Seroprevalence of measles, mumps, rubella, and varicella-zoster antibodies in new female nurses in the Republic of Korea
Article information
Abstract
Background
For health care workers, immune management plays an important role in the protection against infectious diseases. This study investigated the seroprevalence of measles, mumps, rubella, and varicella-zoster in newly employed female nurses.
Methods
We conducted a survey on the seroprevalence of measles, mumps, rubella, and varicella-zoster in newly employed female nurses at a university hospital from 2011 to 2019, before the nurses were given their department placements and duty start. Enzyme-linked immunosorbent and chemiluminescence immunoassays were used to detect immunoglobulin G antibodies. We analyzed whether there was a significant difference in seroprevalence depending on the age, birth year, birth season, and region of residence (metropolitan residency: yes or no).
Results
The arithmetic mean ages of the participants were 28.6 ± 4.8, 23.5 ± 3.2, 23.6 ± 3.0, and 26.1 ± 4.5 years for measles, mumps, rubella, and varicella-zoster, respectively. The seropositivity rates were 93.9% (551/587), 60.2% (50/83), 83.3% (3,093/3,711), and 89.5% (978/1,093) for measles, mumps, rubella, and varicella-zoster, respectively. Significant differences in the seroprevalence when assessed according to the age and birth year were noted with measles, while significant differences in the seroprevalence were only noted with rubella and varicella-zoster when assessed according to birth year and age, respectively.
Conclusions
In this study, we identified the levels of antibody prevalence in new female nurses. Considering the seropositivity levels, cost-effectiveness, and convenience for the participants, we recommend that the measles-mumps-rubella vaccination be provided without serologic testing for all new female nurses and the varicella-zoster vaccination only be performed for persons who are negative after serologic testing. And it would be useful if the vaccinations were combined with compulsory worker health examinations, such as the pre-placement health examinations.
BACKGROUND
In the Republic of Korea (ROK), legal infectious diseases are classified into four grades according to the Infectious Disease Control and Prevention Act, in which measles, mumps, rubella, and varicella-zoster are classified as grade 2 infectious diseases.1 These diseases must be reported to the public health center within 24 hours due to the possibility of transmission. Measles, mumps, rubella, and varicella-zoster can be spread through droplets, and measles and varicella-zoster are considered particularly dangerous because they can be spread through airborne transmission. The incidences of these infectious diseases are not particularly high in the ROK. Specifically, measles and rubella have been certified as eliminated by the World Health Organization (WHO).2 Nevertheless, small outbreaks still occur, mainly in the obstetrics and pediatric wards in hospitals. Thus, it is important that nosocomial infections must be managed because the transmission of these diseases is rapid and fatal.3
Health care workers are exposed to many types of infectious diseases. The routes of infection include blood, skin contact, medical waste, and air.456 When considered in the long term, infectious diseases also cause some occupational cancers (hepatitis B and C).7 In the ROK, the Occupational Safety and Health Act stipulates that employers must take measures to protect all workers, including health care workers, from the damage to health that is caused by exposure to pathogens. However, the specific methods of prevention and precise targets have not yet been determined.8 Moreover, the act recommends vaccinations for health care workers; however, they are not mandatory. The importance of protecting health care workers from infection is also evident when considered in terms of patient safety. Health care workers, especially nurses, have direct contact with multiple patients. Infected nurses could serve as sources of infection for other patients or health care workers. In immunocompromised patients, such an infection could be fatal. Thus, the immunization of health care workers is of higher priority than it is for other occupations. In previous studies that explored the seroprevalence of these diseases in the ROK, only the general population or health care workers without exact job classifications were included as participants. This study investigated the seroprevalence of measles, mumps, rubella, and varicella-zoster in newly employed female nurses before the nurses were given their department placements and duty start. Based on our findings, we aimed to provide a basis information for the decision of a health policy related to the vaccination of nurses.
METHODS
Study participants
The study participants were newly employed nurses at a university hospital aged between 21 and 40 years (dates of birth from January 1, 1980 to December 31, 1999). The study period was from 2011 to 2019. The participants were interviewed about their job histories by a physician before undergoing serologic testing. Participants who had previously worked as nurses in other hospitals were excluded from this study. The number of participants that were investigated for each antibody was as follows: 587, 83, 3,311, and 1,093 for measles, mumps, rubella, and varicella-zoster, respectively. The participants' ages and birth years were classified into four categories with equal intervals. Depending on their birth month, participants were classified into the spring (March–May), summer (June–August), fall (September–November), and winter (December–February) groups. Their residential information was divided into two categories, based on the metropolitan area in which they resided.
Serologic tests
Enzyme-linked immunosorbent assay was used to detect immunoglobulin G (IgG) antibodies against measles, mumps, and varicella-zoster. The following CHORUS kits were used in the Chonnam National University hospital laboratory: CHORUS Measles-IgG, CHORUS Mumps-IgG, and CHORUS Varicella-zoster-IgG (Diesse Diagnostica Senese Spa, Sienna, Italy). The rubella IgG antibody was outsourced to a different laboratory, Samkwang Medical Laboratories (Seoul, Korea), where chemiluminescence immunoassays were used. The Alinity Rubella-IgG (Abbott, IL, USA) serologic test kit was used. The quantitative cut-off values for seronegativity were < 0.8, < 0.8, < 5.0, and < 0.8 IU/mL for measles, mumps, rubella, and varicella-zoster, respectively. The seropositivity cut-off values were > 1.2, > 1.2, ≥ 10, and > 1.2 IU/mL for measles, mumps, rubella, and varicella-zoster, respectively. Values that were neither negative nor positive were defined as equivocal. The laboratories were qualified and certified by the Korean Society for Laboratory Medicine.
Statistical analyses
The arithmetic means and standard deviations for the participants' ages are presented for each serologic test. Pearson's χ2 test or linear-by-linear association were used to analyze the association between seroprevalence and age, birth year, birth season, and metropolitan area of residence. Participants whose addresses were missing (23, 76, and 24 in the measles, rubella, and varicella-zoster groups, respectively) were only excluded from the residential analysis. All statistical tests were performed using SPSS statistics software version 26.0 (SPSS, Inc., Chicago, IL, USA), and the significance level was defined as p < 0.05.
Ethics statement
We conducted a retrospective review of the participants' medical records. The participants' data were anonymized and stored in the Chonnam National University Hospital Clinical Data Warehouse. The data were used for research purposes in accordance with the Personal Information Protection Act. Each participant provided electronic informed consent regarding the collection and use of personal information before the checkup was conducted. The protocol of this study was approved by the Institutional Review Board (IRB) of Chonnam National University Hwasun Hospital (IRB number CNUHH-2020-136).
RESULTS
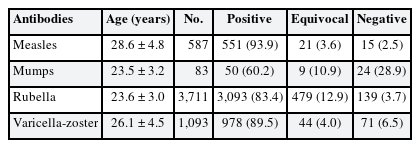
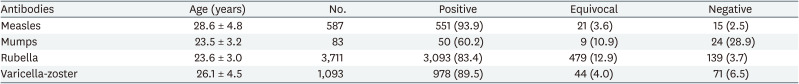
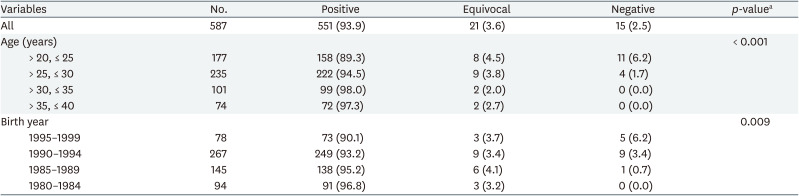
The participants' arithmetic mean ages and standard deviations were 28.6 ± 4.8, 23.5 ± 3.2, 23.6 ± 3.0, and 26.1 ± 4.5 years for measles, mumps, rubella, and varicella-zoster, respectively. The overall seropositivity was 93.9% (551/587), 60.2% (50/83), 83.3% (3,093/3,711), and 89.5% (978/1,093) for measles, mumps, rubella, and varicella-zoster, respectively. The proportion of seronegative participants was 2.6% (15/587), 28.9% (24/83), 3.7% (139/3,711), and 6.5% (71/1,093) for measles, mumps, rubella, and varicella-zoster, respectively. The proportion of equivocal participants was 3.6% (21/587), 10.8% (9/83), 12.9% (479/3,711), and 4.0% (44/1,093) for measles, mumps, rubella, and varicella-zoster, respectively (Table 1).
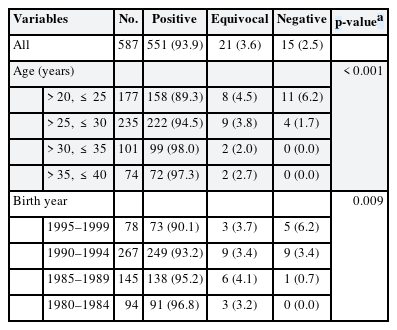
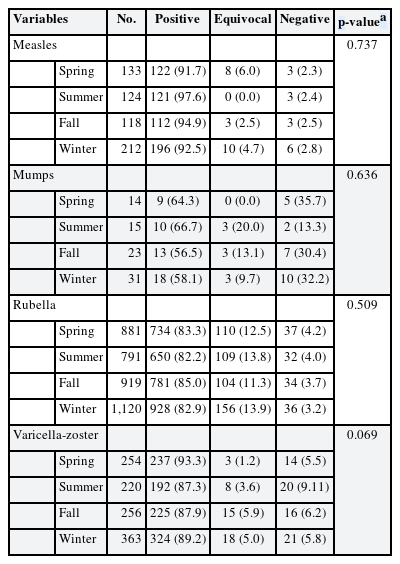
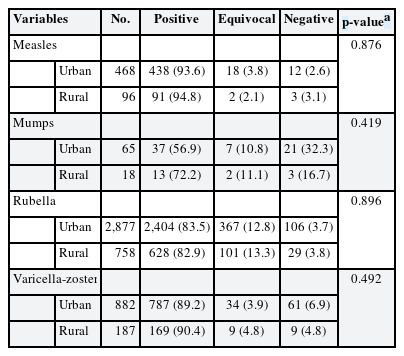
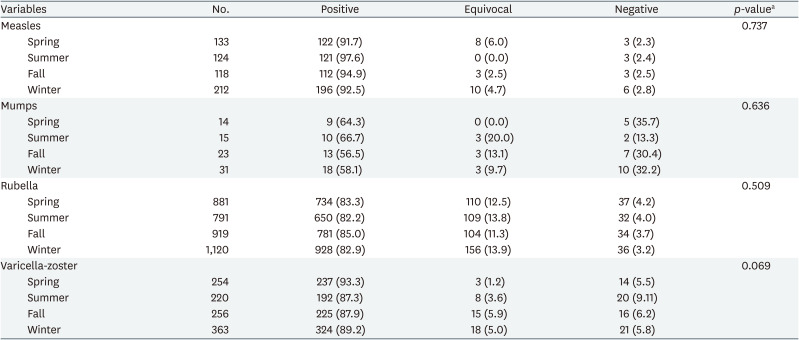
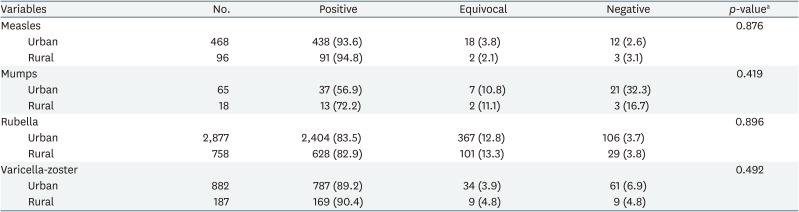
About measles, there were significant differences noted when the participants' ages and birth years were assessed. The seroprevalence was the lowest in nurses who were between the ages of 20 and 25 years (89.3%), and the highest in those aged between 30 and 35 years (98.0%). This difference was statistically significant (p < 0.001). The seroprevalence was the lowest in nurses who were born between 1995 and 1999 (90.1%), and the highest in those born between 1980 and 1984 (96.8%). This difference was statistically significant (p = 0.009; Table 2). There were no significant differences noted when the participants were assessed according to their metropolitan area of residence and birth season (Tables 3 and 4).
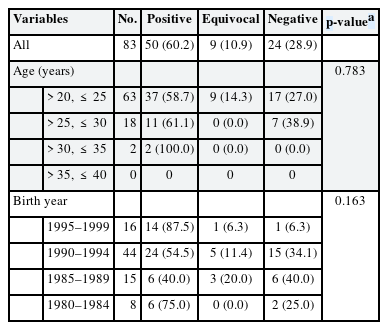
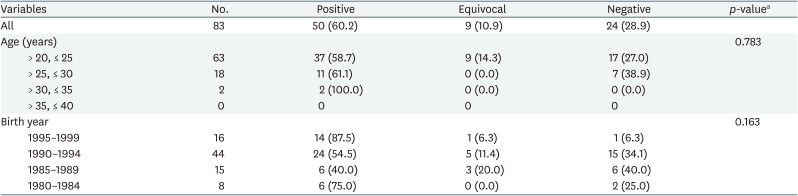
About mumps, there were no significant differences noted when the nurses were compared according to age, birth year, metropolitan area of residence, and birth season. The seroprevalence was the lowest in nurses who were between the ages of 20 and 25 years (58.7%), and the highest in those aged between 30 and 35 years (100.0%). However, this difference was not statistically significant (p = 0.783). The seroprevalence was the lowest in nurses born between 1985 and 1989 (40.0%), and the highest in those born between 1995 and 1999 (87.5%). However, this difference was also not statistically significant (p = 0.163; Table 5).
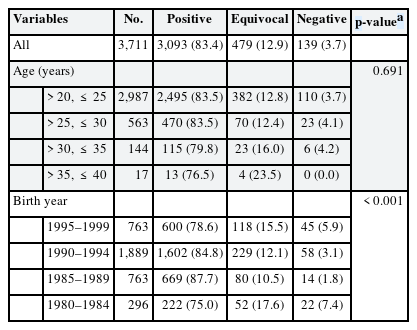
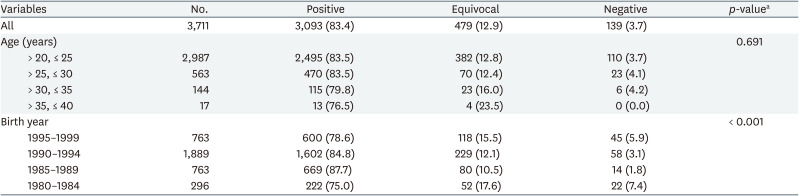
About rubella, there were significant differences noted when the participants were compared according to their birth year. The seroprevalence was the lowest in nurses who were between the ages of 35 and 40 years (76.5%), and the highest in those in those aged between 20 and 25 years (83.5%). However, this difference was not statistically significant (p = 0.691). The seroprevalence was the lowest in nurses born between 1980 and 1984 at (75.0%), and the highest in those born between 1985 and 1989 (87.7%). This difference was statistically significant (p < 0.001; Table 6). There were no significant differences noted when participants were assessed according to age, metropolitan area of residence, and birth season (Tables 3 and 4).
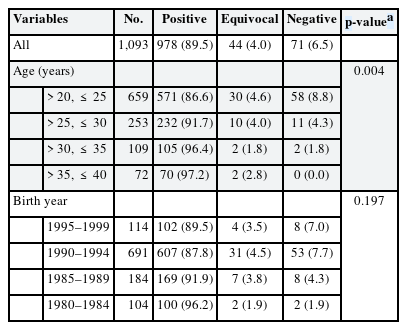
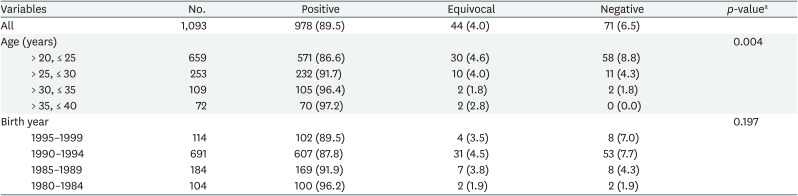
About varicella-zoster, there were significant differences noted when the participants were compared according to their ages. The seroprevalence was the lowest in nurses who were between the ages of 20 and 25 years (86.6%), and the highest in those aged between 35 and 40 years (97.2%). This difference was statistically significant (p = 0.004). The seroprevalence was the lowest in nurses born between 1990 and 1994 (87.8%), and the highest in those born between 1980 and 1984 (96.2%). This difference was statistically significant (p = 0.014; Table 7). There were no significant differences noted when participants were assessed according to birth year, metropolitan area of residence, and birth season (Tables 3 and 4).
DISCUSSION
Seroprevalence is influenced by several factors such as vaccination policies, age, birth year, birth season, sex, occupation, area of residency, and the presence of a health care manager at work or school.91011 In this study, it was confirmed that there are differences in the seroprevalence of some antibodies according to age and birth year. However, there was no significant difference in the prevalence of antibodies with the birth season and area of residence. Seropositivity varies depending on the worker's characteristics and social circumstances, even if vaccination is mandatory at their facility. In terms of vaccinations, measles, mumps, rubella, and varicella-zoster vaccinations are mandatory for all newborns in the ROK. The measles-mumps-rubella (MMR) combination vaccine was included as part of the National Immunization Program (NIP) that began in 1983. In 1997, it was expanded to a two-dose schedule. The first dose is administered at 12–15 months of age and the second dose at 4–6 years of age.12 The varicella-zoster vaccine was adopted in 2005 as part of the NIP, and children are vaccinated at 12–15 months of age.3
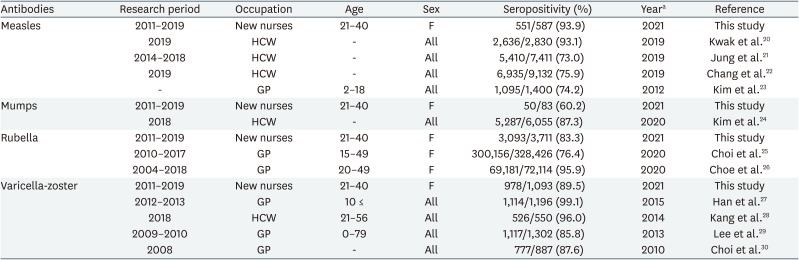
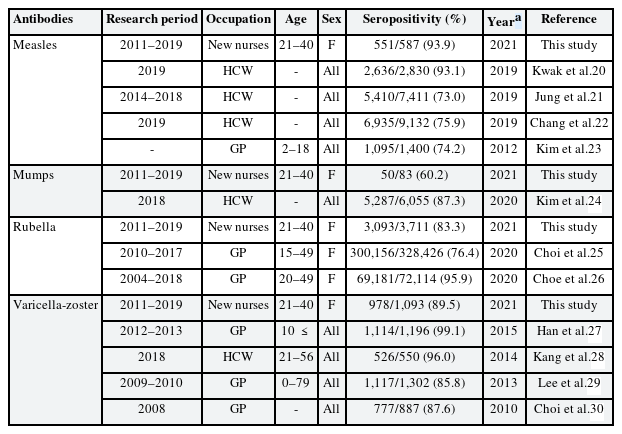
We compared our study findings to recent seroprevalence studies in the ROK. The seropositivity of measles varied between 73.0% and 93.9%. There was only one other study on the seroprevalence of mumps in the ROK; however, the results from that study differed greatly from our findings (60.2% vs. 87.3%). In terms of rubella, there were only studies that used participants from the general population in the ROK, and the seroprevalence varied between 76.4% and 95.9%. For varicella-zoster, the seroprevalence varied between 85.8% and 99.1% (Table 8). The results from this study demonstrated that the proportions of antibody formation among new nurses were not perfect. In general, the chain of infection is suppressed by herd immunity. The serologic crude herd immunity threshold varies from 91% to 94%, 86% to 93%, 83% to 94%, and 86% to 91% for measles, mumps, rubella, and varicella-zoster, respectively.13 These results demonstrate that herd immunity has already been achieved, except in the case of mumps. However, considering the risk of infection due to the large number of people who visit the hospital and the patients susceptible to infection, stricter management is essential. According to the Korean Labor Welfare Corporation database, infectious diseases are an important cause of occupational disease among health care workers.14 From 2004 to 2007, an increasing pattern in numbers of compensation was noted, with 48, 59, 61 and 68 cases in each consecutive year. Of these cases, 32, 42, 50, and 56 occurred in nursing and medical work.1516 In recent data, infectious diseases have accounted for a large proportion of occupational diseases in the health and social welfare sector. In 2018, of the 19 occupational disease cases, 15 were infectious diseases in the health and social welfare sector.17 The proportion of infectious diseases was similar in 2019. Of the 33 occupational disease cases, 26 cases were of infectious diseases.18 The total number of incidents is estimated at a higher value, including unreported cases and cases that were compensated by other pensions.14 In relation to pandemics, such as the coronavirus disease 2019 (COVID-19) outbreak, the number of infectious diseases among healthcare workers will further increase in the future.19
Comparison of the measles, mumps, rubella, and varicella-zoster seropositivity with previous study findings in the Republic of Korea
In the ROK, legal infectious diseases are classified into four grades according to the Infectious Disease Control and Prevention Act, which was revised from the existing 5 group classification in 2020. In the ROK classification, grade 1 infectious diseases include Ebola virus, severe acute respiratory syndrome, Middle East respiratory syndrome, COVID-19, and others., which are terroristic, fatal, or highly contagious diseases. If these diseases are diagnosed, they must be reported to the public health center immediately. Moreover, the infected patients should be isolated in a negative pressure environment. The infectious diseases that were included in this study were grade 2. Other grade 2 infectious diseases include tuberculosis, hepatitis A, and polio. These diseases must be reported to the public health center within 24 hours, and the patients should be isolated (a negative pressure environment is not compulsory). Grade 3 infectious diseases include hepatitis B and C, severe fever with thrombocytopenia syndrome, and tetanus. These diseases must be reported to the public health center within 24 hours; however, isolation is not compulsory. All instances of grade 1–3 infectious diseases are monitored through a mandatory surveillance system. Grade 4 infectious diseases, which are monitored through a sentinel surveillance system, include influenza virus, syphilis, and others.31
Between 2000 and 2001, there was a large measles outbreak in the ROK. In 2000, there were more than 32,000 recorded cases of measles. The Korea Disease Control and Prevention Agency (KDCA) determined that the level of herd immunity for measles was low and decided to implement the measles-rubella (MR) catch-up vaccine.3 Patients who received the vaccination were aged between 8 and 16 years (born between 1985 and 1993). The vaccinations were completed in 2001 with a vaccination rate of over 95%.32 Following the campaign, a significant decrease in the measles incidence was noted; thus, the ROK declared that measles had been eliminated from the country in 2006 and this declaration was authorized by the WHO in 2014.2 The criteria for the elimination of measles in the western pacific region according to the WHO are as follows: interruption of endemic measles virus transmission for a period of at least 36 months, the presence of verification standard surveillance, and genotyping evidence that supports the interruption of endemic measles virus transmission.33 While some small outbreaks have occurred since the declaration was made, these outbreaks have been attributed to imported viruses. Most recently, in 2019, there was an outbreak that was traced back to a hospital in Daegu. Eight of the 16 cases were adults, five of whom were health care workers from the same hospital.34 This outbreak was not considered a result of endemic viral transmission; however, it brought attention to the importance of immunization in hospitals. In this study, measles seropositivity tended to be lower in participants who were younger and born more recently. We considered that the results were affected by the higher incidence of measles in the older generations and influenced by the MR catch-up vaccine that was implemented in 2001. In the past, incidents of measles were common in the ROK, and the natural immunity rate was also high. When the MR catch-up vaccination was implemented in 2001, those born before 1984 were considered to have natural immunity, and the results from this study were consistent with this finding.35
Since 2002, researchers have noted an increase in the incidence of mumps in the ROK. Studies have reported two outbreaks after 2002. One outbreak occurred at a kindergarten in Ulsan, and the other occurred at middle/high schools in Daegu. Moreover, there was a mumps epidemic in 2013.36 In 2018, there were nearly 20,000 recorded patients with mumps. After the two-dose vaccination schedule became mandatory in 1997 as part of the NIP, the outbreaks have occurred more frequently among adolescents and young adults than among children.3 In this study, mumps had a significantly lower seropositivity compared with that found in other studies. There were no significant differences noted when it was assessed according to the variables. However, further evaluation of seroprevalence, which was divided into 2 categories (positive vs. equivocal and negative), demonstrated significant differences when mumps was assessed according to birth year. Participants who were born between 1995 and 1999 had the highest seropositivity, followed by participants who were born between 1980 and 1984 (p = 0.031).
Compared with other infectious diseases, rubella has mild symptoms; however, it can be harmful to pregnant women. It has a teratogenic effect, called congenital rubella syndrome, that is particularly significant in the first trimester. In 2001, in the ROK, there were 128 recorded cases of rubella. It was registered as a legal infectious disease in 2000, and the MR catch-up vaccination schedule was implemented in 2001. Thereafter, the number of new cases decreased to 11 cases between 2014 and 2017, and the patients were mainly infants. There were no official rubella cases recorded in the ROK in 2018.3 Thus, rubella was also declared eliminated in the ROK and certified as such by the WHO in 2017.2 The criteria for the elimination of rubella in the western pacific region according to the WHO are as follows: interruption of endemic rubella virus transmission for a period of at least 36 months, the presence of verification standard surveillance; and genotyping evidence that supports the interruption of endemic rubella virus transmission.33 Rubella rarely occurs in the ROK; however, vaccinations are still important due to the high number of female nurses of child-bearing age. It is also important because some nurses work in departments with vulnerable patient groups, such as obstetrics and pediatrics. Our study found that the birth year was associated with the seroprevalence of rubella. Unlike the findings for measles, age was not a significant factor that affected the seroprevalence of rubella. However, the cluster of birth years that were considered the middle (those born between 1985 and 1994) had a high seropositivity in this study. In 2001, the MR catch-up vaccine was provided for those born between 1985 and 1993. We propose that the seroprevalence was affected by this catch-up vaccination and that the catch-up vaccination was effective in facilitating the formation of measles and rubella antibodies in those who received it.
In the ROK, the incidence of varicella-zoster is increasing pattern. In 2018, there were 96,467 cases recorded. It was registered as a legal infectious disease in 2005. Its incidence peaks during April–June and November–December, and it mainly occurs in children aged between 4 and 6 years and those in elementary school.3 In this study, the older age groups had a higher varicella-zoster seroprevalence. A similar tendency, that was statistically significant, was demonstrated with the past birth year group when the serologic test results were classified into two categories (p = 0.046). Participants who were born between 1980 and 1984 had the highest seropositivity, followed by participants born between 1985 and 1989. We considered that these findings were affected by the higher incidence of the disease in the past; however, there was no detailed information available on varicella-zoster in the ROK before 2005 because it was only registered as a legal infectious disease in 2005. Varicella-zoster vaccinations have been mandatory since 2005, as per the NIP, and children are vaccinated at 12–15 months of age. Therefore, the varicella-zoster seroprevalence for our study's participants was not considered to be related to the vaccination.3
This study had some limitations. First, there was the possibility of selection bias. This research was conducted in a hospital. Therefore, the generalizability of this information to other hospitals or regions may be limited. Particularly since the NIP is somewhat different when compared with systems used in other countries; thus, its principles cannot be applied to other countries. Second, the number of participants for each antibody test was not the same. There were few participants in the mumps group (n = 83). Due to this, there is a point that mumps is difficult to see as a representative data. Third, the study period was long. The investigative period for this study was 9 years in duration and, during this time, various circumstances may have changed both inside and outside the hospital. Fourth, the differences in the immunization policies for student nurses between schools have influenced the outcomes. Some schools have compulsory vaccinations before the student nurses are allowed to practice, while others do not. A unified guideline for this requirement should be developed in future. Fifth, only women were included as study participants; however, the proportion of male nurses is increasing.37 Research that includes men should also be conducted in the future. Despite these limitations, to the best of our knowledge, this is the first study on the baseline seroprevalence of measles, mumps, rubella, and varicella-zoster among newly employed nurses in the ROK. As mentioned before, previous studies only involved the general population or health care workers who were already working in hospitals. Furthermore, previous studies did not include information on specific health care workers' occupations. For this reason, a strength of this study is that the results may prove helpful in developing an immune management policy for new nurses.
A report by the Korea Occupational Safety & Health Agency (KOSHA) recommended that all health care workers be vaccinated against airborne diseases and those transmitted through droplet spread, such as measles, mumps, rubella, and varicella-zoster.38 In the KDCA guidelines for adult immunizations, two doses of the MMR vaccination are recommended without serologic tests being performed. Moreover, the varicella-zoster vaccination is recommended when evidence of immunity is absent. Evidence of immunity is defined as a history of disease, seropositivity, or vaccination history.35 Considering the cost-effectiveness and convenience for the participants, in the case of the MMR vaccine, vaccination without requiring serologic tests should be effective in practice. In 2021, in the ROK, serologic tests cost approximately 30–33 thousand Korean Republic won (KRW) for each antibody (about 27.2–29.9 United States Dollars [USD]), while each vaccination is approximately 18–20 thousand KRW (about 16.3–18.1 USD). Specifically, the MMR vaccination is 2.5 times cheaper than the entire serologic test, even if the two-dose schedule is used. The MMR vaccine has a low incidence of adverse effects.38 And although the occurrence is rare, phlebotomy can cause nerve damage, vasovagal reactions, and infections.39 Therefore, it is safer to vaccinate without performing serologic tests that require blood samples.
CONCLUSION
In this study, we identified the levels of antibody prevalence among new female nurses when they joined hospitals. Our study demonstrated that the proportions of antibody formation among new nurses were not perfect. Considering the seropositivity levels, cost-effectiveness, and convenience for the participants, we recommend that the MMR vaccinations be performed without serologic testing for all new female nurses and that varicella-zoster vaccinations only be performed for participants who are negative after serologic testing. This is consistent with the KDCA guidelines. Moreover, we propose that it would be useful if the vaccinations were combined with compulsory worker health examinations, such as the pre-placement health examinations.
ACKNOWLEDGEMENTS
We thank all the members of the Health Promotion Center at Chonnam National University Hwasun Hospital. We thank all the members of the Department of Occupational and Environmental Medicine at Chonnam National University Hospital. We sincerely thank the nurses for their participation in this study and wish them healthy work.
Notes
Competing Interests: The authors declare that they have no competing interests.
Author Contributions:
Conceptualization: Yoo Y, Park WJ.
Data curation: Cho S, Kang KW, Kim H.
Formal analysis: Kim S, Lim DY.
Investigation: Kim S, Yoo Y.
Writing - original draft: Yoo Y.
Writing - review & editing: Park WJ, Moon JD.
Abbreviations
COVID-19
coronavirus disease 2019
GP
general population
HCW
health care workers
IgG
immunoglobulin G
KDCA
Korea Disease Control and Prevention Agency
KOSHA
Korea Occupational Safety & Health Agency
KRW
Korea Republic won
MMR
measles-mumps-rubella
MR
measles-rubella
NIP
National Immunization Program
ROK
Republic of Korea
USD
United States Dollars
WHO
World Health Organization