Digital health care and arrhythmia: a case of WPW syndrome in South Korea, 2020
Article information
Abstract
Background
The digital health care field is expanding from the daily monitoring of chronic diseases to the detection of acute diseases, such as arrhythmia. Wolff-Parkinson-White (WPW) syndrome, a congenital cardiac disorder due to accessory pathways, causes tachycardia, syncope, and even sudden death.
Case presentation
We presented a 26-year-old female office worker with WPW syndrome managing the disease with a wearable device and discussed its significance in occupational medicine. After reviewing the worker's electrocardiogram results, symptoms, and pulse rate records extracted from the wearable device, we referred the worker to a cardiologist for further evaluations such as electrophysiology study. The worker monitors her symptom recurrence with the wearable device following successful radiofrequency catheter ablation of the bypass tract.
Conclusions
A case of an office worker with WPW syndrome managing the disease using a smart watch is presented. Further research is required to ensure its scientific validity, and we suggest policymakers promptly introduce digital health care to occupational environments.
BACKGROUND
We are witnessing the dawn of a new medical era. Owing to the innovative progression of information technology and electronics, digital health care using wearable devices such as smartwatches has begun to be introduced in our daily lives. Interestingly, digital health care has already gained importance in medicine as a monitoring measure for some health indexes, such as blood pressure, pulse rate, oxygen saturation, and electrocardiogram (ECG) [1].
Digital health care is generally regarded as a tool for managing chronic rather than acute diseases. However, as the accuracy and validity of wearable devices have become acceptable, opportunities to detect acute diseases such as cardiac arrest or arrhythmia are emerging [2].
Wolff-Parkinson-White (WPW) syndrome, a congenital cardiac disorder due to accessory pathways, causes palpitation, syncope, and even sudden death. Tachycardia is the key etiology of WPW syndrome, and the early detection of an abnormally fast heartbeat is critical for timely treatment [3].
We present the case of a 26-year-old female worker with WPW syndrome, who managed the disease with a wearable device, and discuss its significance in occupational medicine.
CASE PRESENTATION
She is an office worker working in a multinational company's quality control department. She worked for almost 12 hours a day, from 8 am to 8 pm. She had no known risk factors for cardiovascular disease.
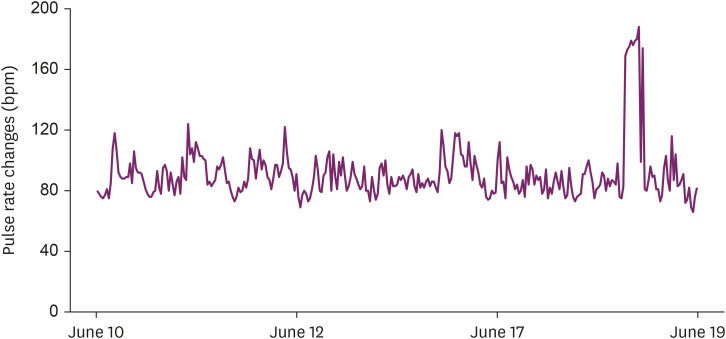
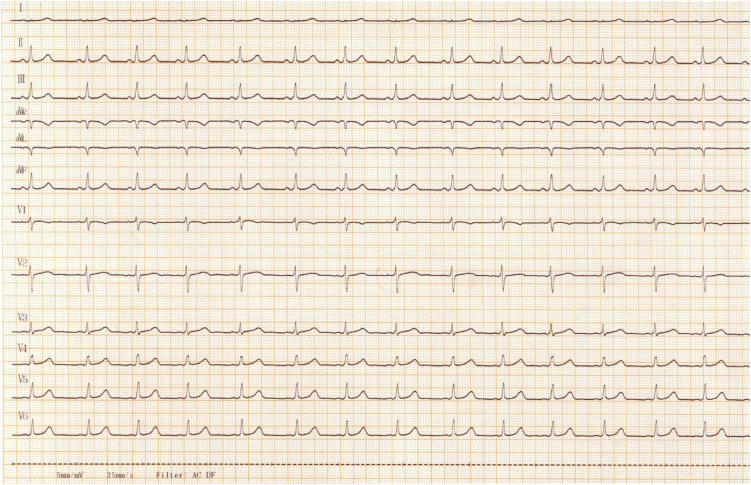
She has been experiencing palpitations for four years. Recently, fatigue, nausea and vertigo, headache, and radiating pain to both axillae were accompanied with palpitations. On June 9, 2020, due to severe palpitation at work, she visited the emergency department of the hospital and received symptomatic treatments. The following day, she purchased a smartwatch (Galaxy Fit, SM R-370; Samsung, Seoul, Korea) with a photoplethysmography (PPG) sensor to check the pulse rate. On June 18, when she experienced severe palpitations for hours, her peak resting pulse rate reached 188 beats per minute (Fig. 1). On June 19, when she was asymptomatic, a standard 12-lead ECG was performed as part of a regular health examination. ECG showed WPW syndrome features such as shortened PR interval and delta waves (Fig. 2). We recommended further evaluations such as electrophysiology study (EPS) based on her ECG results, symptoms, and pulse rate records extracted from her smartwatch (Fig. 1).
She received EPS on June 29 at our hospital, and radio frequency catheter ablation was simultaneously conducted to eliminate the bypass tract. Since her discharge, she has kept monitoring symptom recurrence with a smartwatch.
Ethics statement
This study was approved by the Kangbuk Samsung Hospital Institutional Review Board (IRB No. 2020-06-054). Consent forms were signed by the patient.
DISCUSSION
This novel case successfully demonstrates the potential of digital health care to promote public health, especially workers' health. As in our patient, with the aid of digital health care, workers with underlying cardiac diseases can monitor their vital signs or ECG themselves. This information helps them seek timely medical intervention. It not only visually presents their symptoms, which would otherwise remain uncertain, but also quantifies their needs for proper treatment. Moreover, the information collected via digital health care can provide physicians with auxiliary evidence.
However, there is still room for improvement in digital health care. PPG sensors measure blood volume changes in the microvasculature, which could miscalculate certain arrhythmias such as atrial fibrillation. In addition, the accuracy might be degraded by movement, noise during measurement, or complex patterns. Nevertheless, recent advances in computational power and the advent of powerful deep learning algorithms provide a significant improvement in accuracy [4]. The Apple Watch 4 (Apple, Cupertino, CA, USA), a wrist-worn wearable device using PPG sensors released in 2018, reports 99.6% specificity with respect to sinus rhythm classification and 98.3% sensitivity for atrial fibrillation classification for the classifiable results [5].
Our patient was a young female office worker who frequently overworked, an obvious aggravating factor for WPW syndrome. Little is known about the prevalence of WPW syndrome or arrhythmia in working populations; however, it is clear that numerous workers have underlying conditions that might be worsened by occupational factors such as hypertension, diabetes mellitus, dyslipidemia, or ischemic heart diseases. Therefore, applying digital health care to monitor vulnerable people with occupational hazards is a critical and pressing matter. The Ministry of Employment and Labor of South Korea reported that 1,153 workers had cardiovascular and cerebrovascular diseases due to occupational risks, and 457 workers died in 2018 [67]. Although we do not know how many lives could have been spared with digital health care, it is worth offering modern conveniences to the vulnerable.
Practically, an automatic monitoring system using information technology that detects and reports risky events exceeding a specific screening threshold is required. Both workers and workplace health specialists (such as occupational physicians) should be informed accordingly to take necessary actions for health-promotion purposes. We suggest further research to ensure its scientific validity and that policymakers promptly introduce digital health care to occupational environments.
ACKNOWLEDGEMENTS
The authors would like to thank HRM.
Notes
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests: The authors declare that they have no competing interests.
Author Contributions:
Conceptualization: Lee C.
Investigation: Mun E, Hong J, Kwon S.
Writing - original draft: Mun E, Lee C.
Writing - review & editing: Lee SH, Kim W.
Abbreviations
BPM
beats per minute
ECG
electrocardiogram
EPS
electrophysiology study
PPG
photoplethysmography
WPW
Wolff-Parkinson-White