Ethylene oxide burn in a chemical plant worker: a case report
Article information
Abstract
Background
Ethylene oxide is a chemical agent that is widely used for the sterilization of medical equipment and the manufacture of chemicals. Although ethylene oxide burns are frequent and can be severe, many workers are unaware of their risks.
Case presentation
A 45-year-old man presented with painful exudative lesions on the right foot after working with ethylene oxide solution in a chemical plant. The patient stated that the solution had percolated through his shoe and he had not washed the solution off for 5 hours. Symptoms, including pain and erythema, appeared after a delay of more than 12 hours from the time of initial exposure. The skin of his right foot was irrigated with saline and covered with a wet dressing and topical antibiotics in the emergency department. The patient was followed up for 4 weeks at an outpatient clinic.
Conclusions
Ethylene oxide causes skin irritation, dermatitis, and burns in severe cases. Since skin reactions can be delayed for more than 12 hours after exposure, it is important to remove contaminated shoes and clothing immediately and wash the exposed area even in the absence of symptoms. It is also necessary to provide the appropriate protective equipment and educate workers on the dangers of ethylene oxide.
BACKGROUND
Industrialization has markedly increased the use of chemical substances. The chemical industry has expanded from energy and petrochemical fields to high-tech domains with rapid advances, such as semiconductors, fine organic chemistry, nanoparticles, and diverse types of chemical product development.1 With the surging use of toxic substances, chemical exposure and incidence of occupational injuries have increased. These substances cause acute and chronic health problems in the skin, mucosa, respiratory, cardiovascular, and nervous systems.
Burns are known to be caused by approximately 200,000 chemicals, including ethylene oxide (EO), hydrofluoric acid, phenol, and wet cement.2 These often occur in occupational settings and can lead to more severe tissue damage, scarring, and pigmentation compared to thermal burns. In thermal burns, proteins coagulate quickly due to crosslinking; in contrast, chemical burns induce physiological protein denaturation through a combination of the six different processes, namely reduction, oxidation, corrosion, vesication, desiccation, and protoplasmic poisoning.3
EO is used as a medical equipment sterilizer and as an intermediate for manufacturing ethylene glycol, surfactants, ethanolamine, cosmetic products, detergents, emulsifiers, and plastics. Thus, hospital staff and plant workers may be at risk of occupational exposure.45
Handling EO requires significant care as it is an irritant to the eyes, respiratory system, and skin, and it can even suppress the central nervous system at high concentrations. Direct contact with diluted and concentrated solutions causes characteristic burns. Edema, erythema, blisters, and bullae form 1–5 hours after contact, eventually leading to desquamation.6 Additionally, The International Agency for Research on Cancer has designated it as a group 1 carcinogen with confirmed carcinogenicity in humans.789
In Korea, a case of reversible cerebral vasoconstriction syndrome following EO gas exposure has been reported,10 yet there have been no reports on chemical burns. Despite the wide use of EO in numerous industries, seeking medical attention is often delayed. Physicians are often unaware of the cause of these injuries and EO burns may appear several hours after direct skin contact, delaying decontamination, especially in asymptomatic cases. These can exacerbate the injury and cause complications. Therefore, preventive approaches are crucial. We present a case report of chemical burns caused by direct EO contact in a plant that produces surfactants and concrete hardeners.
CASE PRESENTATION
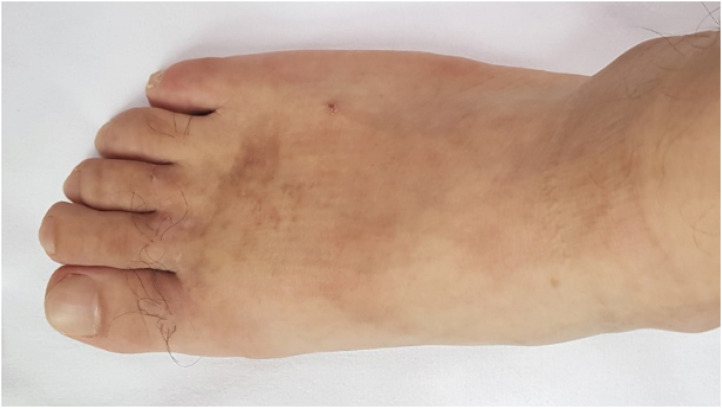
A 45-year-old male patient, without any past medical conditions, presented with a severe burning sensation on the hallux, 2nd, 3rd digits, and dorsum of the right foot. The patient, who works in a chemical plant, was replacing a worn-out flowmeter connected to the EO tank. The patient was not wearing personal protective equipment (PPE), such as chemical-resistant clothing and shoes. According to the Material Safety Data Sheets, EO is supplied through an automatic isolation line. During the incident at 2 PM, a large amount of water mixed with EO solution spilled on his right shoe. The patient did not experience any immediate symptoms and continued working with the wet shoe until approximately 5:30 PM. He returned home around 7 PM (approximately 5 hours after the exposure) and took a shower, effectively decontaminating the region. The next morning, the patient woke up to a severe burning sensation and pain in the dorsum of the right foot and proximal area of the digits. He discovered desquamation, redness, and oozing. The patient then presented to a nearby hospital (Fig. 1).
The patient did not provide any specific family history and was not under treatment for any disease or condition. He reported a smoking habit (10 pack-years) with occasional social alcohol consumption.
The patient had worked in restaurants since his mid-20s. Since 2013, he had been employed at a chemical plant for trial runs of facilities and indicator system maintenance and repair. In 2018, he started to work in production of basic petrochemicals such as surfactants and concrete hardeners. He was responsible for the EO supply from the ingredient tank to the production line, replacement of indicator systems, and facility maintenance. Typically, there is no risk of EO exposure, as it is supplied through an automatic isolated pipeline, but workers may be exposed during the replacement of indicator systems.
The patient had stable vital signs within the normal limits and was alert. However, the patient appeared acutely ill at presentation and had subcutaneous tissue damage on the right dorsum of the foot and digits, with severe redness and dark pink dermal surfaces, serosanguineous exudates, blisters, and desquamation (Fig. 2). The burn area was calculated to be 3.5% of the total body surface area. He did not report dyspnea and had clear breathing sounds upon auscultation.
Hematological analyses (complete blood count, blood chemistry), urinalysis, and plain chest radiograph performed at the emergency department were all within the normal limits.
The area was irrigated and disinfected. Topical antibiotics, silver sulfadiazine, was applied to unhealed burn wounds to protect the burn from becoming infected and the patient was followed-up in the outpatient clinic for 4 weeks. Normal skin was restored without any defects, and at the 9-month follow-up, there were no notable findings in the area other than hyperpigmentation (Fig. 3). At a general health assessment 9 months after the incident, the patient reported reduced sensation in the right foot. After an outpatient consultation at our department of occupational and environmental health, he was referred to hematology-oncology, pulmonology, and neurology. There were no abnormal findings in the peripheral blood smear, bronchial provocation test, nerve conduction study, and electromyography. Follow-up was therefore concluded.
For this study, we obtained approval from the Institutional Review Board (IRB) of Dankook University Hospital (IRB No. 2021-05-009).
DISCUSSION AND CONCLUSION
EO is a cyclic ether that exists as a gas at room temperature and thus, is commonly referred to as EO gas. It is soluble in water and most organic solvents, easily penetrating porous substances. It is involved in the alkylation of terminal carboxyl, amino, sulfhydryl, and hydroxyl groups of proteins.11 Since it is highly reactive, exposed organs can be severely damaged. EO induces nausea, vomiting, irritation of the respiratory tract (pharynx, larynx, trachea, and lungs), and inflammation of the eyes, even corneal burns in severe cases.5 EO suppresses the central nervous system, and exposure to a high concentration can induce convulsions and coma. Chronic exposure has been reported to induce multiple neuropathies, particularly reduced vibratory sensation in the lower limbs that gradually spread to the upper limbs and other areas.12 Direct contact with gaseous or liquid EO may cause irritation, redness, vesicular and crusting ulcers, as well as burns in severe cases.9 In general, organic solutions damage tissues by dissolving their lipid membranes, thereby hindering the physiological processes of the skin.13
Since reports and studies of EO burn are not common, it is a limitation of this paper that the studies we cite are outdated. Previous studies show that cases of EO burns were mainly reported in hospitals. LaDage reported a case of facial burns caused by an anesthesia mask sterilized by EO gas,14 and Biro et al. reported cases of buttock and back burns in postoperative patients after contact with EO-sterilized reusable surgical gowns and drapes.15 Fisher reported a case of hand burns caused by EO-sterilized gloves,16 and Cardenas-Camanena reported a case of burns caused by inappropriately ventilated EO-sterilized breast implants.17 Karacalar and Karacalar18 reported a chemical burn caused by an EO-sterilized blood pressure cuff. The burns in our case occurred in a chemical plant, suggesting that special precautions are necessary not only in the healthcare field but also among workers in industries that heavily utilize EO, such as chemical product synthesis and manufacturing industries.
The typical skin injuries caused by EO include edema, erythema, and tenderness that occur after 1–5 hours of latency. Some patients develop urticaria, and in severe cases, vesicles may form after 6–12 hours. Skin scaling occurs 8–10 days after exposure and the burns usually heal within 21 days, often leaving behind some pigmentation.9 Unlike thermal and acid burns, EO burns are asymptomatic or mildly symptomatic, thus, it is easy to be unaware of the burn for the initial several hours after exposure. The onset of symptoms may be further delayed by 12 hours or more after exposure to diluted EO, therefore close monitoring is necessary.19 In this case report, the patient was exposed to a highly diluted solution and continued working with the wet shoe for more than 3 hours. The patient did not experience any discomfort and performed decontamination 5 hours after exposure. Skin injury after EO exposure is related to the level of EO and the duration of contact. In general, the degree of tissue injury caused by chemical substances is associated with concentration, amount, and duration of contact. Experimentally, the minimum level of EO needed to cause skin irritation in non-sensitized subjects was approximately 1,000 ppm with 4 hours of continuous exposure.20 In addition, mechanical pressure and enclosed area of contact facilitate the penetration into tissues.18 In this case, EO was spilled onto a shoe, and because of the enclosed nature, direct skin contact was prolonged for several hours, and the pressure inside the shoe induced skin abrasions, thereby worsening the damage. Fast decontamination leads to a shorter duration of tissue contact, thus, even with high concentrations, the damage would be minimal.21 Shupack et al.20 reported that even high levels of EO (5,000 ppm) rarely caused damage in patch materials, such as fabric and rubber, from which EO can be quickly removed.
The Korea Occupational Safety and Health Agency recommends first aid for occupational EO exposure.19 Immediately upon exposure, clothes, and shoes must be taken off and exposed skin, eyes, and hair should be washed with clean water for at least 15 minutes. Because there is no antidote for EO, burns are treated empirically. If the patient shows respiratory symptoms or systemic toxicity after inhalation, 800 μg of beclomethasone dipropionate should be administered using a metered inhaler, and 1.0 g of methylprednisolone (or equivalent amount of steroid) should be administered intravenously. If EO is inhaled, humidified air or oxygen should be administered. These patients should be observed for at least 12 hours, with continuous vital signs and oxygen saturation monitoring, along with plain chest radiography, pulmonary function tests, and hematological tests (liver function, renal function, glucose, electrolytes). Eye exposure may lead to corneal burns, so these cases should be treated in the same manner as thermal burns and be immediately referred to an ophthalmologist, followed by a re-examination 24 hours later.
To prevent EO burns, handling techniques and thorough workplace management are crucial. In this particular case, an isolated EO pipeline was used, hence, exposure could have only occurred during repair and maintenance. Old flowmeters should be replaced, and the risk of exposure could be further lowered by wearing proper PPE against the residual EO in the flowmeter and pipe. Thus, education regarding workplace hazards and proper use of PPE must be provided to the workers to ensure their safety. In case of potential exposure, a self-contained breathing apparatus and gas mask, safety goggles, chemical-resistant clothing, shoes, and gloves should be worn. The patient in this case was not wearing chemical-resistant shoes, and the EO seeped in through the gap in the shoelaces. The accident could have been prevented with PPE.
Education and training are crucial for preventing occupational hazards. Workers should be aware of the properties of the chemicals they handle and how to administer first aid in case of exposure. When exposed to EO solution, a burn injury may develop after several hours even without symptoms immediately after exposure. Therefore, the importance of prompt decontamination must be conveyed to the workers. Delayed onset of symptoms coupled with the lack of awareness among patients regarding the properties of EO burns, leads to a delay in medical care that must ideally be sought immediately. Treatment delay can exacerbate deep tissue injury and increase the risk of systemic complications. Although there have not been many cases of EO burns reported in the Korean literature, it is estimated that a considerable number of burns actually occur in various industries. Despite the fact that these damages can be avoided, they occur often because of the lack of awareness. This calls for thorough safety management and education in the workplace.
In conclusion, EO burns are occupational hazards that must be dealt with in the field of occupational medicine. As engineering measures, isolation and ventilation are very effective measures. By isolating sources of EO exposure and installing local ventilation, individual exposure and concentration levels in the working environment can be reduced. Moreover, as occupational medicine deals with the management and prevention of workers with work-related injuries and illnesses, emphasis must be placed on the education of workers regarding safety protocols and timely medical care following occupational exposure to chemicals such as EO. Further, proper instructions and PPE on workplace hazards and their prevention should be provided to the workers.
Notes
Competing interests: The authors declare that they have no competing interests.
Authors contributions:
Conceptualization: Kim Y.
Data curation: Kim Y.
Formal analysis: Roh S.
Investigation: Kim Y.
Writing - original draft: Kim Y.
Writing - review & editing: Roh S.
Abbreviations
EO
ethylene oxide
PPE
personal protective equipment