The relationship between chronotypes and musculoskeletal problems in male automobile manufacturing workers
Article information
Abstract
Background
Previous studies have shown that morning types are less sensitive to pain. This study aimed to examine the relationship between chronotypes and musculoskeletal problems in workers with musculoskeletal burdens at work.
Methods
This cross-sectional study included 119 male production workers from a large automobile manufacturing plant. All the participants worked 2 shifts and worked on the automobile assembly line. Data were obtained using structured questionnaires, including the reduced Morningness-Eveningness Questionnaire (rMEQ), and musculoskeletal symptom questionnaire. Participants with an rMEQ score of 18 points or more were defined as morning-type workers (MTWs). Participants whose scores were less than 18 points were defined as neither-type workers (NTWs).
Results
The arithmetic mean age was 51.8 ± 5.3 years. MTWs and NTWs accounted for 35.3% and 64.7% of the total participants, respectively. Evening- and intermediate-type workers accounted form 6.7% and 58.0% of the participants, respectively. There was no significant difference in the health indicators when the MTW and NTW groups were compared. However, the musculoskeletal symptom questionnaire demonstrated a significant difference between the MTW and NTW groups. In the preceding year, the MTW group had significantly lower musculoskeletal pain and treatment ratios compared to the NTW group (35.7% vs. 62.3%, p = 0.005 and 14.3% vs. 32.5%, p = 0.031, respectively). After adjusting for variables, the odds ratio (OR) for musculoskeletal pain was significantly higher in the NTW group than in the MTW group (OR, 3.112; 95% confidence interval, 1.285–7.535; p = 0.012).
Conclusions
In this study, the musculoskeletal pain ratio was significantly lower for MTWs when compared to NTWs. Chronotypes could play an important role in work-related musculoskeletal disorders. Further, larger-scale, follow-up studies on chronotypes are required to assist in the prevention of musculoskeletal disorders in future.
BACKGROUND
Everyone has an inner biological clock, as well as time zones in which they feel most comfortable waking up and falling asleep. A person's mental state and physical activity can change according to this circadian cycle. This cycle is called a chronotype, and it is often classified into morning, intermediate, and evening types. Morning-type persons go to bed early, wake up early, and achieve their peak mental and physical performance in the early part of the day. By contrast, evening-type persons go to bed and wake up late and perform at their best toward the evening.1 Research has demonstrated that morning- and evening-type persons show differences in various characteristics such as psychology, physiology, behavior, health, and personality.23
Previous studies have shown that morning-type persons are less sensitive to pain. There are several studies that have demonstrated marked differences in pain sensitivity based on a person's chronotype.4567 In a study of healthy men, morning types showed less sensitivity to pain than evening types throughout the day.4 These findings are consistent with those of studies that involved patient groups and specific occupations.567 For example, a patient study found that sleep had strong links to fibromyalgia syndrome symptomology, and late chronotypes were more affected by fibromyalgia.8 These results showed that chronotype could be an important factor in determining sensitivity to pain. Moreover, chronotype is not only associated with pain sensitivity but may also be associated with the morbidity of musculoskeletal disorders. A study conducted in Finland suggests that evening types have higher odds for articular and spinal diseases as compared with morning types after adjusting for confounders (odds ratios [ORs] of 1.8 to 2.1, and 1.6 to 1.8, respectively).9
As of 2016, the number of manufacturing workers in the Republic of Korea (ROK) reached 3.8 million, and automobile manufacturing industries are one of the major manufacturing industries with a significant level of musculoskeletal burden.10 Workers in the automobile manufacturing industry perform high-level musculoskeletal burden tasks, including factors such as repetitive work of upper limbs, neck, and back, and poor posture at work. In such a work environment, active management of musculoskeletal disorders and pain is necessary for the safety, health, and work efficiency of workers. Considering that chronotype is a factor that can affect pain, it is important to have a deep understanding of chronotypes and to actively utilize them to reduce the musculoskeletal burden.11 Thus, this study aimed to examine the relationship between chronotypes and musculoskeletal problems in workers who perform tasks at work that have a musculoskeletal burden.
METHODS
Study participants
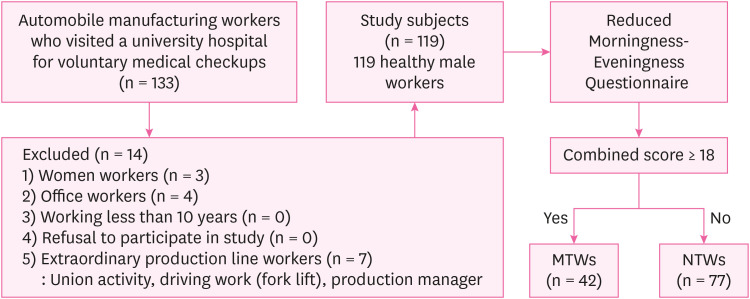
The study participants consisted of 119 male, Korean production workers from a large automobile manufacturing factory who underwent health examinations at a university hospital between January 2020 and December 2020. The participants' ages ranged from 37 to 61 years. All the study participants were two-shift production workers. The production process used a system that ran 2 shifts during the day (a weekly shift runs from 7:00–15:40 and from 15:40–00:30). All the participants performed the same types of shifts and similar assembly tasks (assembly conveyor production within a circular process system). All participants were full-time workers with the same welfare benefits. In this study, the participants were limited to those who had worked at the company for more than 10 years. Women workers, office workers, and non-standard extraordinary production line workers were excluded from the study (Fig. 1).
Data collection
All participants were provided with one day off during their day shift (7:00–15:40) for health examinations. The participants were interviewed by physicians using a structured questionnaire. We investigated their age, smoking and drinking habits, regular exercise, and medical history. Participants who smoked more than 5 packs of cigarettes in the preceding year were defined as current smokers. Participants who ingested more than 20 g of alcohol more than once a week were classified as alcohol drinkers. Participants who exercised for 30 min or longer at least twice a week were classified into the regular exercise group. The participants' heights, weights, and blood pressures were measured. Body mass index (BMI, kg/m2) was calculated by dividing the weight (kg) by the height squared (m2). Obesity was defined as a BMI ≥ 25 kg/m2, according to the guidelines set by the South Korean Ministry of Health and Welfare.12 Blood pressure measurements were taken from the right arm in the sitting position using a digital blood pressure monitor under stable conditions. After 12 hours of fasting, blood samples from all participants were collected via venipuncture. All the participants' blood tests were conducted between 9:00 am and 11:00 am. Total high-density lipoprotein (HDL), and low-density lipoprotein (LDL) cholesterol, triglyceride, cortisol, glycated hemoglobin, and fasting glucose levels were measured. Participants who were taking antihypertensive medications, or who had a systolic blood pressure ≥ 140 mmHg, or who had a diastolic blood pressure ≥ 90 mmHg at the time of the examination were classified as hypertensive. Participants who were being treated for diabetes mellitus, or who had fasting glucose levels ≥ 126 mg/dL, or who had glycated hemoglobin levels ≥ 6.5% at the time of the health examination were classified as diabetes mellitus. Participants who were being treated for dyslipidemia, or who had a total cholesterol levels ≥ 240 mg/dL, or LDL cholesterol levels ≥ 160 mg/dL, or triglyceride levels ≥ 500 mg/dL at the time of the health examination, were classified as dyslipidemia. Serum cortisol levels were measured using a Beckman Coulter Dxl 800 immunoassay system that used chemiluminescent technology (Beckman Coulter Inc., Brea, CA, USA).
Chronotype evaluation
The Morningness-Eveningness Questionnaire (MEQ) was developed by Horne and Östberg in 1976.1314 It contained 19 questions about individual waking and sleeping times, preferred time of physical and mental performance, and alertness after waking and before going to bed. The reduced Horne-Östberg MEQ (rMEQ) is one of the most widely used questionnaires for measuring chronotype. The rMEQ consists of 5 questions; thus, it is both an easier and faster way to survey a large population. Moreover, the rMEQ has been developed and validated in multiple languages. The rMEQ can be used to effectively estimate a person's chronotype when a short questionnaire is required.1516 In this study, participant's chronotypes were investigated using the rMEQ. A combined score of 18–25, 12–17, and 4–11 points indicated morning-type workers (MTWs), intermediate-type workers, and evening-type workers, respectively. Intermediate- and evening-type workers (those with less than 18 points on the rMEQ) were defined as neither-type workers (NTWs).
Evaluation of musculoskeletal problems
We used the symptom survey questionnaire of the legal examination of work-related musculoskeletal risk factors (Korea Occupational Safety and Health Agency Guide H-9-2018) as the musculoskeletal problem assessment survey.17 Regardless of the area where the pain was felt, participants who experienced musculoskeletal pain during the preceding year were categorized into the musculoskeletal pain group. Moreover, regardless of the area where the pain was felt, participants who received medical treatment for musculoskeletal pain in the preceding year were categorized into the musculoskeletal treatment group. In treatment group, participants who received treatment through pharmacies were excluded, and those who were treated using oriental medicine were included.
The Brief Encounter Psychosocial Instrument and Insomnia Severity Index
We used the Korean-language Brief Encounter Psychosocial Instrument (BEPSI-K), an instrument that was developed to measure stress, to measure participants' stress levels.1819 The BEPSI-K consisted of 5 questions. Each of the questions was answered using a 5-point Likert scale. The sum of the scores from the 5 questions was averaged and calculated as the final score. The final score was interpreted as follows: low stress level, 1.0–1.6; moderate stress level, 1.8–2.6; and high stress level, 2.8–5.0. To evaluate whether participants had problems sleeping, the Insomnia Severity Index (ISI) test was conducted. The ISI is considered a validated measurement tool worldwide.20 It consisted of 7 questions. Participants assigned scores of 0–4 points to each question. The total scores were interpreted as follows: absence of insomnia, 0–7; sub-threshold insomnia, 8–14; moderate insomnia, 15–21; and severe insomnia, 22–28.
Other questions
Further investigation was undertaken by adding the following questions to the questionnaire. 1) Sleep time: What was your average sleep duration per day for the past year? Answer: continuous variable. 2) Snoring: Do you snore? Or do you often hear that you snore? Answer: Yes or No. 3) Obstructive sleep apnea: Do you have sleep apnea? Or do you often hear that you have sleep apnea? Answer: Yes or No. 4) Fatigue upon waking up: Do you feel tired when you wake up in the morning? Answer: Yes or No. 5) Daytime fatigue: Do you feel tired when working during the day? Answer: Yes or No.
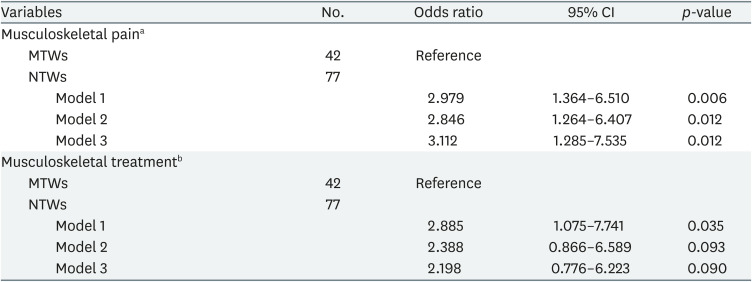
Statistical analyses
Pearson's χ2 test or Fisher's exact test was performed to confirm whether there were differences in the categorical variables according to the chronotype. Student's t-test was performed for the differences in the continuous variables. Multiple logistic regression models were used to estimate ORs and 95% confidence intervals (CIs) for musculoskeletal pain or treatment when the MTW and NTW groups were compared. Model 1 was not adjusted. Model 2 was adjusted for age (continuous). Model 3 was adjusted for age and significant predictors (p < 0.100) of musculoskeletal pain or treatment (BMI [continuous variable], current smoker [yes/no], diabetes mellitus [yes/no], regular exercise [yes/no], BEPSI score [continuous variable], and ISI score [continuous variable]). SPSS version 26.0 (SPSS Inc., Chicago, IL, USA) was used to analyze the data. Statistical significance was defined as a p-value < 0.05.
Ethics statement
The study protocol was approved in advance by the Institutional Review Board of Chonnam National University Hospital (IRB No. CNUHH-2021-035). In addition, each subject provided written, informed consent before participating.
RESULTS
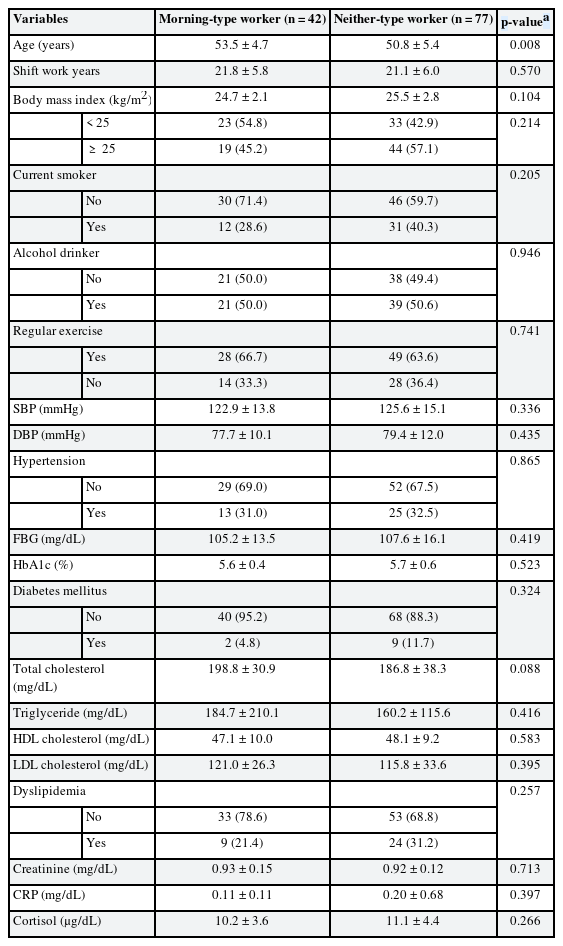
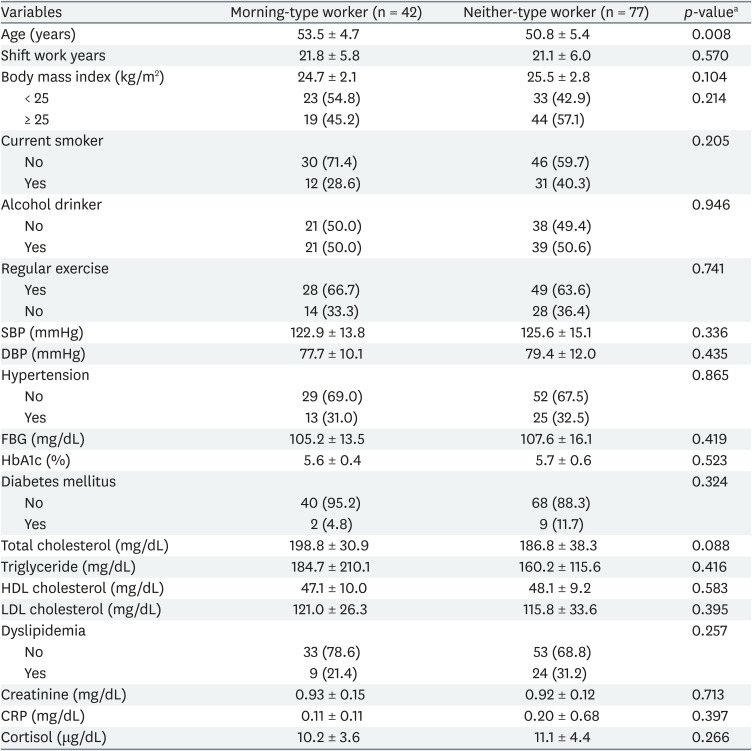
The participants' arithmetic mean age was 51.8 ± 5.3 years (minimum–maximum: 37–61 years). MTWs and NTWs accounted for 35.3% and 64.7% of the total participants, respectively (42/119 and 77/119, respectively). Evening and intermediate types accounted for 6.7% and 58.0% of the participants, respectively (8/119 and 69/119, respectively). General participant characteristics were compared by dividing the participants into the MTW and NTW groups. The arithmetic mean ages of the MTW and NTW groups were 53.5 ± 4.7 years and 50.8 ± 5.4 years, respectively. The mean age of the MTW group was higher than that of the NTW group, and this difference was statistically significant (p = 0.008). The arithmetic means for the number of shift work years for the MTW and NTW groups were 21.8 ± 5.8 years and 21.1 ± 6.0 years, respectively. The MTW group had longer shifts than the NTW group; however, this difference was not statistically significant (p = 0.570). The arithmetic mean BMIs for the MTW and NTW groups were 24.7 ± 2.1 kg/m2 and 25.5 ± 2.8 kg/m2, respectively. The MTW group had lower BMIs than the NTW group; however, this difference was not statistically significant (p = 0.104). There were no significant differences in smoking habits, alcohol consumption, regular exercise, hypertension, diabetes mellitus, dyslipidemia, creatinine, C-reactive protein, and cortisol when the MTW and NTW groups were compared (Table 1).
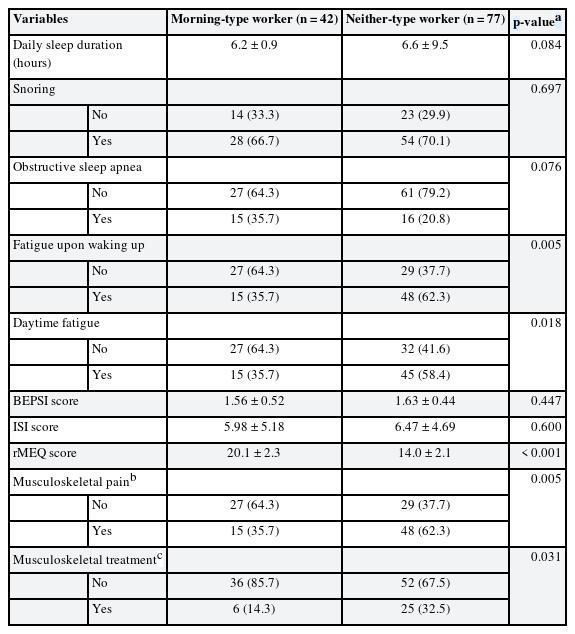
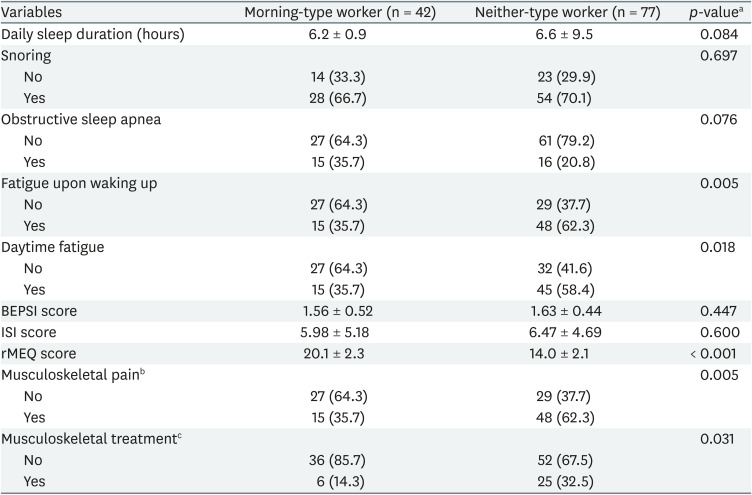
We compared the differences in clinical characteristics between the MTW and NTW groups. The daily sleep duration for the MTW group was 6.2 ± 0.9 hours, which was shorter than the NTW group's 6.6 ± 9.5 hours; however, the difference between the groups was not statistically significant (p = 0.084). The differences between the 2 groups in snoring and obstructive sleep apnea were not statistically significant. The MTW group had a BEPSI score of 1.56 ± 0.52 points, which was lower than the 1.63 ± 0.44 points of the NTW group; however, this difference was not statistically significant (p = 0.447). The ISI score for the MTW group was 5.98 ± 5.18 points, which was lower than the 6.47 ± 4.69 points for the NTW group; however, this difference was not statistically significant (p = 0.600). The proportion of participants in the MTW group that experienced fatigue upon waking was 35.7%, which was lower than the 62.3% in the NTW group. This difference was statistically significant (p = 0.005). The proportion of participants in the MTW group that experienced daytime fatigue was 35.7%, which was lower than the 58.4% in the NTW group, and this difference was statistically significant (p = 0.018). The proportion of participants in the MTW group that experienced musculoskeletal pain in the preceding year was 35.7%, which was lower than the 62.3% in the NTW group, and this difference was statistically significant (p = 0.005). The proportion of participants in the MTW group that received medical treatment for musculoskeletal problems in the preceding year was 14.3%, which was lower than the 32.5% in the NTW group, and this difference was statistically significant (p = 0.031, Table 2).
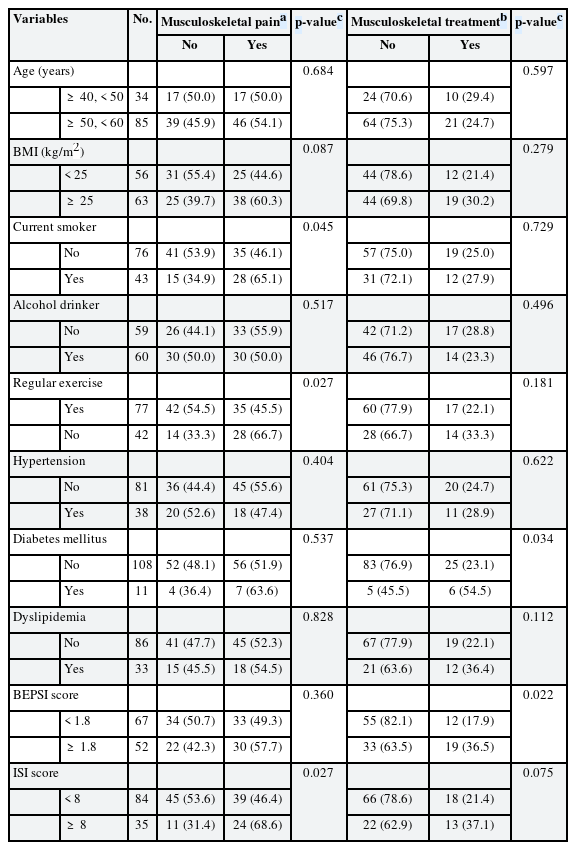
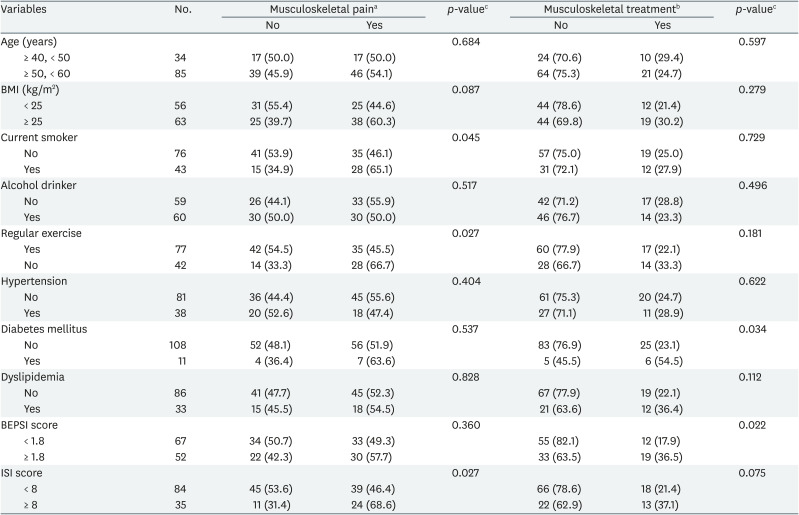
We attempted to determine the predictors of musculoskeletal pain or its treatment. Current smoking, regular exercise, and the ISI score were significant predictors of musculoskeletal pain. Diabetes mellitus and the BEPSI score were significant predictors of musculoskeletal pain treatment (Table 3).
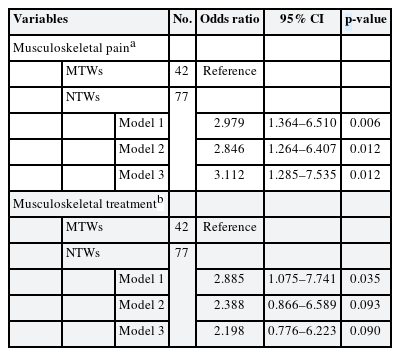
ORs and 95% CIs were calculated using multiple logistic regression analysis. When musculoskeletal pain was used as a variable, the OR was significantly higher in the NTW group than in the MTW group in all models. In the NTW group, the fully adjusted (Model 3) OR for musculoskeletal pain increased to 3.112 (95% CI, 1.285–7.535) when compared to the MTW group, which was statistically significant (p = 0.012). When musculoskeletal treatment was used as a variable, the OR was significantly higher in the NTW group than in the MTW group in Model 1. In the NTW group, the unadjusted (Model 1) OR for musculoskeletal treatment increased to 2.885 (95% CI, 1.075–7.741) compared to the MTW group. This finding was statistically significant (p = 0.035). However, the statistical significance was weakened in Models 2 and 3 (p = 0.093 and p = 0.090, respectively; Table 4).
DISCUSSION
This study demonstrated a significant difference in the presence of musculoskeletal pain according to chronotype. NTW showed about 3.112 times higher OR for musculoskeletal pain than MTW, which was significant even after adjusting for related variables. Previous studies on the relationship between these chronotypes and musculoskeletal pain are limited to the general population, patient group, or few specific occupations. According to our knowledge, this is the first study to confirm the relationship between musculoskeletal pain and chronotype in workers performing a significant level of musculoskeletal burden.
Work-related musculoskeletal disorders (WMSDs) comprise a major component of occupational disease in the ROK.2122 A 2018 report by the Korean Ministry of Employment and Labor found that WMSDs accounted for 57.6% of the occupational diseases approved by the Industrial Accident Compensation Insurance Act (6,603 out of 11,473). Various policies (e.g., legal examinations of work-related musculoskeletal risk factors, prevention and management programs for musculoskeletal disorders, and creation of industry-specific musculoskeletal disorder prevention manuals) have been implemented to prevent WMSDs in the ROK; however, despite these efforts, the number of WMSDs is increasing every year.23 The number of workers who had compensations for WMSDs approved by the Industrial Accident Compensation Insurance Act was 5,074 and 4,835 in 2017 and 2016, respectively.24 A paradigm shift is needed to prevent WMSDs in the ROK.
There have been studies on the effect that chronotype has on pain. Previous studies have consistently reported that people with morning chronotypes were less sensitive to pain. A study that exposed 16 and 15 healthy, morning- and evening-type men, respectively, to pain through heat found that morning types showed less sensitivity to pain than evening types throughout the day.4 In a cross-sectional study of 397 nurses, nurses with evening chronotypes had a significantly increased prevalence ratio of WMSDs (1.32, 95% CI, 1.002–1.72) compared to those with morning chronotypes.5 In patients with fibromyalgia, evening types had increased symptom severity and a poorer quality of life compared to morning types. There are significant correlations between the MEQ, World Health Organization Questionnaire on Quality of Life, and Fibromyalgia Impact Questionnaire scores.6 As in previous studies, here, MTWs showed a significant association with low pain complaint ratios.
There are studies that chronotype is related to not only musculoskeletal pain but also psychological or neurologic pain. Several studies have shown a relationship between the evening chronotype and restless leg syndrome. In a study of 1,253 nurses and midwives, the OR for restless legs syndrome was significantly higher in evening types compared to morning types (OR, 1.95; 95% CI, 1.29–2.94).7 In a 590 Korean high school student study, the OR for restless leg syndrome was significantly higher in students with evening chronotype after adjusting for confounders (OR, 1.95; 95% CI, 1.15–6.43).25 Restless legs syndrome has mechanisms such as sleep disturbance, psychological distress, genetic factors, dopaminergic dysfunction, or central sensitization, which is partly consistent with the mechanisms of musculoskeletal pain.26
The mechanism of this study result has the following possibilities. First, there is a possibility that the effect of sleep played an intermediating factor. Chronotype is closely related to sleep behavior. According to chronotype, there are differences in various sleep-related factors such as sleep quality, sleep onset time, and sleep duration. In addition, sleep is a well-known factor influencing musculoskeletal pain. There is a possibility that the difference in sleep-related factors may have become mediators affecting musculoskeletal pain. A person with poor sleep quality on a day will experience increased pain the next day.27 It is estimated that 50%–88% of patients with chronic pain suffer from inadequate sleep. Not only does pain disturb sleep, but symptoms of insomnia often precede the onset of pain in patients with conditions such as fibromyalgia, musculoskeletal pain, and headaches.28 Musculoskeletal pain causes sleep disruption, and individuals with WMSDs that interfere with sleep often report experiencing more pain. Patients have the potential to lower their sensitivity to pain by getting enough sleep and paying off sleep debts on time.29 Second, the differences in chronotypes are not just differences in personal psychological preferences and life patterns. In several studies, there is a difference in chronotype according to the gene polymorphism,30 and among them, polymorphism of the clock gene PER3 was confirmed to be related to the circadian pattern of the descending pain modulatory system.31 Dysfunction of this descending pain pathway plays an important role in chronic pain.32 Based on these facts, dysfunction of the descending pain pathway can be suggested as a mechanism supporting the relationship between chronotype and musculoskeletal pain in this study. Third, hypothalamic-pituitary-adrenal (HPA) axis may play an factor in the regulation of pain.33 Cortisol is a well-known stress hormone that generally plays a protective role against pain. In chronic pain, dysfunction of the HPA axis may increase the sensitivity of musculoskeletal pain.34 Meanwhile, the HPA axis exhibits a circadian rhythm and thus may also be related to chronotype.353637 In one study, differences in salivary cortisol according to chronotypes were demonstrated.38 However, in this study, there was no significant difference in cortisol concentration according to chronotype. It may also be a result of a relatively small number of samples. A larger and more detailed study will be needed in the future. Another hypothesis is that the chronotype may have directly or indirectly influenced the morbidity of the actual incidence of musculoskeletal disorders. Work adaptations of workers may differ according to their chronotypes. In a previous study, morning-type chronotypes show higher adaptation in the morning shift,39 and a study by Rosa et al.'s suggests40 that early-type workers show the highest level of psychomotor performance regardless of shift. Maladaptation or low performance of late-type workers may have resulted in work-related injury or increased workload, leading to the incidence of actual musculoskeletal disorder. Additional studies on the association between chronotype and work-related injury may clarify this relationship.
Studies across several countries have determined that the MEQ is a reliable measure. Its reliability coefficient ranges from 0.78 to 0.86, and it has a strong stability over a 3-month period (0.88–0.89). However, the MEQ does have some limitations. Most importantly, the scale contains 19 items and may be considered lengthy in some situations. To overcome this limitation, the rMEQ was developed. This scale contains 5 items and is considered a pure measure for morning types. Several studies have reported that the rMEQ and MEQ show satisfactory to good correlation (0.69–0.90) and have good validity. The rMEQ discriminates between morning and evening types based on objectively recorded motor activity.1 In this study, the rMEQ was used. Although the validity of the rMEQ has been proven, we propose that a study that uses the full MEQ is still needed in future.
This study had the following limitations. First, due to the limitations of cross-sectional studies, it was not possible to determine if there was a precise causal relationship. Second, there is a limitation due to the characteristics of the study participants. This study was conducted in a university hospital and focused exclusively on a specific occupation in a factory (automobile manufacturing workers). Therefore, it may be difficult to generalize this information to the entire population. This study only targeted men who performed shift work; thus, persons who work in different types of fields, as well as women, should be studied in future. Third, this study is a questionnaire-based study, which can lead to information bias. In addition, although the symptoms and signs of musculoskeletal disorders were investigated through questionnaires extracted from the Korea Occupational Safety and Health Agency (KOSHA) guide used for legal examination of risk factors of musculoskeletal disorders, there may be limitations as these are not for research purposes. Thus, objective data (Industrial Accident Certification Data, objective medical data, etc.) should be used to verify whether participants were simply less sensitive to pain or whether there was an association with a serious musculoskeletal disorder. Fourth, it is possible that workers with severe musculoskeletal disorders were already excluded from the study due to the healthy worker effect. Fifth, because this study had a small sample size, sub-analysis according to the area in which the pain was felt and the degree of pain could not be performed. In this study, the results for musculoskeletal treatment were not statistically significant. We propose that this was due to the small sample size. Larger-scale research should be performed in the future. Lastly, we could not analyze the detailed tasks performed, which are important factors in musculoskeletal disorders. According to the subdivision classification, there may be differences in worker's tasks, which may have had a significant effect on musculoskeletal pain. Although detailed ergonomic evaluation could not be performed, it could be considered that the subjects of this study have some homogeneity as assemblers of a production line in a factory. Nevertheless, this study had great strengths. It is the first Korean study to demonstrate the relationship between chronotype and musculoskeletal problems in workers who perform tasks that have a high musculoskeletal burden. Another advantage is that various factors that affect musculoskeletal problems were considered (Table 3). Moreover, although a relatively small number of participants were enrolled, a significant relationship was found.
In general, chronotype is said to be an innate factor, and it is one of the personal characteristics that is difficult to change. It may not be possible to change the chronotype completely, but it may be possible to reduce its effect. Although the study participants were limited to adolescents, the previous study showed that interventions could modify the effects of the eveningness chronotype and improve sleep and circadian function.41 In addition, rather than changing the chronotype, an approach that improves work-related factors according to the individual chronotype of the worker can be considered. Depending on the chronotype, adjusting the musculoskeletal burden of the tasks or making a difference in the distribution of shifts could be a possible intervention.38 This study demonstrates the possibility that well-designed, evidence-based interventions may reduce the risk of WMSDs. We hope that various, larger-scale, follow-up studies will be conducted in future.
CONCLUSIONS
In this study, MTWs had a significantly lower proportion of musculoskeletal pain compared to NTWs. Chronotype could play an important role in WMSDs. Further, larger-scale, follow-up studies on chronotypes should be performed to prevent musculoskeletal disorders in future.
ACKNOWLEDGEMENTS
We thank all of the members of the Health Promotion Center at Chonnam National University Hwasun Hospital. We also thank the workers for their voluntary participation.
Notes
Competing interests: The authors declare that they have no competing interests.
Authors contributions:
Conceptualization: Kim S, Park WJ.
Data curation: Cho S, Kang KW.
Investigation: Yoo Y, Kim H.
Formal analysis: Lim DY, Kang W.
Writing - original draft: Kim S.
Writing - review & editing: Park WJ, Moon JD.
Abbreviations
BEPSI
Brief Encounter Psychosocial Instrument
BMI
body mass index
CI
confidence interval
HDL
high-density lipoprotein
HPA
hypothalamic-pituitary-adrenal
ISI
Insomnia Severity Index
LDL
low-density lipoprotein
MTW
morning-type worker
NTW
neither-type worker
OR
odds ratio
rMEQ
reduced Morningness-Eveningness Questionnaire
ROK
Republic of Korea
WMSD
work-related musculoskeletal disorder