Association between nicotine dependency with occupational injury in Korean men
Article information
Abstract
Background
The relationship between smoking status or second-hand smoking and occupational injuries has been the subject of considerable study, but few have studied the relationship between nicotine dependence and occupational injuries. The objective of this study was to investigate the relationship between nicotine dependence and occupational injury among employees at a range of Korean companies.
Methods
Initially, the personal and occupational characteristics and nicotine dependences of workers were measured, and 12 months later a survey was used to determine whether subjects had experienced any occupational injury. This study was conducted in several workplaces on 6,893 male workers in manufacturing and service industries that received health screening at Inha University Hospital in Incheon.
Results
The adjusted odds ratios (ORs) of occupational injury in the low, moderate, and high nicotine dependence groups were 1.38 (95% confidence interval [CI]: 1.04–1.84), 1.52 (95% CI: 1.10–2.10), and 1.71 (95% CI: 0.92–3.19), respectively. For smokers only, adjusted ORs tended to increase linearly (p for trend < 0.05). When only smokers were included, analysis of continuous FTND (Fagerstrom Test of Nicotine Dependence) scores showed that adjusted OR increased by 1.10 (95% CI: 1.03–1.19) per FTND point. After stratifying the data by working type and working hours per week, the non-shift work group maintained this relationship (OR: 1.13, 95% CI: 1.04–1.24) and OR was higher in the group that works more than 60 hours per week with FTND score as a continuous variable (OR: 1.24, 95% CI: 1.07–1.44).
Conclusions
The study shows nicotine dependency might affect occupational injury. From a short-term perspective, addressing worker's nicotine dependence by giving an adequate break time or smoking area might reduce work-related injuries.
BACKGROUND
According to the Industrial Accident Status Analysis conducted by the Korean Ministry of Employment and Labor, 19,073,438 workers at 2,654,107 workplaces applied for Industrial Accident Compensation Insurance 2018, and that 102,305 cases requiring more than 4 days of convalescence an accident rate of 0.54%. Among the cases that required convalescence, there were 2,142 deaths, 89,588 occupational accidents, and 10,302 occupational diseases. Thus overall costs and labor losses associated with occupational accident are considerable [1].
Many studies have described risk factors of occupational accidents or injury. These range from individual factors such as gender, smoking, and drinking [2345], to occupational factors such as exposure to physical and chemical hazards and unsafe working [236], and relationships between some risk factors and occupational injuries have been demonstrated. Recently, it was been reported that psychosocial factors, organization structures, and culture may also have significant impacts on occupational injury rates [78]. In this study, we focused on the relationship between nicotine dependency and occupational injury.
According to the National Health and Nutrition Survey conducted by the Korea Centers for Disease Control and Prevention in 2017, 38.1% of adult Korean men smoke, which is the highest level among OECD countries [9]. Smoking has been shown to have detrimental effects on almost all organs, including the respiratory and cardiovascular systems, and to cause many diseases and deaths [10]. In addition, smoking has been reported to increase the risk of accidental [11]and occupational injuries [121314], as has indirect smoking [1516]. However, the majority of studies conducted to date have been cross-sectional studies, and thus, have been limited in terms of determining causality. Furthermore, few have investigated the relationship between nicotine dependence and work-related injuries.
It is meaningful that the relationship between nicotine dependence and occupational injury be clarified, because smoking and nicotine dependency are correctable factors. Therefore, we conducted the present study to determine the relationship between nicotine dependence and occupational injury by surveying Korean men with different types of jobs.
METHODS
Data and study population
This study was conducted in varied workplaces in accommodation, manufacturing, aviation, and others that received health screening at a university hospital in Incheon. Of the total 10,482 workers, 8,097 male workers were included in the study; 2,385 women were excluded because of their low smoking rate. The first survey was conducted in 2012 to fill out a self-reporting questionnaire details on socio-demographic characteristics, occupational characteristics, and occupational injury. In addition, the Korean version of the Fagerstrom Test of Nicotine Dependence (FTND) questionnaire, which consisted of six questions, was administered. The second survey was conducted from 2013 to 2015 and it included details of experiences of occupational injury over the previous 12 months. The analysis was conducted on 6,893 (85.1%) subjects because 1,204 (14.9%) workers failed to assess the second survey or incomplete response. The study protocol was approved by the institutional review board of Inha University Hospital. All responders provided informed written consent.
Specific details of the primary survey questionnaire (personal characteristics, occupational characteristics, nicotine dependence) and the secondary survey questionnaire (occupational injury experience) were as follows: personal characteristics (age, marital status, education status, chronic disease (stroke, heart disease, hypertension, diabetes, hyperlipidemia, etc.), alcohol consumption (‘heavy’ alcohol consumption indicated at least seven glasses of alcohol two or more times per week), smoking status, and nicotine dependence); and occupational characteristics (occupational classification, employment status(regular or temporary), working type (shift, non-shift), job tenure (< 1, 1–4, 5–9, ≥ 10 years), and working hours per week (< 40, 41–59, ≥ 60).
Nicotine dependence
Nicotine dependence was assessed using the FTND. The FTND is usually used to provide quantitative measures of nicotine dependence, and the version modified by Heatherton et al.[17] is commonly used today and was used in the present study [18]. The FTND questionnaire consisted of six questions. ‘After you wake up, how soon do you smoke your first cigarette?,’ ‘Do you find it difficult to refrain from smoking where it is forbidden?,’ ‘Which cigarette would you hate most to give up?,’ ‘How many cigarettes do you smoke per day?,’ ‘Do you smoke more during the first hours after waking up than during the rest of the day?,’ ‘Do you smoke even when you are ill enough to be in bed?.’ Scores are summed and used to classify nicotine. In this study, those with total score of 0–3, 4–6, ≥ 7 were allocated to a low, moderate, and groups high nicotine dependence groups.
Occupational injury
Occupational injury was defined as an injury requiring hospital treatment for a work-related accident over the previous 12 months, and was determined when a subject answered “Yes” to the question, “Have you received hospital treatment for a work-related injury during the last 12 months?”
Statistical analysis
We generated descriptive statistics for the overall study population, as well as variables stratified by working type and working hours. Also, we divided subjects into cases consisting of only current smokers (FTND score in 3 groups) and cases including non-smokers (Non-smoker & FTND score in 3 groups), and analyzed separately. The chi-square test was conducted to analyze differences between occupational injuries over the previous 12 months with respect to personal (age, marital status, education, chronic disease, drinking habits, smoking habits, and nicotine dependence) and working characteristics (industry classification, employment status, working type, job tenure, and working hours per week, etc.). Adjusted odds ratios (ORs) were calculated by binary logistic regression after adjusting for potential confounders (age, marital status, educational status, chronic disease, alcohol consumption, occupational classification, employment status, working hours) that were significant in correlation analysis with occupational injury or main independent variables. In addition, we analyzed FTND scores as continuous variables to determine whether the risk increases as the nicotine dependency increases for current smokers only. The analysis was conducted using SPSS v.18.0 software.
RESULTS
General characteristics
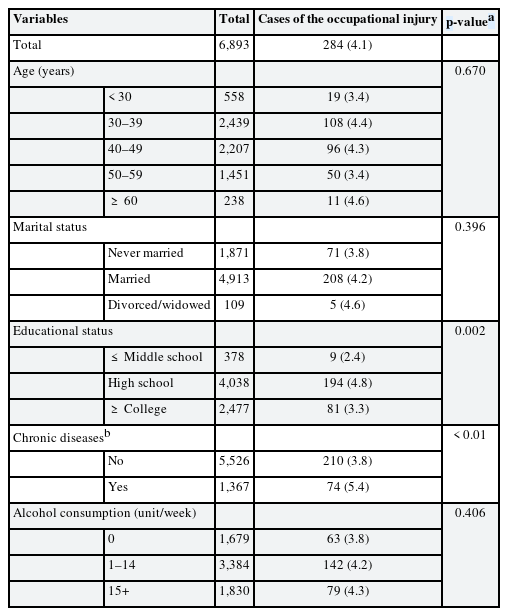
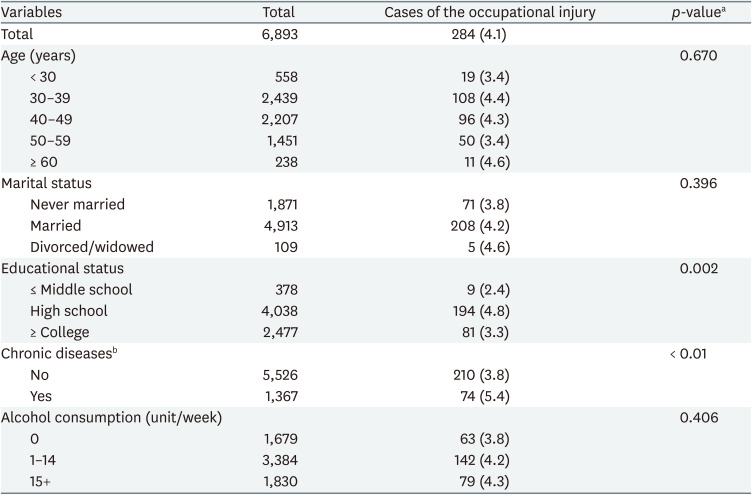
Table 1 shows the relationship between general characteristics and occupational injury rates. In terms of occupational injury rates, those with a high school or college education were had higher rates of 4.8 percent and 3.3 percent, respectively, and these were followed by those with less than junior high school education had a rate of 2.4 percent (p < 0.05). The rate of occupational injury was significantly higher for those with a chronic disease (5.4%) than for those without (3.8%) (p < 0.01). Occupational injury rates were not significantly dependent on age, marital status, or drinking habits (Table 1). The rate of occupational injury was significantly high in the group that works more than 60 hours per week (9.1%) (p < 0.05) (Supplementary Table 1).
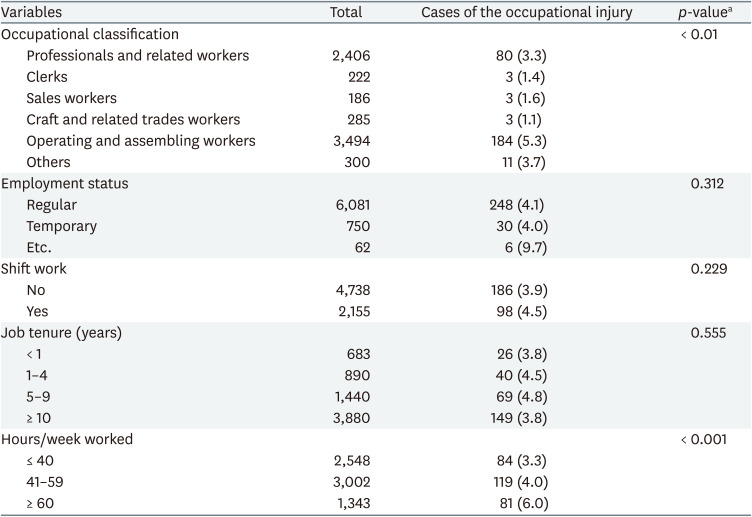
Occupational characteristics
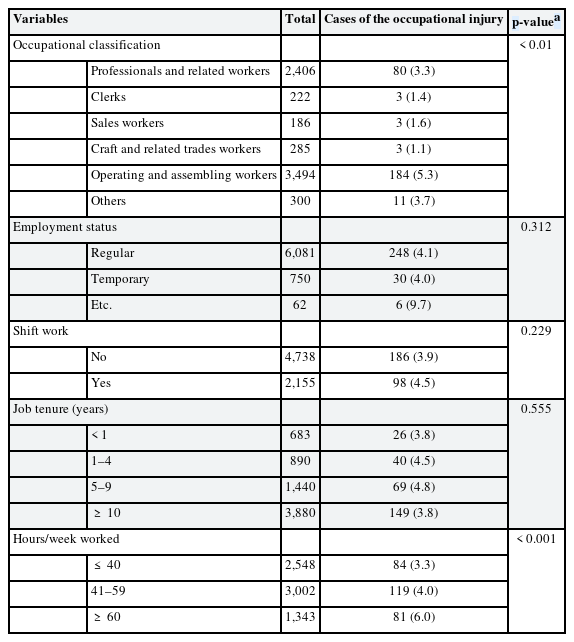
Occupational injury rates significantly depended on occupational classification (p < 0.01). Risk of occupational injury significantly increase with working hours from 3.3% for those that worked < 40 hours per week, to 4.0% at 41–59h ours per week, and to 6.0% at ≥ 60 hours per week. No significant relation was observed between occupational injury rate and job tenure (<1, 1–4, 5–9, or ≥ 10 years), employment status, or shift work (Table 2). Non-shift work group showed similar results to the overall population (Supplementary Table 2).
Association between nicotine dependency and occupational injury
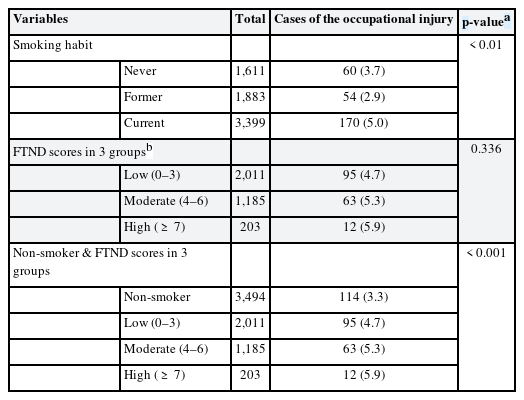
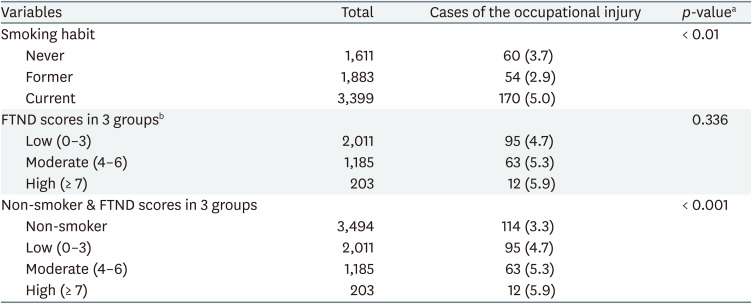
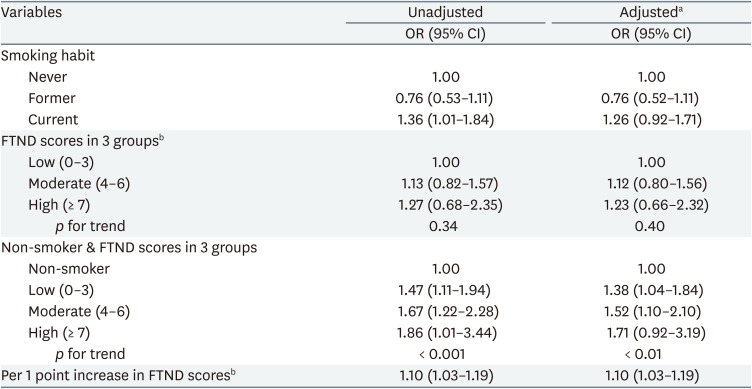
Table 3 shows occupational injury rates with respect to smoking statuses and FTND scores. The occupational injury rate in the current smoking group was 5.0%, which was significantly higher than in the other groups (p < 0.01), and higher in the high nicotine dependence group (5.9%) than in the moderate (5.3%), low (4.7%) groups or non-smoker (3.3%) (p < 0.001). After stratifying the data by working type and working hours per week, there were similar tendency except for the group that works more than 60 hours per week (Supplementary Table 3).
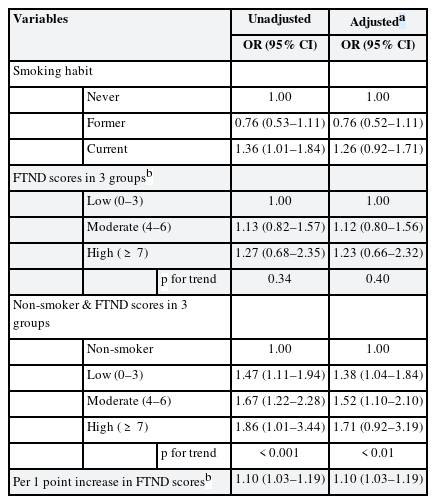
The unadjusted ORs of occupational injury in the low, moderate, and high nicotine dependence groups were 1.47 (95% confidence interval [CI]: 1.11–1.94), 1.67 (95% CI: 1.22–2.28), and 1.86 (95% CI: 1.01–3.44), respectively. The adjusted ORs for the low, moderate, and high nicotine dependence groups were 1.38 (95% CI: 1.04–1.84), 1.52 (95% CI: 1.10–2.10), and 1.71 (95% CI: 0.92–3.19), respectively. In fact, adjusted ORs tended to increase linearly as nicotine dependence increased (p for trend < 0.01) (Table 4).
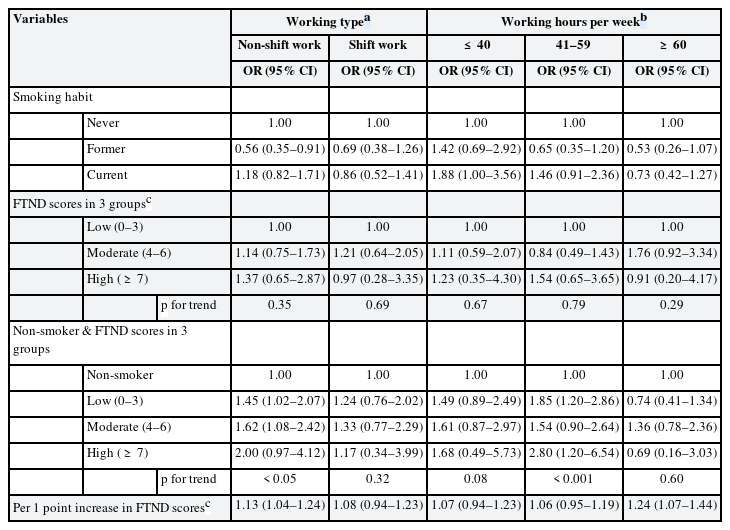
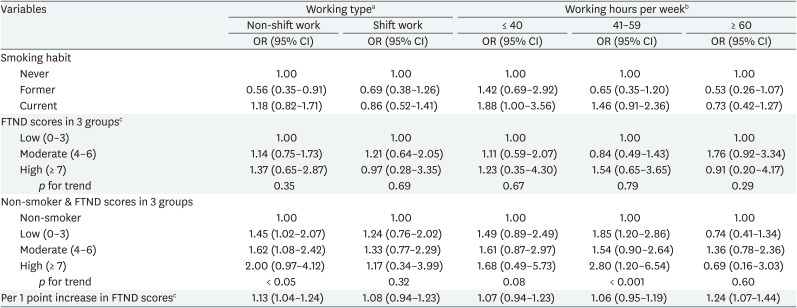
Analysis of continuous FTND scores for current smokers only showed that adjusted ORs increased by 1.10 (95% CI: 1.03–1.19) per FTND point. With FTND score as a continuous variable, the non-shift work group maintained this relationship (OR: 1.13, 95% CI: 1.04–1.24) and OR was higher in the group that works more than 60 hours per week (OR: 1.24, 95% CI: 1.07–1.44) (Table 5).
DISCUSSION
In the present study, the nicotine dependence test (Korean version of the FTND) showed that those with high nicotine dependence group had a higher occupational injury rate than those with low nicotine dependence group, and that the risk of occupational injury tended to increase linearly with nicotine dependence score. Furthermore, we found an interesting result with higher intensity of this effect in non-shift work group than in shift work group. The intensity of the effect of long working hours was higher in the group that works more than 60 hours per week.
One of the possible explanations for nicotine dependency being related to occupational injury is nicotine withdrawal symptom [19]. Animal studies using intracranial self-stimulation (ICSS) have observed that nicotine decreases ICSS threshold, indicating a shift in the reward threshold consistent with its hedonic effects [20]. In contrast, nicotine withdrawal increases ICSS threshold, indicative of an anhedonic state [21]. High level of Nicotine Dependence (FTND) score is related with a high frequency of nicotine withdrawal symptoms such as irritation, nervousness, restlessness, and difficulty in concentration [22] that may lead to occupational injury. The week of No Smoking Day (NSD) generally was generating an excess of reported accidents in UK [23]. Since 1984, the second Wednesday of March has been known as NSD in the UK.
Nicotine withdrawal actually affects the performance of workers. One study observed decrements in performance (i.e., slower reaction time) on the RVIP (Rapid Visual Information Processing) as soon as 30 min post cessation [24]. Serial reaction time task performance of smokers during nicotine withdrawal is poorer than that of non-smokers; whereas the performance of smokers improves after administration of nicotine [25]. Significant withdrawal-induced decreases in blood-oxygen-level-dependent (BOLD) signal in working memory-related brain regions were observed at the highest task loads during an n-back task. In highly dependent smokers, decreased BOLD signal in withdrawal correlated with poorer [26]. Following overnight abstinence, nicotine withdrawal impairs response inhibition across a variety of tasks, including the stop task [27].
Some studies suggested that work conditions are related to smoking or nicotine dependency. Workers who work long hours have difficulty trying to smoking cessation [28]. One study found that a high percentage of night-shift workers are smokers, and they have a tendency to smoke in the workplace [29]. Another study reported that the prevalence of smoking increases with the shift work or long working hours [30]. During anxiety and stress-provoking situations like shift work or long working hours, the sedative effect of nicotine can help reduce muscle tension, stabilize the mood, and reduce aggression [31]. Possibly because shift work and long working hours cause emotional stress, it is difficult to quit smoking [32].
Many previous studies presented that the circadian disruption can increase the risk of substance abuse as circadian misalignment tends to increase reward sensitivity and impulsivity [333435]. Genes that regulate circadian rhythms play a role in regulating dopaminergic reward circuitry, and that regulation can contribute to addictive tendencies [3637]. Individuals who have high nicotine dependency in non-shift work group with less these circadian disturbances or stress from shift work may be biologically more sensitive or vulnerable to nicotine. Moreover, the group that works more than 60 hours per week should be more cautious because the higher the nicotine dependency, the greater the intensity of the increase risk of occupational injury. However, because of lack of studies on the relationship between working condition and nicotine dependency, additional longitudinal studies on working condition and nicotine dependency are needed.
There may be an additional possible reason why the effect of nicotine dependency in this study was greater in the non-shift work group. Although there was no statistical significance, the occupational injury rate in the overall study population was higher in the shift work group (4.5%) than non-shift work group (3.9%). In addition, the occupational injury rate in the non-smoker group which is the reference group in the logistic regression analysis was higher in the shift work group (3.8%) than in the non-shift work group (3.0%) (Supplementary Table 3). Therefore, it is likely that the ORs for occupational injury by nicotine dependency was rather lower in the shift work group. In other words, even if both shift work and nicotine dependency increase the risk of occupational injury, if the effect of shift work is greater than that of nicotine dependency, the ORs for occupational injury by nicotine dependency may be higher in the non-shift work group.
The present study has a number of limitations that warrant consideration. Firstly, some information, including information on nicotine dependence and occupational injury, was obtained using a self-administered questionnaire, which means responses were dependent on individual subjectivity. In particular, subjects with high nicotine dependence were more likely to remember or overreport occupational injuries. It was not reported whether occupational injury required more than four days of medical treatment that is legally recognized. We tried to minimize recall bias by asking about occupational injury experiences during previous 12 months. Second, some workers might fail to assess the second survey, if they had experienced occupational injury or long-term leave just before the second survey. Also, there was no follow up on the change in smoking status or nicotine dependency during the survey period. Third, break times, smoking cessation policies, and working characteristics differed widely. The purpose of this study was to understand the relationship between nicotine dependence and work experience, and thus, we did not include some factors (e.g., individual workplaces, additional understanding of the break times, the smoking cessation policy, working characteristic in the workplace) that might affect occupational injury rates. To devise measures to prevent occupational injuries, additional understanding of workplace practices is needed.
Although many studies have examined the relationship between smoking and occupational injury, most examined the relationship between smoking status or second-hand smoke exposure and occupational injuries, and relatively few studies found any relation between occupational injuries and nicotine dependence. The strength of this study is that it was conducted to determine the relationship between nicotine dependence and occupational injury by surveying a large sample of Korean men with different types of jobs.
CONCLUSIONS
We found that higher levels of nicotine dependence might associated with higher occupational injury rates. It would be best to quit smoking. However, from a short-term perspective, the present study indicates that addressing worker's nicotine dependence by giving an adequate break time or smoking area might reduce work-related injuries. Future studies should address not only nicotine dependency but also additional understanding of workplace practices such as break times, smoking cessation policies, and working characteristics.
Notes
Competing interests: The authors declare that they have no competing interests.
Author Contributions:
Conceptualization: Jang SW, Kim HC.
Formal analysis: Jang SW, Kim HC.
Investigation: Jang SW, Kim HC.
Supervision: Park SG, Leem JH.
Writing - original draft: Jang SW.
Writing - review & editing: Kim HC, Kim JH, Kim MS, Won Y, Ju H, Kim HD, Choi G, Park SG, Leem JH.
Abbreviations
BOLD
blood-oxygen-level-dependent
CI
confidence interval
FTND
fagerstrom test of nicotine dependence
ICSS
intracranial self-stimulation
NSD
no smoking day
OR
odds ratio
RVIP
rapid visual information processing
References
SUPPLEMENTARY MATERIALS
Supplementary Table 1
Prevalence of occupational injury according to general characteristics, stratified by working type and working hours per week
Supplementary Table 2
Prevalence of occupational injury according to occupational characteristics, stratified by working type and working hours per week
Supplementary Table 3
Prevalence of occupational injury according to smoking status and FTND scores, stratified by working type and working hours per week