Association between sleep quality and type of shift work in Korean firefighters
Article information
Abstract
Background
Shift work that interferes with normal sleep patterns, is known to be a cause of sleep disturbance and has been studied through various occupational groups. However, it is not known which shift type is better for sleep health.
Methods
This study included 568 firefighters. Sleep quality was evaluated using Pittsburgh Sleep Quality Index. Sleep quality was categorized into 2 groups; good quality (≤ 5 points) and poor quality (≥ 6 points). Demographic variables, depression, anxiety, type of shift, and job were collected by self-reported questionnaires. The χ2 test, t-test, and multiple logistic regression analysis were used to evaluate the effect of shift type on the sleep quality of firefighters.
Results
Three hundred thirty-seven firefighters (59.3%) have poor sleep quality. Compared to day workers, the odds ratios (ORs) of poor sleep quality were 2.169 (95% confidence interval: 1.137–4.134) in 6-day cycle, 2.161 (1.150–4.062) in 9-day cycle, 1.805 (1.087–2.997) in 21-day cycle, and 1.485 (0.718–3.069) in 3-day cycle. The ORs of poor sleep quality were 1.697(1.021–2.823) in fire suppression and 2.325 (1.213–4.455) in emergency medical service compared to administration.
Conclusions
All shift work type except for the 3-day cycle was associated with poor sleep quality compared to day work.
BACKGROUND
Sleep is an essential physiological process for functional recovery. Poor sleep affects many health problems including hypertension, diabetes mellitus, mental disorder, cancer, and mortality.12345 There are several risk factors for sleep disturbance including older age, anxiety, depression, pain, obesity, and caffeine intake.678 Occupational factors related to sleep disturbance include shift work, job stress, noise, high temperature, and low temperature.910
There are many studies on the association between shift work and sleep disorder/disturbance.11121314 In the United States, the prevalence of sleep disorders in shift work including the night shift was about 10% in 2004.15 In South Korea, according to an analysis of the 2nd Korean Working conditions Survey, shift workers had a higher risk of sleep disturbance than the day shift.10 Night work had a significant effect on sleep disorder. People with shift work experience have usually poor sleep quality compared to day workers. In electronics production workers, the risk of insomnia in shift workers was higher compared to day workers.16
Firefighters are a typical occupation that works in shifts. There were previous studies on shift work and sleep disorders in firefighters. According to a study of Korean male firefighters, the prevalence of sleep disorders was 51.6% in shift workers.17 Depending on the definition of sleep disorder, several studies have reported sleep abnormalities from 26.9% to 73% in firefighters. Factors affecting sleep disturbance related to firefighters were shift work, the number of interruptions at night during work, second job, and type of job.18192021 However, there is very little research about the type of shift in firefighters. Although some studies showed differences depending on the type of shift work, they cannot be applied because shift work patterns differ from country to country.1922 In Addition, a fast rotation shift that changes every 2–3 days or a slow rotation shift that changes every 3–4 weeks are usually recommended for shift workers.232425 Some studies reported that the night shift was better for sleep health.2627 The 9-day cycle and 21-day cycle in firefighters are neither fast nor slow rotation shifts. The purpose of our study is to figure out which environment will provide more appropriate sleep health and to determine which type of shift work is suitable for the quality of sleep of firefighters.
METHODS
Study subjects
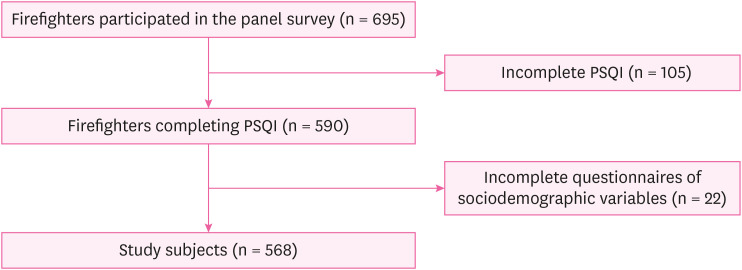
This study used data from the SLEep Panel Study (SLEPS), which was created to study the sleep problems of Korean firefighters.28 The questionnaire for the panel study was conducted as a self-report questionnaire. We conducted the first survey from 2017 October to 2019 October, 695 participated in this panel study, however, this study excluded subjects who could not complete the sleep quality questionnaire (n = 105) or lacked the general characteristics and job-related factors including shift work, type of job, type of shift (n = 22). Finally, 568 participants were included as subjects of this study (Fig. 1).
Questionnaire variable for analysis
This study used a structured and self-report questionnaire. Data in the questionnaire included sociodemographic characteristics such as sex, age, height, weight, education, marital status, monthly income, smoking, drinking, exercise, and sleeping pills. Age groups were classified as 20–29, 30–39, 40–49, and ≥ 50 years old. Body mass index (BMI) was calculated as weight divided by height squared. Obesity was classified by BMI ≥ 25 kg/m2. Education was classified into 3 groups: high school graduation and below, university, and above. The monthly income was divided into 3 categories such as 2,000–2,999, 3,000–4,999, and ≥ 5,000. It was assumed that 1,000 Korean Won equals 1 United States Dollar. Smoking was classified as current smoker, ex-smoker, and non-smoker. Drinking, exercising, and taking sleeping pills were all classified as yes or no. Those who currently drink or take sleeping pills were classified as yes, otherwise, they were classified as no. In the case of exercise, those who answered that they rarely exercise or occasionally walk or take stairs up and down stairs were classified as no, otherwise, they were classified as yes. The job was classified as fire suppression, emergency medical services (EMS), rescue, fire investigation, and administration. Type of shift was investigated and classified into day work, 3-day cycle, 6-day cycle, 9-day cycle, and 21-day cycle. Psychosocial factors included depression and anxiety. Patients Health Questionnaires-9 (PHQ-9) was used for measuring depression and Generalized Anxiety Disorders-7 (GAD-7) was used for evaluating anxiety symptoms.2930 The total scores of PHQ-9 range from 0 to 27 and those of GAD-7 range from 0 to 21. Depression and anxiety were classified into absent and present. Both cut-off scores of questionnaires were 5 points (sum of score < 5 or ≥ 5). The reliability of both questionnaires was confirmed in Korea.3132
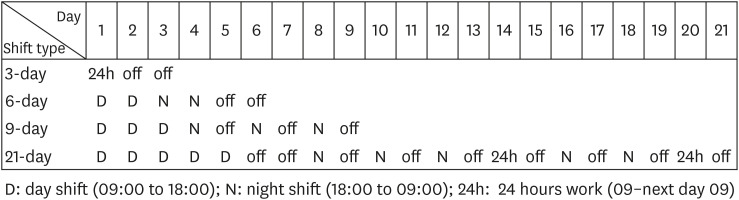
Type of shift
Four types of shift were included in this study. There were 3-day cycle, 6-day cycle, 9-day cycle, and 21-day cycle. Day work is from 9:00 to 18:00, and night work is from 18:00 to 09:00. The 3-day cycle consisted of 24 hours on and 2 days off. The 6-day cycle in order consisted of 2 days of day work, 2 days of night work, and 2 days off. The 9-day cycle in order consisted of 3 days of day work, night work, and off day were alternately repeated 3 times. The 21-day cycle in order consisted of 5-day works, 2 days off, night work and off duty were alternately repeated 3 times, 24-hours on duty, one day off duty, night work and off duty were alternately repeated 2 times, 24-hours on duty, and one day off (Fig. 2).
Measurement of sleep quality: Pittsburgh Sleep Quality Index (PSQI)
PSQI was used to measure the quality of sleep. It is a self-rating questionnaire and consisted of 19 questions. It has 7 components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleeping medication, and daytime dysfunction.33 The sum of the questionnaire scores range from 0 to 21. The cut-off point is 5 points. A PSQI global score ≤ 5 points is classified as a good sleep quality group, and PSQI global score ≥ 6 is classified as a poor sleep quality group. The reliability and validity of PSQI-K, a Korean version of the PSQI were confirmed to evaluate sleep quality.34
Statistical analysis
The χ2 test was performed to examine the relationship between general characteristics, occupational characteristics, and sleep quality. The t-test was used to compare the means of PSQI global score and its components score. In addition, logistic regression analysis was performed to evaluate whether shift work patterns affect sleep quality. Model 1 was adjusted for sex and age. Model 2 was adjusted for sex, age, education, marital status, obesity, income, smoking, alcohol, exercise, sleeping pills, depression, and anxiety. In addition, subgroup analyses by the psychosocial variables were performed. The odds ratio (OR) and 95% confidence interval (CI) were calculated. All analyzes were performed using IBM SPSS 25.0 (IBM Corp., Armonk, NY, USA), and the statistically significant level was set to p < 0.05.
Ethics statement
This study was approved by the Institutional Review Board (IRB) of Yonsei University Wonju Severance Christian Hospital (IRB No. CR318031).
RESULTS
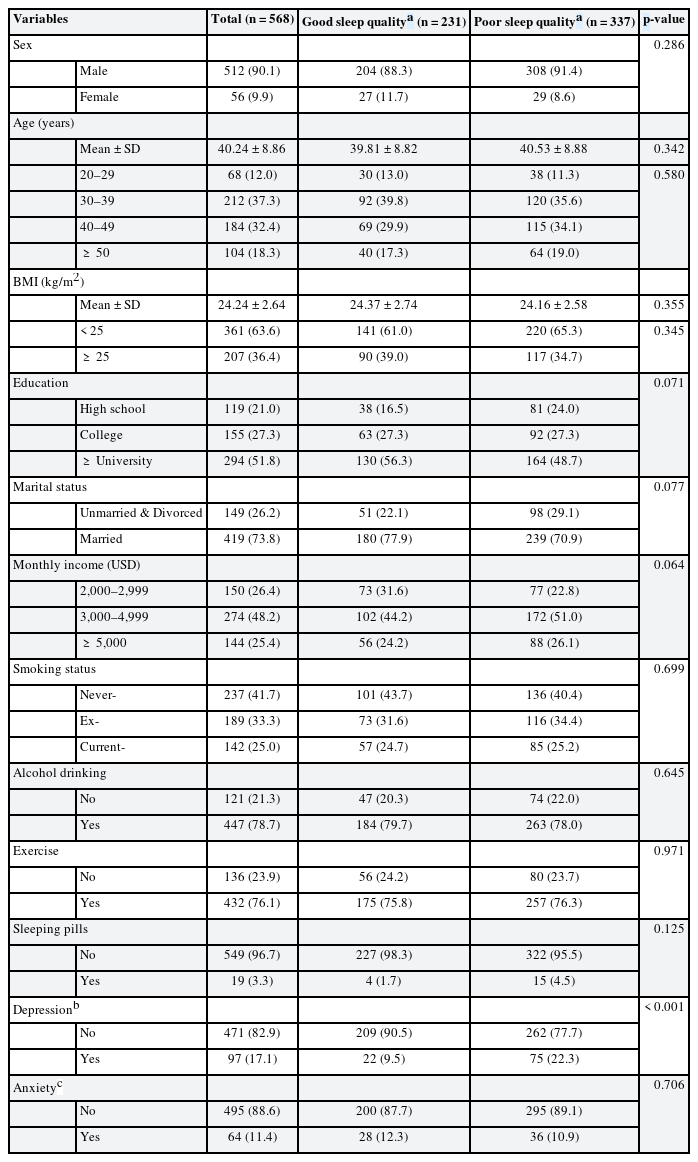
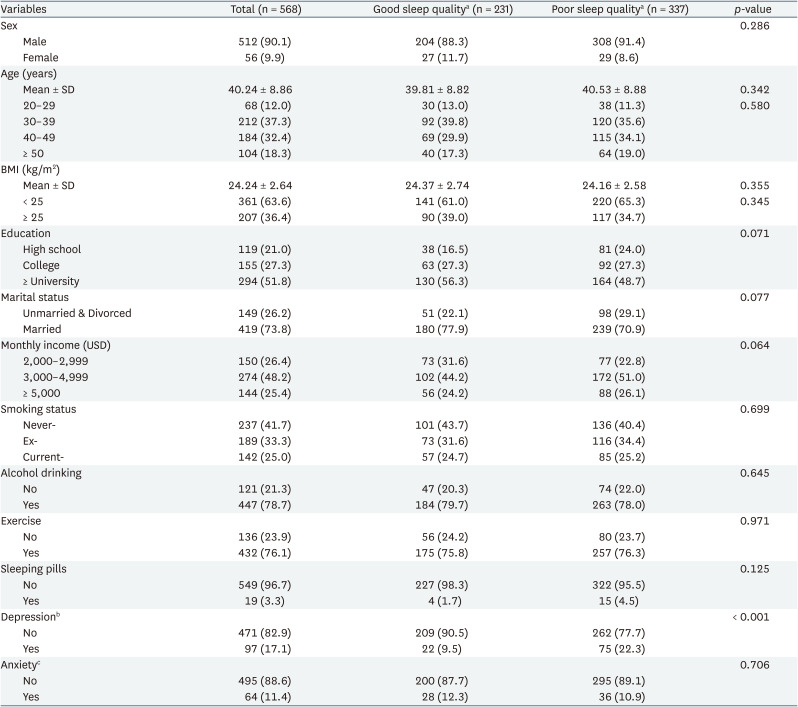
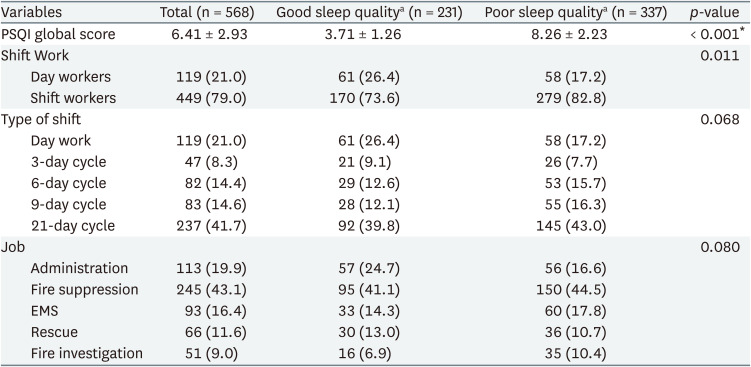
Table 1 describes the sociodemographic variables in the study population. By the quality of sleep by PSQI, the study population was divided into good and poor groups. Two hundred thirty-one participants (40.7%) were classified as having good sleep quality and 337 participants (59.3%) were classified as having poor sleep quality. There were 512 (90.1%) males and 56 (9.9%) females. Ninety-seven participants (17.1%) had depression and 64 participants (11.4%) had anxiety. There was a significant difference in the proportion of sleep quality by depression (p < 0.001). There were not statistically significant differences in other variables including sex, age, BMI (kg/m2), education, marital status, monthly income, smoking status, drinking status, exercise, sleeping pills, and anxiety in the 2 groups (Table 1).
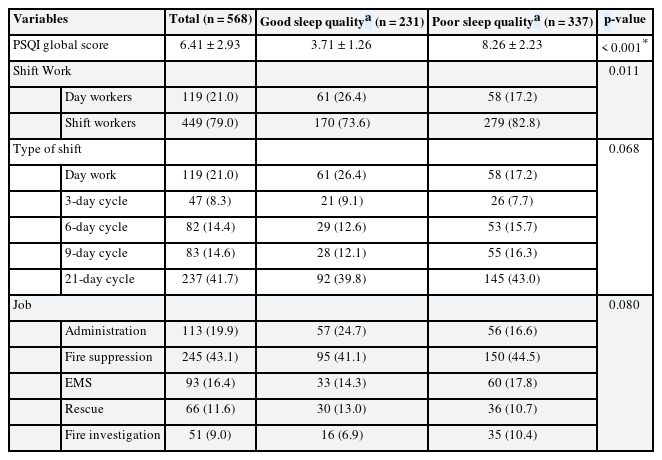
The shift work distributions were significantly different in the 2 groups by sleep quality (p < 0.001). There were 119 (21.0%) in day workers and 449 (79.0%) in shift workers. 58 (17.2%) among day workers and 279 (82.8%) among shift workers had poor sleep quality. By the type of shift work, 58 (17.2%) day workers, 26 (7.7%) 3-day cycle workers, 53 (15.7%) 6-day cycle workers, 55 (16.3%) 9-day cycle workers, and 145 (43.0%) 21-day cycle workers had poor sleep quality. By the type of job, 56 (16.6%) administration workers, 150 (44.5%) fire-suppression workers, 60 (17.8%) EMS workers, 36 (10.7%) rescue workers, and 35 (10.4%) fire-investigation workers had poor sleep quality (Table 2).
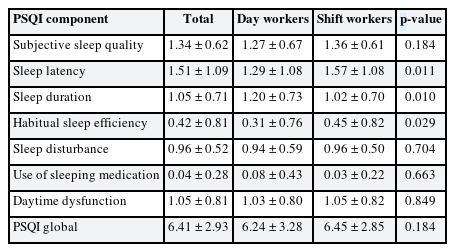
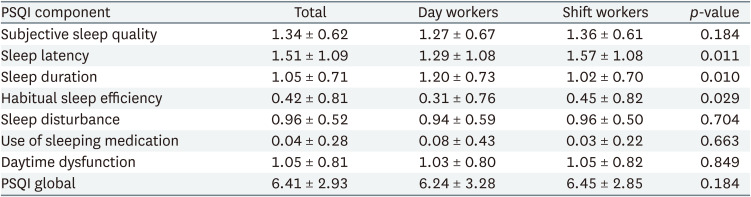
The PSQI global score of this study was 6.41 ± 2.93 (mean ± standard deviation). The score of day workers and shift workers were 6.24 ± 3.28 and 6.45 ± 2.85. There was no significant difference in scores between the 2 groups. The PSQI component scores of day workers and shift workers were 1.29 ± 1.08 and 1.57 ± 1.08 in sleep latency, 1.20 ± 0.73 and 1.02 ± 0.70 in sleep duration, and 0.31 ± 0.76 and 0.45 ± 0.82 in habitual sleep efficiency, respectively. Sleep latency, sleep duration, and habitual sleep efficiency were statistically significant differences between day and shift workers. However, there was no significant difference in PSQI global score (Table 3).
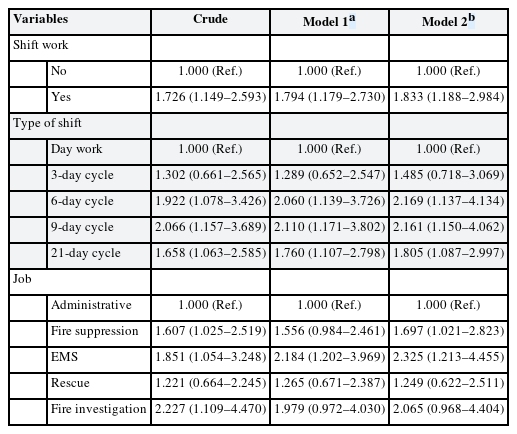
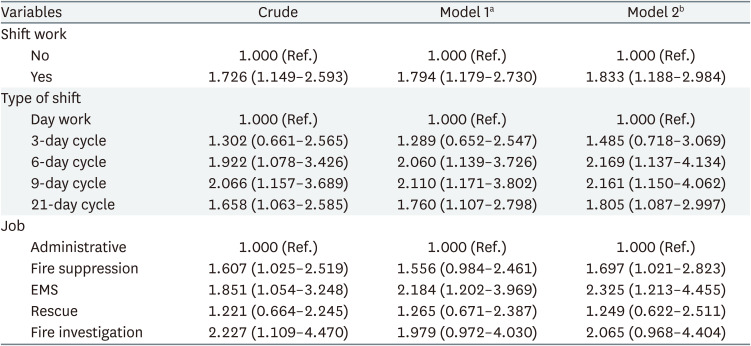
Compared with day workers, shift work was significantly associated with poor sleep quality in all models. After adjusting all sociodemographic and psychosocial variables in our study, the poor sleep quality evaluated by PSQI was associated with shift work (OR: 1.833, 95% CI: 1.188–2.984). All types of shifts except for the 3-day cycle were significantly associated with poor sleep quality compared to day work. The poor sleep quality evaluated by PSQI was associated with a 6-day cycle (OR: 2.169, 95% CI: 1.137–4.134), 9-day cycle (OR: 2.161, 95% CI: 1.150–4.062), and 21-day cycle (OR: 1.805, 95% CI: 1.087–2.997) in model 2. Jobs affecting the sleep quality of firefighters were fire suppression (OR: 1.697, 95% CI: 1.021–2.823) and EMS (OR: 2.325, 95% CI: 1.213–4.455) (Table 4).
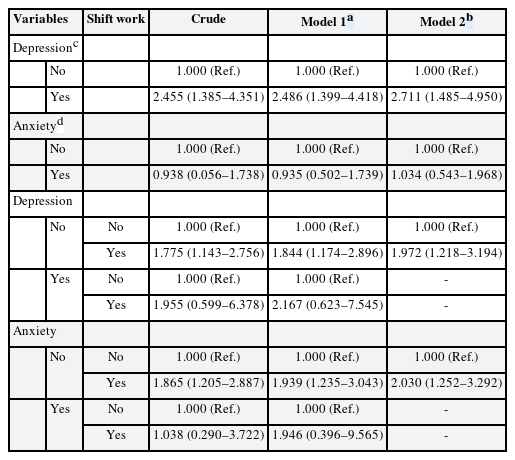
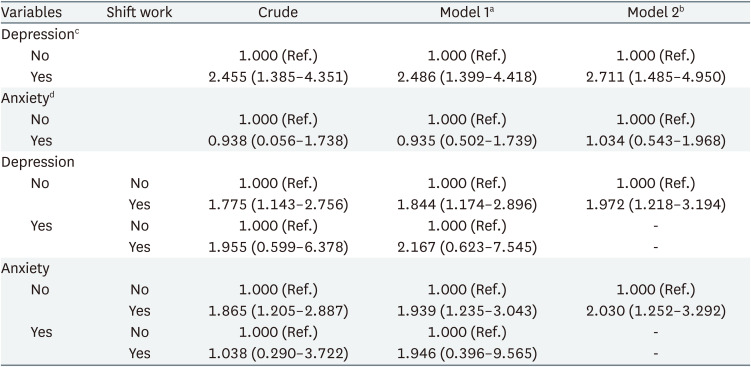
In psychosocial variable, depression was associated with poor sleep quality (OR: 2.711, 95% CI: 1.485–4.950), however anxiety was not (OR: 1.034, 95% CI: 0.543–1.968). After stratification-based on psychosocial variables, shift work was associated with poor sleep quality in the non-depression (OR: 1.972, 95% CI: 1.218–3.194) and non-anxiety group (OR: 2.030, 95% CI: 1.252–3.292). There were no statistically significant associations between shift work and poor sleep quality in depression group (OR: 2.167, 95% CI: 0.623–7.545) and anxiety group (OR: 1.946, 95% CI: 0.396–9.565) (Table 5).
DISCUSSION
Our study shows that shift workers were associated with poor sleep quality than day workers. Further analyses show that 6-day, 9-day, and 21-day cycle shift workers were associated with poor sleep quality, and fire suppression and EMS were associated with poor sleep quality. This association was significant after adjustment for socio-demographic status, healthy habits, and psychosocial variables.
The prevalence rate of poor sleep quality ranges from 52.45% to 86.8% in Korean firefighters.17353637 Our study showed that the poor sleep quality group was 59.3%. The result of this study was also similar to those of the poor sleep quality group compared to previous studies in Korea. In comparison to the sleep quality of firefighters in other countries, the quality of sleep among Korean firefighters is slightly better. The prevalence of poor sleep quality among Iran and American firefighters were 69.9% and 73%, respectively. In contrast, the prevalence rate of poor sleep quality among French firefighters was 26.9%.192038
Compared with the PSQI score of the Korean general population, the scores of the subjects of this study were higher. In the component’s scores of the general population, sleep latency was 0.96 ± 1.02, sleep duration was 1.58 ± 1.04, habitual sleep efficiency was 0.48 ± 0.88, and daytime dysfunction was 0.45 ± 0.74.39 The PSQI component scores of our study subjects were higher in sleep latency and daytime dysfunction than in the general population. Rather, the sleep duration score was 1.05 ± 0.71, which was lower on average than the general population. For firefighters, sleep latency and daytime dysfunction may be particularly worse than in the general population. In our study, sleep latency, sleep duration, and habitual sleep efficiency were statistically significantly different between day and shift workers. In the sleep latency and habitual sleep efficiency, the score of shift workers was higher than that of day workers. In the sleep duration component, however, the score of the shift workers was lower than that of the day workers. There was a report that the sleep latency was good in the non-shift firefighter. However, the sleep duration was shorter than that of the shift firefighter in Iran.21 Sleep latency was significantly worse in other shift work studies as well.
In the logistic analysis, 6-day, 9-day, and 21-day cycle were significantly associated with poor sleep quality compared to the day shift, whereas the 3-day cycle was not significant. In a study evaluating insomnia using Insomnia Severity Index, no significant difference was found by the type of shift work in the final model.18 The risk of insomnia was higher in the 9-day cycle, and 21-day cycle compared to the day shift in some models. In a study conducted on American firefighters, there was no significant difference by the shift work type based on the cut-off of PSQI scores, but the PSQI score showed lower scores in the 3-day cycle (24 on–48 off) shift work.19 Shift workers need at least 48 hours to recover from the night shift. However, the 9-day cycle and 21-day cycle do not have the least amount of time to recover their sleep patterns and correspond to the fast or slow shifts recommended for shift work. In a study measuring cortisol recovery in the same panel, however, the 9-day cycle showed complete recovery of cortisol.40 Wake time after sleep onset and sleep efficiency measured using Actigraph of the 6-day cycle in day shift were better than that of other types of shift.41 Sleep quality of 21-day cycle in night shift was worse than that of other types of shift. Although the most suitable shift work type appears differently depending on the measurement tool, the 21-day cycle has a risk in common.
In the type of job, fire suppression and EMS were significantly associated in model 2. In a previous study, fire suppression, EMS, rescue, and others all had a higher risk of insomnia compared to administrative.18 Therefore, in terms of sleep quality or insomnia, fire suppression and EMS were worse than administration. In a study of firefighters in one city, the number of dispatches, that is, the number of emergency events varies depending on the job. EMS had the highest frequency of dispatching more than 21 times, followed by fire suppression, and rescue. The administration had the lowest number of dispatches.42 Therefore, a job with a high number of dispatches that can cause sleep disturbance may have poor sleep quality. There was no significant difference in the OR by the type of job targeting Korean firefighters.
Sleep disturbance is a common symptom in depressive patients and sleep disorder is considered a risk factor for depression.43 In previous studies showed that depression was closely related to sleep quality.4445 Shift work might be associated with an increased risk of depression with disruption circadian glucocorticoids.46 Our stratification analysis showed that poor sleep quality was significantly affected by shift work in non-depression group but not in the depression group. However, the OR of shift work was similar in the 2 groups after stratification.
Many studies reported an association between poor sleep quality and obesity.6474849 In our study, however, there was no significant difference in obesity between the groups with good sleep quality and poor sleep quality. In this study, the proportion of severe obesity (BMI ≥ 30) was low and there is a limitation of no survey for obstructive sleep apnea. In the cohort of firefighters, the average BMI was 24.83 which was not significantly different from this panel composition.37 In addition, a few studies showed that the sleep problem contributed to weight gain in middle-aged women and men, but it was significant only in women and not in men.50 Also, in a study conducted in Korea, the association between sleep quality and obesity measured by PSQI was related in women, but not in men.51 Because our study had a large number of male subjects, there may not be a significant difference between obesity and sleep quality.
This study has several limitations. First, the study was designed as cross-sectional. Therefore, the causality between sleep quality and shift work type cannot be inferred. Second, other factors including the number of interruptions at night during work, job intensity, frequency of off-duty work, fatigue, post-traumatic stress disorder, and caffeine intake, which were investigated in the previous studies, were not reflected in this study.181952 Thus, several variables affecting sleep quality may not have been considered in this study. Finally, sleep quality, depression, anxiety, and sociodemographic variables such as height and weight were evaluated through a self-reporting questionnaire. Despite the limitations, our study has an advantage in evaluating the quality of sleep by the type of shift work, not just shift work. To overcome these limitations and get more reliable results, a longitudinal follow-up study involving more job-related variables including job intensity.
CONCLUSIONS
Our study showed that poor sleep quality was highly prevalent in firefighters and associated with shift work. Especially, we found that the 6-day cycle, 9-day cycle, and 21-day cycle had poor sleep quality compared to day work. Therefore, the sleep quality may differ depending on the type of shift work. In terms of sleep quality, this study suggests that 3-day cycle is likely to be a better form of shift work for firefighters. More research is needed to evaluate a more suitable type of shift work for firefighters from sleep health perspective.
Acknowledgements
The authors of this paper would like to thank all firefighters who participated in this study.
Notes
Funding: This research was supported by the National Fire Agency, grant number 2017-NFA001-01010000-2020.
Competing interests: The authors declare that they have no competing interests.
Author contributions:
Conceptualization: Oh HJ, Jeong KS.
Data curation: Oh HJ.
Formal analysis: Oh HJ.
Funding acquisition: Ahn YS.
Investigation: Sim CS, Jang TW, Ahn YS, Jeong KS.
Methodology: Oh HJ, Jeong KS.
Software: Oh HJ.
Validation: Jeong KS.
Visualization: Oh HJ.
Writing - original draft: Oh HJ.
Writing - review & editing: Sim CS, Jang TW, Ahn YS, Jeong KS.
Abbreviations
BMI
body mass index
CI
confidence interval
EMS
emergency medical services
GAD-7
Generalized Anxiety Disorders-7
IRB
Institutional Review Board
OR
odds ratio
PHQ-9
Patients Health Questionnaires-9
PSQI
Pittsburgh Sleep Quality Index