dysmenorrhea was higher in the evening group (odds ratio [OR]: 3.209; 95% confidence interval [CI]: 1.685–6.113). The risk of dysmenorrhea was 1.871 times (95% CI: 1.685–6.113) higher in the group with insomnia symptoms than in the group without insomnia.
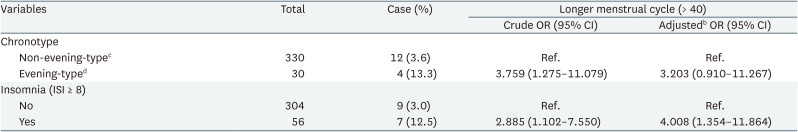
The occurrence of irregular menstrual cycles was analyzed, except for individuals suspected of having amenorrhea (Table 3) for whom the menstrual cycle could not be evaluated. We adjusted for confounding variables such as age, BMI, previous year’s contraceptive experience, and prior shift work experience. We then analyzed irregular menstrual cycles in 420 nurses and found that in the evening-type, the risk of irregular menstrual cycles was 2.698 times (95% CI: 1.167–6.237) higher than that in other groups.
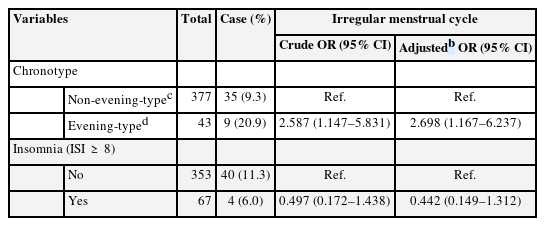
Association of chronotype and insomnia with irregular menstrual cycle among 420a newly employed nurses without amenorrhea
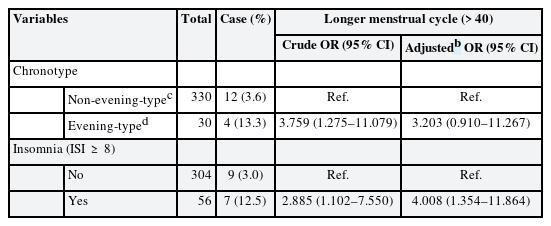
As shown in Table 4, 87 patients with unusual amenorrhea or irregular menstrual cycles were excluded. The remaining 376 nurses who had regular cycles were analyzed for abnormalities. For insomnia, the risk of a longer cycle was 4.008 times higher (95% CI: 1.354–11.864) than that of the other groups.
DISCUSSION
After controlling for age, BMI, contraceptive use, and prior shift work experience, we found that the risk of dysmenorrhea was associated with insomnia symptoms and evening-type. Additionally, an increased risk of an irregular menstrual cycle was independently associated with the evening-type, and an increased risk of an abnormal menstrual cycle > 40 days was independently associated with insomnia.
Two cross-sectional studies have reported an association between circadian rhythm and dysmenorrhea. These studies consistently showed that there was more dysmenorrhea in the evening-type than in other chronotypes.2336 A possible explanation for the increased risk of dysmenorrhea in the evening-type was sleep disruption.3738 The altered sleep timing of the evening-type might be related to the disruption of the 24-hour clock, which is key to reproductive hormone regulation. This suggestion does not support our findings as circadian rhythms are not independently associated with the risk of dysmenorrhea. Another possible explanation was that evening-type used psychoactive substances more frequently.3940 However, a cross-sectional study conducted on female students in Japan reported contrasting findings. In this study, students who frequently experienced dysmenorrhea had more evening-type dysmenorrhea than those who did not. They speculated that the threshold of menstrual pain could be lowered through depressive mood symptoms in the evening-type.
The finding that insomnia was independently associated with the risk of dysmenorrhea is consistent with those of several studies. Among related factors, reduced melatonin levels might explain both insomnia- and evening-type symptoms. Insomnia and evening-type conditions commonly interfere with adequate sleep at night.41 In insomnia and evening-type insomnia, melatonin synthesized in the body by the stimulation of darkness42 may be present at a low concentration. Animal experiments have shown that melatonin inhibits uterine contractions and exerts analgesic effects.43 Additionally, plasma melatonin levels increase during menstruation.44 If melatonin secretion, which contributes to the control of dysmenorrhea, was reduced, it might have affected dysmenorrhea. Other factors include the perturbed actions of several hormones such as estrogen, progesterone, prolactin, and growth hormones.45 In addition, many theories have traditionally reported that insomnia results from dysmenorrhea.38464748
In this study, the risk of an irregular menstrual cycle and abnormal cycle (≥ 40) increased in the evening-type; however, the finding of abnormal cycle was not statistically significant. These results suggest that menstrual cycle-related problems tend to increase in the evening-type. Several studies have supported the association between the evening-type and these problems. They obtained mixed results for irregular49 and abnormal cycles. These results can be explained by differences in reproductive hormones, an increase in melatonin due to sleep debt, and weak zeitgeber effects.
First, 2 cross-sectional studies supported the differences in reproductive hormone levels. In one study, the menstrual cycle was one day longer in the evening than in the morning. In contrast, the luteinizing hormone (LH) peak appeared one day later. If the circadian rhythm changes, mutations can occur in circadian clock genes. Alternatively, the central and peripheral oscillators are not synchronized. This may affect the regulation of reproductive hormones in ovaries and uterus. Second, we hypothesized that an imbalance in melatonin causes changes like sleep debt in the evening-type menstrual cycle. Increased daytime sleep and decreased darkness in the evening can cause an imbalance in melatonin levels.50 One study focused on the fact that an imbalance in melatonin can suppress the secretion of gonadotropin-releasing hormones and affect ovulation. In a study in which reproductive hormones were measured during the day and night depending on the season, nighttime serum melatonin in the follicular phase increased significantly in winter compared with that in summer. Nighttime serum LH levels were higher in summer than in winter. This could affect fertility by regulating LH secretion based on the melatonin levels.51 Finally, weak zeitgebers, which could cause problems in the evening-type menstrual cycle, refer to the weakening of the signal strength that transmits 24-hour changes to the human body in the external environment. The evening-type can be in a state of weak zeitgeber, with longer artificial light exposure during the night and shorter sunlight exposure during the day. A related clinical study reported that in weak zeitgebers, an additional delay in the circadian rhythm could occur, which could increase the effect of melatonin.52
Finally, our findings demonstrated the potential involvement of insomnia in long menstrual cycles. Additionally, although not statistically significant, the risk of irregular cycles reduced in the presence of insomnia. These conflicting results seem to have reduced the statistical stability because the number of cases of insomnia and irregular or long cycles was less than 1% in our study population. Although a few studies have examined the association between insomnia and long cycles, some studies have reported an association between insomnia and irregular cycles. In a 12-month follow-up study, after adjusting for confounding variables, the probability of a new irregular cycle increased compared to those without insomnia at baseline.53 Insomnia causes estradiol levels to remain elevated,5455 and LH pulse frequency is associated with wakefulness.56 The desynchronization of reproductive hormones associated with ovulation may result in sleep disturbances. Hormonal asynchrony related to successful ovulation can be caused by sleep disturbance.
From the above results, it can be seen that chronotype and insomnia are independently related to menstrual health problems. As mentioned in the introduction, it is known that chronotype can affect sleep time and sleep duration, so the interaction between chronotype and insomnia was examined in multiple logistic regression analysis. Although not presented in the result, no statistically significant interaction between chronotype and insomnia was observed for any of the 3 menstrual problems.
This study had several limitations that should be considered when interpreting our findings. First, our study was cross-sectional; hence, causal relationships could not be determined. However, chronotypes are determined by unchanging characteristics, such as genes and age.6 Nurses with secondary causes of menstrual problems were also excluded. We believe that chronotypes are more likely to precede menstrual disorders. Longitudinal data will be helpful in examining the associations between chronotype, insomnia, dysmenorrhea, and menstrual cycle.
Second, variables such as chronotype, insomnia, and menstrual problems were measured using self-report questionnaires. Self-reported data are susceptible to recall bias or denial of problem. Measurement tools for chronotype5 and insomnia32 have been validated in several studies. Menstrual problems are less likely to be affected by recall bias because menarche problems may occur monthly.57 Studies that have reported menstrual problems have mainly used self-reports, whereas studies using hormone measurements are rare.
Finally, although randomized sampling was used to ensure the representativeness of all nurses working at a tertiary hospital, our study findings might not be generalizable. Because the sample size was large, the effect of the selection bias was thought to be less significant.
There have been studies that analyzed the relationship between chronotype and insomnia,5859 or insomnia and specific menstrual problem such as dymenorrhea37 and menstrual cycles.53545556 But few studies had analyzed the relationship between chronotype, insomnia, and menstrual problems such as dysmenorrhea or menstrual cycle together. Our study population is a random sample extracted from newly employed nurses in a university hospital, so it is difficult to generalize it to working women. It might be possible to apply our result to young nurses similar to our study population. In terms of occupational medicine, it is important to establish measures to protect workers with vulnerable characteristics from health problems related to hazards that workers might be exposed to. Therefore our research results can contribute to protecting these workers.
CONCLUSIONS
Our study found that the risk of dysmenorrhea increased among nurses who were of evening-type or had insomnia. The risk of irregular menstrual cycles increased in the evening-type, and the risk of a longer cycle was higher in those with insomnia. Since this study is a cross-sectional study, it is not possible to establish a causal relationship. However, the association between chronotype, insomnia and menstrual problems observed in our study may provide a hypothesis when designing studies on menstrual problems in nurses.
Acknowledgements
The authors thank the staff of the Ewha Medical Examination Center of Ewha Womans University Mokdong Hospital for their assistance in this study.
Notes
Funding: This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (grant number: 2018R1A2B6004110).
Competing interests: The authors declare that they have no competing interests.
Authors contributions:
Conceptualization: Jung HN, Kim H.
Data curation: Jung HN, Ryu J.
Formal analysis: Jung HN, Suh D, Kim H.
Funding acquisition: Kim H.
Investigation: Jung HN, Kim H.
Writing - original draft: Jung HN, Kim H.
Writing - review & editing: Jung HN, Suh D, Ryu J, Jeong WC, Kim YM, Yoon S, Kim H.
Abbreviations
BMI
body mass index
CI
confidence interval
ISI
Korean version of the Insomnia Severity Index
KtCS
Korean Translation of the Composite Scale
LH
luteinizing hormone
OR
odds ratio